ARTIGO ORIGINAL
Functional gait assessment in patients with
relapsing-remitting Multiple Sclerosis and relation to the risk of falls
Avaliação funcional da marcha em pacientes
com esclerose múltipla recorrente-remitente e relação com o risco de quedas
Bruno Moraes*, Marco Orsini**, Rossano Fiorelli***, Victor Marinho****, Silmar
Teixeira****, Victor Hugo Bastos****, André Matta*
*Neurology Service, Federal Fluminense
University, University Hospital Antônio Pedro, Niterói/RJ, **Rehabilitation Science Program, Analysis of Human
Movement Laboratory, Augusto Motta University Center (UNISUAM), Rio de Janeiro,
Master's Program in Health Applied Sciences – USS, Vassouras,
Rio de Janeiro, ***Master's Program in Health Applied Sciences – USS, Vassouras, Rio de Janeiro, ****Brain Mapping and Plasticity
Laboratory, Federal University of Piauí (UFPI), Parnaíba/PI
Received 2017 June 29; accepted 2018 February 15.
Correspondence: André Matta, Neurology
Service, Federal Fluminense University, University Hospital Antônio Pedro, Niterói, Rio de Janeiro,
Brazil, E-mail: andrepcmatta@hotmail.com; Bruno
Moraes: brunofisio19@gmail.com; Marco Orsini:
orsinimarco@hotmail.com; Victor Marinho: victormarinhophb@hotmail.com; Silmar Teixeira: silmar_teixeira@yahoo.com.br; Victor Hugo
Bastos: victorhugobastos@ufpi.edu.br
Resumo
Objetivo: Demonstrar as
avaliações funcionais e sua correlação nos padrões de marcha de pacientes com
Esclerose Múltipla, utilizando um método não invasivo por meio do Timed Up and Go, teste de Tinetti, teste de caminhada de 25 pés e escala de Expanded Disability Status
Scale (EDSS). Métodos:
Foram avaliados 40 pacientes com Esclerose Múltipla, usando Timed
Up and Go,
teste de Tinetti, teste de caminhada de 25 pés e
escala de EDSS. Resultados: No
presente estudo, observamos correlações moderadas a altas entre EDSS e Timed Up and
Go, teste de Tinetti e teste
de caminhada de 25 pés (p < 0,0001). Os pacientes relataram tempos de
execução mais longos para os testes Timed Up and Go
e 25-Foot Walk
e menores escores no teste de Tinetti. Encontramos
uma correlação direta entre a duração da doença, a escala EDSS, o tempo de
execução Timed Up and Go, o tempo de execução de
25-Foot Walk e o escore do teste de Tinetti (p < 0,0001). Conclusão: avaliações adequadas de risco de marcha e queda são
importantes para evitar complicações relacionadas à Esclerose Múltipla.
Palavras-chave: esclerose múltipla,
avaliação da marcha, EDSS, risco de quedas.
Abstract
Objective: To
demonstrate correlation functional evaluations of gait on the patients with
Multiple sclerosis, using a noninvasive method by means of Timed Up and Go, Tinetti test, 25-Foot Walk test and Expanded Disability
Status Scale (EDSS). Methods: We evaluated
40 patients with Multiple sclerosis using Timed Up and Go, Tinetti
test, 25-Foot Walk test and EDSS scale. Results:
In present study, we have observed moderate to high correlations between EDSS
and Timed Up and Go, Tinetti test and 25-Foot Walk test
(p<0.0001). The patients reported longer execution times for Timed Up and Go
and 25-Foot Walk tests and lower scores on the Tinetti test. We found a direct correlation between illness
duration, EDSS scale, Timed Up and Go execution time, 25-Foot Walk execution
time and Tinetti test score (p<0.0001). Conclusion: Proper gait and fall risk
evaluations are important in order to avoid complications that are related to
Multiple sclerosis.
Key-words: multiple
sclerosis, gait evaluation, EDSS, risk of falls.
Introduction
Multiple Sclerosis (MS) is a chronic immune disease of the central
nervous system, in which an inflammatory and degenerative process of white and
gray matter occurs [1]. MS is one of the most common neurological diseases
affecting gait in young adults, with approximately 2.3 million people globally
living with some form of MS. It is a degenerative condition of the central
nervous system in which inflammation causes demyelination, disrupting
neurological conduction [2].
