ORIGINAL ARTICLE
Effect of early intervention in an interdisciplinary
group of children with Down syndrome in a special integration center
Efeito da estimulação precoce em grupo
interdisciplinar de crianças com síndrome de Down em um centro de integração
especial
Renata Pianezzola de
Oliveira*, Daniela Azambuja Ilha**, Carolina Maria Mugnol**, Rejane
Terezinha Gonçalves Conceição***, Sílvia Bitencourt****, Viviane da Silva
Machado*****, Laís Rodrigues Gerzson******, Carla Skilhan de
Almeida, D.Sc.*******
*Fisioterapeuta,
Universidade Federal do Rio Grande do Sul (UFRGS), Porto Alegre/RS,
**Fisioterapeuta, Kinder - Centro de Integração da Criança Especial,
Porto Alegre/RS, ***Fonoaudióloga, Kinder - Centro de Integração da
Criança Especial, Porto Alegre/RS, ****Psicóloga, Kinder - Centro de
Integração da Criança Especial, Porto Alegre/RS, *****Terapeuta
Ocupacional, Kinder - Centro de Integração da Criança Especial,
Porto Alegre/RS, ******Fisioterapeuta, Doutoranda do Programa de Pós
graduação Saúde da Criança e do Adolescente da Universidade Federal do Rio
Grande do Sul (UFRGS), Porto Alegre/RS, *******Fisioterapeuta, Docente do Curso
de Fisioterapia da Universidade Federal do Rio Grande do Sul (UFRGS),
Porto Alegre/RS
Received: April 20,
2018; Approved: August 9, 2018.
Corresponding
author:
Carla Skilhan de Almeida, Rua Felizardo, 750 Jardim Botânico 90690-200 Porto
Alegre RS, E-mail: carlaskilhan@gmail.com; Renata Pianezzola de Oliveira:
pianezzola.re@gmail.com; Daniela Azambuja Ilha: reabilitação@kinder.org.br;
Carolina Maria Mugnol: carolinamugnol@yahoo.com.br; Rejane Terezinha Gonçalves
Conceição: rejanifono@hotmail.com; Sílvia Bitencourt:
bitencourtsilvia@hotmail.com; Viviane da Silva Machado: vivica2608@gmail.com;
Laís Rodrigues Gerzson: gerzson.lais@yahoo.com.br
Abstract
Objective: To verify the
effects of early stimulation on the motor and cognitive development of children
with Down syndrome taking part of an interdisciplinary early stimulation group at
a Special Child Integration Center. Methods:
Prospective Observational Study carried out at a Special Child Integration Center
with children from 0 to less than 1 year of age, taking part of an early stimulation
group and who were not participating in any other intervention. Children included
were evaluated in the rehabilitation sector of the institution. The instrument used
was the Child Behavior Development Scale and the data were presented descriptively
with percentage based on the answers of individual behavior and on the group average
pre- and post-intervention. Results: The
group was homogeneous regarding the characteristics and possible factors associated
to developmental delay. In the motor and cognitive performance, individually all
children had an improvement on their performance equal or greater than 50% in comparison
to the initial assessment, and the group had a 62.5% growth in comparison to the
initial evaluation. Conclusion: In group
early stimulation brings benefits on the motor and cognitive development of children
with Down syndrome in interdisciplinary care.
Key-words: early stimulation,
child development, Down syndrome.
Resumo
Objetivo: Verificar os efeitos
da estimulação precoce sobre o desenvolvimento motor e cognitivo de crianças com
síndrome de Down que participam do grupo interdisciplinar de estimulação precoce
oferecido em um Centro de Integração da Criança Especial. Métodos: Estudo observacional prospectivo. Foi realizado em um Centro
de Integração da Criança Especial com crianças de zero a um ano incompleto, que
estivessem participando do grupo de estimulação precoce e que não participassem
anteriormente de outra intervenção. As crianças incluídas foram avaliadas no setor
de reabilitação da instituição. O instrumento utilizado foi a Escala do Desenvolvimento
do Comportamento da Criança e os dados foram apresentados de forma descritiva com
percentual baseado nas respostas do comportamento individual e da média do grupo
pré e pós-intervenção. Resultados: O grupo foi homogêneo em relação às características e possíveis
fatores associados ao atraso do desenvolvimento. No desempenho motor e cognitivo,
individualmente todas as crianças obtiveram um crescimento em seu desempenho igual
ou superior a 50% comparado com a avaliação inicial e o grupo obteve crescimento
de 62,5% comparado com a avaliação inicial. Conclusão:
A estimulação precoce em grupo traz benefícios sobre o desenvolvimento motor e cognitivo
de crianças com síndrome de Down em atendimento interdisciplinar.
