ARTIGO
ORIGINAL
Preoperative
physical activity has a protective effect against postoperative pulmonary
complications after abdominal surgery
Atividade física
pré-operatória tem efeito protetor contra complicações pulmonares após cirurgia
abdominal
Fernando Wegner, M.Sc.*, Elinaldo da Conceição dos Santos, PhD**, Daniel Correia
Souza, M.Sc.*, Luciana Dias Chiavegato,
PhD***, Adriana Claudia Lunardi, PhD****
*Master’s
and Doctoral Programs in Physical Therapy of Universidade
Cidade de São Paulo, **Master’s and Doctoral Programs
in Physical Therapy of Universidade Cidade de São Paulo, Department of Biological and Health
Sciences, Universidade Federal do Amapá,
***Master’s and Doctoral Programs in Physical Therapy of Universidade
Cidade de São Paulo, Department of Pneumology, Universidade Federal de São Paulo, ****Master’s and
Doctoral Programs in Physical Therapy of Universidade
Cidade de São Paulo, Department of Physical Therapy
of School of Medicine of University of São Paulo
Received
on: March 13, 2020; accepted on: July 17, 2020.
Corresponding author: Adriana Claudia Lunardi, Master’s and Doctoral Programs
in Physical Therapy,
Universidade Cidade de São Paulo, Cesário Galeno Street, 448/475, 03071-000 São
Paulo SP, Brazil
Fernando Wegner: ferwegner@yahoo.com.br
Elinaldo da Conceição dos
Santos: drelinaldo@yahoo.com.br
Daniel Correia Souza:
daniel.cds01@hotmail.com
Luciana Dias Chiavegato: luciana.chiavegato@unicid.edu.br
Adriana Claudia Lunardi: adrianalunardi@hotmail.com
Abstract
Physical
activity level and fitness condition seem to be related with pulmonary surgical
risk in thoracic and cardiac surgeries; however, in abdominal surgery this
relation is not clear. Objective: To compare the physical activity level in
daily life and during hospitalization before surgery between patients who
developed and did not develop postoperative pulmonary complications (PPC) after
abdominal surgery and to relate to this outcome. Methods: This prospective
cohort enrolled 191 hospitalized candidates (52 ± 14yrs; BMI = 29 ± 11 kg/m2) for
upper abdominal surgery. Two different tools related to two distinct moments
were used to assess preoperatively the physical activity level. First, to
assess life physical activity level, the questionnaire Human Activity Profile
(HAP) was administered for all patients. During hospitalization, the
accelerometry was performed during 4 consecutive days to assess the time in
activity. In addition, lung function, muscle strength and resting energy
expenditure were assessed. PPC (pneumonia, atelectasis or severe hypoxemia)
were checked until discharge. Multivariate analyses were used. Results: 92% of
patients were classified as moderately to physically active in daily life.
During hospitalization, patients were inactive during 90% ± 5% of time. There
was no association with HAP score and acelerometry.
10.5% of patients developed PPC. Being physically active in daily life and
during hospitalization have a protective effect against PPC. Our results show
that the physical activity behavior in hospital do not reflect the daily life
even in patients not restricted to bed and on preoperative period, patients
physically actives on daily life and during hospitalization present less chance
to develop PPC after abdominal surgery.
Keywords: surgery, physical activity, postoperative complication, pneumonia,
accelerometry, hospitalization.
