ORIGINAL
ARTICLE
Effects
of aquatic physiotherapy versus conventional physical therapy on the risk of
fall in the elderly: a randomized clinical trial
Efeitos da fisioterapia
aquática versus fisioterapia convencional no risco de queda em idosos: ensaio
clínico
Christye Ramos da Silva*,
Leonardo Farias Rodrigues Magalhães**, Fernanda Manaia
Gonçalves Chaves***, Erica Cardaretti do Nascimento
Vieira****, Ana Paula Radies Adames*****, Igor da Silva Diniz Brauns******
*Graduated
in Physiotherapy – Veiga de Almeida University,
Postgraduate student in Human Performance Science - Federal University of the
State of Rio de Janeiro, Physiotherapist of TRATA Institute, Member of the
Technological Evaluation Center in Rehabilitation and Health – NATReS/UVA, **Graduated in Physiotherapy – Veiga de Almeida University; Member of the Technological
Evaluation Center in Rehabilitation and Health – NATReS/UVA,
***Graduated in Physiotherapy – Veiga de Almeida
University; Master in Psychiatry and Mental Health – Federal University of the
State of Rio de Janeiro; Professor at Veiga de
Almeida University,****Graduated in Physiotherapy – Estácio
de Sá University; Master in rehabilitation science – University Center Augusto
Motta, Professor at Veiga de Almeida University,
*****Graduated in Physiotherapy – Veiga de Almeida
University, Postgraduate student in Applied Neuroscience – Federal University
of the State of Rio de Janeiro; Physiotherapist of TRATA Institute and
Institute for Applied Neuroscience, Member of the Technological Evaluation
Center in Rehabilitation and Health – NATReS/UVA,
******Graduated in Physiotherapy – Veiga de Almeida
University; Master in Psychiatry and Mental Health – Federal University of the
State of Rio de Janeiro; Professor at Veiga de
Almeida University
Received: Dec
11, 2019; accepted: May 16, 2020.
Corresponding author: Christye
Ramos da Silva, Praça da Bandeira, 149, Praça da Bandeira, 20270-150 Rio de
Janeiro RJ
Christye Ramos da Silva:
christyeramos@yahoo.com.br
Leonardo Farias
Rodrigues Magalhães: leonardo92_farias@hotmail.com;
Fernanda Manaia Gonçalves Chaves: manaiafernanda@gmail.com
Erica Cardaretti do Nascimento Vieira: erica.nascimento@uva.br
Ana Paula Radies Adames:
ana.adames712@gmail.com
Igor da Silva Diniz Brauns: braunsigor@gmail.com
Abstract
Objective: To identify whether physiotherapy treatment in water is more effective
than the treatment in land environment, aiming at improving the process of
physical limitation or functional inability (gait speed, balance, motor
abilities) caused by lack of balance in elderly with risk of fall. Methods:
Randomized clinical trial, experimental study. The sample was composed of 35
senior individuals of both sexes, with average age of 65. Nineteen people
composed the control Group /Conventional Physiotherapy, while the rest composed
the experimental Group/Aquatic Physical therapy. Both groups were submitted to
twenty sessions of physical therapy, twice a week, for 50 minutes in individual
treatment. Aerobic activities were conducted for both groups separately. Exercises
using water specific therapy, such as Halliwick
rotation control and Bad Ragaz ring method, were used
in the aquatic group and in the conventional group, physiotherapeutic
techniques were applied, approaching the concepts of proprioceptive
neuromuscular facilitation (PNF) and decubitus change training. The following
tests were used to measure the risk of fall/balance: Timed Up and Go Test,
Sit-to-Stand in 30 seconds and Functional Reach. Results: Both
physiotherapeutic interventions, aquatic and conventional, showed to be greatly
efficient however aquatic physiotherapy showed certain advantages compared to
conventional physical therapy, promoting more beneficial effects in the gait
speed, balance, motor abilities and, mainly, in the reduction of the risk of
fall.
Keywords: elderly, Halliwick, Bad Ragaz,
Physical therapy, aquatic, risk of fall.
