ARTIGO ORIGINAL
Functional capacity of patients with chronic stroke
based upon their physical activity levels
Capacidade funcional de indivíduos
pós-acidente vascular cerebral crônico baseada nos níveis de atividade física
Janaine C. Polese*,
Thaianne C. Servio**, Gabriela S. S. Chaves**, Luci F. Teixeira-Salmela**
*Department
of Physical Therapy, Universidade Federal de Minas Gerais, Belo Horizonte/MG,
Department of Physical Therapy, Faculdade Ciências Médicas de Minas Gerais,
Belo Horizonte/MG, **Department of Physical Therapy, Universidade Federal de
Minas Gerais, Belo Horizonte/MG
Recebido em 15 de
novembro de 2016; aceito em 11 de maio de 2017.
Corresponding
author:
Janaine Cunha Polese, PhD, Departamento de Fisioterapia, Universidade Federal
de Minas Gerais, Avenida Antônio Carlos, 6627, Campus Pampulha 31270-901 Belo
Horizonte MG, E-mail: janainepolese@yahoo.com.br; Thaianne Servio:
thaiservio@hotmail.com; Gabriela Chaves: gabischaves@hotmail.com; Luci Fuscaldi
Teixeira-Salmela: jhsalmela@hotmail.com
Abstract
Introduction: People with stroke commonly show low levels of physical activity and
reduced functional capacity, independent of the severity of the impairments.
The use of simple measures that are able to produce transferable information
from clinical practice to life in society is crucial within clinic contexts. Objective: To compare the functional
capacity of patients with chronic stroke based upon their physical activity
levels. Methods: For this cross
sectional study, functional capacity and levels of physical activity were
assessed by the Duke Activity Status Index (DASI) and the adjusted activity
score (AAS) of the Human Activity Profile (HAP), respectively. One-way analysis
of variance (ANOVA), followed by LSD post-hoc tests were employed to
investigate differences between the physical activity groups regarding their
DASI scores. Results: Fifty-one
individuals with mean age 58.8 ± 13.5 and a mean time since the onset of stroke
of 25.5 ± 13.9 months participated. According to their HAP AAS, 18 individuals
were classified as impaired, 28 as moderately active, and five as active.
Between-group differences were observed for the DASI scores [F(2,48)=13.72;
p < 0.01]. Conclusion: Increases
in functional capacity were observed with increases in physical activity
levels.
Key-words: stroke,
motor activity, activities of daily living.
Resumo
Introdução: Indivíduos pós acidente vascular cerebral (AVC) geralmente apresentam
baixos níveis de atividade física e redução da capacidade funcional,
independente da gravidade. O uso de medidas simples, capazes de transferir
informações da prática clínica para a vida em sociedade, é crucial dentro do
contexto clínico. Objetivo: Comparar
a capacidade funcional dos indivíduos com AVC crônico estratificados pelo nível
de atividade física. Métodos: Para
este estudo transversal, a capacidade funcional e os níveis de atividade física
foram avaliados pelo Duke Activity Status
Index (DASI) e pelo escore de atividade ajustado (EAA) do Perfil de
Atividade Humana (PAH), respectivamente. Análise de variância One-way (ANOVA), seguida de testes
post-hoc LSD foram realizados para investigar diferenças entre os níveis de
atividade física considerando os escores do DASI. Resultados: Cinquenta e um indivíduos com idade média de 58,8 ±
13,5 anos e tempo médio pós AVC de 25,5 ± 13,9 meses
participaram. De acordo com o EAA PAH, 18 indivíduos foram classificados como
inativos, 28 como moderadamente ativos, e 5 como
ativos. Diferenças entre-grupos foram observadas para os escores do DASI [F(2,48)
= 13,72; p < 0,01]. Conclusão:
Aumentos na capacidade funcional foram observados com aumentos nos níveis de
atividade física.
Palavras-chave: acidente vascular
cerebral, atividade física, atividades cotidianas.