Resumo
O nível de atividade
física e o condicionamento físico parecem estar relacionados ao risco cirúrgico
pulmonar em cirurgias torácicas e cardíacas; no entanto, na cirurgia abdominal,
essa relação não é clara. Objetivo: Comparar o nível de atividade física na
vida diária e durante a hospitalização antes da cirurgia entre pacientes que
desenvolveram e que não desenvolveram complicações pulmonares pós-operatórias
(CPP) após cirurgia abdominal e relacionar esses desfechos. Métodos: Esta
coorte prospectiva recrutou 191 pacientes hospitalizados não restritos ao leito
e candidatos a cirurgia abdominal (52 ± 14 anos; IMC = 29 ± 11 kg/m2;
VEF1 = 98 ± 19% do predito; CVF = 96 ± 16% do predito). Duas ferramentas
diferentes relacionadas a dois momentos distintos foram utilizadas para avaliar
o nível no pré-operatório de atividade física. Primeiro, para avaliar o nível
de atividade física da vida diária, o questionário Perfil de Atividade Humana
(PAH) foi aplicado a todos os pacientes. O PAH possui 94 perguntas sobre a
execução de atividades gradualmente mais intensas. O PAH classifica o paciente
como inativo (<54 pontos), moderadamente ativo (54 a 73 pontos) e ativo
(>73 pontos). Segundo, a acelerometria
foi realizada durante 4 dias consecutivos para avaliar o tempo de atividade
durante a hospitalização. As CPP (pneumonia, atelectasia ou hipoxemia grave)
foram verificadas até a alta. Análises multivariadas foram utilizadas.
Resultados: 92% dos pacientes foram classificados como moderados a fisicamente
ativos na vida diária. Durante a hospitalização, os pacientes ficaram inativos
em 90% ± 5% do tempo. Não houve associação com escore do PAH e acelerometria. Cerca de 10,5% dos pacientes desenvolveram
CPP. Ser fisicamente ativo na vida diária e durante a hospitalização tem um
efeito protetor contra CPP (Odds ratio
[OR] = 0,69, IC 95% 0,01-0,93; OR=0,61, IC 95% 0,12-0,87, respectivamente).
Nossos resultados mostram que o comportamento da atividade física no hospital
não reflete o da vida diária, mesmo em pacientes não restritos ao leito e no
período pré-operatório, e os pacientes ativos fisicamente na vida diária e
durante a internação apresentam menor chance de desenvolver CPP após cirurgia
abdominal.
Palavras-chave: cirurgia, atividade
física, complicação pós-operatória, pneumonia, acelerometria,
hospitalização.
Introduction
Postoperative pulmonary complications (PPC) are frequent after major
surgeries [1] and increase the morbidity and mortality risks and the length of
hospital stay [2]. Clinical and surgical aspects are involved in the risk of
development of PPC as chronic respiratory diseases, aged and obesity [3].
Recently, the poor exercise tolerance has been also considerate as a risk
factor for developing of postoperative complications after cardiothoracic [4,5]
and non-cardiothoracic surgeries [6,7]. Probable, the relation between the
exercise tolerance and development of PPC is associated with physiologic
reserve and the capacity of recovery after a large trauma expected in major
surgeries [4].
The patients’ exercise tolerance reflects the daily life physical activity
behavior [8]. Patients with poor exercise tolerance, especially those with
chronic respiratory diseases, frequent present the harms from a sedentary
lifestyle as the early development of other chronic diseases, obesity, deficit
of oxygen transport and impaired functionality [9]. In surgical population,
Cook et al. observed that patients with poor exercise tolerance had presented
higher risk for complications and longer length of hospital stay after cardiac
surgery [10]. On the other hand, some studies have showed that preoperative
physical activities programs for vulnerable patients (older, oncologic,
abnormal lung function and with cardiac diseases) seems to improve their
functional status before surgery and accelerate their functional recovery and hospital
discharge after surgery) [11,12]. However, the evidences that physical activity
programs decrease the incidence of PPC after major surgeries stills weak
[11,12].
Considering that the preoperative hospitalization for finish the exams
and preparation for surgery increases the time in inactivity impairing the
muscle strength [13], the nutritional status [14] and the functionality [13]
and that these are factors associated with PPC [14], it is possible to admit
the hypothesis that physical activity behavior before and during
hospitalization can be related with PPC.
Objective
To compare the physical activity level in daily life and during
hospitalization before surgery between patients who developed and who did not
develop PPC after abdominal surgery and to relate to this outcome.
Methods
Design
Two hundred twelve consecutive candidates for elective abdominal surgery
were enrolled for this prospective cohort study in a University hospital. The
exclusion criteria adopted were: restriction to bed,
refuse to wear the accelerometer over 4 days, hospital discharge before
surgery, undergoing mechanical ventilation longer than 48h after surgery and
reoperation. The Ethics Committee of the Clinics Hospital, University of São
Paulo approved this protocol study (CAAE: 06324412.9.0000.0068).
