Fisioter
Bras 2021;22(1):37-48
doi: 10.33233/fb.v22i1.4387
ARTIGO ORIGINAL
Impact of two methods of pulmonary re-expansion in
patients undergoing bariatric surgery by videolaparoscopy
Impacto
de dois métodos de reexpansão pulmonar em pacientes
submetidos a cirurgia bariátrica por videolaparoscopia
Fabiana
Della Via, D.Sc.*, Admar Concon Filho**, Carolina Kosour, D.Sc.***, Carlos Eduardo Ferraresi
Andrade****, Emanuel Guedes****, Desanka Dragosavac, D.Sc.*
*Universidade
Estadual de Campinas, Campinas, SP, Brazil, **Serviço
de cirurgia, Hospital Galileo, Valinhos, SP, Brazil,
***Curso de Fisioterapia, Universidade Federal de Alfenas, Alfenas, MG, Brazil **** Serviço de Anestesiologia, Hospital Galileo,
Valinhos, SP, Brazil
Received:
October 30, 2020; accepted:
February 2, 2021.
Correspondence: Fabiana Della Via Rua Adelino Venturini, 83, Casa 6,
Jardim Lorena 13277630 Valinhos SP
Fabiana Della Via: fabianadv@yahoo.com.br
Admar Concon
Filho: conconaf@uol.com.br
Carolina Kosour: ckosour@fcm.unicamp.br
Carlos Eduardo Ferraresi Andrade:
ceedu@uol.com.br
Emanuel Guedes: ecrguedes@gmail.com
Desanka Dragosavac:
desankadragosavac@gmail.com
Abstract
Evaluating the impact of lung re-expansion methods on
the postoperative pulmonary function and respiratory complications such as
atelectasis, pneumonia and hypoxemia in videolaparoscopy-based bariatric surgery. Prospective
clinical study conducted with 105 patients randomly divided into three groups:
control (conventional postoperative physical therapy), recruitment
(intraoperative alveolar recruitment) and decompression (postoperative chest
compression and decompression maneuver). Spirometry, respiratory and
hemodynamic variables were analyzed. All groups have presented worsened values
in spirometry measurements within the postoperative period (p < 0.00) and
there was significant decrease in respiratory rates in comparison to the immediate
preoperative period (p = 0,01). Mean end-expiratory carbon dioxide pressure in
the recruitment group was higher than in the control in all assessed time
intervals (p = 0.03). Chest compression and decompression maneuver and alveolar
recruitment were beneficial to pulmonary function recovery. There were no
differences in postoperative pulmonary complications and function in the three
assessed groups, except for significant decrease in respiratory rates and in
the end-expiratory carbon dioxide pressure level in the recruitment group.
Keywords: bariatric surgery, pulmonary
atelectasis, Physical Therapy.
Resumo
Avaliar
o impacto de métodos de re-expansão pulmonar na
função pulmonar e incidência de complicações respiratórias como as
atelectasias, pneumonias e hipoxemia no pós-operatório de cirurgia bariátrica
por videolaparoscopia. Estudo clínico, prospectivo realizado com 105 pacientes,
randomizado em três grupos: grupo controle (fisioterapia convencional no
pós-operatório), grupo recrutamento (recrutamento alveolar no intraoperatório)
e grupo descompressão (manobra de compressão e descompressão torácica no
pós-operatório). Foram analisadas variáveis espirométricas,
respiratórias e hemodinâmicas. No pós-operatório todos os grupos apresentaram
piora nas medidas espirométricas (p < 0,00) e
redução significativa da frequência respiratória quando comparado o período pré e pós-operatório imediato em todos os grupos (p =
0,01). As médias de pressão expiratória final de gás carbônico no grupo
recrutamento foram maiores que no grupo controle em todos os intervalos de
tempos avaliados (p = 0,03). A manobra de compressão e descompressão torácica e
o recrutamento alveolar foram benéficos para a recuperação da função pulmonar.
Nos três grupos avaliados não houve diferença nas complicações e função
pulmonar no pós-operatório, exceto redução significativa da frequência
respiratória e da pressão expiratória final de dióxido de carbono no grupo
recrutamento alveolar.
Palavras-chave: cirurgia bariátrica; atelectasia
pulmonar; Fisioterapia.