Resumo
Objetivo: Identificar se a
Fisioterapia aquática é mais eficaz que a fisioterapia convencional, visando a
melhora do processo de limitação física ou incapacidade funcional (Velocidade
da marcha, equilíbrio, habilidades motoras) causada por desequilíbrio em
pacientes idosos com risco de queda. Métodos: Ensaio clínico
randomizado, estudo experimental. A amostra foi composta por 35 idosos de ambos
os sexos, com uma média de idade de 65 anos. Dezenove pessoas compuseram o
Grupo Controle/Fisioterapia Convencional, enquanto o restante constituiu o
Grupo Experimental / Fisioterapia Aquática. Ambos os grupos foram submetidos a
vinte sessões de fisioterapia, duas vezes por semana, durante 50 minutos em
tratamento individual. As atividades aeróbicas foram realizadas para ambos os
grupos separadamente. Exercícios utilizando terapia específica da água, como o
controle de rotação de Halliwick e o método do anel
de Bad Ragaz, foram
utilizados no grupo aquático e, no grupo convencional, foram aplicadas técnicas
fisioterapêuticas, abordando os conceitos de facilitação proprioceptiva e
treinamento de mudança de decúbito. Os seguintes testes foram usados para medir
o risco de queda/equilíbrio: Timed Up and Go Teste, Teste de sentar e levantar em 30 segundos e Teste de Alcance
Funcional. Resultados: Ambas as intervenções fisioterapêuticas,
aquáticas e convencionais se mostraram bastante eficientes, entretanto a
fisioterapia aquática apresentou certas vantagens em relação à fisioterapia
convencional, promovendo efeitos mais benéficos na velocidade da marcha,
equilíbrio, habilidades motoras e, principalmente, na redução do risco de
queda.
Palavras-chave: idosos, Halliwick, Bad Ragaz, Fisioterapia, ambiente aquático, risco de queda.
Introduction
When becoming older, our body goes through changes that, even when not
related to any pathological process, result in the progressive degradation of
the organism, thus generating a decrease in the individual capacity of
executing certain daily life tasks. Such systemic change is reflected in an
increase in the fall predisposition in older individuals [1]. According to the
IT department of the Brazilian Health System (DATASUS), falling was the highest
cause of hospitalization among the senior population, especially in individuals
in the age of 70 or older, reaching 57.53 for every 10,000 Brazilian residents.
In individuals between the age of 20 and 45, the tendency to fall is
18.5%, going up to 21% in middle-aged people, and increasing even more up to
35% in people over 65. Within the young population, such phenomenon occurs, in
most times, during physical activity practice, especially in the case of
running, while in elderly persons, such incident occurs during basic daily
activities, such as walking [2]. Fall represents a great risk for the health of
the elderly, resulting in morbidity or mortality, due to their greater
vulnerability to loss of balance [3].
It is possible to relate different sensory-motor areas, which guarantee
the integrity of balance while walking [4]. Through neuroimages, Ferraye [5] showed the activation of many different parts
of the motor and sensory systems for balance regulation, highlighting fronto-parietal regions, basal nuclei, cerebellum and
supplementary motor area.
In addition, Bakker [6] related cerebral areas to the precision of
walking, detecting both the need for efferent information to execute the motor
act and the need for sensory information to identify some kind of instability
and provoke appropriate stabilizing responses, through programmed feeding
reactions or through continuous and updated feedback corrections, thus
activating the necessary muscles for movement orientation of the body within
space [7].
On the other hand, the insufficiency of such sensory, neural and/or
musculoskeletal systems causes the slowdown reaction response to the mass
center movement, which is triggered by sudden external disruption, to be
reduced and not efficiently executed [8]. The degeneration of such systems due
to aging is associated to lower functional performance and to higher risk of
falling, thus possibly making these individuals dependent on others. However,
many different treatments have been used; among them, conventional physical
therapy can be highlighted, featuring many intervention techniques to reduce
the aging effects, such as the combination of balance and strength training
[9], gait training [10] and others, thus helping these people to return to
their daily life activities with better quality.
With regards to the other techniques, aquatic physical therapy is able
to generate greater instability in the individual, when compared to the land
therapy (conventional physical therapy), increasing the neuron inputs to the
central nervous system, which will regulate the musculoskeletal system to
balance postural instability [11]. Despite some studies demonstrating
improvement in mobility of individuals submitted to the aquatic physical
therapy, these are still limited [12]. Therefore, there is a need for more
researches comparing the treatment in water versus the land environment, aiming
at improving the process of physical limitation or functional inability, including
decreased gait speed and motor abilities caused by lack of balance that may
also increase the risk of falling which is the purpose of this work.
Methods
This work consists of an experimental study – a randomized clinical
trial. It has been submitted to the Brazil Platform with the title “Comparison
between an aquatic physiotherapy protocol versus conventional physiotherapy in
the risk of fall in the elderly” and it has been approved by the Ethics
Committee of Research at Veiga de Almeida University,
nº 2.904.741 CAAE: 80453417.8.0000.5291. All intervention and data collection
have been conducted at the Veiga de Almeida Health
Center (CSVA in the Brazilian acronym), an institution linked to Veiga de Almeida University.