Setting
Hospital of Clinics, School of Medicine, University of Sao Paulo, Sao
Paulo, Brazil
Experimental
design
All eligible candidates for surgery were invited to participate of this
study. After they had signed the consent forms, the patients were assessed for
anthropometric characteristics, medical history, serum albumin level, lung
function, muscle strength, resting energy expenditure, the physical activity
level on daily life and during hospitalization before surgery. After surgery,
all patients received standard medical and physiotherapist care and they were
followed for PPC recorder until the hospital discharge.
Assessments
Clinical history: data about comorbidities, smoking and drinking habits
were collected.
Serum albumin level: was collected at baseline.
The critical level for poor nutritional status was set at 3.5 dl/g [15].
Lung function: Spirometry (Spirobank II, MIR,
Italy) was performed according to the guidelines [16]. The relative values were
expressed in the percentage of prediction for Brazilian normality [17]. The
following variables were considerate: forced vital capacity (FVC), forced
expiratory volume in the first second (FEV1).
Respiratory muscle strength: Maximal inspiratory pressure and maximal
expiratory pressure indicate the muscle respiratory strength and were measured
as previously described (M120, GlobalMed, Brazil)
[18]. The best value from three acceptable maneuvers (variation <10%) was recorded.
Peripheral muscle strength: Skeletal muscle strength of the dominant
hand was measured by a dynamometer (Crown Manual, Filizola,
Brazil), with patient in sit position and elbow flexed at 90 degrees. The best
value from three acceptable maneuvers (variation <10%) was recorded.
Resting energy expenditure: This variable was assessed by
indirect-calorimetry (Metacheck, Korr,
USA) and reflect the basal metabolic rate. All patients had fasted for four
hours and stayed lying down during the measurement at rest. The gas analyzer
was connected to the patient by a mask and was calibrated following
recommendation of the manufacturer before each test. The amounts of oxygen and
carbon dioxide were collected breath by breath by the calorimeter for 10
minutes with the patient lying supine. The equipment uses the Harris-Benedict
equation to calculate the estimate of calories spend for 24 hours [19].
Physical activity level: Assessed referring for two distinct moments.
On
daily life: was assessed via Human Profile Activity (HAP). It is a questionnaire
containing 94 items that measures the energy expended in daily activities and
fitness [20]. The questions do not address a specific point in time, and the
patient responses concerning the opportunity / chance to perform a given
activity are that he / she is able to do it, is no longer able to do it or
never did it. The overall score constantly increases and ranges from 0 to 94
[21]. The adjusted score was used, given by the more intense activity that the
patient still engages in subtracted from the number of activities he / she
stopped performing. Activities never performed were not considered in the final
score [20]. The classification of the physical activity level is determined as
low (inactive) if the score is less than or equal to 53 points, moderate
(moderately active) if the score is between 54 and 73 points and high (active)
for a score of 74 points or more [21].
During
hospitalization: was assessed via accelerometer (Actigraph
GTX3, Actigraph, USA) installed on the patient’s
waist using a stretchable elastic band and maintained for four consecutive
days, as recommended by the manufacturer, starting until 24 hour after
admission. The device is waterproof and therefore the patient does not need to
remove it at any time. The device measures the acceleration in three orthogonal
planes (vertical, medial-lateral and antero-posterior) and is separately valid
for each of the three axes of acceleration [22]. After the results of the
activities are captured, the software can infer the caloric expenditure during
the performance of daily living activities of the patients monitored [22]. In
addition, the accelerometer quantifies the time that the patient spends at each
level of physical activity. Inactivity, which is the expected predominant level
of physical activity among hospitalized patients, is determined as zero to 199
movements per minute [22]. The mean values of the four sampling days were used.
Postoperative
pulmonary complications: The following PPC
were considered: atelectasis with clinical consequences [23], hypoxemia with
oxygen saturation <85% and need of supplemental O2 [24] and pneumonia [25].