Introduction
Physical activity practice has shown to positively influence multiple
physical and psychosocial domains after stroke [1]. The literature supports
that exercise after stroke improve cardiovascular
fitness [2], walking ability [3] and strength of the upper-extremity and
lower-extremity muscles [4]. Additionally, the benefits of physical activity on
depressive symptoms, memory, and fatigue were reported [5-7]. Although it is it
well known the importance of physical activity practice, stroke individuals
commonly demonstrate low levels of physical activity [8].
Functional capacity after stroke is also frequently reduced, independent
of the severity of the impairments [9]. Since functional capacity is related to
physiological variables, i.e., oxygen consumption, the use of simple and
reliable measures is crucial within clinical environments. Although the Duke
Activity Status Index (DASI) was originally developed for the evaluation of
patients with cardiovascular diseases [10], it has also been used with stroke
individuals, since its scores were shown to be highly related to physical
performance measures [11].
Also, DASI showed significant positive correlations with VO2 max (r =
0.51, p <0.001) in patients with cardiovascular diseases [10]. In addition,
this instrument was correlated with the distance covered in the six-minute walk
test (r = 0.55) in patients with chronic obstructive pulmonary disease (COPD)
[12]. In this sense, the instrument was validated and have
adequate measurement properties for different populations.
Given the need to use simple clinical measures, which are able to
produce transferable information from clinical practice to life in society, the
aim of this study was to compare functional capacity of chronic stroke individuals,
based upon their physical activity levels. Therefore, the specific research
question for this study was: Stroke individuals with different levels of
physical activity show differences in functional capacity?
Material and methods
Participants
For this cross-sectional study, people with chronic stroke were
recruited from the general community of the city of Belo Horizonte, Brazil from
September to December 2014. They were included if they: were ≥ 20 years
of age; had a mean time since the onset of a unilateral stroke between one and
five years, and were able to walk independently. They were excluded if they had
cognitive deficits, as determined by the Mini-Mental State Examination
Brazilian cut-off scores (18/19 for illiterate individuals and 24/25 for those
with a basic education) [13] and/or had any other neuromuscular and
musculoskeletal disorders. As participants provided written consent, based upon
previous approval from the Institutional ethical review board (CAAE:
0254.0.203.000-11).
First, for characterization purposes, all participants underwent a
physical examination and an interview for the collection of clinical,
anthropometric, and demographic data, which included age, sex, body mass,
height, time since the onset of the stroke, number of medications, associated
diseases, and comfortable walking speed (10-meter walking test) [14].
Following, clinical measures of functional capacity and physical activity
levels were collected by one trained researcher.
Functional capacity
The participants’ perceived functional capacity was assessed by the
Brazilian version of the DASI [10,15], which has
demonstrated adequate measurement properties [10]. The DASI scores reflect the
role of physiological factors on the individuals’ daily lives and consider all
relevant spheres related to functional capacity status, including personal
care, ambulation, household tasks, sexual function, and recreation [16]. The
DASI contains 12 items with a yes/no response format, which describes activities
of daily living and their correspondent metabolic equivalents (METS). Its
scores range from zero to 58.2 and higher scores indicates greater functional
capacity.
Levels of physical activity
The individuals’ levels of physical activity were assessed by the
Brazilian version of the HAP [17], a survey including 94 activities, such as
self-care, transportation, home maintenance, entertainment/social, and physical
exercises, which are sequentially rated according to their required metabolic equivalents,
so that a score of 1 represents the lowest and 94 the highest metabolic
equivalent value. For example, item number 1 corresponds to getting in and out
of chairs or bed without help, whereas item number 94 corresponds to running or
jogging 4.8 kilometres in 30 minutes or less.
For each item, there were three possible responses: “still doing the
activity”, “have stopped doing the activity”, and “never did the activity”. The
administration and scoring procedures followed recommended protocols [18,19] and scores were tallied to provide a maximum activity
score, which indicated the highest metabolic equivalent activity level, at
which the individual could still perform. An adjusted activity score (AAS) was
determined by subtracting the number of activities that the respondent had
discontinued performing from the maximum score and indicated the average
typical metabolic equivalent levels. From the AAS values, the participants were
classified into impaired (AAS<53), moderately activity (53<AAS<74), and
active (AAS>74) [18]. Coefficients for test-retest reliability have been
reported at 0.84 for the maximum and 0.79 for the adjusted activity scores
[20].