The impact of MS varies widely, ranging from mild to severely disabling
as the disease progresses. It has several clinical manifestations including,
but not limited to, sensory disturbance, weakness, ataxia, muscle spasticity,
and cognitive difficulties [3]. Different sub-types of the condition
significantly increase the variety and timing of symptoms in a condition that
is already extremely diverse in its effect on each individual. Of note, MS is a
chronic, lifelong condition, and most people who are diagnosed with MS are 20
to 40 years old [2,4]. Among disabilities, gait
disorders are the most frequent since proprioceptive, pyramidal tracts and the
cerebellum are frequently affected [5]. During gait patterns, various aspects
can be affected, for example, the speed, the length of the step, the maximum
distance, the quality of the movements and the ability to maintain balance
[5-8].
The motor skills involvement, especially gait disturbances, are relevant
in studies involving MS patients since walking is a domain of fundamental
neurobiological and muscular association for life. In view of the above, MS may
cause deficiencies in mobility tasks [9]. In addition, Kelleher et al. [3] demonstrate that gait
impairment is the main target, which becomes a priority in studies that target
rehabilitation in people diagnosed with MS since 85% of study participants
reported gait changes as their main complaint. The impairment in sensory
function and mobility is a frequent and disabling consequence of MS that may
lead to greater deficits [10], for instance, muscular atrophy and increased
risk of falls traumas [9,11]. Thus, the balance-gait relationship through
functional evaluations of Tinetti test (TT), Time Up
and Go (TUG) test and Timed 25-Foot Walk (T25FW) are
frequently used as indicators of the motor incapacity progression [12]. A
cross-sectional study corroborates that gait speed acts as a spatiotemporal
measure of greater sensitivity to disease severity [10,12,13].
Inevitably, interventions for MS include drug therapy as well as the
joint action of rehabilitation activities and constant assessment through
walking domain scales [14,15]. Therefore, we used TT,
TUG, T25FW and EDSS scale in order to evaluate and direct the therapeutic
protocol for MS patients. However, a complementation is necessary, with
diagnosis based on a thorough medical history associated with clinical and
laboratory examination [16]. According to clinical evolution, MS has specific
classifications: remitting-relapsing (MS-RR), primary progressive (MS-PP),
primary progressive with episode (MS-PP with episode) and secondary progressive
(MS-SP) [4,17]. The most common classification is
MS-RR, accounting for 85% of all newly diagnosed cases. MS-SP form is a natural
evolution of the first one. In approximately 50% of cases, after 10 years of
the initial form diagnosis (MS-RR) a conversion to the MS-SP form happens [18].
As for MS-PP and MS-PP with the episode, they add up to 10%-15% in all cases
[16]. Accordingly, the present study examined the relation between the TT, TUG,
T25FW and EDSS scale as a cognitive behavior evaluation and gait performance,
of the few non-pharmaceutical therapies that maintain or improve the ability to
walk and size the potential risk of falls in MS patients [19].
Material and methods
Participants
Transversal study with MS-RR patients attended at Hospital Antônio Pedro of Fluminense
Federal University (HUAP/UFF), Rio de Janeiro, between May 2013 and July 2015.
The present study evaluated 40 patients with MS-RR (11 men and 29 women,
average age = 41.5 ± 11.0 years). We selected participants aged over 18 years,
with a diagnosis of MS-RR, Expanded Disability Status
Scale (EDSS) lower than 6.5. Exclusion criteria were comorbid conditions that
could cause changes in the tests such as orthopedic (arthrosis,
ligament injuries), rheumatological (rheumatoid
arthritis), cardiological (heart failure) and
neurological diseases (i.e., Parkinson's disease). Additionally, recent
episodes (last three months), cognitive deficit preventing the understanding of
tests and people’s refusal to sign an FPIC were used as exclusion criteria.
Finally, all subjects signed the Free and Informed Consent Form. This study
research project was submitted to the Ethics Committee of the Medical School of
the Fluminense Federal University, approved under the
registration no. 12300413.2.0000.5243.
