Fisioter Bras 2021;22(3):290-305
ORIGINAL ARTICLE
Two types of inspiratory muscle training on muscle
strength in patients submitted to coronary artery bypass grafting: clinical trial
Dois
tipos de treinamento muscular inspiratório sobre a força muscular de pacientes
após revascularização do miocárdio: ensaio clínico
André
Luiz Lisboa Cordeiro*, Lucas Oliveira Soares**, Meire Laiana
Lima Vasconcelos**, Taiane Ribeiro da Paixão
Correia**, Adriele Santos de Souza**, André Raimundo
França Guimarães***, Jefferson Petto****, Pedro Henrique Cerqueira de Andrade*****
*Curso
de Fisioterapia, Faculdade Nobre, Feira de Santana, BA, Departamento de
medicina e Saúde Humana, Escola Bahiana de Medicina e
Saúde Pública, Salvador, BA, **Curso de Fisioterapia, Faculdade Nobre, Feira de
Santana, BA, ***Departamento Médico, Instituto Nobre de Cardiologia, Feira de
Santana, BA, ****Curso de medicina e Saúde Humana, Escola Bahiana
de Medicina e Saúde Pública, Salvador, BA, Curso de Fisioterapia, Universidade
Salvador, Feira de Santana, BA, Curso de Fisioterapia, Faculdade Adventista da
Bahia, Cachoeira, BA, *****Serviço de Fisioterapia, Hospital Geral Clériston Andrade, Feira de Santana, BA
Received:
May 31, 2021; Accepted: June
6, 2021.
Correspondence: André Luiz Lisboa Cordeiro, Faculdade Nobre, Avenida
Maria Quitéria, Kalilândia 44001-008 Feira de Santana
BA, E-mail: andrelisboacordeiro@gmail.com
André Luiz Lisboa Cordeiro: andrelisboacordeiro@gmail.com
Lucas Oliveira Soares: lucassoaresft@gmail.com
Meire Laiana Lima Vasconcelos:
meirelaianavasconcelos@gmail.com
Taiane Ribeiro da Paixão
Correia: taianecorreia@gmail.com
Adriele Santos de Souza:
adrielesouza.fisio@gmail.com
André Raimundo França Guimarães: andremed@bol.com.br
Jefferson Petto:
petto@cardiol.br
Pedro Henrique Cerqueira de Andrade: pedroandrade@gmail.com
Abstract
Introduction: Coronary
artery bypass grafting (CABG) causes changes in the respiratory musculature
that affects functional capacity and postoperative complications (POC).
Inspiratory muscle training (IMT) is a tool used for these patients, but it is
not known what the best form is to increase strength. Objective: To
investigate whether IMT with a linear pressure load device is superior to the
inspiratory incentive on functional capacity and muscle strength of patients
undergoing CABG. Methods: This is a clinical trial. Patients were
assessed preoperatively for inspiratory muscle pressure (MIP), expiratory
pressure (MEP), peak expiratory flow (PEF), six-minute walk test (6MWT) and
functional independence measure (FIM). After surgery, they were divided into three
groups: control group (CG), training group with linear pressure load (IMT) and
inspiratory incentive group (IG). On the day of discharge, all patients had
their previous variables reassessed. Results: The study included 56
patients, 31 (55.4%) were male and an average age of 55 ± 12 years. There was a
significant reduction in all variables, in relation to MIP, the IMT showed a
higher value in the postoperative period 83 ± 19 cmH2O, against 70 ±
15 cmH2O in the CG and 80 ± 15 cmH2O in the IG (p < 0.001). The
same behavior was observed in MEP, 77 ± 12 cm H2O in IMT, 67 ± 14
cmH2O in CG and 75 ± 10 cmH2O in IG (p < 0.001). Regarding the 6
MWT, there was a lesser loss in the IMT from 434 ± 15 m to 398 ± 20 m in IG (p
< 0.001). Conclusion: It is concluded that muscle training with a
linear pressure load device is superior to training with incentive on
functional capacity and muscle strength in patients undergoing CABG.
Keywords: physical therapy; myocardial
revascularization; muscle strength.