Sample
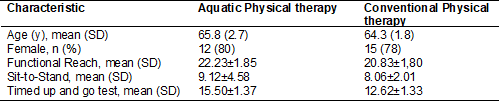
The sample initially was composed of 38 senior individuals of both
sexes, with average age of 65 but just 35 individuals concluded the study and
received the full intervention. Table I presents the description of
characteristics for each group. The reasons for non-compliance was
hospitalization for anemia, cancer treatment and one death (figure 1).
The inclusion criteria demanded that all seniors were over the age of 60
and had reported fall incidents in the last 6 months, while the exclusion
criteria involved individuals who were conducting other types of treatment that
could interfere in the sample, such as: osteopathic manipulative techniques,
conventional physiotherapeutic treatments, recent fractures, neurological
diseases, fecal and/or urinary incontinence, arthritis in the hips or limiting
knees, and severe aphasia, identified by individual reports or by medical
opinion.
The sample calculation was obtained through the GPower
program, version 3.1, through F-test, a priori, considering assessment time as
intra-individual factor and group as among-individuals factor. In the
calculation, we consider the type I error in 5% (α=0.05) and power of 90%.
The effect size has been delimited through collection of data on the number of
elderly people attending the Veiga de Almeida Health
Center. So, considering two groups and three variables, the statistical program
suggested a sample with eighteen individuals in each group.
Table
I - Baseline characteristics.
A randomization was conducted by a third appraiser who was no involved
in recruitment. The sequence was obtained through the Random Integer Generator
app for Android, where the participants were numbered from 1 to 38. Group
allocation was concealed from the investigator through sealed, opaque
envelopes.
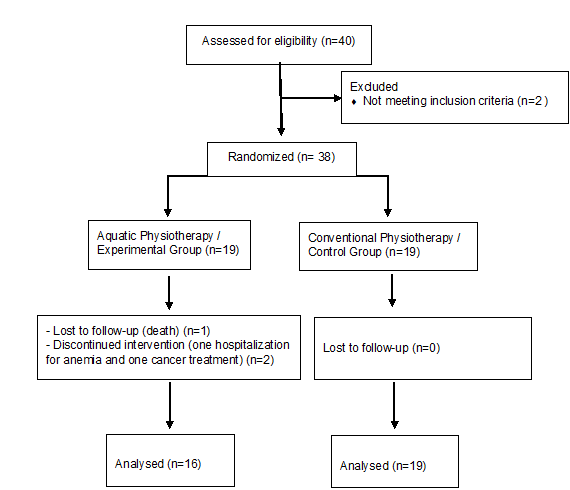
Figure
1 - Flow diagram for randomization: A randomized
clinical trial.
The patients agreed on participating voluntarily in the study by signing
the Free and Clarified Consent Term submitted to the following address: Veiga de Almeida Health Center, Praça
da Bandeira, 149 - Praça da Bandeira, Zip Code
20270-150. The study was conducted between December 2016 and November 2018,
after completing all necessary assessments.
Experimental design
Both interventions were provided by physical therapists who received
training from experts in Orthopedic Trauma and aquatic therapy (Bad Ragaz Ring Method and Hallick).
This training included a 3-week and the same experts organized regular meetings
during the trial to monitor delivery of interventions. No changes in the
protocol were observed.
The groups showed very similar conducts (table II). Both groups were
submitted to twenty sessions of physical therapy, twice a week, for 50 minutes
in individual treatment. Both interventions were provided by physical
therapists who received training from experts in orthopedic trauma and aquatic
therapy (Bad Ragaz Ring Method and Hallick). This training included a 3-week and the same
experts organized regular meetings during the trial to monitor delivery of
interventions. No changes in the protocol were observed.
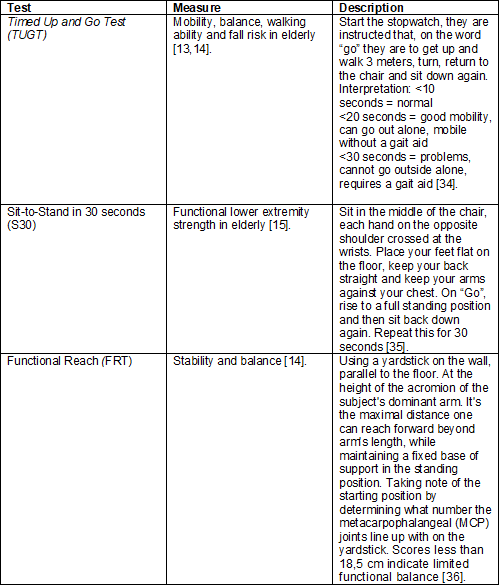
All participants were submitted to the following kinetic-functional
tests that were used to measure the risk of fall/balance: Timed Up and Go Test
(TUGT) used to measure mobility, balance, walking ability and fall risk in
elderly [13,14]. Sit-to-Stand in 30 seconds (S30) is a tool that assesses
functional lower extremity strength in elderly [15] and Functional Reach (FRT)
used to assess an elderly stability and balance, with the goal of obtaining the
initial parameters for fall predisposition and of comparing them at a later
moment [14]. These functional tests evaluate important parameters for balance
and describe the patient's functional profile in your daily tasks.