Experimental procedure
Functional Activity Evaluation: Two neurologists evaluated the
neurological involvement by the EDSS scale, as well as three tests that evaluate
patients functionality: TT, TUG and T25FW [19,20]. We
instructed all patients to avoid any activity that could cause muscle fatigue,
for instance, long walks or stairs in which the energy expenditure is higher
[21]. In order to complement the results about the functional disability of
patients, the results were classified by using EDSS [22], whose score refers to
the functions involvement. The scale ranges from 0 to 10 [20].
TT has been used to evaluate balance and gait abnormalities. A score above
24 points means low fall risk, between 19 and 24 points means moderate risk and
lower than 19 points means low risk. The maximum score is 28 points [20].
T25FW is a quantitative measure of lower extremity function described by
Fischer et al. [23]. The time required to walk 25 feet was measured to evaluate
the functional activity of the patients. The reliability of this test has
previously been confirmed. The test was repeated three times, with 5-minute
rest intervals to prevent fatigue. The time required to complete the test was
measured using a standard chronometer, and the lowest time was considered [20,24].
TUG Test is a valid and reliable test to evaluate functional activity in
patients with MS and is based on the time required to complete a complex
activity. Validity and test-to-test reliability have been proved in previous
studies. The procedure is as follows: the patient must get up from a sitting
position in a standard chair, advance for 3 m, return to the chair, and sit
down again. The test was repeated three times, with 5-minute rest intervals to
prevent fatigue. The time required to complete the test was measured using a
standard chronometer, and the lowest time was considered [25].
Statistical analysis
We described the variables using means (standard deviation [SD]) for
continuous variables. We use Pearson’s Correlation for calculate to detect the
relationship between the TT, TUG, T25FW and EDSS variables, and with the
objective of relating to risk of falls. We used the descriptive statistics in
tables to show contingency, calculation of averages, standard deviations and
results of the group. Statistical significance was considered in the case of
p<0.05. All analyses were performed with the SPSS software for Windows version
320 20.0.
Results
The results of the EDSS showed scores between 0 and 6.5 with an average
of 3.02 ± 2.16 for patients with MS. In view of this question, with the
statistical analysis already mentioned, variables of TT, TUG and T25FW test
were correlated. All tests are correlated with each other and with moderate to
strong relationships (p<0.001) (Table I). Only the TT relationship with all
others is inversely proportional, that is, the greater the TT score, the
shorter the TUG and T25FW execution times will be. In addition, as for the
relationship between TUG and T25FW it is directly proportional, the greater the
value of TUG, the greater the value of T25FW. In summary, correlation of EDSS
was also calculated with other tests and it showed that TUG, T25FW. In addition,
T25FW replication has significant positive relationship with EDSS; in the case
of TT, the correlation is negative (Table I).
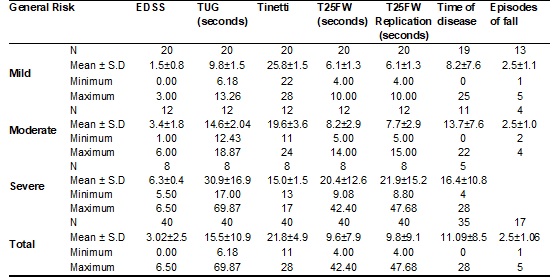
With the final data about functional activity evaluation, we calculated
the average of the result of TT, TUG and T25FW (table II). For each patient,
risk types were assigned based on TUG and another on TT. The total average of
these test were referred to as general fall risks (Table III). EDSS and T25FW
averages for each type of risk were also included. The risks were classified as
mild, moderate and severe (Table III).
Table I – Pearson’s Correlation for detect the
relation between the TUG test, TT, T25FW and EDSS variables.