Data analyses
Descriptive statistics and tests for normality (Shapiro-Wilk) were
carried-out for all outcomes. Kruskal-Wallis was
performed, followed by Mann-Whitney a post-hoc test was employed to investigate
differences between the impaired, moderately active, and active groups
regarding their DASI scores. All analyses were performed with the SPSS for
Windows software (Version 17.0) with a significance level of 5%.
Results
Participants’ characteristics
Fifty-one individuals, 33 men, mean age 58.8±13.5 years and a mean time
since the onset of the stroke of 25.5 ± 13.9 months, participated. Their mean
DASI and AAS scores were 29.8 ± 13.5 and 54.7 ± 16, respectively. Based upon
their AAS scores, 18 participants were classified as impaired, 28 as moderately
active, and five as active. Their characteristics are described in Table I
Table I - Characteristics of the participants
expressed in Mean ± SD and percentage (n=51).
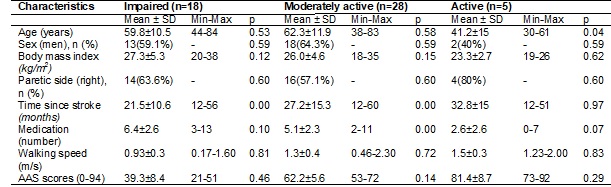
Shapiro-Wilk
test was performed no evaluate normality; AAS = Adjusted activity scores of the
Human activity profile.
Functional capacity according to the physical activity
levels
Table II shows the comparisons between the impaired, moderately active,
and active groups regarding their DASI scores. Between-groups differences were
observed for the DASI scores [F(2,48)=13.72;
p<0.01], indicating that individuals with higher levels of physical activity
demonstrated higher functional capacity.
Table II - Mean (SD) DASI scores of the impaired,
moderately active, and active groups, mean (SD) and mean (95% CI) of the
differences between groups (n = 51).
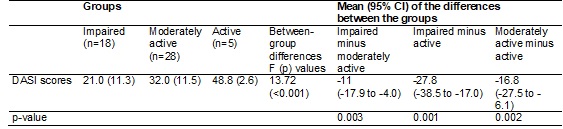
Test
used was Kruskal-Wallis and Mann-Whitney post-hoc
test.
Discussion
This was the first study that used two simple questionnaires for the
assessment of functional capacity and levels of physical activity after stroke.
Both questionnaires are simple, accessible and easily applicable in clinical
practice. The results of this study answered the main question, since it was
found that the individuals with stroke with higher levels of physical activity
demonstrated higher functional capacity, i.e., present higher METS energy cost
(in METS). Recently, the study of Polese et al. [11] was the first to use the
DASI for the assessment the functional capacity of a sample of 31 chronic
stroke individuals, and found a mean DASI score of 27.3. This value was similar
to that observed in the present study for the moderately active group, who
showed a mean DASI score of 32.0 (SD 11.5).
In a previous study with 98 chronic stroke individuals, Polese et al.
[21] reported that stroke individuals with higher levels of physical
activity, as determined by the HAP scores, showed higher levels of functional
capacity, as demonstrated by the distance covered during the 6-minute walking
test (6MWT). They also found that individuals, who had lower strength deficits
of the lower limb muscles, had higher physical activity levels. These findings
corroborate those of the present study. However, in the present study,
functional capacity was assessed with a simple and low-cost questionnaire,
which does not depend on the environment context, like the 6MWT.
