REVIEW
Physiotherapeutic resources
in vaginismus
Recursos
fisioterapêuticos no vaginismo
Nathália Torres Levandoski*, Magda Patrícia Furlanetto**
*Undergraduate
student in Physiotherapy at Centro Universitário
Ritter dos Reis – UniRitter, **Adviser, teacher of
the Discipline of Urogenital Physiotherapy at Centro Universitário
Ritter dos Reis
Received
on: July 28, 2020; accepted on: September 29, 2020.
Corresponding author: Nathália Torres Levandoski, Rua Coronel Claudino, Cristal, 91910-670 Porto
Alegre RS
Nathália Torres Levandoski: nathilevandoski@gmail.com
Magda Patrícia Furlanetto: magdafurlanetto@hotmail.com
Abstract
Vaginismus
consists of involuntary spasms in the external musculature of the vagina, the
etiology of which is still unknown, but there are cases of biopsychosocial
factors such as sexual abuse, strict sex, education, emotional trauma,
religious beliefs, low-quality sexual relations, fear of sex, or even changes
of ostemioarticular origin, can lead to this
condition, making vaginal penetration impossible during sexual intercourse,
gynecological exams or use of tampons. Objective: To highlight as physical therapy
practices, their validation for the treatment of vaginismus and to verify the
effectiveness of the analyzed practices. Methods: Systematic literature review
carried out through digital bibliographic research on scientific articles
published in electronic and electronic journals, randomized clinical trials,
with no period between the years 2010 to 2020, in the electronic databases
PubMed, Bireme and PEDro. Results: There was no great
variability in the resources used and the studies showed positive and similar
results. Conclusion: Physical therapy proved to be beneficial for cases of
vaginismus, with the use of functional electrical stimulation (FES) in an
analogue way, pelvic floor muscle relaxation exercises, local desensitization
performed with vaginal dilator and massage. However, more research is needed,
considering the moderate methodological scores found in the studies analyzed.
Keywords: vaginismus, physical therapy, rehabilitation.
Resumo
Vaginismo consiste em
espasmos involuntários na musculatura do terço externo da vagina, com etiologia
ainda desconhecida, mas há evidências de que fatores biopsicossociais como
abuso sexual, sexo estrito, educação, trauma emocional, crenças religiosas,
relações sexuais de baixa qualidade, medo do sexo, ou mesmo alterações de
origem osteomioarticular, podem acarretar nesta
condição, impossibilitando a penetração vaginal em relações sexuais, exames
ginecológicos ou no uso de absorventes internos. Objetivo: Evidenciar as
práticas fisioterapêuticas, sua validação para o tratamento do vaginismo e
verificar a eficácia das práticas analisadas. Material e métodos: Revisão
sistemática de literatura realizada através de busca bibliográfica digital em
artigos científicos publicados em revistas impressas e eletrônicas, ensaios
clínicos randomizados, no período compreendido entre os anos de 2010 a março de
2020, nas bases de dados eletrônicas Pubmed, Bireme e
Pedro. Resultados: Não houve grande variabilidade dos recursos utilizados e os
estudos apresentaram resultados positivos e semelhantes. Conclusão: A
fisioterapia mostrou-se benéfica para os casos de vaginismo, com a utilização
de estimulação elétrica funcional (FES) de forma analgésica, exercícios de
relaxamento da musculatura do assoalho pélvico, dessensibilização local realizada
com dilatador vaginal e massagem. No entanto, mais pesquisas são necessárias,
tendo em vista os escores metodológicos moderados encontrados nos estudos
analisados.
Palavras-chave: vaginismo,
fisioterapia, reabilitação.
Introduction
Female sexual dysfunctions (FSD) are conditions resulting from several
biological, psychological, social and cultural factors and it is estimated that
they are present in about 20 to 73% of women in the world. They encompass both
disturbances of desire, as well as psychoanatomophysiological
changes that characterize the sexual response, causing distress and
interpersonal difficulties [1]. According to the expanded concept of health,
they constitute a public health problem, an aggravation to the quality of life
and need the attention of multidisciplinary teams [2].