Palavras-chave: estimulação precoce,
desenvolvimento infantil, síndrome de Down.
Introduction
Early childhood, from birth to three years of age, is marked by an accelerated
growth rate [1]. Infant motor development is characterized by the child’s motor
acquisitions, from the simpler to the more complex, which allow a wide and precise
succession of movements and interaction with her/his environment [1,2]. Such changes
are intrinsically related to the interactions within the subject and also interactions
between the subject, the environment and the proposed task [2]. In this period,
movement is extremely important for the child’s cognitive development, and such
experiences offered to the child can positively influence the development of his/her
motor skills [3].
However, there are many factors which can compromise child development, such
as biological risks – which affect prenatal development and usually are associated
with gestation and birth conditions; environmental risks – which include the aspects
related to deficient family structure and inadequate stimulation [3]. Other factors,
such as prematurity and low birthweight and inborn errors
of metabolism are also found in the literature as being responsible for a higher
risk for deficits in neuropsychomotor development. Thus,
the child can present learning difficulties, problems with language, social interaction
and motor coordination [4,5]. Down syndrome (DS), a genetic
condition with specific physical and mental characteristics, also leads to neuropsychomotor developmental delay. In the realm of motor
activities, children with DS reach basic motor milestones at slower times than children
with normal development and, from the cognitive point of view,
the language area is highly compromised [6].
Given the importance and impact of developmental delay, early identification
of infants at risk is vital to minimize the consequent effects [7]. Each child has
her/his own characteristics, that is, s/he is an individualized being, and genetic
and environmental factors influence her/his neuropsychomotor
development. Therefore, the treatment shall consider the individuality of each child,
as well as the familiar context in which s/he is inserted [8]. The main goal of
the Physical Therapy intervention is to stimulate motor development, in association
with the acts initiated by the child herself/himself, encompassing her/his neuropsychomotor aspects and the context in which s/he lives
[8].
In light of such reality, the Early Intervention Program (EIP) exists as
part of the special education realm and targets children with special needs from
birth to three years of age [9]. The EIP consists of a set of encouraging activities
designed to provide the child with meaningful experiences, aiming at reaching the
full development of her/his evolutionary process [10]. The EIP also consists of
planning specific psychomotor activities, respecting the age group and encouraging
the child to interact in the environment without threating her/his freedom of expression
[11]. Thus, it is important to stress that the EIP’s role is not to make the child
a typical one, but to make up for the deficiencies and their effects [10]. With
that, the EIP’s main goal has been to minimize, remedy or prevent, through actions,
the adverse effects of the development of children with disabilities [9].
The human being is an integral individual that requires a care which understands
her/his integrality, which meets her/his biopsychosocial
needs. Thus, interdisciplinarity is fundamental because
it allows for a new configuration of health knowledge and a new way to provide health
[12]. Therefore, health is viewed as interdisciplinary, so, health professionals
need to be ready and committed to the reality of health. In addition to that, they
must be willing to share their knowledge to attain a common goal [13].
Hence, the objective of this study was to determine the effects of early
intervention on the motor and cognitive development of children with Down syndrome
who participated in an early intervention interdisciplinary group offered at a Special
Child Integration Center.
Methods
Sample
This study had a quasi-experimental design and was devised according to the
guidelines and regulatory norms for research involving human beings, presented to
the Ethics and Research Committee and approved under No. 1.009.551, with the participation
of 6 children of the Early Intervention Program First Steps at Kinder - Special
Child Integration Center. The sample was intentional, with infants between 4 and
7 months of age. All children who participated in the study met the following inclusion
criteria: 1) were under one year of age; 2) did not participate in any other intervention.
