Enferm Bras.
2023;22(2):211-18
CASE REPORT
Post-polio syndrome induced by Long Covid?
Marco Orsini1,
Daniel Antunes Pereira1, Mauricio de Sant Anna Jr2,
Phamela de Freitas Geraldo Antunes3, Luciana Armada Dias1, Antonio Marcos da Silva Catharino1
1Universidade Iguaçu (UNIG), Nova Iguaçu, RJ, Brazil
2Instituto Federal de Educação, Ciência e Tecnologia
(IFRJ), Rio de Janeiro, RJ, Brazil
3Hospital HEMORIO, Rio de Janeiro, RJ, Brazil
Recebido
em: 20 de fevereiro de 2023; Aceito em: 11 de abril de 2023.
Correspondence: Marco Orsini, orsinimarco@hotmail.com
Pereira DA, Orsini MA, Sant Anna Jr M, Antunes PFG, Dias LA, Catharino
AMS. Post-polio syndrome induced by Long Covid? Enferm
Bras. 2023;22(2):211-18 doi: 10.33233/eb.v22i2.5462
Abstract
Introduction: A disease known as post-polio syndrome (PPS)
develops 30 to 40 years after an individual has been acutely infected with the
paralytic and non-paralytic poliovirus. The most recognizable symptoms are the
gradual development of muscle atrophy and wasting accompanied by joint and
muscle discomfort. Long covid is a syndrome of
persistent symptoms of COVID-19 and is challenging to diagnose, but it is
believed to appear three to twelve weeks after infection. Notably, there still
needs to be a confirmed correlation between COVID-19 and PPS, hence the
importance of this report. Case report: CRC, 58 years old, female,
history of Acute Anterior Poliomyelitis at age 4. The disease affected all four
limbs, with several surgical interventions on the spine, in addition to 3
tendon transpositions. In 2021, after acute infection with Sars-Cov-2, she
began a clinical condition marked by alopecia, dyspnea on medium exertion, and
new paresis in the upper and lower limbs and trunk. She had initially been
diagnosed with Long Covid, but after a neurological
examination, she found signs and symptoms consistent with Post-Polio Syndrome. Conclusion:
This case report highlights the complex need for understanding and further
studies of the possible relationship between PPS and Long Covid.
In addition, patients need rehabilitation to regain independence after
diagnosis of PPS after Sars-Cov 2 infection.
Keywords: postpoliomyelitis
syndrome, neurologic manifestations, SARS-CoV-2.
Resumo
Síndrome
pós-pólio induzida por Covid longa?
Introdução: A síndrome pós-pólio (SPP)
desenvolve-se geralmente décadas após o episódio agudo de poliomielite
anterior. Os sintomas mais reconhecíveis são o desenvolvimento gradual de
amiotrofia e danos musculares, acompanhados de lesões articulares. Covid longa é caracterizada como uma síndrome, com sintomas
persistentes de COVID-19. Acredita-se que emerge após 3 semanas da primoinfecção. Ressaltamos que deve haver uma correlação
confirmada entre COVID-19 e SPP - fato que justifica a importância da
apresentação do caso. Relato de caso: CRC, 58 anos, sexo feminino,
antecedentes de Poliomielite Anterior Aguda aos 4 anos. A doença afetou as
quatro extremidades, com várias intervenções cirúrgicas na coluna vertebral,
além de 3 transposições tendinosas. Em 2021, padeceu por infecção aguda por
Sars-Cov-2, iniciando quadro clínico por alopecia, dispneia e paresia nos
membros e tronco. Inicialmente, o diagnóstico clínico fora somente de Covid longa, mas, após minucioso exame neurológico e exames
complementares, sinais e sintomas compatíveis com o Síndrome Pós-Pólio
faziam-se presentes. Conclusão: O artigo de caso destaca a necessidade
de compreender e realizar mais estudos sobre a possível relação entre PPS e Covid longa. Além disso, os pacientes necessitam de
reabilitação física direcionada, visando otimizar a independência funcional
depois do diagnóstico de SPP após infecção de Sars-Cov-2.
Palavras-chave: síndrome pós-poliomielite;
manifestações neurológicas; SARS-CoV-2.