Among FSD, vaginismus is classified as a painful sexual disorder, with a
prevalence of 5 to 17% of the female population with an active sex life [3]. In
Brazil, about 2 in every 1000 women have this condition [4]. The provided data
may change, considering the profile of the accommodations, which may show shame
and embarrassment due to the condition and, consequently, end up not seeking
professional help or omitting their information [3,4].
Vaginismus consists of involuntary spasms of the pelvic muscles, which
have no external effects of the vagina associated with fear and/or pain [5].
There are divergences in the literature regarding these spasms being chronic or
whether they occur only in the presence of something considered as a threat.
The etiology is still unknown [6], but there are factors that cause
biopsychosocial that can be affected in this condition, such as sexual abuse,
strict sex, education, physical or emotional trauma, low quality sexual, religious
beliefs, or even fear of sexual intercourse for the first time [7]. In
addition, a therapy for gynecological cancer may be involved in genetics, as it
causes fibrosis and atrophy of the genital tract due to injury and
chemotherapy, thus hindering lubrication and penetration [8].
These physiological reactions cause distressed recurrent and inability
to perform any vaginal penetration [9], whether in sexual relations,
gynecological exams or in the use of tampons. The manifestations occur with
variations in severity and, thus, vaginismus can be classified as primary, when
the woman has never had sexual intercourse without pain and secondary, when the
woman has had any previous pain-free experience. It can also be classified as
global, when contractions occur regardless of partner and/or circumstances, and
situational, when contractions occur only with certain partners and/or specific
circumstances [7].
Among the forms of diagnosis found in the literature, the gynecological
exam is the most used, but due to the peculiarity of the condition, care in the
performance must be judicious and the exam should only be performed after the
patient is reassured so as not to raise the level of trauma of this woman [10].
Tools such as biofeedback, which enable the analysis of muscle contractions,
and the application of the Female Sexual Function Index (FSFI) questionnaire
can also be used as an aid to diagnosis [6]. In contrast, the diagnostic
approach is based on persistent or recurrent difficulties in vaginal penetration
during sexual intercourse, marked pelvic pain during intercourse or attempts at
penetration and fear in anticipation, and allows assessment as a disorder not
only sexual, but also as a behavioral problem [11].
Physical therapy applied in cases of vaginismus has as its main
objectives to develop awareness, control of the pelvic floor muscles (PFM),
restoration of function and mobility, as well as pain relief [10]. The
approaches consist of techniques such as biofeedback associated with surface
electromyography and PFM relaxation to help identify contractions and, thus,
promote greater muscle control [9]. Vaginal dilators for stretching the PFM
[12], gradual desensitization [13] for pain relief and myofascial release of
trigger points [14] have also been reported in the literature [12].
Considering the information provided, a physiotherapeutic approach is
essential for this dysfunction, due to the importance of the plurality of
techniques used for greater treatment effectiveness. In counterpart, the literature
has shown that there are no studies that validate these techniques. Thus, this
systematic review aims to highlight physical therapy practices found in the
literature for the treatment of vaginismus and to verify the practical
practices analyzed.
Methods
This study deals with a systematic literature review carried out from
March to June 2020, through digital bibliographic research in scientific
articles published in magazines and electronics, with no period between 2010
and 2020, in the databases Pubmed, Bireme and PEDro. Studies with the language of publication in
Portuguese and English were selected in different strategies to protect a
comprehensive search (Table I). Manual searches were also performed based on
the references of the included studies. The guiding question of this study was
to discover the effectiveness of physiotherapeutic resources in the treatment
of vaginismus. This question was able to generate descriptors related to the
population, type of intervention of interest, comparisons and outcomes.
Table
I - Boolean descriptors and operators used to search
databases.

The searches were carried out by two independent evaluators who selected
the potentially relevant studies from the titles and summaries of the results
obtained in the databases. When these sections did not provide enough
information to be included, the full text was verified. Subsequently, the same
reviewers independently evaluated the complete studies and made the selection
according to the eligibility criteria, that is, the use of a publication that
involved the performance of physical therapy in cases of vaginismus in the
research. Disagreeing cases were resolved by consensus. Authors, year of
publication, participants, type of intervention and results of the variables of
interest were obtained independently by the two reviewers, using a standardized
form. Data analysis was performed in a descriptive manner, proceeding to
categorize the data extracted into thematic groups based on the variables of
interest.