The parents/guardians of each child were previously informed about the collection
procedures and signed a Free and Clarified Consent Term (FCCT).
Instruments
The children included in the study were assessed in the rehabilitation sector
at Kinder - Special Child Integration Center, located in Porto Alegre, the capital of the State of Rio Grande do Sul. Each participant was assessed by the same trained researcher,
who used the Child Behavior Development Scale in the First Year of Life [14]. The
collection happened in two moments and was carried out with the presence of the
person responsible for the child in a room with a tatami and the materials composing
the assessment kit. Thus, the first assessment happened at the beginning of the
program and, the second one, four months later.
This scale allows the assessment of an infant’s development in 64 behaviors
distributed month to month and in different age groups. This scale presents motor,
cognitive and social behaviors, which can be axial or appendicular; stimulated or
spontaneous; communicative or non-communicative. The axial motor behavior was designated
as motor organization related to posture, equilibrium and movement and sound emission;
the appendicular motor behavior was designated as organization in skills and dexterity,
encompassing manual, hearing and visuomotor coordination.
The classification of stimulated or spontaneous motor behavior was associated
to a specific stimulation, such as sounds and verbal communication, or a non-specific
one, triggered by the child’s position and environmental stimuli; such classifications
indicated the motor behavior.
As for the communicative or non-communicative, exteriorization in relation
to the child’s interaction with other people was observed, indicating the activity
behavior. Hence, the instrument was divided into eight subscales: Axial Spontaneous
Non-Communicative (fifteen activities of movement and posture); Axial Spontaneous
Communicative (eight activities of sound emission and repetition); Axial Stimulated
Communicative (five activities of body games and interaction with the examiner);
Appendicular Spontaneous Non-Communicative (eleven activities of perceiving and
manually exploring objects); Appendicular Spontaneous Communicative (one activity
of interaction with the researcher); Appendicular Stimulated Non-Communicative (eight
activities of handling and recognition of object function) and Appendicular Stimulated
Communicative (nine activities of task completion on request) [15].
Procedures
The interventions took place once a week with the presence of a family member/responsible
for the child during four months, according to the proposal offered by the institution,
with each session lasting one hour and twenty minutes. The Early Intervention Program
First Steps proposes group sessions with an interdisciplinary intervention model.
The professionals who work in that institution and are part of the program involve
a physical therapist, a psychologist, a speech therapist and an occupational therapist.
The professionals work in pairs, with physical therapy being matched with psychology
and occupational therapy with speech therapy, alternating their actions in the groups
fortnightly. The physical therapist guides the child’s proper positioning at home
and explains the stages of development; teaches movements to facilitate postural
changes and improve postural control (head and trunk); makes referrals, performs
exams and requests lower limbs orthoses. The psychologist
stimulates mother-infant bond, interaction among children, child’s acceptance, and
interaction and integration of the families; establishes group routines and gives
attention to the necessities of each family and helps build up a support network
for the families.
The speech therapist guides the positioning when eating, watches out for
food consistency, daily utensils and oral hygiene, makes exercises to facilitate
eating and communication; stimulates language – comprehension and speaking – and
observes hearing alteration and/or loss. The occupational therapist guides the positioning
to facilitate the use of the upper limbs to play, eat and do other daily activities;
indicates the adequate toy for each age group, helps with clothing, shower and makes
visual stimulation; requests furniture to keep the sitting position and hand orthoses; adapts utensils – cutlery, pencil, baby bottle, wheelchair
– and provides the infants with sensory and motor experiences to stimulate functionality.
The program aims at providing the families, in addition to the stimulation of their
children, with a moment of exchange of experiences, stories, fears and hopes, bringing
them closer and creating a support network for them.
At the end of this period, a reassessment was scheduled to carry out a new
collection, just like the first assessment.