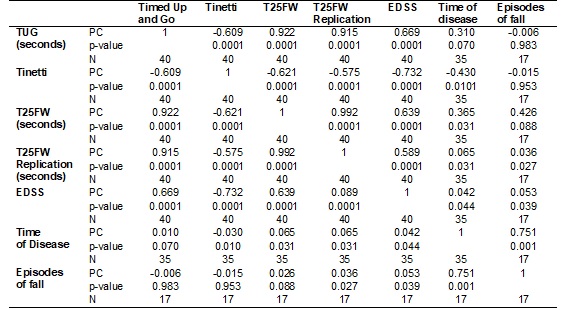
PC
= Pearson’s Correlation
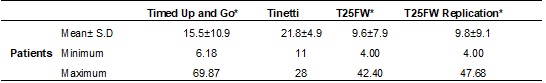
Table III – Mean data with Risk analysis of fall in MS
patients.
Discussion
This study include a sample of patients with Multiple Sclerosis
remitting-relapsing to examine the relationship of neurological involvement by
the EDSS scale, as well as three tests that evaluate patients’ functionality:
TT, TGU, T25FW with changes in gait and association with the risk of falls. The
results will be discussed on the basis of this paradigm.
Overall, our findings show that quantitative measures by the TT, TGU and
25FW detect specific deficiencies in MS patients, and these relate to global
measures of disability and ambulation. The functional measures analysis has
shown a decline in the strength of muscle control during gait, which may be
associated with the increase in fatigue that is more frequent in patients with
multiple sclerosis remitting-relapsing. The mean scores for the TT, TGU, T25FW
and EDSS scale suggest a greater tendency for changes in light sensory
perception embedded in motor skills [19,26,27]. Thus,
it is essential to emphasize that the Report of the Quality Standards
Subcommittee of the American Academy of Neurology establishes a level of
recommendation for all patients in a neurological doctor’s office with risk
factors identified as gait and balance disorders, the use of walking
assistance, weakness of limbs, or sensory loss. The report recommends that
patients with these risk factors are evaluated for fall risk.
Accordingly, altered gait is a major problem for many MS individuals
because it limits their participation in regular activities, decreases their
ability to participate in physical exercise, and increases the episode of falls
and injuries [6,28,29]. Interestingly, our variables
correlated with the EDSS cognitive ability test demonstrate limited mobility as
well as the overall health impact of MS patients. Therefore,
being identified as the main determining factor for physical and social
limitations [10]. Through this study, it was possible to analyze several
secondary variables as the relation between the number of episodes, the illness
duration and the age of patients with risk. It was found thereby that the
illness duration is at the limit of significance, giving the impression the
greater the illness duration, the greater the execution time in TT, TGU and
T25FW. This shows that even “stable” patients, i.e. no new lesions on MRI,
suffer functional decline regardless.
The factors TT, TGU, T25FW and EDSS scale were correlated,
traditionally accurate measures to determine the distance covered over a period
of time through protocols standardized [15]. It acts as evaluative anchors of
gait domain, a possible means of rehabilitation, as well as measuring potential
risks of falls for patients. Several studies were used to evaluate the
prediction failure. In one of them, Mazumder et al. [30] reported on fall prediction,
which evaluated 54 patients with EDSS scores of 6 or lower. It used the Twelve
Item MS Walking Scale (MSWS-12), T25FW, computerized balance assessment and the
fall FES-1 questionnaire as a methodology. The results showed thirty-seven
(71%) individuals fell at least once in the six-month period according to
FES-1. AUC measurement, a statistical method of summary information of a series
of measures in individuals, was used to predict falls in the following 6
months. In this evaluation model, the methods are potentially accurate, since
the evaluations are supported in statistical norms from diverse clinical and
physiological data of the patient [2,5,6]. In
exemplification of the questioning, despite the natural variability among the
patients, the gait may be a personal trait rather than an impact of the fatigue
induced by the neurological disease. Therefore, changes in gait characteristics
over a given period of time may be measured by the joint action of the TT, TGU
and T25FW, in order to draw clinical conclusions and remove the variability
between subjects.
We similarly report that mobility limitations measured by the
performance of TT, TGU and T25FW correspond to changes in employment and
functional independence, and propose that MS individuals are more likely to be
functionally impaired. The results assume that mobility deficits correspond to
changes in functional gait use and MS progression related disability. Comparing
the parameters of TT, TGU and T25FW, we observed significant differences when
correlating the major gait effects and cognition-related.