An evaluation of the quality of the studies was performed using the
Downs & Black scale [15] which was developed in order to fill gaps in the
evaluation of studies that are not randomized clinical trials. This scale
includes 5 sub-items related to: 1) how to report the results (if the
information presented in the study allows the reader to interpret the data and
results without bias), 2) external validity, 3) the cases, 4) the factors of
confusion, and 5) power of the study. To correspond to these sub-items, 27 are
listed, which, if the appraiser identifies them, will be scored with
"one" value. The absence of criteria corresponds to the evaluation of
"zero". It is allowed to apply aspects such as: if the hypotheses and
objectives are applied, if the measures are considered measures in the
introduction and methods section, if the individuals lost in the follow-up are
not reported, if the randomness of the sample is guaranteed, or anonymity of
the subjects, there is reference to statistical procedures, among others.
This scale is recognized as “methodologically strong” and is more
flexible than others, since it allows to evaluate in a credible way, a greater
range of types of study. It also has the advantage that it is possible to
evaluate and highlight potential strengths and weaknesses of the studies under
evaluation. Studies were considered methodologically strong with scores equal
to or greater than 80% of the maximum score, scores between 60 and 80% as
moderate, and those below 60% were considered methodologically unsatisfactory
(weak) [16].
Results
In the initial search, 124 references were found in total, of which 1
was found through manual search in the studies included through the initial
selection. Of these, 97 articles were found in the Bireme database, with 93
articles not being applied to the object of analysis. In Pubmed,
25 articles were found, where 22 did not apply to the object under analysis and
3 were duplicated. Only one article was found in the PEDro
database, but it was duplicated. Finally, 7 studies, after reading the titles,
abstracts and analytical reading of the articles, were selected as the object
of analysis, as they presented aspects that answered the guiding question. Upon
reading in full, four studies were removed, as they did not address the subject
in the desired manner, thus leaving 3 selected articles. Figure 1 represents
the reported research flowchart and the 3 selected studies, which consist of
randomized clinical trials.
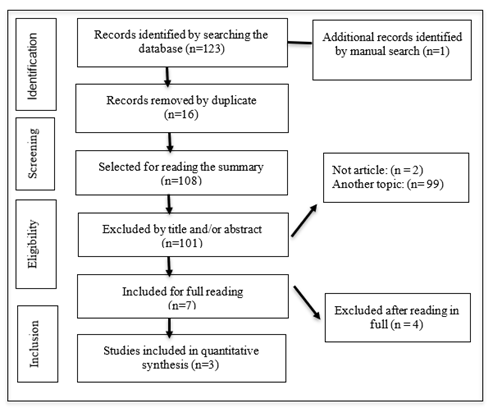
Figure
1 - Flowchart of study selection. Prisma, 2009 [17].
Characteristics
of included studies
Studies on the performance of physical therapy in vaginismus have been
found only in international publications. Treatments such as functional
electrical stimulation (FES) at analgesic frequencies, pelvic floor relaxation
exercises associated and not associated with infrared light and desensitization
[18], digital relaxation and vaginal dilators [19,20] were addressed. Table II
presents the selected studies characterized by author, year and country, type
of study, sample size, age and treatments.
Table
II - Bibliographic sources identified, type of study,
sample size, sample characteristic (age) and treatment addressed.
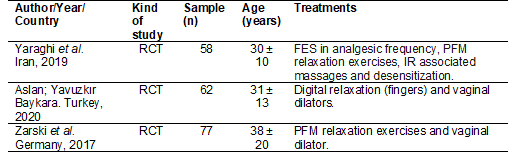
FES
= Functional Electrical Stimulation; IF = Light Infra-Red; PFM = Pelvic Floor
Muscles; RCT = Randomized Clinical Trials.
Study
bias risk assessment
About the scores obtained using the Downs and Black Methodological
Scale, studies obtained an average of 20 points (71%) considering the maximum
score of 28 possible. Among the methodological criteria that most failed,
alluded to is the absence of a control group, not description of the random
variability of the data of the main findings and not the attempt to blind
participants and measurers. Among the studies analyzed, all obtained scores
between 60 and 80% and were considered as moderate.

Graphic
1 - Percentage obtained through the Downs and Black
scale for the selected works.