Resumo
Introdução: A cirurgia de revascularização do
miocárdio (CRM) causa alterações na musculatura respiratória que afetam a
capacidade funcional e complicações pós-operatórias (DCP). O treinamento
muscular inspiratório (TMI) é uma ferramenta utilizada por esses pacientes, mas
não se sabe qual é a melhor forma de aumentar a força. Objetivo:
Investigar se o TMI com dispositivo de carga de pressão linear é superior ao
incentivo inspiratório na capacidade funcional e força muscular de pacientes
submetidos à CRM. Métodos: Este é um ensaio clínico. Os pacientes foram
avaliados no pré-operatório para pressão muscular inspiratória (PImáx), pressão expiratória (PEF), pico de fluxo
expiratório (PFE), teste de caminhada de seis minutos (TC6) e medida de
independência funcional (MIF). Após a cirurgia, eles foram divididos em três
grupos: grupo controle (GC), grupo treinamento com carga linear de pressão
(IMT) e grupo incentivo inspiratório (GI). No dia da alta, todos os pacientes
tiveram suas variáveis anteriores reavaliadas. Resultados: O estudo
incluiu 56 pacientes, 31 (55,4%) eram do sexo masculino e idade média de 55 ±
12 anos. Houve redução significativa em todas as variáveis, em relação à PImáx, o IMT apresentou valor maior no
pós-operatório 83 ± 19 cmH2O, contra 70 ± 15 cmH2O no GC
e 80 ± 15 cmH2O no GI (p < 0,001). O mesmo comportamento foi
observado na PEmáx, 77 ± 12 cmH2O
no IMT, 67 ± 14 cmH2O no GC e 75 ± 10 cmH2O no GI (p <
0,001). Em relação ao TC6, houve menor perda no TMI de 434 ± 15 metros para 398
± 20 metros no GI (p < 0,001). Conclusão: Conclui-se que o
treinamento muscular com dispositivo de carga pressórica linear é superior ao
treinamento com incentivo inspiratório na capacidade funcional e da força
muscular em pacientes submetidos à CRM.
Palavras-chave: fisioterapia; revascularização
miocárdica; força muscular.
Introduction
Coronary artery
bypass grafting (CABG) despite all advances is associated with complications in
the postoperative period (PO) that change pulmonary function causing
pneumothorax, pleural effusion, atelectasis, and pneumonia. These complications
can lead to an increase in hospital stay, risk of functional decline and
increased mortality rate. In this sense, inspiratory muscle training (IMT)
appears as a tool for hospital rehabilitation of this population [1,2,3,4,5].
Some intra and
postoperative procedures are directly linked to these complications: the median
sternotomy, the effects of anesthesia, cardiopulmonary bypass (CPB), use of
chest tubes and invasive mechanical ventilation can alter respiratory mechanics
[6,7].
To detect all
these complications, it is important to monitoring of pulmonary function by
measuring the maximum respiratory pressures, which are the maximum inspiratory
pressure (MIP) and expiratory pressure (MEP), both of which assess muscle
strength using a manovacuometer [8]. The measure of
the patient's functional limitation can be assessed using the 6-Minute Walk
Test (6MWT) simple and low-cost procedure, which aims to measure the patient's
functional capacity [10]. The level of dependence during motor and cognitive
activities is determined using the Functional Independence Measure (FIM) scale
[11].
From the
detection of changes in muscle strength, inspiratory muscle training (IMT) is
performed, which is aimed at strengthening the respiratory musculature,
benefiting the efficiency in airway clearance, maximum inspiratory and
expiratory pressure and prevention of muscle fatigue
[12]. Among these trainings are the pressure load device and the flow
incentive.
The pressure
device, also known as Threshold®, works by a spring system, with a
pre-determined pressure based on MIP [13]. The flow incentive, has a turbulent
and variable initial flow increasing the respiratory work, also promotes visual
feedback, stimulating the patient to take maximum and sustained inspirations, leading
to an increase in transpulmonary pressure [14].
There are still
few studies that talk about the comparison of the respiratory stimulator with
the Threshold® in postoperative patients of CABG. Therefore, the objective of
this research was to investigate whether inspiratory muscle training with a
linear pressure load device is superior to the inspiratory stimulator on
functional capacity, pulmonary complications, functionality, pulmonary function and length of hospital stay of patients undergoing to
CABG.
Methods
The study is a
randomized and controlled clinical trial, approved by the Research Ethics
Committee of Faculdade Nobre
under the number 2,088,636. All patients were informed of the research
objectives and signed a Free and Informed Consent Form (ICF). Data collection
was carried out from October 2019 to July 2020 at the Instituto Nobre de Cardiologia (INCARDIO),
Feira de Santana-Bahia, a regional reference center for cardiological
treatments. The work was registered in the Brazilian Registry of Clinical
Trials (ReBec) under the number RBR-36fvws.