Conduct
of the experimental and control group
During the first fifteen minutes, aerobic activities were conducted for
both groups differentiating only the environment, including gait exercises with
and without obstacles, direction changes and double tasking. After thirty-five
minutes, exercises using water specific therapy in experimental group, such as Halliwick rotation control and Bad Ragaz
ring method and pool with the temperature between 31° and 34° degrees Celsius.
In the CG, physiotherapeutic techniques were applied, approaching the concepts
of proprioceptive neuromuscular facilitation (PNF), decubitus change training
and balance training aiming at bringing closer the conducts of the experimental
and control groups, considering that the Bad Ragaz
method utilizes the PNF principles, and the Halliwick
rotation control simulates the decubitus changes. In the experimental group
balance training was not applied.
Table
II - Conducts executed within the aquatic physical
therapy and conventional physical therapy groups.
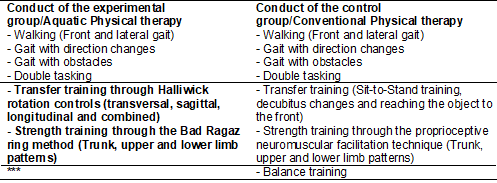
***In
the aquatic physical therapy group, balance training was not applied.
Outcomes
In the beginning of treatment all participants received a booklet
containing the main information about the elderly falls
prevention. The primary outcomes were risk of falling (measured with TUG, FRT
and S30) and effectiveness of both physical therapy treatment (measured with
the three kinetic-functional tests). Secondary outcomes were gait speed
(measured with TUG), balance (measured TUG and FRT) and motor abilities (TUG
and S30) [13-15]. The assessments were carried out at three moments. First
assessment was carried out before the start of interventions. The second
assessment was carried out in the end of the 10th session and the third
assessment, at the end of the 20th session. Approximate interval of assessments
lasted for at least one month except for the first. A total of 3 months of
treatment. The nature of the interventions precluded blinding of the subjects
and therapists.
Statistical
analysis
The data analysis was obtained through the Stata program, version 25.0,
through a Mixed Variance Analysis (ANOVA) with two factors and repeated
measures, considering time (first, second and third assessment) as
intra-individual factor and group as among-individuals factor. The data
distribution was analyzed by the Shapiro-Wilk test (p<0.05), considering the
normality standard. This study aims at showing the interaction between the
groups, through the following fall-predicting tests: TUGT, FRT and S30 with a
time interval of 10 sessions.
Results
Out of the initial sample, 35 individuals concluded the study and
receive the full intervention. The average age was of 65.
In the FRT, time proved to have an effect for the Aquatic Physical
therapy group (EG), with an increase between the first and second assessment
[DF = 5.053; p = 0.0001], between the first and third assessment [DF = 11.941;
p = 0.0000000004] and between the second and third assessment [DF = 6.888; p
=0.00002]; for the Conventional Physical therapy group (CG), an increase
occurred between the first and second assessment [DF = 4.278; p = 0.001] and
between the first and third assessment [DF = 6.833; p = 0.00001], while no
significant difference was found between the second and third assessment [DF =
2.556; p = 0.146].
Therefore, when comparing the two groups, it is possible to observe
greater average and difference for the aquatic physical therapy group (Figure
2).
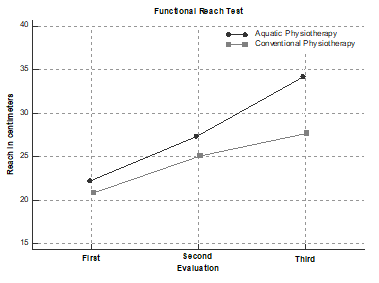
*
Significance value < 0.05.
Figure
2 - Average and comparison of the assessments of the
Functional Reach Test between the aquatic physical therapy (EG) and the
conventional physical therapy groups (CG).
For the S30, time showed an effect for the EG with an increase between
the first and second assessment [DF = 1.647; p = 0.001], between the first and
third assessment [DF = 3.882; p = 0.00008] and between the second and third
assessment [DF = 2.235; p =0.008] and for the CG, an increase occurred between
the first and second assessment [DF = 1.111; p = 0.025], between the first and
third assessment [DF = 3.556; p = 0.0001] and between the second and third
assessment [DF= 2.444; p =0 .003].
This way, when comparing the two groups, it is possible to observe
greater average and difference for the aquatic physical therapy group (Figure
3).