Resumen
Síndrome
post-polio causada por COVID largo?
Introducción: Una enfermedad
conocida como síndrome post-polio
(PPS) se desarrolla de 30 a 40 años
después de que un individuo
ha sido infectado de forma aguda anteriormente. Los síntomas más reconocibles son el desarrollo
gradual de atrofia y desgaste muscular acompañado de molestias en las
articulaciones y los
músculos. El covid largo es un
síndrome de síntomas persistentes de COVID-19 y es
difícil de diagnosticar, pero se cree que aparece de tres a doce semanas después de la infección. En
particular, aún debe haber una correlación confirmada
entre COVID-19 y PPS, de ahí la
importancia de este informe. Reporte de caso:
CRC, 58 años, sexo femenino,
antecedentes de Poliomielitis Anterior Aguda a los 4 años. La enfermedad afectó a las cuatro extremidades, con varias intervenciones quirúrgicas en la columna, además
de 3 transposiciones tendinosas. En
2021, tras infección aguda
por Sars-Cov-2, inició cuadro
clínico caracterizado por alopecia, disnea de
medianos esfuerzos y nuevas
paresias en miembros
superiores e inferiores y tronco. Inicialmente le habían diagnosticado Covid largo,
pero después de un examen neurológico, se encontró
signos y síntomas compatibles
con el Síndrome Post-Polio. Conclusión: Este
informe de caso destaca la compleja
necesidad de comprender y
realizar más estudios sobre la
posible relación entre PPS
y Covid largo. Además, los pacientes necesitan rehabilitación para recuperar la independencia después del diagnóstico de PPS después de
la infección por
Sars-Cov-2.
Palabras-clave: síndrome pospoliomielitis; manifestaciones neurológicas; SARS-CoV-2.
Introduction
Acute Anterior Poliomyelitis (AAP)
is a disease of viral etiology (caused by three types of poliovirus - I, II,
and II - of the enterovirus genus). In summary, it destroys the lower motor
neurons of the spinal cord, brain, and brainstem, through viral invasion
(sensory neurons are spared) [1,2]. As a result, it ends up causing a flaccid
and asymmetrical paralysis of the muscles of the spine and lower limbs [1,3,4], which can be partial or total.
An illness known as post-polio
syndrome (PPS) develops 30 to 40 years after an individual has been acutely
infected with the paralytic and non-paralytic poliomyelitis virus [2,5]. The
most recognizable symptoms are gradually developing muscular atrophy and
weakening accompanied by joint and muscle discomfort [6]. These symptoms may
appear in both clinically afflicted and unaffected muscles during a primary
polio infection. After polio (PPMA), progressive muscle atrophy is used when
just the limb muscles are weak. Muscle weakness typically develops gradually
over many years [3,7].
After a COVID-19 infection,
persistent symptoms are called "Long COVID." Long COVID is
challenging to diagnose, but it is thought to appear three to twelve weeks
after infection [8,9].
It is worth noting that there is
still no confirmed correlation between COVID-19 and PPS. Therefore, the
importance of this report already finds resonance in other reports in the
literature. Many central and peripheral nervous system manifestations
associated with coronavirus disease-19 (COVID-19) infection have been reported
in the literature in recent years. In addition to neurological manifestations,
we may still have much to learn about this new virus's neuropathological
mechanism of infection [10].
Case report
CRC, 58 years old, woman,
businesswoman. History of Acute Anterior Poliomyelitis at age 4. At the time,
she remained hospitalized with severe respiratory impairment, with the use of
“lungs of steel.” The disease compromised the four limbs, with several surgical
interventions in the spine, in addition to 3 tendon transpositions (Figures 1,
2, and 3). In 2021, after acute Sars-Cov-2 (asymptomatic) infection, she
started a clinical picture marked by alopecia, dyspnea on medium exertion, and
new paresis in the upper and lower upper limbs and trunk. She had initially
received a diagnosis of Long Covid, but after a
neurological examination, she found signs and symptoms compatible with
Post-Poliomyelitis Syndrome. Currently, her clinical condition remains stable,
and she is taking an antidepressant (desvenlafaxine 100mg/day). Electroneuromyographic examination showed chronic
preganglionic motor impairment (anterior tip) of myotomes usually supplied by
C5-T1 and L2-S1 roots. Signs of acute denervation were observed in muscles of
the shoulder girdle and upper limbs. Respiratory Function Test: moderate
restrictive ventilatory disorder. Standard Lab. Cardiac Function: Normal. After
an acute and long viral infection, we believe that Sars-Cov-2 may have
compromised already weakened neurons in the anterior tip of the spinal cord,
triggering PPS.