In relation to the previous questions, we interpret this as connection
deficiencies in the neuronal inputs of sensorimotor integration promoted by the
neurological disease, since they have a greater impact on the patient daily
life. The results show that MS patients showed scores related to decreased
motor control and had a high variation of gait cycle length in the tests. It is
also observed that the EDSS components of the cognitive evaluation scale
related to the functional evaluation tests corroborate with the literature that
the cognitive domain has a relation with the sensorimotor integration level in
gait activity. In view of this, it is important that rehabilitation therapists
understand the nature of gait dysfunction in MS people and the effect of
interventions that target gait symptoms. In short, cognitive behavior
assessment and gait performance favor physical rehabilitation, which is one of
the few non-pharmaceutical therapies to maintain or improve the ability to walk
and size the potential risk of falls in MS patients [20,24,25].
Study limitations
Despite the finding of correlations between the gait evaluation tests,
the cognitive decline test and the risk of falls episode, the present study has
some limitations. At first, the results come from a small sample of
convenience. Second, the study design did not include a corresponding control
group to consider the extent of these results beyond the current sample.
Another point is that the risk of falls was measured in a population in which
memory deficits are common since it requires caution in interpreting the results.
However, it is important to note that our findings provide some support that
leads to the understanding of the cognitive decline relation and gait changes
as possible markers of falls episodes in patients with neurological diseases.
Conclusion
Tests and functional evaluations of lower limbs were able to trace
possible fall risk and/or gait disorder. Thus, it was possible not only to
correlate test variables with EDSS with fall risk, but also compare TT, TGU and
T25FW in patients with MS. The study observations suggest that a decrease in
walking resistance, in addition to being associated with a higher risk of
falls. Our findings, although with some limitations, support the monitoring of
future falls in MS patients. In this context, future research is needed to
understand the consistency of fall risk factors across the disability spectrum
in MS patients, and thus to determine a model of interventions designed to
reduce and prevent falls. In summary, we highlight that these tests are fast, easy
to perform, low cost and present high sensitivity which helps optimize
outpatient care.
References
- Bethoux F. Gait disorders in
multiple sclerosis. Continuum (Minneap Minn) 2013;19:1007-22.
- Behm K, Morgan P. The effect of
symptom-controlling medication on gait outcomes in people with multiple
sclerosis: a systematic review. Disabil Rehabil 2017;4:1-12.
- Kelleher KJ, Spence W, Solomonidis S et al. The characterization of gait patterns of people with multiple
sclerosis. Disabil Rehabil
2010; 32:1242-50.
- Lublin FD, Reingold SC, Cohen JA, Cutter GR, Sørensen PS, Thompson AJ et al. Defining the clinical
course of multiple sclerosis: the 2013 revisions. Neurology 2014;83:278-86.
- Monticone M, Ambrosini E, Fiorentini R, Rocca B, Liquori V, Pedrocchi A, Ferrante S.
Reliability of spatial-temporal gait parameters during dual-task interference
in people with multiple sclerosis. A cross-sectional study.
Gait Posture 2014;40:715-8.
- Sosnoff J, Molt R, Morrison
S.: Multiple sclerosis and falls - an evolving tale: US Neurology 2013;
9(1):30-4
- Bethoux F, Bennett S.
Evaluating walking in patients with multiple sclerosis. which
assessment tools are useful in clinical practice? Int
J MS Care 2011;13:4-14.
- Kalron A, Dvir
Z, Achiron A. Walking while talking-Difficulties
incurred during the initial stages of multiple sclerosis disease process. Gait
Posture 2010;32:332-5.
- Galea MP, Cofré Lizama
LE, Butzkueven H, Kilpatrick TJ. Gait and balance deterioration over a 12-month period in multiple
sclerosis patients with EDSS scores ≤ 3.0. NeuroRehabilitation
2017;40(2):277-84.
- Newsome SD, Wang JI, Kang JY, Calabresi PA, Zackowski KM. Quantitative measures detect sensory and
motor impairments in multiple sclerosis. J Neurol Sci 2011;305:103-11.
- Gunn H, Creanor S, Haas B, Marsden J, Freeman
J. Frequency, characteristics, and consequences of falls in multiple sclerosis:
findings from a cohort study. Arch Phys Med Rehabil 2014;95(3):538-45.