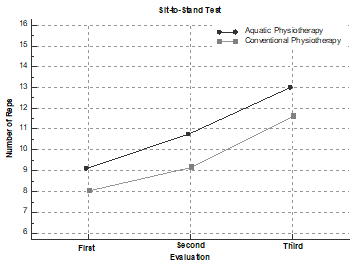
*Significance
value 0.05.
Figure
3 - Average and comparison of the assessments of the
Sit-to Stand in 30 seconds between the aquatic physical therapy (EG) and the
conventional physical therapy groups (CG).
With regards to the effect of time on the dynamic balance TUGT,
difference was found for the EG, with a reduction in the average between the
first and second assessment, [DF = -2.182; p = 0.05], between the first and
third assessment [DF = -5.915; p = 0.0002] and between the second and third
assessment [DF = -3.734; p = 0.00001]. No significant difference was found
among the values in the CG (Figure 4).
Assessment
average of the Timed Up and Go Test
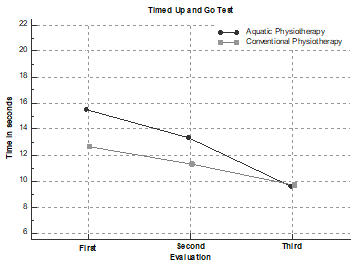
*Significance
value < 0.05
Figure
4 - Average and comparison of the assessments of the
Timed Up and Go Test between the aquatic physiotherapy (EG) and the
conventional physical therapy groups (CG).
The two-way mixed ANOVA showed that time has an effect on the TUGT [F
(1.253, 41.363) = 20.752; p <0.05], Sit-to-Stand [F(1.408, 1.408) = 34.117;
p <0.05] and FRT [F(2, 2) = 60.461; p <0.05]. No effect was found for the
group, but interaction between time and group was observed for the functional
reach test [F (2, 2) = 5.199; p <0.05]; a difference of 6.5 cm was found in
the third assessment [F(7.156); DF = 6.510; p = 0.012] between the Aquatic
Physical therapy (34.176±1.745 mean ± sd) and the
Conventional Physical therapy (27.667 ± 1.696 mean ± sd)
groups (Table III). Our trial blinding of all assessor who measured outcome.
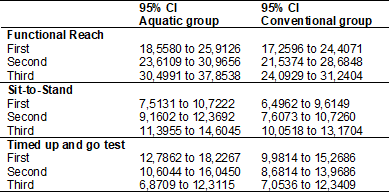
Table
III - Intra-group analysis of the Time effect. *value
< 0.05, Bonferroni Post Hoc Analysis.
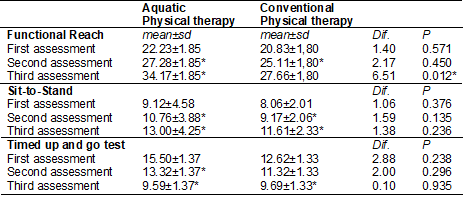
Table
IV - Intra-group analysis of confidence interval.
Discussion
Many authors argue in favor of certain functional tests to be fall
predictors in elderly individuals, especially the TUGT, FRT and S30 [16,17]. In
the present study, such tests classified the participating elderly people to be
at risk of fall at the moment previous to the experiment; however, at the end
of the intervention period, values were found that put them out of the fall
risk, defined through the prediction for the elderly [18].
A few factors seem to be related to the results and the difference
between physiotherapeutic conducts in different environments. For aquatic
physical therapy, it is possible to highlight instability triggered by the
junction of hydrodynamic and physiological immersion properties [19]. The
influence of the aquatic environment can be initially described as adaptation
and response to the instability offered by the surroundings. However, the
better performance of the elderly in the functional tests that demanded balance
and mobility indicates the activities executed to have influenced the
participants and to have decreased the risk of fall.
Likewise, it is possible to observe participants in the conventional
physical therapy improve, thus supporting some of the results found in a
systematic analysis conducted by MAT [20], which showed strength exercises,
balance training and aerobic exercises to optimize balance and improve gait
performance. On the other hand, for the aquatic physical therapy method, no
balance training was used with the participants of this group; however, the
results were satisfactory, which could be related to the aquatic environment
[21].
According to Marinho-Buzelli [22], water
physical characteristics can provoke greater instability to the immersed body,
submitting it to constant challenges for balance maintenance. Therefore, the
results obtained in the present study, specifically for the functional reach
test, showed better capacity of the participants to shift their gravity center
front to back, and to remain inside the support basis, mainly in the aquatic
environment. Possibly, such environment was able to offer the individual a
greater participation of the central nervous system to regulate the joints,
mainly of the trunk and lower limb muscles, to compensate the oscillations
caused by water, trying to maintain the individuals stable within the offered
circumstances [23].