Figure 1 - Tendon transposition in the
anterior tibial of the right lower limb

Figure 2 - Genu recurvatum of the knee
joint with right pelvic girdle elevation
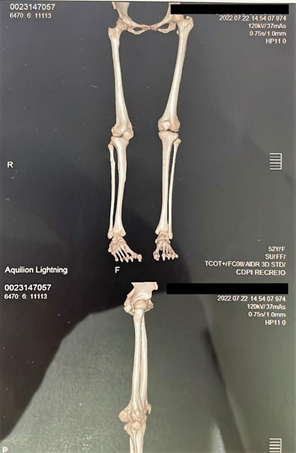
Figure 3 - Internal hip rotation with
inverted tibiotarsal joint and plantar flexion.
Compensatory tibial peroneal rotation
Discussion
Numerous ideas are looking at the
origins of PPS. One of the theories has a pathophysiology that is similar to
shingles. It is thought to be a reactivation of the dormant virus that prevents
reinnervation and causes motor neurons to continue degenerating. Not every
person with polio experiences viral reactivation [1,4].
Other hypotheses include an
autoimmune disorder affecting the motor neurons brought on by prior
poliomyelitis. The presence of elevated protein and oligoclonal bands in the
CSF of some PPS patients serves as evidence for this [7,11].
So far, the literature needs to
bring more evidence to support such theories. However, both can be highlighted
as possibilities for a pathophysiological explanation of the case suggested in
this article. Of these, the most significant emphasis is on the first
hypothesis mentioned above.
Long-term tissue damage brought on
by COVID-19 infection may be related to neurological symptoms in COVID
patients. Through the olfactory bulb, the SARS-CoV-2 virus can affect the
central nervous system, causing neuroinflammation that damages the neuron and,
because neurons rarely regenerate, long-lasting neuronal dysfunction that could
cause neurological symptoms in long-term COVID [9]. This neuronal damage may be
related to the onset of PPS. There was no definite evidence to support the
direct neuro pathogenicity of SARS-CoV-2 [12].
One of the first methods to reduce
PPS symptoms were active motor rehabilitation through gradual muscle
strengthening. Thus, some muscle mechanisms polio survivors adapt during
rehabilitation programs [13,14].
Several rehabilitation strategies
are possible for PPS, aiming to readjust the affected individual's lifestyle
and activities. It is also worth mentioning that pulmonary rehabilitation, with
and without physical/aerobic component, can improve pulmonary, physical, and
psychosocial functions in patients with COVID-19 or Long Covid
and patients with PPS, in view of the respiratory impairment in both diseases
at their levels of involvement [14].
However, overuse or overtraining
should be avoided, given the muscle injury that may occur and the
pathophysiological sequelae of the diseases in question, as they affect
musculoskeletal structures, glycogen depletion, fatigue, oxidative stress,
cytokine storm, and others [15].
Conclusion
This case report highlights the
complex need for understanding and further studies of the possible relationship
between PPS and Long Covid, especially in the
pathophysiological mechanisms for neuropathies that may be related to the
coronavirus. In addition, patients need rehabilitation to regain independence
after diagnosing of PPS after Sars-Cov 2 infection.
Conflict of interest
No conflict of interest associated with the article
Funding
This study did not receive financing
Author’s contributions
All authors contributed equally during the writing
of the work. Whether in the search for references, review of the clinical case and
discussion.
Acknowledgements
The authors would like to thank FAPERJ and Institute
of Radiology Lara Brandão
References
- Lima V,
Fernanda F, Quadros AAJ, Oliveira OAB, Fontes SV, Fávero FM. Estudo
retrospectivo do comportamento da força muscular em pacientes com Síndrome
Pós-Poliomielite. Rev Neurocienc.