A physician who was blinded to preoperative assessment results performed the
diagnosis of PPC. If any complication was diagnosed, the patient received the
proper treatment according to the clinical criteria.
Statistical
analysis
Sample size was calculated considering a difference of 10% on incidence
of PPC in active and inactive patients, power of 0.80 and p<0.05 [2]. A
sample of 107 patients would be necessary.
Data underwent descriptive analyses. The normality was tested by
Kolmogorov-Smirnov. Spearman’s correlation was used to test association between
HAP adjusted score and variables from accelerometry as well as calorimetry and
variables from muscle strength and HAP points. T test, Mann-Whitney and
chi-square tests were used to compare the groups with and without PPC,
depending on data distribution. Models of multiple logistic regression analysis
were tested for predicting PPC using as independent variables: age, BMI,
presence of comorbidity (yes or not), presence of cancer (yes or not), smoker
(yes or not), alcoholic (yes or not), serum albumin, points on HAP, scoring as
inactivity or active on HAP, percentage of time in activity or in inactivity
during hospitalization and muscle strength. Univariate analysis were performed to calculate odds ratio. The level of
significance was set at 5%. The software SigmaPlot
12.1 (San Jose, USA) was used.
Results
Of 212 patients assessed at baseline, 191 underwent surgery and 21 were
excluded (15 for cancelled surgeries and 6 for clinical complications before
surgery). All presented data are from 191 patients who complete the study. The
demographic, anthropometric, lung function, clinical characteristics and muscle
strength of 191 patients assessed are in Table I.
The physical activity level in daily life and during hospitalization of
candidates for surgery are in Table II. On daily life, 92% patients were
considerate moderately to physically actives. During hospitalization, patients
spent 10.4% of total time being actives independent of the intensity of the
activity (Table II).
There was no correlation between points obtained from HAP questionnaire
relative to daily life and variables from accelerometer during hospitalization
on preoperative period (p>0.05) (Table III).
There was positive correlation between resting energy expenditure
assessed indirect calorimetry and daily life physical activity level obtained
from HAP questionnaire and muscle strength assessed in the first 24h after
hospitalization, on preoperative period (Table IV).
The average of surgical duration was 282.50 ± 92.72 minutes and 46%
(n=88) of surgeries was via laparoscopic. The procedure carried out were: 42
(22%) rectosigmoidectomy/colectomy, 40 (21%)
gastrectomy, 29 (15%) bariatric surgery, 25 (13%) esophagectomy, 24 (13%)
cholecystectomy, 15 (8%) hiatoplasty, 13 (7%) hepatectomy and 3 (2%)
pancreatectomy.
After surgery, the incidence of pulmonary complications was 10.5%
(n=20), being 18 pneumonia and 2 atelectasis with clinical repercussion.
Observing the group that developed PPC, they had higher age, number of smokers
and alcoholics, ASA score classification and surgical duration as well as lower
predict value of FEV1 than the group that did not developed PPC (Table V). We
did not observe difference in physical activity level before and during
hospitalization or in muscle strength (Table V) between groups.
In regression models, age and being alcoholic were independent predictor
factor for PPC (R2 = 0.30). On the other hand, the physical activity in daily
life (assessed by HAP questionnaire) (Odds ratio = 0.69, 95% IC 0.01 to 0.93)
and the percentage of time in activity, independent of the intensity of the
activity, during hospitalization (Odds ratio = 0.61, 95% IC 0.12 to 0.87) had a
protective effect against postoperative pulmonary complications, as
demonstrated in follow equation:
PPC=3.194
- (3.335 * % of time in activity) - (1.878* physically active by HAP)
Table
I - Characteristics of assessed patients (n = 191).
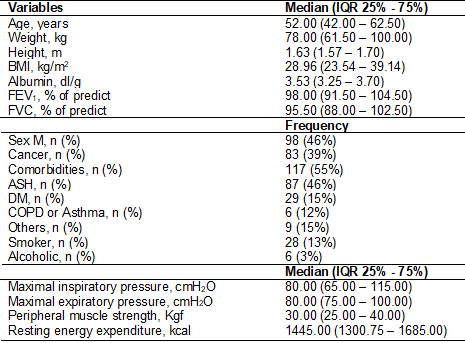
Data
are presented as median (IQR=interquartile range 25% – 75%) and frequency.