Additionally, a study conducted by KIM [24], compared the influence of
PNF in the aquatic and land environments, quantifying them through some
functional tests also utilized in this study, such as the TUGT and FRT. The
results showed both groups to improve after the intervention; however, when
comparing one group to the other, the aquatic one performed better. This
reinforces even more the good results found in the present study, indicating
that the Bad Ragaz, which is based on PNF,
effectively promoted improved muscular activity, through its diagonals, maybe
because it recruited a greater quantity of muscular fibers, due to the
conditions offered by the aquatic environment. This possibly maximized the
proprioceptive stimulation and the offered resistance, thus fostering improved
muscular strength, flexibility and balance [25].
In general, aquatic physical therapy takes advantage of such
three-dimensional environment to potentialize the motor learning process. The Halliwick method allowed the individuals to progress with
their independence in water through mental adaptation and through rotation
control that can reproduce basic daily life activities, such as decubitus
change for example. Therefore, improvement in muscular strength, joint mobility
and movement amplitude reinforce the positive findings of the tests applied. We
believe that, possibly, aquatic physical therapy may have also positively
influenced the results, by reducing the fear of falling after perceiving that
they were able to execute tasks they previously thought to not be possible
outside of such environment, even though the present study did not use any
tools to measure this aspect [26,27].
Menant [28], in his
systematic review, observed some essential factors for fall prediction in the
elderly, mainly highlighting the gait speed, considering that the fall usually
occurs due to the limitations these individuals have when walking. In a
complementary way, it is necessary to highlight the importance of the positive
results this study obtained for the TUGT, where the individuals were able to
cover the same distance in a shorter time and with better quality. Such gain,
for the group that executed the task in the aquatic environment, can be
justified by the easiness that the thrust offered, thus allowing the human body
to float, reducing the body overweight and facilitating certain movements, for
example some key movements in the gait, such as dorsiflexion and the hip joint
flexion, thus contributing to better walking [24,25]. On the other hand, no
significant improvement in decreasing the time occurred for the TUGT test in
the control group.
The gradual improvement in the kinetic-functional tests used inspires
the relevance of intervention programs in the balance increase through the
activities executed. Among the methods, neuroplasticity stimulation through learning
new abilities can be highlighted, done by reorganizing the neural network in
response to the stimulus, generating memory consolidation thanks to
experimentation. Among the groups, with certain advantage for the aquatic
group, the research observed that postural changes offered by the aquatic
environment, together with the slowdown of movements due to viscosity, allowed
the immersed individuals to have more time to plan the balance reaction. Such
property possibly allowed for the subjects to experiment attempts of trial and
error, thus stimulating better motor planning [12,29].
The results of the present study can be justified by the occurrence of
the learning factor after a period of repetition, once the pool allowed for the
slowdown of movements, facilitating repetition and, as a result, the
acquisition of new information through working memory and the information
already stored in the long-term memory and, according to the stimuli
recurrence, such information became stronger and stronger until getting fixed
[30]. In addition, physical exercise stimulates angiogenesis, sinaptogenesis and cellular proliferation by liberating the
Insulin-like growth factor 1 (IGF-1), the Brain-derived Neurotrophic Factor
(BDNF) and the Vascular Endothelial Growth Factor (VEGF). Such factors that are
optimized within the aquatic environment can promote brain plasticity, thus
increasing cortical activity and causing better learning and motor memory
[31,32].
Among the limitations of the study, a suggestion is to use
electromyography in future researches to compare and measure muscular electric
activity; an accelerometer to determine more detailed gait parameters (pace,
length, speed); neuroimage resources to analyze the activation of cortical and
sub-cortical areas in the aquatic environment and measure of the psychological
aspects. It is worth highlighting that, considering the positive results, the
methodology of the present study allowed to reach the main objectives,
collaborating for the knowledge about strategies to reduce the risk of fall and
the facilitation of aquatic physical therapy in this process. Current evidence
highlights that sedentarism, which is a very common factor in the elderly
population, results in an aggravation of the health of such individuals,
triggering greater fragility and dependence, thus showing that regular physical
activity decreases the risk of fall, cardiovascular diseases, cognitive
alterations, muscular weakness and others [33].
Conclusion
Both physiotherapeutic interventions, aquatic and conventional, showed
to be greatly efficient, promoting beneficial effects in the gait speed,
balance, motor abilities and, mainly in the reduction of the risk of fall,
which may have possibly influenced the elderly participants of this study to
reintegrate again their activities. Aquatic physical therapy involved aerobic
exercise and water-specific exercises, approaching the concepts of Halliwick and the Bad Ragaz Ring
Method, and showed certain advantages compared to conventional physical
therapy. We suggest this improvement to be related to the physical properties
of the aquatic environment. This essay can also demonstrate the patient’s
gradual evolution process, showing us the importance and relevance of each
assistance technique.