2014;22(3):351-8. doi: 10.34024/rnc.2014.v22.8066 [Crossref]
- Silva
LJ. Poliomielite: a próxima na lista da erradicação? Boletim Epidemiológico
Paulista [Internet]. 2014 [cited 2022 jul 10]; Available from:
https://docs.bvsalud.org/biblioref/ses-sp/2014/ses-36364/ses-36364-6158.pdf
- Durante ALTC, Poz MRD. Global Health and Brazilian Health responsibility: the case of polio eradication. Saúde em Debate. 2014;38:129-38. doi: 10.5935/0103-104.20140007 [Crossref]
- Barbosa FSS. Demographic profile of patients with
post-polio syndrome in JI-Paraná city Rondônia state: correlations with physioterapeutic rehabilitation. Revista Científica da Faculdade de
Educação e Meio Ambiente [Internet]. 2014 [cited 2022 Jul 10]; Available
from: https://revista.faema.edu.br/index.php/Revista-FAEMA/article/view/198/358
- Pastuszak Ż, Stępień A, Tomczykiewicz K, Piusińska-Macoch R, Galbarczyk D, Rolewska A. Post-polio syndrome. Cases report and review of literature. Neurol Neurochir Pol. 2017;51(2):140-5. doi: 10.1016/j.pjnns.2017.01.009 [Crossref]
- Balzien B, Hofner B, Harlander-Weikert E, Frommelt P, Bork H, Forst R, et al. Musculoskeletal symptoms in patients with post-polio syndrome. Z Orthop Unfall. 2014;152(3):241-6. doi: 10.1055/s-0034-1368531 [Crossref]
- Sáinz MP, Pelayo R, Laxe S, Castaño B, Capdevilla E, Portell E. Describing post-polio syndrome. Neurologia. 2022;37(5):346-54. doi: 10.1016/j.nrl.2019.03.011 [Crossref]
- Greenhalgh T, Knight M, A’Court C, Buxton M, Husain L. Management of post-acute covid-19 in primary care. BMJ. 2020;370. doi: 10.1136/bmj.m3026 [Crossref]
- Pinzon RT, Wijaya VO, Jody A al, Nunsio PN, Buana RB. Persistent neurological manifestations in long COVID-19 syndrome: A systematic review and meta-analysis. J Infect Public Health. 2022;15(8):856-69. doi: 10.1016/j.jiph.2022.06.013 [Crossref]
- Agircan D, Ethemoglu O, Gesoglu-Demir T. COVID-19 and post-poliomyelitis syndrome: coincidence? Ideggyogy Sz. 2022;75(5/6):207-10. doi: 10.18071/isz.75.0207 [Crossref]
- Howard RS. Poliomyelitis and the postpolio
syndrome. BMJ. [Internet]. 2005 Jun 6 [cited 2022 dec
19];330(7503):1314. doi: 10.1136/bmj.330.7503.1314 [Crossref]
- Maury A, Lyoubi A, Peiffer-Smadja N, de Broucker T, Meppiel E. Neurological manifestations associated with
SARS-CoV-2 and other coronaviruses: A narrative review for clinicians. Rev
Neurol (Paris) [Internet]. 2021 Jan 1 [cited 2023 Feb 21];177(1/2):51-64.
Available from: https://pubmed.ncbi.nlm.nih.gov/33446327/
- Tiffreau V, Rapin A, Serafi R, Percebois-Macadré L, Supper C, Jolly D, et al. Post-polio syndrome and rehabilitation. Ann Phys Rehabil Med. 2010;53(1):42-50. doi: 10.1016/j.rehab.2009.11.007 [Crossref]
- Debeuf R, Swinnen E, Plattiau T, de Smedt A, de Waele E, Roggeman S, et al. The Effect of physical therapy on impairments in COVID-19 patients from intensive care to home rehabilitation: A rapid review. J Rehabil Med. 2022;54. doi: 10.2340/jrm.v53.8 15 [Crossref]
- Cardoos N. Overtraining syndrome. Curr Sports Med Rep. 2015;14(3):157-8. doi: 10.1177/194173811143440 [Crossref]