BMI=body mass index; M=male; n=absolute number FEV1=forced expiratory volume in
the 1st. second; FVC=forced vital capacity; % of predict for Brazilian
population16; ASH = arterial systemic hypertension; DM=diabetes mellitus;
COPD=chronic obstructive pulmonary disease; cmH2O=centimeter of water; Kgf=kilogram force; kcal=kilocalorie.
Table
II - Physical activity behaviour
(n=191).
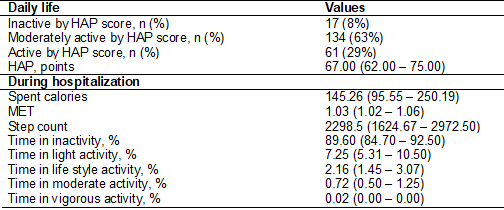
Data
are presented in median (IQR=interquartile range 25% – 75%) and in frequency.
Physical activity behavior during hospitalization was assessed by accelerometry
before surgery. HAP=Human Activity Profile; MET=metabolic equivalent;
%=percentage of total time of accelerometry.
Table
III - Correlation between physical activity in daily
life and during hospitalization (n=191).
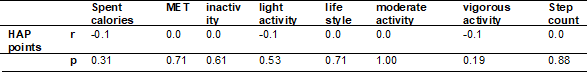
HAP
= Human Activity Profile points from adjusted score; r = correlation factor;
MET = metabolic equivalent.
Table
IV - Correlation among resting energy expenditure,
daily life physical activity level and muscle strength (n=191).
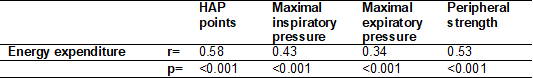
HAP=Human
Activity Profile points from adjusted score; r=correlation factor. p value from
Spearman’s correlation test.
Table
V - Comparison between patients with and without PPC
after elective abdominal surgery (n = 191).
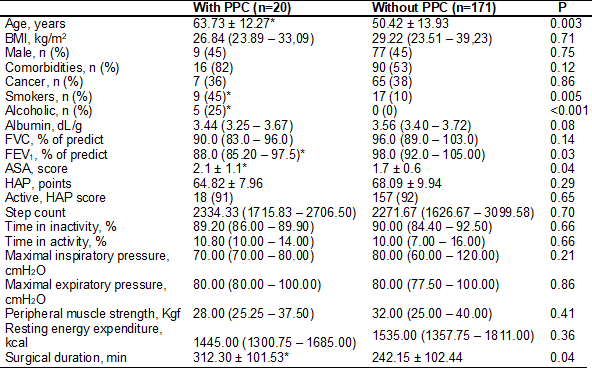
Data
are presented as median (IQR=interquartile range 25% – 75%), frequency and mean
± standard deviation. BMI=body mass index; n=absolute number; PPC=postoperative
pulmonary complication; FVC=forced vital capacity; FEV1=forced expiratory
volume in the 1st. second; ASA=American Society of Anesthesiology Index;
cmH2O=centimeter of water; Kgf=kilogram force;
min=minutes; kcal=kilocalorie; PPC=postoperative pulmonary complications;
p<0.05 value from t test or Mann-Whitney depend on continuous data
distribution or chi-square for categorical data.
Discussion
This prospective cohort aimed to verify if the physical activity
behavior on daily life and during hospitalization influence the development of
PPC. Our results show that being physically active in daily life and during
hospitalization on preoperative period have a protective effect against
pulmonary complications after elective abdominal surgery. Besides, the
patients’ daily life physical behavior is not transposed to inside the hospital
even on preoperative period of elective surgeries and without bed rest need. In
our knowledge, it is the first time that this association is reported.
The most part of assessed patients was classified as moderate to
physically active on daily life. This good functional capacity was reflected by
the preserved overall muscle strength, basal metabolic rate and nutritional
status early hospitalization. Previous studies also observed the great
functional capacity of candidates for elective abdominal surgery [2,25],
however they could not associate this variable with PPC, probable because all
patients presented high performance on applied tests, making it difficult to
differentiate patients with and without risk of PPC. Before these previous
studies reports, a new tool for surgical risk assessment was chosen, the HAP questionnaire.