Data analysis
Motor and cognitive development was assessed through the Child Behavior Development
Scale and the data are presented descriptively with percentage based on the responses
of the individual behavior and the group average pre- and post-intervention. To
that, a score from one to five was given to classify the child: with delay, at risk,
regular, good and excellent, respectively.
Results
Six children with Down syndrome participated in the study, being two boys
and four girls, with ages between four and seven months (the mean age was 5.67 months).
Only one child was born preterm (gestational age ≥ 36 weeks) and with low
birthweight (≥ 2.500g). However, for the assessment,
her/his age was corrected. In relation to the Apgar score, none of the infants had
a score lower than 7 in the fifth minute, and no operative vaginal delivery was
performed, therefore, all babies were delivered either vaginally or by C-section.
As for the parents’ educational attainment, all of them had high school or a degree.
In terms of housing conditions, all children lived in proper places with water and
power supplies and sanitation. All children were accompanied by their mothers during
the intervention period (Table I).
Table I - Characteristics and possible factors associated
with developmental delay.
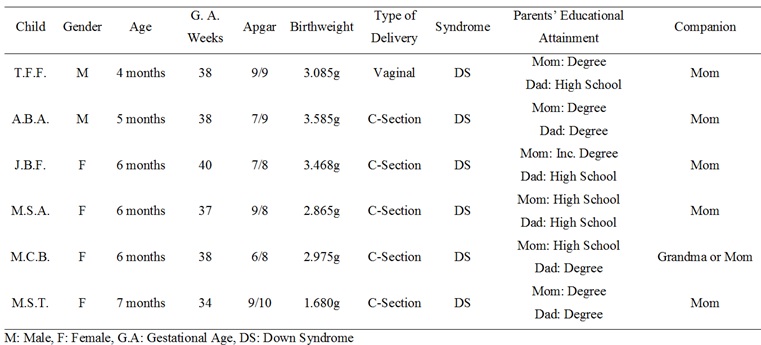
Figure 1 displays pre- and post-intervention results distributed into eight
subscales. The data indicate that participant A.B.A boosted his performance in five
out of eight subscales (62.5%), improving on the items related to posture and movement;
auditory reaction and visual sensitivity; body games and interaction with the examiner;
perception and manual exploration of objects; handling and recognition of object
function. As for the sound emission and repetition activities; interaction with
other people and task completion on request, it was noted that the child kept the
same classification pre- and post-intervention.
The participant T.F.F. boosted his performance in five out of eight subscales
(62.5%), improving on the items related to sound emission and repetition; auditory
reaction and visual sensitivity; body games and interaction with the examiner; perception
and manual exploration of objects; handling and recognition of object function.
He kept the same classification in the activities related to movement and posture;
interaction with other people and task completion on request.
The participant J.B.F. boosted her performance in four out of eight subscales
(50%), improving on the items related to posture and movement; auditory reaction
and visual sensitivity; body games and interaction with the examiner; perception
and manual exploration of objects, while keeping the classification in sound emission
and repetition; interaction with other people; handling and recognition of object
function and task completion on request.
The participant M.S.A. boosted her performance in five out of eight subscales
(62.5%), improving on the items related to posture and movement; auditory reaction
and visual sensitivity; body games and interaction with the examiner; interaction
with other people and handling and recognition of object function, while keeping
the same classification in the activities related to sound emission and repetition
and having a decrease in perception and manual exploration of objects and task completion
on request.
The participant M.C.B. boosted her performance in four out of eight subscales
(50%), improving on the items related to auditory reaction and visual sensitivity;
body games and interaction with the examiner; perception and manual exploration
of objects and handling and recognition of object function, while keeping the same
classification in the activities related to posture and movement; sound emission
and repetition; interaction with other people and task completion on request.
The participant M.S.T. boosted her performance in five out of eight subscales
(62.5%), improving on the items related to posture and movement; sound emission
and repetition; auditory reaction and visual sensitivity; body games and interaction
with the examiner; and perception and manual exploration of objects, while keeping
the same classification in the activities involving interaction with other people
and task completion on request and having a decrease in the activities related to
handling and recognition of object function.