Outcome
analysis
The results obtained in relation to the evaluation methods, intervention
groups, results and main conclusions are shown in Table III.
Chart
1 - Results obtained in relation to the evaluation
methods, groups, results and main conclusions. (see PDF annexed)
Discussion
Three randomized controlled trials were the object of this systematic
review, which, in at least one evaluated item, showed improvement in some
parameter evaluated after the use of some physical therapy resource. When
physical therapy intervention was compared with standard therapy or
non-intervention, it showed superior results. The studies reported the
physiotherapeutic performance with FES in analgesic frequency, PFM relaxation
exercises, massages associated with IR light and use of vaginal dilators. In
terms of evaluation, the FSFI sexual function evaluation questionnaire was used
in all studies. Personal reports, questionnaires about fear of sexual relations
and satisfaction questionnaire appeared on time in only one study.
In methodological terms, according to the Check list Downs and Black,
the evaluated articles presented results with moderate scores. Essential
criteria for the scientific request for studies have not been widely met, which
may put the reliability of studies in doubt. Among the missing quality
indicators, there is unanimous emphasis on the non-attempt to blind
participants and measurers and, in the majority, the absence of a control group
and the lack of description of the random variability of the data.
Among the studies presented, all used techniques to promote
desensitization of the pelvic region. Yaraghi et
al. [18], however, did not specify which technique was used and two authors
of this review [19,20] used the vaginal dilator. Aslan et al. [19]
compared the effectiveness of the instrument with the technique performed
manually. Generally, treatment begins with genital observation using a mirror,
progressing to genital touch [21] and the use of a dilator in a progressive
manner guided by a physiotherapist to ensure a safe and effective treatment
[12]. These studies have shown the effectiveness of this method and, when
compared with the manual technique, it has proved to be advantageous in
relation to the outcome of desire and orgasm. Ratifying these findings, this
technique was considered effective for sexual satisfaction in the study
conducted by Franceschini, Scarlato,
Cisi [22]. However, it is worth emphasizing the
importance of understanding the etiology of the case before the treatment is
performed, given the nature of a psychological bias, this technique may lose
its purpose if used inappropriately [23]. In counterpart, Melnik
et al. [24] reported that desensitization performed systematically, that
is, with PFM relaxation techniques and gradual desensitization with dilators,
was not as effective as cognitive therapy and drug use.
Since PFM and sexual function are interconnected, since the muscles must
exercise their function in a healthy way for there to be a normal function
[25]. Yaraghi et al. [18], as well as Zarski et al. [20] used PFM relaxation exercises in
order to promote the reduction of muscle spasms present in the dysfunction and
presented positive results in relation to penetrative sexual intercourse. The
continuous contraction of the pelvic floor muscles often results in pain and
makes sexual intercourse impossible. It is essential to treat vaginismus techniques
that aim to reduce this condition and not only treat pain exclusively, since
they are the result of these spasms. However, for the use of exercises with the
objective of desensitization, this treatment does not have as effective results
as other techniques [24] and demonstrate the need for association with
analgesic techniques.
In the results of the Aslan study, Aslan et al. [19] showed
success in the treatment of vaginismus with electrostimulation (FES) used in
analgesic frequency, producing a defensive reflex as a mechanism against
nociception [26]. In this way, tolerance to touch was potentiated and,
subsequently, there was an improvement in sexual function allowing for a
satisfactory sexual relationship [27]. However, the relaxation techniques of
PFM and massage must be associated, as the mobilization of tissues causes heat
and helps in the organization of collagen and reduction of adhesions and can
relieve local pain [28]. This study, despite a moderate score, was the only one
to demonstrate a greater association of techniques in the treatment of
vaginismus with physical therapy techniques. With a focus on the complexity of
chronic pain within a biopsychosocial context, in 2018, a study conducted by
Kaiser et al. [29] showed positive results generating the recommendation
of multimodal therapies with the presence of physiotherapeutic techniques for
the treatment of chronic pain, with the aim of improvements in physical, mental
and social factors and having as parameters the intensity and frequency of
pain, physical activity, emotional well-being, satisfaction with social
activities, productivity, health-related quality of life and the patient's
perception of the achievement of the goals of the treatment.