Introduction
Bariatric
surgery is an effective method adopted to treat obese patients [1], but
patients face the risk of developing postoperative pulmonary complications such
as bronchospasm, respiratory failure, pneumonia, atelectasis and hypoxemia
[2,3], that mostly derive from the association between patients’ obesity and
intraoperative factors such as the use of anesthetics, neuromuscular blockers
and analgesics, prolonged surgical time, inadequate mechanical ventilation,
age, and postoperative pain [4,5].
According to Pazzianotto-Forti et al. [6], preoperative and
postoperative respiratory physical therapy is beneficial and essential to help
morbid obesity patients maintaining their pulmonary function and to prevent
pulmonary complications. Manual chest compression and decompression maneuver
(CCDM) is a physical therapy technique adopted to help opening collapsed
alveoli by both increasing the transpulmonary pressure gradient and guiding air
flow and volume to the airways to increase oxygenation [7].
Some ventilatory
strategies, such as alveolar recruitment maneuver (ARM) and protective
intraoperative ventilation with lower tidal volume and higher positive
end-expiratory pressure (PEEP) level [8,9] are used to improve pulmonary gas
exchange during, and after, anesthesia in patients subjected to bariatric
surgery [10,11,12,13].
Based on the
hypothesis of respiratory physical therapy improves the pulmonary function and
respiratory mechanics, the aim of the study was to evaluate the effects of ARM,
as well as of CCDM on pulmonary function recovery and on the incidence of
postoperative pulmonary complications in patients subjected to bariatric
surgery by video laparoscopy.
Methods
Prospective,
randomized, and quantitative research carried out at Galileo Hospital. The
research was approved by the Research Ethics Committee of Medical Sciences
School/UNICAMP-N. 392672. All participants have signed the Free Informed
Consent Form.
The study
included patients in the age group 18 to 59 years subjected to Roux-en-Y
gastric bypass surgery. Patients who required laparotomy intervention were
excluded from the study.
All pulmonary
function tests were following guidelines set by the American Thoracic Society
[12]. Spirometric measurements were performed in Contec™ Med SP10® Digital Spirometer calibrated for each
patient. The measurements were taken in the preoperative period, right after
the surgery, in the first and second postoperative days. The measured
parameters included forced expiratory volume in one second (FEV1), forced vital
capacity (FVC), maximal voluntary ventilation (VVM) and forced expiratory flow
at 25-75% of pulmonary volume (FEF25-75 %).
Randomization
was carried out after patients underwent a pre-operative evaluation. The
patients were randomly divided into three intervention groups by a draw using
sealed envelopes: control (CG) - patients subjected to conventional physical
therapy (CP); recruitment group (RG) - patients subjected to intraoperative
ARM; and decompression group (DG) - patients subjected CCDM in the
postoperative period.
All surgeries
were performed by the same professionals. The same anesthesia and protective
mechanical ventilation recommended in the Brazilian Guidelines for Mechanical
Ventilation [13] were applied to all groups. The volume-controlled mode was
applied to ventilation patients during anesthesia carried out with anesthetic
machine (Takaoka®).
Patients from
the all intervention groups were removed from bed and taken to armchair six hours
after surgery, and after 1 hour they were taken for a walk. Subsequently, they
were subjected to CP session, which consisted of 40 repetitions in load-free
incentive spirometer and 20 repetitions of breathing exercises.
Patients
belonging to the recruitment group (RG) were subjected to intraoperative ARM
after pneumoperitoneum deflation based on the protocol recommended by the
institution, as well as to CP. The volume-controlled mode was initially
adjusted to pressure-controlled ventilation. The initial control pressure was
set at 20 cmH2O, respiratory rate was adjusted to 10 cycles per
minute, PEEP was set at 5 cmH2O and the inspired oxygen fraction was
adjusted to 50%. This technique consisted of increasing PEEP and control
pressure to 20 and 40 cmH2O respectively, at most by the addition of
5 cmH2O every 2 minutes.
Besides
undergoing CP, patients in the decompression group (DG) were subjected to CCDM,
six hours after surgery. They were placed in dorsal decubitus and anatomical
position with their heads elevated at 30° to enable 10 repetitions of CCDM in
each hemithorax within 10 consecutive breaths - this technique consists of
compressing patients’ chest at the final expiratory phase. Chest compression
was kept until the initial third of the inspiratory phase, when it was abruptly
released.