This questionnaire includes daily life activities ranging from very easy to
very strenuous, with good properties of measurement [19], and it has been
widely used in healthy and populations with chronic diseases however no in
surgical population. The questions involve self-care activities, work, social
activities and exercises, and activities that require the use of muscle groups
of the hands, legs, trunk and use of wheelchairs [19]. Obviously, the use of an
instrument that objectively assess the level of physical activity seems to be
more attractive than applying a questionnaire, but, in clinical practice,
devices as pedometer or accelerometer are not cheap, requires consecutive days
of assessment and at least two visits at hospital or clinics, making it
difficult to use for surgical risk assessment out of protocol studies.
Inside the hospital, previously actives patients adopted a sedentary
behavior with no correlation with their daily life behavior, and it is related
to development of PPC. Our hypothesis is that the hospital structure, the lack
of information and the poor stimulus from health care staff are the most
important factors related to this change. Previous studies have showed that
hospitalization seems to be associated with impairments in functionality,
independency and muscle strength [13,26,27], probable because of long time in
inactivity [28]. This result from hospitalization could be partially
responsible for older, more obstructive, smokers, alcoholic and patients with
high surgical risk present more PPC after abdominal surgery [13,28].
The incidence of PPC observed was 10.5% which is similar with the
literature [2,14]. Pneumonia was the most frequent complication recorded in our
population. Santos et al. observed that when walking is also used to treat
patients undergoing thoracic surgery, the rate of pneumonia decreases [29]. The
association among postoperative pneumonia and elderly, alcoholics, smokers and
low FEV1 was previously descripted. The impairment of muscle strength and
immunity capacity age-related is related to loss of cough potency and higher
incidences of pneumonia [2,3,14]. The smoking habit increases mucus production,
impairs clearing of secretions, leading to sputum retention favoring the
development of pneumonia [30]. While, the alcoholic patients showed
immunological modifications as increased levels of IL-10, suppression of the
IL-6/IL-10 ratio and hypercortisolism immediately after surgery that were
associated with a postoperative pneumonia [31,32]. Often, smoking and drink
habits are associated with a sedentary behavior [33], so our hypothesis is that
these patients developed more PPC because they had unhealthy lifestyles.
The strong points of this study were the use of a simple questionnaire and
the accelerometer to assess candidates’ physical activity behavior before
abdominal surgery. Our results show that patients able to upstairs 50 steps or
walking 2 miles into 1 hour or swimming 25 meters (related to 74 points on HAP)
have 31% less change of developed PPC after abdominal surgery. In the other
hand, if during hospitalization waiting for surgery, the patients were able to
walk and do not spend most part of time sitting or lying down, they have 39%
less chance to developed PPC. Often, candidates for elective abdominal surgery
are not vulnerable patients compared to patients with lung or cardiac diseases,
however presented higher incidence of pulmonary complications, and simple
orientations from health care staff can be enough to prevent PPC. Other
populations, as candidate for thoracic and cardiac surgeries, can need of more
advantage preoperative fitness programs for prevent PPC, but it does not seem
to be the case of candidates for abdominal surgery.
This study has two important limitations. The impact of hospitalization
on muscle strength and this association with development of PPC were not
assessed, and the accelerometry was not performed before hospitalization;
however, the use of a questionnaire to assess the physical activity level
showed to be enough and it can expanding the clinical utility and applicability
of our results.
Conclusion
Our results show that the physical activity behavior in hospital does
not reflect the daily life even in patients not restricted to bed. However, if
patients perform simple activities as to upstairs, to walk or to swing before
hospitalization and still physically active during hospitalization their chance
to develop PPC after abdominal surgery decreases. Therefore, the health-care
staff has a very important role in this prevention.