Therefore, according to the results obtained in the present review, it
was possible to observe that there was a consensus on the physiotherapeutic
techniques used in the treatment of vaginismus, considering that the study
approaches are similar or complement each other and presented positive
outcomes. It was possible to verify the scarcity of investigations about this
dysfunction in the general field of health, as well as physical therapy and its
possible treatments, limiting this work and highlighting the need for further
research to identify the most appropriate physiotherapeutic treatments.
Conclusion
The main findings of the present study were the consensus of the studies
on physical therapy techniques used in the treatment of vaginismus and greater
effectiveness when the techniques were associated, showing improvements in
sexual function with the use of FES in analgesia parameters, PFM relaxation
exercises, local desensitization performed with vaginal dilator and massage.
Even if the present studies show positive and consensual results, there is
still a need for more studies in the area, in view of the moderate
methodological scores, the current scarcity of the literature in relation to
vaginismus and treatment methods.
References
- Holanda JBL, Abuchaim ESV, Coca KP, Abrão ACFV. Disfunção sexual e
fatores associados relatados no período pós-parto. Acta Paul Enferm 2014;27(6):573-8.
https://doi.org/10.1590/1982-0194201400093
- Prado DS, Mota VPLP,
Lima TIA. Prevalência de disfunção sexual em dois grupos de mulheres de
diferentes níveis socioeconômicos. Rev Bras Ginecol Obstet
2010;32(3):139-43. https://doi.org/10.1590/S0100-72032010000300007
- Maseroli E, Scavello
I, Cipriani S, Palma M, Fambrini
M, Corona G, et al. Psychobiological correlates of
vaginismus: an exploratory analysis. The Journal of Sexual Medicine
2017;14(11):1392-1402. https://doi.org/10.1016/j.jsxm.2017.09.015
- Lima MG, Silva MEA,
Souza TA, Souza LP. A episiotomia e o retorno à vida sexual pós-parto. Revista
Uningá 2013;16.
- Engman M, Wijma
K, Wijma B. Long-term coital behaviour
in women treated with cognitive behaviour therapy for
superficial coital pain and vaginismus. Cogn Behav Ther 2010;39(3):193-202.
https://doi.org/10.1080/16506070903571014
- Pacik PT. Understanding and treating
vaginismus: a multimodal approach. Int Urogynecol J
2014;25(12):1613-20. https://doi.org/10.1007/s00192-014-2421-y
- Souza
MCB, Gusmão MCG, Antunes RA, Souza MM, Rito ALS, Lira P, et al. Vaginismus in assisted
reproductive technology centers: an invisible population in need of care. JBRA
Assist Reprod 2018;22(1):35-41.
https://doi.org/10.5935/1518-0557.20180013
- Fleury
HJ, Abdo CHN. Female genital pain. Diagn Tratament
2013;18(3):124-7. https://doi.org/10.1590/S0100-72032006001200008
- Hope
ME, Farmer L, McAllister KF, Cumming GP. Vaginismus in peri- and postmenopausal
women: a pragmatic approach for general practitioners and gynaecologists.
Menopause Int 2010;16(2):68-73. https://doi.org/10.1258/mi.2010.010016
- Lahaie MA, Boyer SC, Amsel
R, Khalifé S, Binik YM.
Vaginismus: A Review of the literature on the classification/diagnosis,
etiology and treatment. Womens Health (Lond) 2010;6(5):705-19. https://doi.org/10.2217/whe.10.46
- Conforti C. Genito-Pelvic
Pain/Penetration Disorder (GPPPD): An overview of current terminology,
etiology, and treatment. Women's Health 2017;7.
https://doi.org/10.1055/s-0038-1675805
- Macey
K, Gregory A, Nunns D, Nair R. Women’s experiences of
using vaginal trainers (dilators) to treat vaginal penetration difficulties
diagnosed as vaginismus: a qualitative interview study. BMC Women's Health
2015;15. https://doi.org/10.1186/s12905-015-0201-6
- Fageeh WMK. Different treatment
modalities for refractory vaginismus in Western Saudi Arabia. The Journal of
Sexual Medicine 2011;8:1735-9.
https://doi.org/10.1111/j.1743-6109.2011.02247.x
- Reissing ED, Armstrong HL,
Allen C. Pelvic floor physical therapy for lifelong vaginismus: a retrospective
chart review and interview study. J Sex Marital Ther 2013;39:306-20. https://doi.org/10.1080/0092623X.2012.697535
- Downs
S, Black N. The feasibility of creating a checklist for the assessment of the
methodological quality both of randomised and non-randomised studies of health care inter-ventions.
