Fisioter Bras 2021;22(3):412-424
ORIGINAL ARTICLE
Rebalancing thoraco-abdominal method does not increase
immediate pain assessed by Neonatal Infant Pain Scale: a randomized clinical trial
O
método reequilíbrio tóraco-abdominal não aumenta a
dor avaliada pela Neonatal Infant Pain
Scale: estudo clínico randomizado
Miriana
Carvalho de Oliveira, M.Sc.*, Cristina Ortiz Sobrinho
Valete**, Esther Angélica Luiz Ferreira***, Claudia Maria Valete Rosalino****, Marco Orsini*****
*Mestrado
em Saúde Maternal e Infantil, Universidade Federal Fluminense, Niterói, RJ, Professor
Adjunta de Fisioterapia, Universidade de Serra dos Órgãos, Teresópolis, RJ,
Brasil, **Professora associada, Área da Criança e Adolescente (ASCrA), Departamento de Medicina, Universidade Federal São
Carlos (UFSCar), SP, Brasil, ***Professor Assistente, Área da Criança e
Adolescente (ASCrA), Centro de Estudos
Epidemiológicos em Saúde Perinatal, Neonatal e da Infância, Departamento de
Medicina, Universidade Federal São Carlos (UFSCar), SP, Brasil, ****Instituto
Nacional Evandro Chagas de Doenças Infecciosas, Fundação Oswaldo Cruz, Rio de
Janeiro, RJ, Brasil, Professor do Departamento de Otorrinolaringologia e
Oftalmologia, Faculdade de Medicina, Universidade Federal do Rio de Janeiro,
RJ, Brasil, Programa de Produtividade da Pesquisa, Conselho Nacional de
Desenvolvimento Científico e Tecnológico (CNPq), Brasília, DF, Brasil,
*****Professor do Mestrado de Neurologia, Universidade Iguaçu, Rio de Janeiro,
RJ, Brasil
Correspondence: Cristina Ortiz Sobrinho Valete, PhD, Professor at Department of
Medicine, Universidade Federal São Carlos, Rodovia Washington Luis SP 310, Km 235, 13565-905 São Carlos SP
Miriana Carvalho de Oliveira:
mirianacarvalho@gmail.com.
Cristina Ortiz Sobrinho Valete: cristina.ortiz@ufscar.br
Esther Angélica Luiz Ferreira: draestherferreira@gmail.com.
Claudia Maria Valete Rosalino: cmvalete@gmail.com
Marco Orsini: orsinimarco@hotmail.com
Abstract
Objective: To compare in neonates with
transitory tachypnea if chest rebalancing thoraco-abdominal method (RTA)
increased immediate pain. Methods: This was a randomized controlled
clinical trial. Forty-nine neonates with transitory tachypnea and aged < 72
hours were included to receive either conventional physiotherapy (CP) or RTA
method. Participants received usual care and one 15-minute session of chest
physiotherapy. Neonatal Infant Pain Scale (NIPS), peripheral oxygen saturation,
heart rate, respiratory rate, axillary temperature before and after chest physiotherapy
were recorded. Kruskal-Wallis ANOVA and Mc Nemar test
were used to compare differences between measures. The relative risk (RR) for
pain after interventions was calculated using a Poisson regression model
(robust estimation). A significance level of 5% (p < 0.05) was adopted for
all analyses. Results: RTA was not associated to pain. After chest
physiotherapy, NIPS reduced (2 versus 3, p < 0.001) and number of neonates
with pain reduced (10.2% versus 28.6%, p = 0.02). RR for pain after chest
physiotherapy in comparison to before was 0.3 (95% CI 0.15-0.41; p = 0.02);
respiratory frequency decreased after chest physiotherapy (58 versus 70, p <
0.001) and peripheral oxygen saturation increased (98% versus 96%, p <
0.001). Conclusion: In neonates with transitory tachypnea, in the first
72 hours of life, RTA did not influence pain evaluation, chest physiotherapy
was safe and reduced immediate pain.