References
- Balzer
K, Bremer M, Schramm S, Lühmann D, Raspe H. Falls prevention for the elderly. GMS Health Technol
Assess 2012;8. https://doi.org/10.3205/hta000099
- Talbot
L, Musiol RJ, Witham EK, Metter EJ. Falls in young, middle-aged
and older community dwelling adults: perceived cause, environmental factors and
injury. BMC Public Health 2005;5(1):86. https://doi.org/10.1186/1471-2458-5-86
- Rubenstein
LZ. Falls in older people: epidemiology, risk factors and strategies for prevention.
Age and Ageing 2006;35(suppl2):ii37-ii41. https://doi.org/10.1093/ageing/afl084
- Baezner H, Blahak
C, Poggesi A, Pantoni L, Inzitari D, Chabriat H et al. Association
of gait and balance disorders with age-related white matter changes The LADIS Study.
Neurology 2008;70(12):935-42. https://doi.org/10.1212/01.wnl.0000305959.46197.e6
- Ferraye MU, Debû B, Heil L, Carpenter M, Bloem
BR, Toni I. Using motor imagery to study the neural substrates of dynamic balance.
PloS one 2014;9(3)e91183, 2014. https://doi.org/10.1371/journal.pone.0091183
- Bakker
M, De Lange FP, Helmich RC, Scheeringa
R, Bloem BR, Toni I. Cerebral correlates of motor imagery
of normal and precision gait. Neuroimage 2008;41(3):998-1010. https://doi.org/10.1016/j.neuroimage.2008.03.020
- Grush R. The emulation theory of representation:
Motor control, imagery, and perception. Behav Brain Sci.
2004;27(3):377-96. https://doi.org/10.1017/S0140525X04000093
- Maki
BE, MCilroy, William E. Control of rapid limb movements
for balance recovery: age-related changes and implications for fall prevention.
Age and ageing 2006;35(suppl2):ii12-ii18. https://doi.org/10.1093/ageing/afl078
- Lacroix
A, Kressig RW, Muehlbauer T,
Gschwind YJ, Pfenninger B, Bruegger O, Granacher U. Effects of
a supervised versus an unsupervised combined balance and strength training program
on balance and muscle power in healthy older adults: a randomized controlled trial.
Gerontology 2016;62(3):275-88. https://doi.org/10.1159/000442087
- Mochizuki
L, Bigongiari A, Franciulli
PMA, Francica JV, Alonso AC, Ervilha
UF, et al. The effect of gait training and exercise programs on gait and balance
in post-stroke patients. Medical Express 2015;2(4). https://doi.org/10.5935/MedicalExpress.2015.04.01
- Bayraktar D1, Guclu-Gunduz A, Yazici G, Lambeck J, Batur-Caglayan HZ, Irkec C, Nazliel B. Effects of Ai-Chi on balance, functional mobility, strength and fatigue
in patients with multiple sclerosis: a pilot study. Neuro Rehabilitation 2013;33(3):431-7.
https://doi.org/10.3233/NRE-130974
- Marinho-Buzelli AR, Bonnyman AM, Verrier MC. The effects of aquatic therapy on mobility
of individuals with neurological diseases: a systematic review. Clin Rehabil 2015;29(8):741-51. https://doi.org/10.1177/0269215514556297
- Bohannon
RW. Reference values for the timed Up and Go test: a descriptive meta-analysis.
J Geriatr Phys Ther 2006;29(2):64-8.
https://doi.org/ 10.1519/00139143-200608000-00004
- Brooks
D, Davis AM, Naglie G. Validity of 3 physical performance
measures in inpatient geriatric rehabilitation. Arch Phys Med Rehabil 2006;87(1):105-10. https://doi.org/ 10.1016/j.apmr.2005.08.109
- Rikli RE1, Jones CJ. Development and validation
of criterion-referenced clinically relevant fitness standards for maintaining physical
independence in later years. Gerontologist 2013;53(2):255-67. https://doi.org/10.1093/geront/gns071
- Bhatt
T(1), Espy D, Yang F, Pai YC. Dynamic gait stability, clinical
correlates, and prognosis of falls among community-dwelling older adults. Arch Phys
Med Rehabil 2011;92(5):799-805. https://doi.org/10.1159/000442087
- Nocera
JR, Stegemöller EL, Malaty IA,
Okun MS, Marsiske M, Hass CJ. Using the Timed Up &
Go test in a clinical setting to predict falling in Parkinson's disease. Arch Phys
Med Rehabil 2013;94(7):1300-5. https://doi.org/10.1016/j.apmr.2013.02.020
- Kage H, Okuda M, Nakamura I, Kunitsugu I, Sugiyama S, Hobara T.