Statistical analysis
Sample size was
calculated based on a pilot study conducted with ten patients. ANOVA was
applied to repeated measurements to compare variables and time-periods between
groups at type I error equal to 5% (significance level) and type II error equal
to 20% (test power equal to 80%). At least 30 patients were gathered per group
during the trial.
Kruskal-Wallis
test was used to compare age, body mass index and surgery duration between
groups. Repeated measures ANOVA was applied to compare hemodynamics and
spirometry parameters and surgery duration between groups. Significance level
was set at 5%. The Statistical Analysis System (SAS) software for Windows,
version 9.3, was used to calculate the sample and in the statistical analyses.
Results
Two out of 107
patients were excluded from the research in the intraoperative period. One of
them had severe bronchospasm after anesthetic induction and the other one needed
surgery conversion into laparotomy due to technical difficulties. Thus, only
105 patients composed the cohort.
Based on the
comparison between groups, patients were homogeneous in factors age, sex, body
mass index (BMI) and comorbidity incidence. The most common comorbidities were
arterial hypertension 43.80%, metabolic syndrome 36.19% and diabetes mellitus
14.28% (Table I).
Table I - Demographic profile of the
overall population in the study

F =
female; BMI = Body Mass Index. Values were expressed as mean ± SD and
percentage
Based on the
analysis applied to the Torrington-Henderson scale criteria, all
patients presented minimal risk of developing respiratory complications. The
adopted protocols did not cause significant changes in patients’ peripheral
oxygen saturation, heart rate and mean arterial pressure.
Respiratory rate
analysis performed right after the surgery showed significantly lower values
than the ones observed in the preoperative period in all groups and evidenced
statistically significant difference between RG and DG; this variable presented
higher values in RG than in DG at all periods (p = 0.0152), as shown in graphic
1.
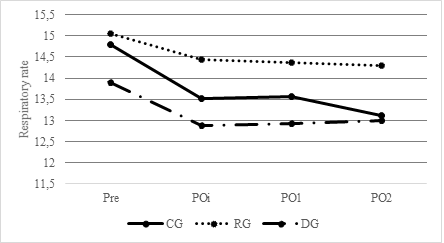
Pre = preoperative;
Poi = immediate postoperative period; PO1 = first postoperative day; PO2
= second postoperative day
Graphic 1 - Respiratory rate
Spirometry
variable comparisons in the postoperative period did not show statistically
significant differences between groups; however, all groups presented improved
values for all variables recorded between moments right after the surgery and
the second postoperative day (p < 0.0001), as shown in Table II.
Table II - Values recorded for
spirometry variables in the preoperative period (pre), after the surgery (POi), first (PO1) and second (PO2) postoperative
days

L =
liters; L/s = liters per second; L/min = liters per minute; % = percentage;
values were expressed as mean ± standard deviation. p = value compared with
times (preoperative period (pre), after the surgery (POi),
first (PO1) and second (PO2) postoperative days), **p = value
compared with the groups (control group (CG); recruitment group (RG) and
decompression group (DG))
There were
significant changes in end-expiratory carbon dioxide pressure (PETCO2)
between time intervals (p = 0.00) and between groups (p = 0.03). RG recorded
higher PETCO2 means than CG in all tested time-intervals, as shown
in graphic 2.

Pre =
before pneumoperitoneum; Pos-p = after pneumoperitoneum; Pos 24 = 24 minutes
after pneumoperitoneum; Pos 34 = 34 minutes after pneumoperitoneum; Pre-ext = before extubation
Graphic 2 - End-expiratory carbon dioxide
pressure at pre and postoperative alveolar recruitment
Mean
hospitalization time was 4.58 days. All patients were subjected to one-month
follow-up in the postoperative period. None of the groups presented
postoperative pulmonary complications such as atelectasis, pneumonia
and hypoxemia.
Discussion
There were no
significant differences in FVC, FEV1, FEF 25%-75% and MVV values in the
preoperative period between groups. This outcome can be explained by the
prevalence of patients with obesity grade II in the sample, unlike the sample assessed
by Paisani et al. [14], whose patients
presented mean BMI 50.4 kg/m2 and were categorized as super obese.