Keywords: neonate; physiotherapy
specialties; pain assessment; respiratory care.
Resumo
Objetivo: Comparar em recém-nascidos com
taquipneia transitória se o método reequilíbrio tóraco-abdominal
(RTA) aumentou a dor imediatamente após. Métodos: Estudo de ensaio
clínico randomizado. Quarenta e nove recém-nascidos com diagnóstico de
taquipneia transitória com menos de 72 horas de vida, foram incluídos para
receber fisioterapia respiratória. Os participantes receberam os cuidados
usuais e uma sessão de fisioterapia convencional ou do método reequilíbrio tóraco-abdominal. Foram registradas a escala NIPS (Neonatal
Infant Pain Scale), a saturação periférica de oxigênio, a
frequência cardíaca, a frequência respiratória e a temperatura axilar antes e
depois da fisioterapia. Para as comparações entre as medidas, foram utilizados
o teste de ANOVA de Kruskal-Wallis e o teste de McNemar. O risco relativo de dor após os procedimentos foi
calculado usando o modelo de regressão de Poisson (estimação robusta). Foi
considerado o nível de significância de 5% para todas as análises (p <
0,05). Resultados: O método RTA não foi associado a dor. Após a
fisioterapia respiratória, a escala NIPS reduziu (2 versus 3, p < 0,001) e a
proporção de recém-nascidos com dor também reduziu (10,2% versus 28,6%, p =
0,02). O risco relativo de dor após a fisioterapia respiratória em comparação a
antes, foi de 0,3 (IC 95% 0,15-0,41; p = 0,02), a frequência respiratória
diminuiu (58 versus 70, p < 0,001) e a saturação periférica de oxigênio
aumentou (98% versus 96%, p < 0,001). Conclusão: Em recém-nascidos
com taquipneia transitória nas primeiras 72 horas de vida, o método RTA não
influenciou a avaliação da dor, a fisioterapia respiratória foi segura e
reduziu a dor imediatamente após.
Palavras-chave: recém-nascido; modalidades de
fisioterapia; dor; cuidado respiratório.
Introduction
Pain is a “bad
sensorial and emotional experience” [1]. In the neonate, pain has been studied
for a long time. At first, it was believed that the neonate was unable to
localize and interpret pain, though pain pathways, cortical, subcortical
centers and neurotransmissors were functionally
present. Many neonates were not treated with analgesics during painful
procedures due to this thinking. It is surprising that neonate nociceptives fibers density is superior to adults. Some
pain pathways are myelinated by the 30th gestational week and this process is
completed by the 37th gestational week [2]. Even if some pathways were not
completely myelinated, the shorter distance the impulse needs to travel in the
neonate seems to offset the slower conduction associated to uncomplete
myelination [2].
Currently, we
know that neonates submitted to severe and prolonged pain may have a higher
morbidity and moreover, the lack of a behavioral response does not assure that
there is no pain. At our knowledge, painful experiences during the neonatal
period may be related to pain feedback in the future [3].
Pain evaluation
in the infant is a challenge. The Neonatal Infant Pain Scale (NIPS scale) was
validated in 1993. This scale evaluates facial expression, cry, members movimentation, respiratory pattern and wakefulness. It has
been widely applied in the neonate and varies from 0 to 7. Pain is present when
the scale ponctuation is ≥ 4 [4].
During
hospitalization, neonates are submitted to many procedures that are necessary
for clinical recovery, some of them potentially painful. It is estimated that
half of neonates under hospitalization have pain during the first week of life
[5].
Transitory
tachypnea of the neonate is caused by a delayed pulmonary liquid clearance,
resulting in the presence of fetal liquid in the neonate lungs and leading to
an increase in the interstitial compartment. This condition causes a
respiratory distress that regress spontaneously in most cases. In some cases,
the neonate requires respiratory support [6,7].