As for the group, the results suggest that the post-intervention performance
has significantly progressed in comparison to the initial period in five out of
eight subscales (62.5%) in the activities related to posture and movement; auditory
reaction and visual sensitivity; body games and interaction with the examiner; perception
and manual exploration of objects; and handling and recognition of object function.
The group did not get any increase or decrease in the activities related to sound
emission and repetition; interaction with other people and task completion on request.
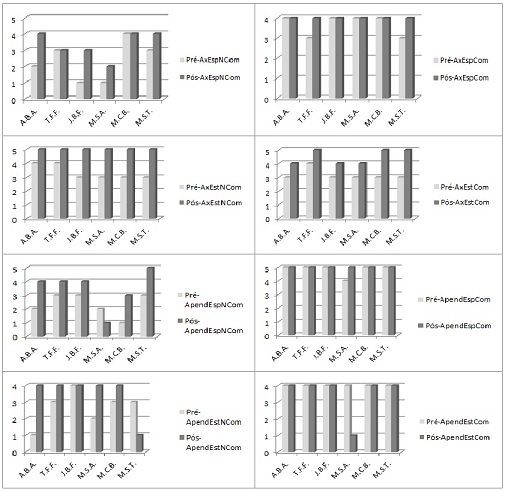
Figure 1 – Pre- and post-intervention assessment results.
Discussion
The results are favorable concerning physical environment and family structure,
because virtually all children came from structured families who had good housing
conditions. Studies point to peculiar issues related to the physical structure of
the house and the external environment in which the child is inserted as factors
which can help or harm her/his development, as well as the interpersonal relations
and the roles played by the family members [16]. Low-stimuli environments can negatively
interfere, that is, the place in which the baby lives offers different formats or
shapes aspects of her/his behavior [17]. Thus, the context in which the child is
inserted, including social interactions and family environment, influences either
positively or negatively both skill acquisition and functional independence [1,3,17,18].
This study wanted to determine the effects of early intervention on the motor
and cognitive development of children with Down syndrome who currently participate
in an early intervention interdisciplinary group offered at a Special Child Integration
Center. Studies provide evidence on the characteristics of the motor and cognitive
development of children with Down syndrome. When developing motor skills, studies
indicate that this public presents a delay in basic motor milestones, which manifest
at slower times than children with typical development, and cognitive developmental
delay stems from the symptom manifestation of this genetic condition [6]. It is
also seen in the literature that motor deficits are predominant in early childhood,
whereas cognitive deficits are predominant at school age [6]. A study which evaluated
the functional performance of children with Down syndrome in relation to the performance
of children with typical development (with average age of 5-7½ years) suggests that,
as the child with delay is acquiring skills, these are incorporated in her/his daily
life and, consequently, they will increase her/his independence [19].
The intervention proposed by the institution recommends interdisciplinary
and group care to provide the children and their families with a thorough follow-up.
We find in the literature the bases to structure this kind of intervention regarding
the organization and the way to provide care. Thus, the work of early stimulation
must be structured so as to welcome the child and her/his family. Regarding integrality,
professionals need a broader view of health, including their different forms of
production and the users’ perception of their biopsychosocial
totality. The professional must listen the user attentively, receive her/him in
a humanized way, using adequate answers, and then becoming responsible, generating
links, humanization, care and welcoming, actions which can contribute to the construction
of integrality. The professionals must understand the context of people and identify
assistance, prevention and health promotion needs, hence exchanging knowledge among
professionals [20].
Therefore, the care should be weekly, lasting between twenty and forty minutes
for individual care, and between one hour and one hour and forty minutes in groups.
Family members play a fundamental role in this context and need to receive the due
support and necessary orientations from the professionals involved to ensure the
continuity of the treatment at their homes [10]. The materials and physical spaces
should also be taken into account, with the former being suitable for each age group,
and the latter ventilated and adapted to the child’s needs [10,21]. The team of professionals must be willing to play an active
part in the intervention processes, take part in triage and assessment processes,
as well as provide the families with orientation and information for the program’s
full implementation [10]. The child with Down syndrome presents deficiency in the
motor, cognitive, sensory and vestibular system, thus, the treatment with an interdisciplinary
team is vital, since the therapies complement each other [22]. There is also the
possibility of a single therapist, in case there is not any multidisciplinary team
available, but such professional must pay attention to all the child’s needs and
not stick to the knowledge field of her/his speciality
[10].