Previous studies have demonstrated that the encouragement of physical
activity practice in stroke individuals resulted in beneficial effects on
physiological, psychological, sensorimotor, strength, endurance, and functional
measures [22-25]. Substantial health benefits are obtained from accumulating
150 minutes per week of moderate intensity or 75 minutes per week of
vigorous-intensity aerobic activity, associated with strengthening exercises of
moderate to high intensity performed ≥2 days per week [1,26]. Although it is well recognized the benefits of high
levels of physical activity practice [1], little is known about the intensity
of free-living physical activity in stroke individuals [27]. In this sense,
only about 10% of the sample in the present study was considered active.
Chronic stroke individuals are able to perform about 50% of their peak
oxygen consumption and their oxygen cost of walking is elevated, compared to
that of able-bodied individuals of similar body weight [28]. They often show
reduced fitness and are predisposed to sedentary lifestyles, which limit them
to perform activities of daily living and contribute to increased risks for
recurrent stroke and cardiovascular diseases [28]. Additionally, the sedentary
behavior is an independent risk factor for cardiovascular diseases [27]. Thus,
the results of the present study support the importance of assessing functional
capacity, based upon the physical activity levels of these individuals, to
better guide clinical practice.
Due to the nature of the study design, causal relationships between the
studied variables cannot be determined. In addition, the data was not equally
distributed between the groups regarding their physical activity levels, and
this factor could influence the results. However, it is not common to find
stroke individuals with high levels of physical activity in real life. It was
observed a statistically significant difference in the baseline between the
impaired, moderately active and active groups in the variables age, time since
stroke and medication. These differences could be influenced by the different
levels of physical activity of the individuals. Finally, the findings of the
present study could not be extrapolated to individuals with different
characteristics from the studied sample.
Conclusion
In conclusion, physical activity levels of chronic stroke individuals
influence their levels of functional capacity. Higher functional capacity was
observed with increases in physical activity levels.
Support
Brazilian National Funding Agencies (CAPES, CNPQ and
FAPEMIG).
References
- Billinger SA, Arena R,
Bernhardt J, Eng JJ, Franklin BA, Johnson CM et al.
Physical activity and exercise recommendations for stroke survivors: a
statement for healthcare professionals from the American Heart
Association/American Stroke Association. Stroke 2014;45(8):2532-53.
- Pang MY, Eng JJ, Dawson AS, Gylfadottir S. The use of aerobic exercise training in
improving aerobic capacity in individuals with stroke: a meta analysis. Clin Rehabil 2006;20:97-11.
- Veerbeek JM, Koolstra M, Ket JC, van Wegen EE, Kwakkel G. Effects of
augmented exercise therapy on outcome of gait and gait-related activities in
the first 6 months after stroke: a meta-analysis. Stroke 2011;42:3311-5.
- Harris JE, Eng JJ. Strength training improves
upper-limb function in individuals with stroke: a meta-analysis. Stroke 2010;41:136-40.
- Graven C, Brock K, Hill K, Joubert L. Are rehabilitation and/or care coordination interventions
delivered in the community effective in reducing depression, facilitating
participation and improving quality of life after stroke? Disabil
Rehabil 2011;33:1501-20.
- Quaney BM, Boyd LA, McDowd
JM, Zahner LH, He J, Mayo MS, Macko RF. Aerobic
exercise improves cognition and motor function post stroke. Neurorehabil
Neural Repair 2009;23:879-85.
- Zedlitz AM,
Rietveld TC, Geurts AC, Fasotti
L. Cognitive and graded activity training can alleviate persistent fatigue
after stroke: a randomized, controlled trial. Stroke 2012;43:1046-51.
- Gebruers N, Vanroy C, Truijen S, Engelborghs S, De Deyn PP. Monitoring of physical activity after stroke: a
systematic review of accelerometry based measures.
Arch Phys Med Rehabil 2010;91:288-97.
- Muren MA, Hütler
M, Hooper J. Functional capacity and health-related quality of life
in individuals post stroke. Top Stroke Rehabil 2008;15(1):51-8.
- Coutinho-Myrrha MA,
Dias RC, Fernandes AA, Araújo CG, Hlatky MA, Pereira DG et
al. Duke activity status index for cardiovascular
diseases: validation of the portuguese translation. Arq Bras Cardiol 2014;102(4):383-90.