Chest
physiotherapy (CPT) has been part of respiratory care in neonatal units for a
long time. Initial studies enrolled small samples and had the objectives to
show physiotherapy efficacy, particularly in removing airway secretions [8,9].
Literature regarding CPT in the neonate is still scarce and the validation of
physiotherapy techniques is necessary. Recent studies evaluated CPT effects in
infants and neonates with acute viral bronchiolitis and suggested that slow
expiration techniques in this situation caused a relief in moderate patients
and no harmful side effects [10,11]. Rebalancing thoracoabdominal method (RTA)
is a CPT method based on muscle tonus, length, and strength normalization
through inspiratory and expiratory balance. This method has been practiced in
neonatal units. A clinical trial that included preterm infants suggested that
RTA reduced respiratory rate and respiratory distress and did not change
neonate behavior [12].
Few studies
evaluated pain after CPT in the neonate. A recent study suggested that preterm
neonates not submitted to ventilatory support presented more pain immediately
after CPT and this was stabilized after 15 minutes [13]. A systematic review
suggested that airway suctioning, and chest compressions caused pain in
neonates. However, because of methodological differences between studies, the
authors concluded that more studies using adequate designs are needed to
evaluate if physiotherapy techniques really cause pain in the neonate [14].
Therefore, the
research question for this study was: does RTA cause immediate pain in the
neonate with transitory tachypnea?
Methods
Study design
This was a
two-armed randomized controlled clinical trial conducted at a private
university-affiliated tertiary hospital in Teresópolis,
Rio de Janeiro, Brazil. The study was approved by the UNIFESO Research Ethics Committee
(CAAE: 45519415.1.0000.5247) and the study protocol was registered online at
the Brazilian Clinical Trials Register -ReBec (RBR
2FFV9G). This study is reported in accordance with the CONSORT guidelines [15].
Study population and sample size
A sample of 49
neonates with transitory tachypnea was recruited to receive a conventional
protocol (CP) of CPT or RTA method. Sample was calculated considering a 54%
difference and a 6% frequency, a statistical power of 80% and setting alpha at
5%.
Between
September 2015 and October 2016, neonates with transitory tachypnea were
approached consecutively. Inclusion criteria were: age
< 72 hours with respiratory distress due to a diagnosis of transitory
tachypnea of the neonate. Exclusion criteria were congenital malformations,
pneumothorax, use of analgesics or sedatives, 5th minute Apgar < 7.
Blinding and randomization
The statistician
was blinded to treatment allocation. The allocation was conducted by an
independent researcher. A simple randomization was made by draw. When a neonate
was included, an independent researcher made the raffle and decided the
intervention.
Outcome measures
The primary
outcome was pain after the CPT session defined as a NIPS scale evaluation ≥
4. All neonates were evaluated in a calm ambient, during a 5-minute period
immediately after the intervention, by the same physiotherapist. Heart rate, respiratory
rate, peripheral oxygen saturation, axillary temperature, were assessed before
and after the intervention.
Procedures
Usual nursing
and medical care were provided to all participants. All neonates with
respiratory distress were submitted to a 15-minute CPT session, performed by
the same physiotherapist, shortly after birth. One of the following two methods
was applied: the conventional protocol (CP) consisted of manual passive
expiratory therapy, chest expiratory vibration, chest expiratory compression,
chest vibration or prolonged slow expiration [16]; The rebalancing
thoraco-abdominal (RTA) method protocol consisted of inferior abdominal
support, thoraco-abdominal support, ileo-costal support, and inspiratory aid
[12]. Airway aspiration was applied only when considered necessary, by the
physiotherapist. All neonates were in the supine position.
Respiratory rate
(breath per minute), heart rate (beat per minute), peripheral oxygen saturation
(%), axillary temperature (°C) and NIPS scale evaluation were assessed before
and after CPT. The following data were also collected: gestational age (days),
birth weight (grams), sex, age (hours), oxygen/ventilatory support (none;
supplementary oxygen; non-invasive ventilation; invasive ventilation).