However, values recorded for spirometry variables have decreased in the three
postoperative periods. This result is like outcomes in the studies by Paisani et al. [14] and Remístico
et al. [15].
According to Pouwels et al. [16] and Alsumali
et al. [17], patients have recorded significantly worsened values for
spirometry variables due to the adopted surgical procedure, although it was performed
by videolaparoscopy, as well as to the administered
anesthetics. Consequently, this technique seems to lead to deleterious effects
on patients’ pulmonary function, besides increasing their likelihood to develop
respiratory complications such as atelectasis, pneumonia, and hypoxia [3].
Almarakbi et
al. [18] observed that the best oxygenation results were recorded right
after ARM application and the maintenance of ARM effects depends on maneuver
repetition. Almarakbi et al. [18] also
investigated the effect of ARM repetition on patients’ oxygenation and
atelectasis reduction. Their studies have evidenced that ARM repetition
increased lung compliance and PaO2, as well as reduced PaCO2,
improved gas exchange efficiency and respiratory mechanics, and maintained its
beneficial effects at the postoperative period.
ARM was applied
only once during the procedure and there were no differences in spirometry
variables and postoperative pulmonary complications in comparison to the
conventional or decompression groups. On the other hand, like results in the
present study, Defresne et al. [19] did not find any
additional benefit from alveolar recruitment application in association with
protective ventilation to FVC, FEV1; or any oxygenation changes in the postoperative
period.
In comparison to
non-obese individuals, morbid obesity and pneumoperitoneum compromise patients’
respiratory mechanics and lead to carbon dioxide retention [20]. Systemic
carbon dioxide resorption during videolaparoscopy
surgeries can have deleterious effects on lung function, as well as increase
ventilatory load due to increased transperitoneal pressure; thus, it is in
opposition to diaphragmatic contraction.
The collected
data have shown increased PETCO2 right after alveolar recruitment
due to decreased tidal and minute volumes during alveolar recruitment, whose
values significantly dropped until pre-extubation.
Similar findings were recorded by Remíticos et al.
[15], who observed increased PETCO2 right after ARM application with
PEEP at 30 cmH2O and inspiratory pressure at 45 cmH2O -
PETCO2 values dropped minutes after ARM application. According to
the literature [21,22], reduced PETCO2 indicates improved alveolar
ventilation due to higher alveoli recruitment and lower collapsed alveoli
rates. Literature still lacks studies focused on investigating the immediate
effect of CCDM in comparison to ARM during the postoperative period of patients
subjected to bariatric surgery. Therefore, the present study included a group
of patients who were subjected to CCDM right after surgery to test the
hypothesis that lungs subjected to this maneuver can present lower atelectasis
incidence without patients’ subjection to ARM.
The use of CCDM
right after surgery has reduced atelectasis incidence and improved patients’
lung function. This outcome was like the ones recorded when ARM and
conventional physical therapy were adopted in the intraoperative period. The
positive response of obese patients to CCDM use in the postoperative period
(six hours after surgery) likely derived from hypoventilation correction.
According to Via et al. [7], CCDM reduced the incidence of pulmonary
complications such as hypoventilation and atelectasis, as well as the
development of acute hypoxemia after surgery due to pulmonary ventilation
restoration, which improved oxygenation and decreased CO2 levels. Unoki et al. [23] applied CCDM to 31 mechanically
ventilated patients and found that this maneuver enabled bronchial hygiene by
increasing expiratory time and peak expiratory flow. However, the maneuver did
not contribute to pulmonary re-expansion because it required the application of
high inspiratory pressure.
Lack of
pulmonary expansion after CCDM application in the study conducted by Unoki et al. [23] was explained by differences in
protocols adopted in other studies. Patients assessed in the current study did
not present changes in bronchial hygiene needs. Via et al. [7] performed
bronchial hygiene before CCDM application in all patients; however, Unoki et al. [23] performed CCDM without previous
bronchial hygiene, which may have reinforced its effects on bronchial hygiene,
but not on pulmonary expansion.
According to Paisani et al. [13], obese patients presented
shallower breathing in the postoperative period, as well as increased
respiratory rate due to the need of maintaining the minute volume. This finding
was not observed in the present study. In compliance with Tomich
et al. [24], exercises performed through slow and deep inspirations
contributed to uniform inhaled-gas distribution in pulmonary parenchyma,
increased the transpulmonary pressure, improved tidal volume and, consequently,
reduced respiratory rates.