Motor performance, which is addressed in the activities related to posture
and movement; auditory reaction and visual sensitivity; body games and interaction
with the examiner; perception and manual exploration of objects and handling and
recognition of object function had the highest growth when comparing pre- and post-intervention
results. It is believed that, in this case, the early stimulation program has allowed
for the integration of multiple systems and, therefore, made it easier for the children
to reach such motor milestones more rapidly. A study concluded that children who
received in group motor intervention showed a dramatic increase in their basic motor
skills, such as lying down and rolling, crawling and kneeling, in comparison to
children who only received individual training [23]. In a systematic review of the
motor performance of children with Down syndrome, it has been found that early intervention
can be used to reach motor milestones more rapidly, mainly in gait, and that such
positive response in motor performance is fundamental to the child’s integral development
[24].
It is noted that the activities related to sound emission and repetition;
interaction with other people and task completion on request kept the same classifications.
These activities address areas concerning language/cognition. In regard to the activities
of task completion on request, that is, to stop the activity when asked to, to clap,
to stroke and to reply to the request to hand objects in, these are behaviors which
usually appear at the end of the third trimester of life and normalize and stabilize
in the fourth trimester [14]. It is possible to infer, from this, that the children
were not able to perform such activities because, in the second assessment, most
of them were at the end of the second trimester of life. Our results corroborate
the findings of another study on motor performance, coordination and language which
observed that language had the lowest scores than the control group and that such
developmental area is the most compromised in children with Down syndrome [25,26].
It is widely known that the three first years of a child are crucial, because
her/his brain potentialities are fully developing. It is fundamental to provide
children with a welcoming and appropriate environment, to create strong bonds with
their careers, thus forming the bases for a full development [27].
Conclusion
In group early stimulation has brought benefits on the motor and cognitive
development of children with Down syndrome in a Special Child Integration Center.
It should be noted that this study has some limitations, such as the small number
of children assessed and the absence of a control group. Despite these limitations,
this study has raised pertinent issues concerning the interdisciplinary care of
children with Down Syndrome aiming at their full development.
References
- Illingworth RS. The development of the
infant and the young child: Normal and abnormal. Elsevier Health Sciences; 2013
- Palma MS, Pereira BO, Valentini NC. Guided play and free play in an enriched environment:
Impact on motor development. Motriz: Revista de Educação Física 2014;20(2):177-85.
- Ammar D, Acevedo GA, Cordova A. Affordances
in the home environment for motor development: a cross-cultural study between American
and Lebanese children. Child Dev Res
2013. http://dx.doi.org/10.1155/2013/152094
- Caçola P, Bobbio
TG. (2010). Low birth weight and motor development outcomes: the current reality.
Rev Paul Pediatr 2010;28(1):70-6.
- Gallahue DL, Ozmun JC, Goodway JD. Compreendendo
o desenvolvimento motor-: bebês, crianças, adolescentes e adultos.
Porto Alegre: AMGH; 2013.
- Martin GE, Klusek J, Estigarribia B, Roberts
JE. Language characteristics
of individuals with Down syndrome. Topics in Language Disorders 2009;29(2):112.
- Saccani R, Valentini NC. Cross-cultural analysis of the motor development of Brazilian, Greek and
Canadian infants assessed with the Alberta Infant Motor Scale. Rev Paul Pediatr 2013;31(3):350-8.
- Saccani R, Valentini NC, Pereira KR, Müller AB, Gabbard
C. Associations of biological factors and affordances in the home with infant motor
development. Pediatr Int 2013;55(2):197-203.
- Bolsanello
MA. Interação mãe-filho
portador de deficiência: concepções e modo de
atuação dos profissionais em estimulação
precoce [Dissertation]. São Paulo: Universidade de São
Paulo; 1998.
- Brasil.