Patients
Inclusion
criteria were individuals of both genders, older than 18 years and submitted to
coronary artery bypass grafting via median sternotomy and extracorporeal circulation.
Exclusion criteria: patients who did not understand how to perform the
techniques, who presented hemodynamic instability (20% more or less of heart
rate, systolic blood pressure or diastolic blood pressure) during the
assessment of inspiratory pressure maximum or muscle training, diagnosis of
pneumopathy, uncontrolled arrhythmias and cognitive alterations, length of stay
in the Intensive Care Unit (ICU) longer than 4 days and those who required
Invasive Mechanical Ventilation for more than 24 hours.
Patients were
assessed preoperatively for maximum inspiratory pressure (MIP), maximum
expiratory pressure (MEP), peak expiratory flow (PEF), six-minute walk test
(6MWT) and functional independence measure (FIM). On the first postoperative
day, they were randomized by simple drawing into three groups. The groups were
as follows: control group (CG), inspiratory muscle training group (IMT) and
inspiratory incentive group (IG).
The Control
Group (CG) received routine care from the hospital without any interference
from the researchers; the conducts applied were sedation, ambulation, breathing
exercises, cycle ergometry and kinesiotherapy. The IMT group performed
inspiratory muscle training using the linear pressure load device (Threshold
IMT®) with a load corresponding to 40% of MIP, performing three sets of 10
repetitions, twice a day until the moment of hospital discharge. The third
group (IG) carried out training with the inspiratory flow motivator, performing
maneuvers with deep inspirations and with the highest possible inspiratory flow
peak, aiming to reach a load equivalent to 50% of MIP, with 30 inspirations and
twice per day until hospital discharge. These last two groups underwent
conventional physical therapy with the addition of the muscle training protocol
prescribed for their group.
Pulmonary function and muscle strength
Preoperative
assessment of inspiratory muscle strength (MIP) was performed using an Indumed® (São Paulo, Brazil) analogue manovacuometer.
During the evaluation, a maximal expiration until the residual volume was
requested, and then a maximal and slow inspiration to the total lung capacity
was required. This test was done using the unidirectional valve method, being
possible a flow through a hole of one millimeter, aiming to exclude the action
of the buccinator, and repeated for three times, being used the highest value
reached, if this value was not the last. MEP was evaluated using the same
apparatus and the patient was instructed to perform a maximal inspiration until
he reached his total pulmonary capacity, the mask was placed, and after that a
maximum expiration was requested until the residual capacity was reached. The
test was repeated three times and it was considered the highest value result, if this value was not the last [8]. Both tests were
performed with the patient seated, lower limbs resting on the ground.
To assess VC, we
used the analogue ventilometer Ferraris Mark 8 Wright
Respirometer (Louisville, Colorado, Unite States of America). The ventilometer was unlocked, cleared, and soon after the
facial mask was placed on the face of the individual. The patient underwent
deep inspiration until he/she reached his/her total pulmonary capacity, and
soon after a slow and gradual expiration until reaching the residual volume.
After this, the ventilometer was locked and the
result observed and noted. The test was repeated three times, being considered
the highest value result [10].
Peak expiratory
flow was evaluated using the peak flow of the Mini Wright® brand. During the
evaluation, the patient was seated, with his head in a neutral position and a
nasal clip to prevent air from escaping through the nostrils. The patient took
a deep breath, until total pulmonary capacity, followed by forced expiration
with the mouth in the device. After three measurements, the highest value was
chosen and there could be no difference > 40 liters between measurements
[9].
Measurement of functional capacity
The 6MWT was
used following the recommendations of the American Thoracic Society, or ATS,
being conducted in a 30-meter, flat, and totally obstacle-free corridor. Prior
to the test, patients had a rest period of at least 10 minutes. During this
period, they were evaluated for contraindications, blood pressure data (through
Premium aneroid sphygmomanometer and 3M Littmann
stethoscope), pulse oximetry (Rossmax), dyspnea level
(Borg scale), heart rate (assessed by palpation of the radial artery and
counting over a period of one minute), and respiratory rate (evaluated by
verifying the respiratory incursion during one
minute). The patient was advised to walk as fast as possible, without running,
in this corridor for six minutes. During the test, encouragement phrases were
used each minute. At the end of the test, the examiner quantified the distance
covered within those six minutes [10].