Lack of gasometry, ventilometry, manovacuometry and the impossibility of performing patient
follow-up after hospital discharge can be considered limitation factors in the
current study. Based on these mechanisms, other important ventilation variables
could be explored during the respiratory follow-up of morbid obesity patients.
The assessed
parameters should be investigated in future clinical trials focused on
clarifying the best follow-up protocol to be applied to bariatric surgery
patients during the postoperative period.
Conclusion
Conventional
physical therapy, manual chest compression and decompression maneuver, and
alveolar recruitment were beneficial to pulmonary function recovery. There were
no differences in postoperative pulmonary complications and pulmonary function
of patients in the three experimental groups, except for significant decrease
in respiratory rate and end-expiratory carbon dioxide pressure level in the ARM
group.
Authors' contribution
Conception and design of the study, acquisition of
data, analysis and interpretation of data, manuscript writing: Fabiana Della
Via and Desanka Dragosavac;
Technical procedures, final approval: Admar Concon Filho; Preparation and critical revision: Carolina Kosour; Alveolar recruitment and critical review: Carlos
Eduardo Ferraresi Andrade and Emanuel Guedes
References
- Benaiges D, Goday A, Pedro-Botet J, Más A, Chillarón JJ, Flores-Le Roux JA. Bariatric surgery: To whom
and when? Minerva Endocrinol 2015;40:119-28.
https://doi.org/10.4103/aer.AER_126_19
- Rivas
E, Arismendi E, Agustí A,
Sanchez M, Delgado S, Gistau C et al. Ventilation/Perfusion
distribution abnormalities in morbidly obese subjects before and after
bariatric surgery. Chest 2015;147(4):1127-34.
https://doi.org/10.1378/chest.14-1749
- Baltieri
L, Peixoto-Souza FS, Rasera-Junior I, Montebelo MI, Costa D, Pazzianotto-Forti
EM. Analysis of the prevalence of atelectasis in patients undergoing
bariatric surgery. Braz J Anesthesiol
2016;66:577-82.
https://doi.org/10.1016/j.bjan.2015.10.002
- Forno E, Han YY, Mullen J, Celedon JC. Overweight, obesity, and lung function in children and adults-a meta-analysis. J Allergy Clin Immunol Pract 2018;6(2):570-81. https://doi.org/10.1016/j.jaip.2017.07.010
- Dixon AE, Peters U. The effect of obesity on lung
function. Expert Review of Respiratory Medicine 2018;12:755-67.
https://doi.org/10.1080/17476348.2018.1506331
- Pazzianotto-Forti EM, Costa MCM, Merino DFB, Rocha MRS, Mori TA, Júnior
IR. Effects of inspiratory exercise with linear and nonlinear load on
respiratory variables post-bariatric surgery. Respir Care 2019;64(12):1516-22.
https://doi.org/10.4187/respcare.05841
- Via F, Oliveira R, Dragosavac
D. Effects of manual chest compression and descompression
maneuver on lung volumes, capnography and pulse oximetry in patients receiving
mechanical ventilation. Rev Bras Fisioter 2012;16(5):354-59.
https://doi.org/10.1590/S1413-35552012005000028
- Bluth T, Teichmann R, Kiss T, Bobek J, Canet J, Cinnela G
et al. Protective intraoperative ventilation with higher
versus lower levels of positive end-expiratory pressure in obese patients
(PROBESE): study protocol for a randomized controlled trial. Trials
2017;18(202):1-22. https://doi.org/10.1186/s13063-017-1929-0
- Bime C,
Fiero M, Lu Z, Oren E, Berry CE, Parthasarathy S et al. High positive
end-expiratory pressure is associated with improved survival in obese patients
with acute respiratory distress syndrome. Am J Med 2017;130(2):207-13.
https://doi.org/10.1016/j.amjmed.2016.09.029
- Ball L, Pelosi P. Positive end-expiratory pressure and recruitment maneuvers in obese patients: should
we chase oxygenation? Minerva
Anestesiol 2018;84(4):429-31.