- Polese JC, Sérvio TC,
Chaves GSS, Britto RR, Teixeira-Salmela LF. Relationships between self-reported and performance-based measures of
functional capacity in individuals with chronic stroke. J
Phys Ther Sci 2016;28(4):1208-12.
- Tavares LDA, Barreto
NJ, Jardim JR, Souza GMDC, Hlatky MA, Nascimento OA. Adaptação cultural e
avaliação da reprodutibilidade do Duke Activity Status Index para pacientes com
DPOC no Brasil. J Bras. Pneumol
2012;38(6):684-91.
- Bertolucci PH, Brucki SMD, Campacci SR, Juliano Y. Suggestions for utilization of the mini-mental
state examination in Brazil. Arq Neuropsiquiatr
1994;52:1-7.
- Flansbjer UB, Holmbäck AM, Downham D, Patten C,
Lexell J. Reliability of gait performance tests in
men and women with hemiparesis after stroke. J Rehabil
Med 2005;37(2):75-82.
- Hlatky MA, Boineau
RE, Higginbotham MB, Lee KL, Mark DB, Califf RM, et
al. A brief self-administered questionnaire to determine functional capacity
(the Duke Activity Status Index). Am J Cardiol 1989;64(10):651-4.
- Wenger NK, Mattson ME, Furberg CD, Elii J. Assessment of quality of life in clinical trials of
cardiovascular therapies. Am J Cardiol 1984;54:908-13.
- Souza AC, Magalhães
LC, Teixeira-Salmela LF. Cross-cultural adaptation and analysis of the psychometric properties in
the Brazilian version of the Human Activity Profile. Cad Saúde Pública
2006;22(12):2623-36.
- Davidson M, Morton N. A systematic review of the Human
Activity Profile. Clin Rehabil
2007;21(2):151-62.
- Teixeira-Salmela LF, Devaraj
R, Olney SJ. Validation of the human activity profile in stroke: A comparison
of observed, proxy, and self-reported scores. Disabi
& Rehabi 2007;29(19):1518-24.
- Fix A, Daughton D.
Human activity profile professional manual. Florida: Psychological Assessment
Resources. Odessa; 1988.
- Polese JC, Pinheiro
MB, Faria CD, Britto RR, Parreira VF, Teixeira-Salmela LF. Strength of the respiratory and lower limb muscles and
functional capacity in chronic stroke survivors with different physical
activity levels. Braz
J Phys Ther 2013;17(5):487-93.
- Gordon NF, Contractor A, Leighton RF. Resistance training for
hypertension and stroke patients. In: Graves JE, Franklin BA, eds. Resistance
Training for Health and Rehabilitation. Champaign, Ill: Human Kinetics; 2001;237-51.
- Macko RF, Smith GV, Dobrovolny CL,
Sorkin JD, Goldberg AP, Silver KH. Treadmill training improves fitness reserve
in chronic stroke patients. Arch Phys Med Rehabil
2001;82(7):879-84.
- Rimmer JH, Riley B, Creviston T, Nicola T. Exercise
training in a predominantly African-American group of stroke survivors. Med Sci Sports Exerc
2000;32(12):1990-6.
- Shepherd EF, Toloza E, McClung CD, Schmalzried TP. Step activity
- monitor: increased accuracy
in quantifying ambulatory activity. J Orthop Res 1999;17:703–8.
- Strath SJ, Kaminsky LA, Ainsworth BE, Ekelund U, Freedson PS, Gary RA
et al. Guide to the Assessment of Physical Activity: clinical and research
applications: a scientific statement from the American Heart Association.
Circulation 2013;128:2259-79.
- English C, Manns PJ, Tucak
C, Bernhardt J. Physical activity and sedentary behaviors in people with stroke
living in the community: a systematic review. Phys Ther 2014;94(2):185-96.
- Gordon NF, Gulanick M, Costa F, Fletcher G,
Franklin BA, Roth EJ et al. Physical Activity and Exercise Recommendations for Stroke
Survivors.
Circulation 2004;109:2031-41.