During the
protocol, patients were monitored, and in the presence of an increase in
systolic and/or diastolic blood pressure > 30% of baseline, heart rate <
20% of baseline, peripheral oxygen saturation < 90%, and increased
respiratory rate > 25 breaths per minute, the test was discontinued.
Functionality assessment
These
individuals were also assessed for the Functional Independence Measure (FIM), a
questionnaire that uses a 7-point scale to assess 18 items in the areas of
personal care, sphincter control, mobility, locomotion, communication, and
social cognition. This assessment was designed to measure the patient's level
of dependence. Each dimension is analyzed by the sum of its categories from 1
to 7, the lower the score, the greater the degree of dependence. Adding the
points of the dimensions of the instrument, it reaches a minimum total score of
18 and a maximum of 126 points, which characterize the levels of dependence
[11].
Surgical procedure
Coronary artery
bypass grafting was performed through median sternotomy and cardiopulmonary
bypass. Left internal thoracic artery or saphenous vein graft was used. The
surgical procedure has always been carried out by the same team, ending with
the positioning of a subxiphoid drain, left intercostal drain and sternorrhaphy. Analgesia was optimized for all patients and
was referred to the Intensive Care Unit.
Postoperative management
After the
surgical procedure, all patients were referred to the Intensive Care Unit (ICU)
to receive the immediate care necessary for their recovery. They underwent
Invasive Mechanical Ventilation (IMV) in assisted mode controlled by volume or
pressure, with tidal volume from 6 ml/kg to 8 ml/kg of the predicted weight,
with respiratory rate (RF) of 12 to 18 ipm, inspired
fraction of oxygen (FiO2%) to maintain a peripheral oxygen saturation
(SpO2%) of 93 and 97%, an inspiration/exhalation ratio of 1: 2 and
a positive pressure at the end of exhalation (PEEP) of 5 cmH2O [21].
After interrupting ventilation or extubation,
patients continued to receive medical and physiotherapeutic care until
discharge from the ICU. Then they were taken to the ward where they continued
to receive their usual care until discharge from the hospital where a new
assessment of maximum inspiratory pressure (MIP), maximum expiratory pressure
(MEP), peak expiratory flow (PEF) was performed, six-minute walk test (6MWT)
and functional independence measure (FIM) to make a comparison with the data
obtained in the preoperative moment.
Clinical results
During the
hospitalization period, pulmonary complications in the postoperative period
were analyzed: atelectasis, pleural effusion, pneumothorax, and pneumonia,
which were diagnosed with the aid of chest radiography. CPB duration,
mechanical ventilation, hospital stay, number of bridges and drains
(mediastinum and hemothorax) were also recorded.
Statistical analysis
For data
analysis, the program SPSS 20.0 was used. To evaluate the normality of the
sample, the Kolmogorov-Smirnov test was used. Categorical variables were
analyzed using the Chi-square. For pre and post training evaluation within the
group, the paired Student's T-Test was used and for comparison in the three
groups, the ANOVA Test was used. It was considered significant when p <
0.05.
Results
Between August
2017 and February 2018, 60 patients were admitted to the Instituto Nobre de Cardiologia (INCARDIO),
in Feira de Santana/BA and 56 answered the inclusion criteria. The flowchart
shows the progress of the study and how each group was divided (Figure 1).
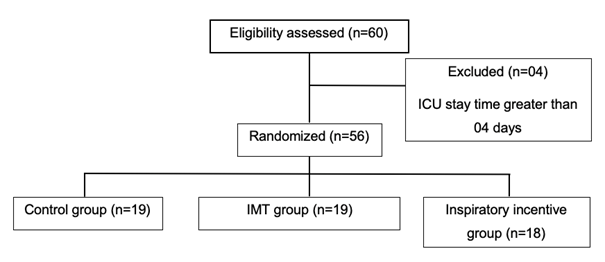
Figure 1 - Study progression and division
of the studied groups
In the sample,
we found 31 (55.4%) males with a mean age of 55 ± 12 years. The most common
comorbidity was systemic arterial hypertension (SAH) in 44 (78.5%) of the
patients (Table I).
Surgical data
showed an average CPB time of 80 ± 14 minutes and an average MV time of 8 ± 4
hours. The other data are shown in Table II.