Diretrizes Educacionais
sobre Estimulação Precoce. In: Ministério da
Educação: Organização das
Nações Unidas
para a educação, a ciência e a cultura. Brasília: MEC/
Unesco; 1995.
- Nair MKC, Resmi VR, Krishnan R, Nair GH, Leena ML, Bhaskaran D et al. CDC Kerala 5: developmental
therapy clinic experience–use of child development centre
grading for motor milestones. Indian J Pediatr 2014;81(2):91-8.
- Farias Brehmer
LC, Souza Ramos FR. O modelo de atenção à
saúde na formação
em enfermagem: experiências e percepções.
Interface-Comunicação, Saúde,
Educação
2016;20(56).
- Silva TRD, Canto GDL.
Dentistry-speech integration:
the importance of interdisciplinary teams formation. Revista CEFAC 2014;16(2):598-603.
- Pinto EB, Vilanova LC.
O desenvolvimento do comportamento da criança no primeiro ano de vida: padronização
de uma escala para a avaliação e o acompanhamento. Casa do Psicólogo; 1997.
- Almeida CS, Valentini NC, Lemos CXG. (2006). A influência de um programa
de intervenção motora no desenvolvimento de bebês em creches de baixa renda. Temas Desenvolv 2006;14(83/84):40-48.
- Souza ESD, Magalhães LDC. Motor and functional
development in infants born preterm and full term: influence of biological and environmental
risk factors. Rev Paul Pediatr 2012;30(4):462-70.
- Miquelote AF, Santos DC, Caçola PM, Montebelo MIDL, Gabbard C. Effect of the home environment on motor and cognitive
behavior of infants. Infant Behav Dev
2012;35(3):329-34. http:// doi:
10.1016/j.infbeh.2012.02.002
- Sgandurra G, Bartalena L, Cioni G, Greisen G, Herskind A, Inguaggiato E, et al.
Home-based, early intervention with mechatronic toys for preterm infants at risk
of neurodevelopmental disorders (CARETOY): a RCT protocol. BMC Pediatrics 2014;14(1):268.
- Martins MRI, Fecuri MAB, Arroyo MA, Parisi MT. Evaluation of functional skills and self care of Down's syndrome people included in therapeutic
workshop. Revista
CEFAC 2013;15(2):361-5.
- Sanchez HF, Werneck MAF,
Amaral JHL, Ferreira EF. Integrality in everyday
dental care: review of the literature. Trab Educ
Saúde 2015;13(1):201-14.
- Frônio JDS, Silva LMDA, Gonçalves
RJ, Chagas PSDC, Ribeiro LC. Influence of object position
on the frequency of manual reaching in typically developing infants. Fisioter Pesqui
2011;18(2):139-44.
- Edgin JO. Cognition in Down syndrome: a developmental cognitive neuroscience
perspective. Wiley Interdisciplinary Reviews: Cognitive Science 2013;4(3):307-17.
- Fiss ACL, Effgen SK, Page J, Shasby
S. Effect of sensorimotor groups on gross motor acquisition for young children with
Down syndrome. Pediatr Phys
Ther 2009;21(2):158-66.
- Bertapelli F, Silva FF, Costa LT,
Gorla JI. Desempenho motor de crianças com Síndrome de
Down: uma revisão sistemática. J Health Sci Inst 2011;29(4):280-84.
- Priosti PA, Blascovi-Assis SM, Cymrot
R, Vianna DL, Caromano FA. Grip strength and manual dexterity in Down Syndrome
children. Fisioter Pesqui 2013;20(3):278-85.
- Carvalho AMDA, Befi-Lopes DM, Limongi SCO. (2014, June).
Mean length utterance in Brazilian children: a comparative
study between Down syndrome, specific language impairment, and typical language
development. CoDAS 2014;26(3):201-7. http://dx.doi.org/10.1590/2317-1782/201420140516.
- Cunha AJLAD, Leite AJM,
Almeida ISD. The pediatrician's role in the first thousand days of the
child: the pursuit of healthy nutrition and development. J Pediatr
2015;91(6):S44-S51.