- Fritz NE, Jiang A, Keller J, Zackowski KM.
Utility of the six-spot step test as a measure of walking performance in
ambulatory individuals with multiple sclerosis. Arch Phys Med Rehabil
2016;97(4):507-12.
- Lizrova Preiningerova
J, Novotna K, Rusz J, Sucha L, Ruzicka E, Havrdova E. Spatial and temporal characteristics of gait as
outcome measures in multiple sclerosis (EDSS 0 to 6.5). J Neuroeng
Rehabil 2015;12:14.
- Döring A, Pfueller
CF, Paul F, Dörr J. Exercise in multiple sclerosis –
an integral component of disease management. EPMA J 2011;24;3(1):2.
- Yamout B, Alroughani
R, Al-Jumah M, et al. Consensus guidelines for the
diagnosis and treatment of multiple sclerosis. Curr
Med Res Opin 2013; 29:611-21.
- Polman CH, Reingold
SC, Banwell B, Clanet M,
Cohen JA, Filippi M et al. Diagnostic criteria for
multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol 2011;69(2):292-302.
- NeamŢu MC, NeamŢu OM, Marin MI, Enescu Bieru D, Rusu L. Prediction of
motor disorders in multiple sclerosis using muscle change structure assessment.
Rom J Morphol Embryol 2016;57(4):1331-5.
- Dujmovic I, Radovanovic S, Martinovic V, Dackovic J, Maric G, Mesaros S, Pekmezovic T, Kostic V, Drulovic J. Gait
pattern in patients with different multiple sclerosis phenotypes. Mult Scler Relat
Disord 2017;13:13-20.
- Samaei A, Bakhtiary
AH, Hajihasani A, Fatemi E,
Motaharinezhad F. Uphill and downhill walking in
multiple sclerosis: a randomized controlled trial. Int
J MS Care 2016;18(1):34-41.
- Goldman MD, Motl RW, Scagnelli
J, Pula JH, Sosnoff JJ, Cadavid D. Clinically meaningful performance benchmarks in
MS: timed 25-foot walk and the real world. Neurology 2013; 81(21):1856-63.
- Kiesseier B, Pozzilli C. Assessing walking disability in multiple
sclerosis. Mult Scler 2012;18:914-24.
- Kurtzke JF. Rating
neurologic impairment in multiple sclerosis: an expanded disability status
scale (EDSS). Neurology 1983;33(11):1444-52.
- Fischer JS, Jak AJ, Kniker
JE, Rudick RA. Administration and
scoring manual for the National Multiple Sclerosis Society; 2001.
- Learmonth YC, Paul L, McFadyen AK, Mattison P, Miller
L. Reliability and clinical significance of mobility and balance assessments in
multiple sclerosis. Int J Rehabil
Res 2012;35:69-74.
- Coote S, Gallagher S, Msetfi R, Larkin A, Newell J, Motl RW, Hayes S. A randomised
controlled trial of an exercise plus behaviour change
intervention in people with multiple sclerosis: the step it up study protocol.
BMC Neurol 2014;14:241.
- Shahraki M, Sohrabi M, Taheri Torbati HR, Nikkhah K, NaeimiKia M. Effect of rhythmic auditory stimulation on
gait kinematic parameters of patients with multiple sclerosis. J Med Life 2017;10(1):33-7.
- Nilsagård Y, Westerdahl E, Wittrin A, Gunnarsson M. Walking distance as a predictor of falls in
people with multiple sclerosis. Physiother Res Int 2016;21(2):102-8.
- Fjeldstad C, Pardo G. Immediate effect of a service dog on walking speed
in individuals with multiple sclerosis and gait dysfunction: a pilot study. Int J MS Care 2017;19(1):40-1.
- Zwibel HL. Contribution
of impaired mobility and general symptoms to the burden of multiple sclerosis.
AdvTher 2009;26:1043-57
- Mazumder R, Lambert WE, Nguyen T, Burdette DN, Cameron MH. Fear of falling is associated with recurrent falls in people with
multiple sclerosis: a longitudinal cohort study. Int J MS Care 2015;17(4):164-70. doi: 10.7224/1537-2073.2014-042.