Regarding the
functional variables, it was found that the TMI group in the 6MWT obtained a
longer distance than the other groups (IMT 398 ± 20 m vs CG 305 ± 21 m vs IG
356 ± 19 m). As for the FIM, the Control Group was the one that lost the most
points when compared to the two moments before 123 ± 2 and 112 ± 5 afterwards
(< 0.001). The other variables are shown in Table III.
Pulmonary
complications were less evident in the group that underwent conventional
inspiratory muscle training when compared to the control group and the
incentive group, with statistical significance in pneumothorax GTMI 0 vs GC 1
(p < 0.32), hypoxemia GTMI 3 vs GC 8 (p < 0.02), atelectasis GTMI 3 vs GC
8 (p < 0.02) and pneumonia GTMI 0 vs GC 2 (p < 0.45). The complete data
on complications in the postoperative period are described in the table below
(Table IV).
The information
related to pulmonary function and strength is shown in table V. A statistically
significant reduction was observed in all groups, but a greater decline in
variables was observed in the control group during hospitalization. We can
observe the behavior of MIP in the CG before 110 ± 9 vs 70 ± 15 after (p <
0.001), GTMI before 107 ± 8 vs 83 ± 19 after (p < 0.001) and GI before 107 ±
10 vs 80 ± 15 after (p < 0.001).
Table I - Clinical characteristics of
the patients included in the study
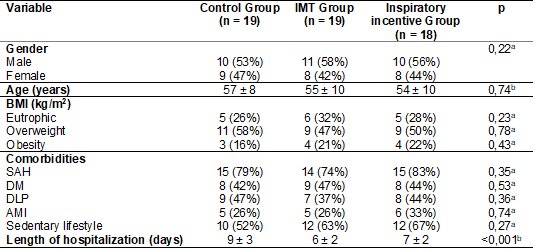
aChi-square test; bANOVA;
IMT = Inspiratory Muscle Training; BMI = Body Mass Index; SAH = Systemic
Arterial Hypertension; DM = Diabetes Mellitus; DLP = Dyslipidemia; AMI = Acute
Myocardial Infarction
Table II - Surgical characteristics of
the studied patients
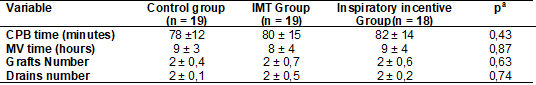
aANOVA; IMT = Inspiratory Muscle
Training; CPB = Cardiopulmonary bypass; MV = Mechanical Ventilation
Table III - Behavior of functional
variables between groups
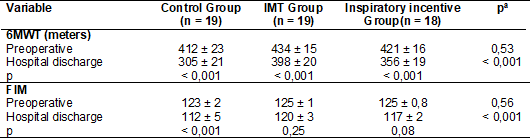
aANOVA; bPaired
Student's t test; IMT = Inspiratory Muscle Training; 6MWT = Six-minute walk
test; FIM = Functional Independence Measure
Table IV - Pulmonary complications of
patients randomized according to the group
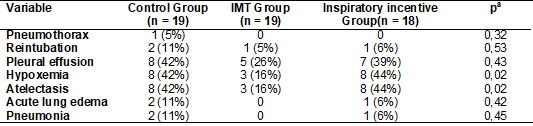
aANOVA; IMT = Inspiratory muscle training
Table V - Behavior of pulmonary
variables between groups
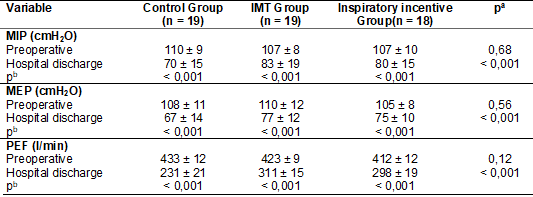
aANOVA; bPaired
Student's t test; MIP = Maximum Inspiratory Pressure; MEP = Maximum Expiratory
Pressure; PEF = Peak Expiratory Flow
Discussion
The present
study aimed to verify which type of inspiratory muscle training is most
effective to reduce the impact on functional capacity, pulmonary complications,
functionality, lung function and length of hospital stay. It was shown that an
IMT program with a linear pressure load device is efficient to minimize the
loss of functional capacity, reduce postoperative complications and decline in
functionality, decrease the worsening of pulmonary function, mainly of
inspiratory muscle strength, and shorten the length of stay of this studied population.