Measuring methods for functional reach test: comparison of 1-arm reach and 2-arm
reach. Arch Phys Med Rehabil 2009;90(12):2103-7. https://doi.org/10.1016/j.apmr.2009.07.021
- Bergamin M, Ermolao
A, Tolomio S, Berton L, Sergi G, Zaccaria M. Water-versus
land-based exercise in elderly subjects: effects on physical performance and body
composition. Clin Interv Aging 2013;8:1109-17.
https://doi.org/10.2147/CIA.S44198
- Mat
S, Tan MP, Kamaruzzaman SB, Ng CT. Physical therapies
for improving balance and reducing falls risk in osteoarthritis of the knee: a systematic
review. Age Ageing 2015;44(1):16-24. https://doi.org/10.1093/ageing/afu112
- Mann
L, Kleinpaul JF, Mota CB, Santos
SG. Influence of aquatic exercise training on balance in young adults. Fisioter Mov 2014;27(4):573-81. https://doi.org/10.1590/0103-5150.027.004.AO09
- Marinho-Buzelli AR, Rouhani H, Masani K,
Verrier MC, Popovic MR. The influence of the aquatic environment on the control
of postural sway. Gait Posture 2017;51:70-6. https://doi.org/10.1016/j.gaitpost.2016.09.009
- de
Waroquier-Leroy L, Bleuse S, Serafi R, Watelain E, Pardessus V, Tiffreau AV, et
al. The Functional Reach Test: strategies, performance and
the influence of age. Ann Phys Rehabil Med 2014;57(6-7):452-64.
https://doi.org/ 10.1016/j.rehab.2014.03.003
- Kyoung K, Dong-Kyu
L, Eun-Kyung K. Effect of aquatic dual-task training on
balance and gait in stroke patients. J Phys Ther Sci 2016;28(7):2044-47.
https://doi.org/10.1589/jpts.28.2044
- Becker
BE. Aquatic therapy: scientific foundations and clinical rehabilitation applications.
PM & R
2009;1(9):859-72. https://doi.org/10.1016/j.pmrj.2009.05.017
- O Conceito Halliwick 2010, Comitê de Educação e Pesquisa da Associação
Halliwick Internacional. [citado 2017 Nov 20]. Disponível em: http://www.halliwick.org
- Tripp
F, Krakow K. Effects of an aquatic therapy approach (Halliwick-Therapy)
on functional mobility in subacute stroke patients: a randomized controlled trial.
Clin Rehabil 2014;28(5):432-9. https://doi.org/10.1177/0269215513504942
- Menant JC, Schoene
D, Sarofim M, Lord SR. Single and dual task tests of gait speed are equivalent in
the prediction of falls in older people: a systematic review and meta-analysis.
Ageing Res Rev 2014;16:83-104. https://doi.org/10.1016/j.arr.2014.06.001
- Kolb
B, Gibb R. Searching for the principles of brain plasticity and behavior. Cortex 2014;58:251-60.
https://doi.org/10.1016/j.cortex.2013.11.012
- Herzfeld DJ, Vaswani PA, Marko MK, Shadmehr R3. A memory of errors in sensorimotor
learning. Science 2014;345(6202):1349-53. https://doi.org/10.1126/science.1253138
- Knaepen K, Goekint
M, Heyman EM, Meeusen R. Neuroplasticity - exercise-induced response of peripheral
brain-derived neurotrophic factor. Sports Med 2010;40(9):765-801. https://doi.org/10.2165/11534530-000000000-00000
- Cassilhas RC, Tufik S, Mello MT. Physical exercise, neuroplasticity, spatial
learning and memory. Cell Mol Life Sci 2016;73(5):975-83. https://doi.org/10.1007/s00018-015-2102-0
- McPhee
JS, French DP, Jackson D, Nazroo J, Pendleton N5, Degens H. Physical activity in older age: perspectives for healthy
ageing and frailty. Biogerontology 2016;17(3):567-80. https://doi.org/10.1007/s10522-016-9641-0
- Podsiadlo D, Richardson S. The timed
“Up & Go”: a test of basic functional mobility for frail elderly persons. J
Am Geriatr Soc 1991;39(2):142-8. https://doi.org/10.1111/j.1532-5415.1991.tb01616.x
- Rikli RE. Functional fitness normative scores
for community-residing older adults, ages 60-94. J Aging Phys Activity 1999;7:162-81.
- Duncan
PW1, Weiner DK, Chandler J, Studenski S. Functional reach:
a new clinical measure of balance. J Gerontol 1990;45(6):192-7.
https://doi.org/10.1093/geronj/45.6.m192
Anexo
Outcome Measures