References
- Carvalho CR, Paisani DM, Lunardi AC. Incentive spirometry in major surgeries: a systematic review. Braz J Phys Ther
2011;15(5):343-50. https://doi.org/10.1590/S1413-35552011005000025
- Paisani DM, Fiore Junior JF,
Lunardi AC, Colluci DB, Santoro IL, Carvalho CR, et
al. Preoperative 6-min walking distance does not predict pulmonary
complications in upper abdominal surgery. Respirology
2012;17(6):1013-7.
- Smetana
GW, Lawrence VA, Cornell JE, American College of P. Preoperative pulmonary risk
stratification for noncardiothoracic surgery:
systematic review for the American College of Physicians. Ann Intern Med
2006;144(8):581-95. https://doi.org/10.7326/0003-4819-144-8-200604180-00009
- Bayram
A, Candam T, Gebitekin C.
Preoperative maximal exercise oxygen consumption test predicts postoperative
pulmonary morbidity following major lung resection. Respirology
2007;12(4):505–10. https://doi.org/10.1111/j.1440-1843.2007.01097.x
- Arbane
G, Tropman D, Jackson D, Garrod R. Evaluation of an
early exercise intervention after thoracotomy for non-small cell lung cancer
(NSCLC), effects on quality of life, muscle strength and exercise tolerance: randomised controlled trial. Lung Cancer 2011;71:229-234.
https://doi.org/10.1016/j.lungcan.2010.04.025
- Smith
TB, Stonelli C, Purkayastha
S, Paraskevas P. Cardiopulmonary exercise testing as
a risk assessment method in non cardiopulmonary
surgery: a systematic review. Anaesthesia
2009;64(8):883-93. https://doi.org/10.1111/j.1365-2044.2009.05983.x
- Hightower
CE, Riedel BJ, Morris GS, Ensor JE Jr, Woodruff VD, et al. A pilot study evaluating predictors of postoperative outcomes after
major abdominal surgery: physiological capacity compared with the ASA physical
status classification system. Br J Anaesth
2010;104(4):465–71. https://doi.org/10.1093/bja/aeq034
- Troosters T, van der Molen
T, Polkey M, Rabinovich RA,
Vogiatzis I, Weisman I, et al. Improving physical
activity in COPD: towards a new paradigm. Respir Res 2013;14:115.
https://doi.org/10.1186/1465-9921-14-115
- Fagard RH, Cornelissen VA. Effect of
exercise on blood pressure control in hypertensive patients. Eur J Cardiovasc Prev Rehabil 2007;14(1):12-7.
https://doi.org/10.1097/HJR.0b013e3280128bbb
- Cook
JW, Pierson LM, Herbert WG, Norton HJ, Fedor JM, Kiebzak GM, et al. The influence of patient strength,
aerobic capacity and body composition upon outcomes after coronary artery
bypass grafting. Thorac Cardivasc
Surg. 2001;49(2):89-93. https://doi.org/ 10.1055/s-2001-11703
- Pouwels S, Willigendael
EM, van Sambeek MR, Nienhuijs
SW, Cuypers PW, Teijink JA.
Beneficial effects of pre-operative exercise therapy in patients with an
abdominal aortic aneurysm: a systematic review. Eur J Vasc
Endovasc Surg 2015;49(1):66-76. https://doi.org/
10.1016/j.ejvs.2014.10.008
- Hoogeboom TJ, Dronkers JJ, Hulzebos EH, van Meeteren NL. Merits of exercise therapy before and after
major surgery. Curr Opin Anaesthesiol 2014;27(2):161-6.
https://doi.org/10.1097/ACO.0000000000000062
- Suesada MM, Martins MA,
Carvalho CRF. Effect of short-term hospitalization on functional
capacity in patients not restricted to bed. Am J Phys
Med Rehabil 2007;86:455-62. https://doi.org/10.1097/PHM.0b013e31805b7566
- Lunardi AC, Miranda CS, Silva
KM, Cecconello I, Carvalho CR. Weakness of expiratory muscles and pulmonary complications in
malnourished patients undergoing upper abdominal surgery. Respirology
2012;17(1):108-13. https://doi.org/10.1111/j.1440-1843.2011.02049.x
- Laky
B, Janda M, Cleghorn G, Obermair
A. Comparison of different nutritional assessments and body-composition
measurements in detecting malnutrition among gynecologic cancer patients. Am J
Clin Nutr 2008;87(6):1678–85. https://doi.org/
10.1093/ajcn/87.6.1678
- Miller
MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of
spirometry. European Respiratory Journal
2005;26(2):319-38. https://doi.org/ 10.1183/09031936.05.00034805
- Pereira CAC.