The
post-operative of myocardial revascularization is a large and very invasive
procedure, which is why it requires some specific care, as patients can usually
present pneumothorax, atelectasis, pleural effusion
and pneumonia, reduced lung function and pain [16,17,18,19,20,21,22,23]. These complications lead
to a decline in lung function, directly impacting functionality and functional
capacity, leading this patient to stay in the hospital for more days. We
noticed in our results that the patients who had more pulmonary complications
in the postoperative period were those in the control group, which also had a
greater decline in lung function, observed by the reduction of MIP, MEP, PEF,
walked less on the 6MWT, lost more point in the FIM when comparing pre and post
intragroup and intergroup values.
We noticed in
our study that the group that performed the IMT Threshold IMT® had fewer
complications in the postoperative period, less three days of hospitalization
when compared to the control group, lost less in the 6MWT compared to the pre-
and postoperative moment and in relation to functionality was the group that
lost the least points in the MIF. This result shows us that TMI with Threshold
IMT® is beneficial for this audience and can have an influence on the patient's
functional capacity and functionality. IMT becomes an essential tool in the
rehabilitation of these patients, preventing these negative events from
occurring.
Other authors
have already shown that IMT is a safe and viable resource for the
rehabilitation of patients in the Intensive Care Unit regardless of whether
they are in invasive mechanical ventilation, helping to gain strength in the
inspiratory muscles, especially in the activation of the diaphragm, improving
the pulmonary function, functional capacity and, consequently, their quality of
life [24,25,26].
Silva et al.
[27] demonstrated that the IMT with the inspiratory flow motivator was able to
increase the inspiratory muscle strength and the distance covered in the 6MWT
in patients after cardiac surgery. A result like the study by Silva et al.
[13] also found a significant increase in MIP in patients who used Threshold
IMT®, and an inspiratory incentive to flow at volume in relation to the moment
before training, and in the control group, no change was observed of MIP.
These results,
like ours, the patients who underwent IMT with Threshold IMT® and with the
inspiratory flow incentive lost less points in the FIM, walked more in the 6MWT
and stayed less time hospitalized when compared with the patients in the
control group, showing that the loss was minimized, showing a superior
inspiratory muscle training.
It is worth
highlighting the differences between the incentives that can influence the
outcome of the training. Cordeiro et al. [4] show that patients
undergoing cardiac surgery have reduced pulmonary function, inspiratory muscle
strength, peak expiratory flow up to one month after surgery, generating
changes in ventilatory mechanics.
Of the variables
evaluated, MIP, MEP and PEF showed a significant reduction in the immediate
postoperative period of myocardial revascularization due to the changes
suffered in the procedure, or because they already had predispositions related
to cardiopulmonary problems. Data also observed by Santos et al. [28] in
which changes in MIP and MEP were found after surgery when compared with the
preoperative period. It was also reported the advantage that the IMT groups had
in terms of restoring ventilatory function.
Ge [29] and
Gomes Neto [30] corroborate the same results when they report that inspiratory
muscle training in the postoperative period of cardiac surgery increases
inspiratory muscle strength, improves tidal volume, peak expiratory flow,
improving the effectiveness of coughing consequently. Better removal of
secretion decreasing the risk of complications and the length of hospital stay.
The maximum
respiratory pressures that had negative variations after surgery and recovered
after the completion of physical therapy interventions. Among the three groups
studied, two were used respiratory muscle training (IMT), which acts to recover
ventilatory muscle strength.
The TMI presented
significant indices with the use of the pressure device (Threshold IMT®) and
the inspiratory incentive to flow. The control group that did not have any type
of intervention related to the research relied only on the institution's
physiotherapy protocol. This did not present significant results when compared
with the Threshold IMT® and respiratory incentive to flow, maintaining
disadvantage before the technique.
The present
study has as limitations the lack of a sample calculation and the non-assessment
of confounding factors, such as pain, through logistic regression.
Conclusion
Based on the
findings of the present study, it is concluded that inspiratory muscle training
with a linear pressure load device is superior to training with the inspiratory
flow motivator and has a positive impact on functional capacity, pulmonary
complications, functionality, lung function, and it is also capable of reducing
the length of hospital stay of patients undergoing coronary artery bypass
grafting. It is noteworthy that the achievements of the two forms of
inspiratory muscle training proved to be superior to conventional treatment.
References
- Chen X, Hou L, Zhang Y, Liu X, Shao B, Yuan B, et al.