https://doi.org/10.23736/S0375-9393.18.12608-3
- Barbas
CS, Isola AM, Farias AM, Cavalcanti AB, Gama AM, Duarte AC et al. Brazilian recommendations of mechanical ventilation
2013. Part 2. Rev Bras Ter Intensiva 2014;26(3):215-39.
https://doi.org/10.5935/0103-507X.20140034
- Culver
BH, Graham BL, Coates AL, Wanger J, Berry CE, Clarke
PK et al. Recommendations for a standardized pulmonary function
report: an official American Thoracic Society Technical Statement. Am J Respir
Crit Care Med 2017;196:1463-72.
https://doi.org/10.1164/rccm.201710-1981ST
- Sümer I, Topuz U, Alver S, Umutoglu T, Bakan M, Zengin SÜ et al. Effect of the "recruitment"
maneuver on respiratory mechanics in laparoscopic sleeve gastrectomy surgery. Obes Surg
2020;30(7):2684-92. https://doi.org/10.1007/s11695-020-04551-y
- Paisani M, Chiavegato L, Faresin A. Volumes, capacidades pulmonares e força muscular respiratória no pós-operatória de gastroplastia. J Bras Pneumol 2005;31(2):25-32. https://doi.org/10.1590/S1806-37132005000200007
- Remístico
P, Araújo S, Figueiredo LC, Aquim EE, Gomes LM,
Sombrio ML et al. Impacto da manobra de recrutamento alveolar no pós-operatório
de cirurgia bariátrica videolaparoscópica. Rev
Bras Anestesiol 2011;61(2):163-76.
https://doi.org/10.1590/S0034-70942011000200006
- Pouwels S, Smeenk FW, Manschot L, Lascaris B, Nienhuijs S, Bouwman RA et al. Perioperative respiratory care in obese
patients undergoing bariatric surgery: Implications for clinical practice.
Respir Med 2016;117:73-80.
https://doi.org/10.1016/j.rmed.2016.06.004
- Alsumali A,
Al-Hawag A, Bairdain S, Eguale T. The impact of bariatric surgery on pulmonary
function: a meta-analysis. Surg Obes Relat Dis 2018;14(2):225-36. https://doi.org/10.1016/j.soard.2017.09.533
- Almarakbi WA,
Fawzi HM, Alhashemi JA. Effects of four
intraoperative ventilatory strategies on respiratory compliance and gas
exchange during laparoscopic gastric banding in obese patients. Br J Anaesth 2009;102(6):862-8. https://doi.org/10.1093/bja/aep084
- Defresne AA, Hans GA, Goffin PJ, Bindelle SP, Amabili PJ, De Roover AM et al. Recruitment of lung volume during surgery neither affects the postoperative spirometry nor the risk of hypoxaemia after laparoscopic gastric bypass in morbidly obese patients: a randomized controlled study. Br J Anaesth 2014;113(3):501-7. https://doi.org/10.1093/bja/aeu101
- Sen
O, Doventas YE. Effects of
different levels of end-expiratory pressure on hemodynamic, respiratory
mechanics and systemic stress response during laparoscopic cholecystectomy. Braz J Anesthesiol 2017;67:28-34. https://doi.org/10.1016/j.bjane.2015.08.015
- Masa JF, Pépin JL, Borel JC, Mokhlesi B, Murphy PB,
Sánchez-Quiroga MA. Obesity hypoventilation syndrome. Eur Respir Rev 2019;28(151):180097.
https://doi.org/10.1183/16000617.0097-2018
- Piper A. Obesity hypoventilation syndrome: weighing in
on therapy options. Chest 2016;149(3):856-68.
https://doi.org/10.1378/chest.15-0681
- Unoki T, Kawasaki Y, Mizutani T, Fujino Y, Yanagisawa Y,
Ishimatsu S et al. Effects of expiratory rib-cage compression on
oxygenation, ventilation, and airway-secretion removal in patients receiving
mechanical ventilation. Respir
Care 2005;50(11):1430-7. Disponível em:
http://rc.rcjournal.com/content/respcare/50/11/1430.full.pdf
- Tomich
GM, França DC, Diniz MT, Britto RR, Sampaio RF, Parreira VF. Effects
of breathing exercises on breathing pattern and thoracoabdominal motion after
gastroplasty. J Bras Pneumol 2010;36(2):197-204.
https://doi.org/10.1590/S1806-37132010000200007