J Epidemiol Community Health 1998;52(6):377-84.
https://doi.org/10.1136/jech.52.6.377
- Bento T. Revisões
sistemáticas em desporto e saúde: Orientações para o planeamento, elaboração,
redação e avaliação. Motricidade 2014;10:107-23.
https://doi.org/10.6063/motricidade.10(2).3699
- Itens P, Revis R, Uma P. Principais itens para relatar revisões
sistemáticas e meta-análises: A recomendação PRISMA. Epidemiol
e Serviços Saúde 2015;24(2):335–42.
https://doi.org/10.5123/S1679-49742015000200017
- Yaraghi M, Ghazizadeh
S, Mohammadi F, Ashtiani EM, Bakhtiyari M, Mareshi SM, et al. Comparing
the effectiveness of functional electrical stimulation via sexual
cognitive/behavioral therapy of pelvic floor muscles versus local injection of
botulinum toxin on the sexual functioning of patients with primary vaginismus:
a randomized clinical trial. Int Urogynecol J 2019;30:1821-8. https://doi.org/10.1007/s00192-018-3836-7
- Aslan
M, Yavuzkir S, Baykara S.
Is "dilator use" more effective than "finger use" in
exposure therapy in vaginismus treatment? J Sex Marital Ther
2020;46:354-60.
https://doi.org/10.1080/0092623X.2020.1716907
- Zarski AC, Berking
M, Fackiner C, Rosenau C, Elbert DD. Internet-based
guided self-help for vaginal penetration difficulties: results of a randomized
controlled pilot trial. J Sex Med 2017;14:238-54.
https://doi.org/10.1016/j.jsxm.2016.12.232
- Rosenbaum
T. Addressing anxiety in vivo in physiotherapy treatment of women with severe
vaginismus: a clinical approach. J Sex Marital Ther
2011;37(2):89-93. https://doi.org/10.1080/0092623X.2011.547340
- Franceschini J, Scarlato
A, Cisi MC. Fisioterapia nas principais disfunções sexuais
pós-tratamento do câncer do colo do útero: revisão bibliográfica. Rev Bras Cancerol
2010;56:501-6.
- Santos LMSS, Silva MRG,
Latorre GFS, Jorge LB. Tratamento da disfunção sexual
feminina através da utilização de dilatadores vaginais. Revista da AMRIGS 2019;63:85-88.
- Melnik T, Hawton
K, McGuire H. Interventions
for vaginismos. Cochrane Library 2012:1-32.
https://doi.org/10.1002/14651858.CD001760
- Piassarolli VP, Hardy E, Andrade NF, Ferreira NO, Osis
MSD. Pelvic floor muscle training in female sexual
dysfunctions. Rev Bras Ginecol Obstet 2010;32(5).
https://doi.org/10.1590/S0100-72032010000500006
- Lima RGR, Silva SLS,
Freire AB, Barbosa LMA. Tratamento fisioterapêutico nos transtornos sexuais
dolorosos femininos: revisão narrativa. Revista Eletrônica da Estácio Recife
2016;2(1).
- Wolpe RE, Toriy AM, Silva FP, Zomkowski K, Sperandio FF. Eletroterapia aplicada às disfunções sexuais
femininas: revisão sistemática. Revista Eletrônica da Estácio Recife 2015;22:87-92. https://doi.org/10.5935/0104-7795.20150017
- Batista MCS.
Fisioterapia como parte da equipe interdisciplinar no tratamento das disfunções
sexuais femininas. Diagn Tratamento 2017;22:83-87.
- Kaiser
U, Kopkow C, Deckert S,
Neustadt K, Jacobi L, Cameron P, et al. Developing a core outcome domain set to
assessing effectiveness of interdisciplinary multimodal pain therapy: the vapain consensus statement on core outcome domains. Pain 2018;159:673-83.
https://doi.org/10.1097/j.pain.0000000000001129