The effects of five days of intensive preoperative inspiratory muscle training
on postoperative complications and outcome in patients having cardiac surgery:
a randomized controlled trial. Clin Rehabil
2019;00(0):1-10. doi: 10.1177/0269215519828212 [Crossref]
- Santos TD, Pereira SN, Portela LOC, Cardoso DM, Lago PD, Guarda NS. Moderate-to-high intensity inspiratory muscle training improves the effects of combined training on exercise capacity in patients after coronary artery bypass graft surgery: A randomized clinical trial. Int J Cardiol 2019;279:40-6. doi: 10.1016/j.ijcard.2018.12.013 [Crossref]
- Apostolakis E, Filos KS, Koletsis E, Dougenis D. Lung dysfunction following cardiopulmonary
bypass. J Card Surg 2010;25(1):47-55. doi: 10.1111/j.1540-8191.2009.00823.x [Crossref]
- Cordeiro ALL, Silva LGR, Pinto MO, Araújo JS, Guimarães AR, et al. Behavior of pulmonary function after hospital discharge in patients submitted to myocardial revascularization. Int J Cardiovasc Sci 2019;32(2)104-9. doi: 10.5935/2359-4802.20180092 [Crossref]
- Oh HC, Han JW, Choj JW, Kim YH, Hwang HY, Kim KB. Concomitant off-pump coronary artery bypass and non-cardiovascular surgery. J Thorac Dis 2016;20(8):2115-20. doi: 10.21037/jtd.2016.07.80 [Crossref]
- Mathis MR, Duggal NM, Likosky DS, Haft JW, Douville NJ, Vaughn MT, et al. Intraoperative mechanical ventilation and postoperative pulmonary complications following cardiac surgery. Anesthesiology 2019;131(5):1046-62. doi: 10.1097/ALN.0000000000002909 [Crossref]
- Zochios V, Klein AA, Gao F. Protective invasive ventilation in cardiac surgery: a systematic review with a focus on acute lung injury in adult cardiac surgical patients. J Cardiothorac Vasc Anesth 2018;32(4):1922-36. doi: 10.1053/j.jvca.2017.10.031 [Crossref]
- Pessoa IMBS, Neto MH, Montemezzo D, Silva LAM, Andrade AD, Parreira VF. Predictive equations for respiratory muscle strength according to international and Brazilian guidelines. Braz J Phys Ther 2014;18(5):410-11. doi: 10.1590/bjpt-rbf.2014.0044 [Crossref]
- Leiner GC, Abramowits S, Small MJ, Stenby VB, Lewis WA. Expiratory peak flow rate. Standard values for normal subjects. Use as a clinical test of ventilatory function. Am Rev Respir Dis 1963;88:644-51. doi: 10.1164/arrd.1963.88.5.644 [Crossref]
- American Thoracic Society (ATS). Committee on proficiency standards for clinical pulmonary function laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 2004;166(1):111-7. doi: 10.1164/ajrccm.166.1.at1102 [Crossref]
- Riberto
M, Miyazaki MH, Jucá SSH, Sakamoto H, Pinto PPN. Validation of
the Brazilian version of functional independence measure. Acta Fisiatr
2004;11(2):72-6.
- Cordeiro
ALL, Melo TA, Neves D, Luna J, Esquivel MS, Guimarães ARF, et al. Inspiratory
muscle training and functional capacity in patients undergoing cardiac surgery.
Braz J Cardiovasc Surg 2016;31(2):140-4. doi: 10.5935/1678-9741.20160035 [Crossref]
- Paiva DN, Assmannb LB, Bordinb DF, Gassb R, Jostc RT, Bernardo-Filho M, et al. Inspiratory muscle training with threshold or incentive spirometry: Which is the most effective? Rev Port Pneumol 2015;21(2):76-81. doi: 10.1016/j.rppnen.2014.05.005 [Crossref]