Espirometria - Diretrizes para testes de função pulmonar 2002. J Bras Pneumol 2002;28:S1-S8.
- Volianitis S, McConnell AK, Jones
DA. Assessment of maximum inspiratory pressure. Prior submaximal respiratory
muscle activity ('warm-up') enhances maximum inspiratory activity and
attenuates the learning effect of repeated measurement. Respiration
2001;68(1):22-7. https://doi.org/ 10.1159/000050458
- Frankenfield DC, Muth ER, Rowe WA. The Harris-Benedict studies of human
basal metabolism: history and limitations. J Am Diet Assoc 1998;98(4):439-45.
- Davidson
M, Morton N. A systematic review of the human activity profile. Clin Rehabil 2007;21(2):151-62.
https://doi.org/10.1177/0269215506069475
- Fix
AJ, Daughton DM. Human activity profile –
professional manual. Nebraska: Psychological Assessment Resources; 1988.
- Freedson PS, Melanson E, Sirard J. Calibration
of the Computer Science and Applications, Inc. accelerometer. Med Sci Sports Exerc 1998;30(5):777-81.
https://doi.org/10.1097/00005768-199805000-00021
- Duggan
M, Kavanagh BP. Pulmonary atelectasis: a pathogenic perioperative entity.
Anesthesiology 2005;102(4):838-54.
- Kallstrom TJ. AARC Clinical
Practice Guideline: oxygen therapy for adults in the acute care facility-2002
revision & update. Respir Care 2002;47(6):717-20.
- Polverino E, Torres A.
Diagnostic strategies for healthcare-associated pneumonia. Semin
Respir Crit Care Med 2009;30(1):36-45.
https://doi.org/10.1055/s-0028-1119807
- Cheifetz O, Lucy SD, Overend TJ, Crowe J. The effect of abdominal support on
functional outcomes in patients following major abdominal surgery: a randomized
controlled trial. Physiother Can 2010;62(3):242-53.
- Brovold T, Skelton DA, Sylliaas H, Mowe M, Bergland A. Association between health-related quality of
life, physical fitness, and physical activity in older adults recently discharged
from hospital. J Aging Phys Act 2014;22(3):405-13.
- Coker
RH, Hays NP, Williams RH, Wolfe RR, Evans WJ. Bed rest promotes reductions in
walking speed, functional parameters, and aerobic fitness in older, healthy
adults. J Gerontol A Biol Sci Med Sci
2015;70(1):91-6. https://doi.org/ 10.1093/gerona/glu123
- Dos Santos EDC, Silva JS, Assis Filho MTT,
Vidal MB, Monte MC, Lunardi AC. Adding positive airway pressure to mobilisation
and respiratory techniques hastens pleural drainage: a randomised
trial. J Physiother 2020;66(1):19-26.
- Covinsky KE, Pierluissi E, Johnston CB. Hospitalization-associated
disability: "She was probably able to ambulate, but I'm not sure".
JAMA 2011;306(16):1782-93.
- Katznelson
R, Beattie WS. Perioperative smoking risk. Anesthesiology 2011;114(4):734-6.
https://doi.org/10.1097/ALN.0b013e318210fedc
- Sander
M, Irwin M, Sinha P, Naumann E, Kox WJ, Spies CD.
Suppression of interleukin-6 to interleukin-10 ratio in chronic alcoholics:
association with postoperative infections. Intensive Care Med
2002;28(3):285-92. https://doi.org/10.1007/s00134-001-1199-9
- Zhu
S, St-Onge MP, Heshka S, Heymsfield
SB. Lifestyle behaviors associated with lower risk of having the metabolic
syndrome. Metabolism 2004;53(11):1503-11.
https://doi.org/10.1016/j.metabol.2004.04.017