- Sarmento
GJV. Fisioterapia respiratória de A a
Z. Barueri: Manole; 2016.
- Barbas CS, Ísola AM, Farias AM, Cavalcanti AB, Gama AM, Duarte AC, et al. Brazilian recommendations of mechanical ventilation 2013. Part I. Rev Bras Ter Intensiva 2014;26(2):89-121. doi: 10.5935/0103-507X.20140017 [Crossref]
- Stephens RS, Whitman GJR. Postoperative critical care of the adult cardiac surgical patient: part II: procedure-specific considerations, management of complications, and quality improvement. Crit Care Med 2015:43(9);1-20. doi: 10.1097/CCM.0000000000001171 [Crossref]
- Stephens RS, Whitman GJR. Postoperative critical care
of the adult cardiac surgical patient: part i: routine postoperative care. Crit
Care Med 2015:43(7):1-21. doi: 10.1097/CCM.0000000000001059 [Crossref]
- Mashaqi B, Iamail I, Siemeni TT, Ruemke S, Fleissner F, Zhang R, et al. Local anesthetics delivered through pleural drainages improve pain and lung function after cardiac surgery. Thorac Cardiovasc Surg 66(2):198-202. doi: 10.1055/s-0035-1558994 [Crossref]
- Katsura M, Kuriyama A, Takeshima T, Fukuhara S, Furukawa TA. Preoperative inspiratory muscle training for postoperative pulmonary complications in adults undergoing cardiac and major abdominal surgery (Review). Cochrane Database of Systematic Reviews 2015:1-87. doi: 10.1002/14651858.CD010356.pub2 [Crossref]
- Naseer BA, Al-Shengiti AM,
Rahman AHAli, Aljeraisi T.
Effect of cardiac surgery on respiratory muscle strength. J Taibah Univ Med Sci
2019:14(4);337-42. doi: 10.1016/j.jtumed.2019.06.002 [Crossref]
- Mans CM, Reeve JC, Elkins MR. Postoperative outcomes following preoperative inspiratory muscle training in patients undergoing cardiothoracic or upper abdominal surgery: a systematic review and meta analysis. Clin Rehabil 2014;1-13. doi: 10.1177/0269215514545350 [Crossref]
- Canet J, Gallart L, Gomar C, Paluzie G, Vallès J, Castillo J, et al. Prediction of postoperative pulmonary complications in a population-based surgical cohort. Anesthesiology 2010;113:1338-50. doi: 10.1097/ALN.0b013e3181fc6e0a [Crossref]
- Guizilinia S, Alvesa DF, Bolzana DW, Cancia ASA, Regengaa MM, Moreira RSL, et al. Sub-xyphoid pleural drain as a determinant of functional capacity and clinical results after off-pump coronary artery bypass surgery: a randomized clinical trial. Interac Cardiovasc Thorac Surg 2014;382-7. doi: 10.1093/icvts/ivu138 [Crossref]
- Bissett B, Leditschke IA, Green M, Marzano V, Collins S, Haren FV. Inspiratory muscle training for intensive care patients: A multidisciplinary practical guide for clinicians. Aust Crit Care 2019:249-255. doi: 10.1016/j.aucc.2018.06.001 [Crossref]
- Walterspachera S, Pietschc F, Walkera DJ, Rockerd K, Kabitza Hans-Joachim. Activation of respiratory muscles during respiratory muscle training. Resp Phys Neurobiol 2018:126-32. doi: 10.1016/j.resp.2017.10.004 [Crossref]
- Elkins M, Dentice R. Inspiratory muscle training facilitates weaning from mechanical ventilation among patients in the intensive care unit: A systematic review. J Physiother 2015;61(3):125-34. doi: 10.1016/j.jphys.2015.05.016 [Crossref]
- Silva
PE, Almeida KMG, Dias VS, Andrade FMD, Almeida MLO. Does inspiratory
muscle training with the flow-oriented incentive spirometer Respiron®
on late postoperative cardiac surgery improve functional outcomes? A double-blind,
randomized, sham-controlled
study. Assobrafir Ciência
2015;6(2):43-54.
- Santos TD, Pereira SN, Portela LOC, Cardoso DM, Lago PD, Guarda NS, et al. Moderate-to-high intensity inspiratory muscle training improves the effects of combined training on exercise capacity in patients after coronary artery bypass graft surgery: A randomized clinical trial. Int J Cardiol 2019;(279):40-6. doi: 10.1016/j.ijcard.2018.12.013 [Crossref]
- Ge X, Wang W, Hou L, Yang K, Fa X. Inspiratory muscle training is associated with decreased postoperative pulmonary complications: Evidence from randomized trials. The Journal of Thoracic and Cardiovascular Surgery 2018;(156)5:1-48. doi: 10.1016/j.jtcvs.2018.02.105 [Crossref]
- Gomes Neto M, Martinez BP, Reis HFC, Carvalho VO. Pre- and postoperative inspiratory muscle training in patients undergoing cardiac surgery: Systematic review and meta-analysis. Clin Rehabil 2016;1(1):1-11. doi: 10.1177/0269215516648754 [Crossref]