Statistical analysis
Statistical
analysis was performed using Stata 13.0 program (StataCorp,
LC). Data did not follow a normal distribution and were presented as medians,
interquartile range (IQR) and 95% confidence intervals (95% CI). The
Kruskal-Wallis ANOVA was used to test the continuous variables. The McNemar test was used to compare categorical variables.
Spearman correlation coefficient was applied to measure correlation between
measures before and after intervention. The relative risk (RR) for pain after
CPT in comparison to before, was calculated using a Poisson regression (robust
estimation). A significance level of 5% (p < 0.05) was adopted for all
statistical analyses.
Results
Flow of participants
During the study
period, 1,660 patients were born at the reference hospital, and 49 had
transitory tachypnea of the neonate diagnosis. Figure 1 presents the flowchart
of enrolment of the research participants.
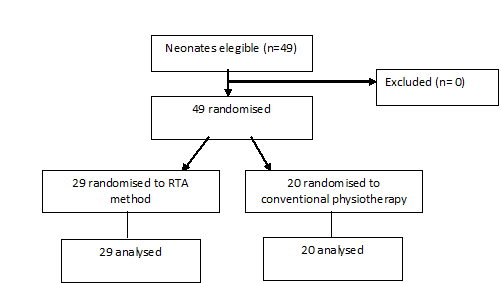
Figure 1 - CONSORT flow diagram
Baseline characteristics of participants
Median birth
weight was 2,980 g (IQR 2,510-3,340) and gestational age was 266 days (IQR
255-275). Median age was 4 hours (IQR 2-10) and 51% were male sex. Eleven
(22.5%) neonates were not using respiratory support, 34 (69.4%) were using
supplementary oxygen, 3 (6.1%) were using non-invasive ventilation and 1 (2.0%)
was on invasive ventilation. Table I shows baseline comparisons between RTA
method and CP groups. There were no appreciable differences between the two
groups with respect to gender, birth weight, gestational age, age, respiratory
and heart rate, peripheral oxygen saturation and axillary temperature.
Table I - Baseline
parameters and demographic characteristics between RTA method and CP groups,
Rio de Janeiro, Brazil, 2020 (n = 49)
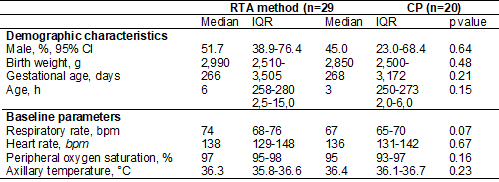
g = grams; h = hours;
bpm = breaths per minute; bpm = beats per minute; °Celsius = Celsius degree. *p
value associated to Mc Nemar or Kruskal-Wallis
Overall effects of chest physiotherapy
Physiological
parameters and NIPS were compared for all the sample before and after CPT
(Table II). We observed an increase of peripheral oxygen saturation, a
reduction in respiratory rate and NIPS scale after CPT.
Table II - Physiological
parameters and Neonatal Infant Pain Scale (NIPS scale) before and after CPT in
neonates aged < 72h with transitory tachypnea, Rio de Janeiro, Brazil, 2020
(n = 49
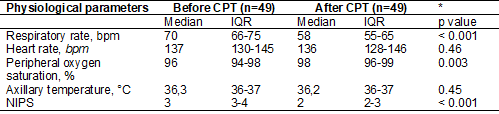
bpm = breaths per
minute; bpm = beats per minute; °C = Celsius degree; NIPS = Neonatal Infant
Pain Scale; *p = value associated to Kruskal Wallis ANOVA
A 18.4%
reduction in the proportion of neonates with pain was observed after CPT (28.6%
vs 10.2%; p = 0.02). The correlation between NIPS scale before and after the
intervention was weak (Spearman 0,21; p value = 0.12). Among neonates with pain
after CPT, two received no respiratory support and three were receiving
supplementary oxygen.
We observed no
differences (p value 0.35) in NIPS median after CPT according to CPT method
(Graph 1).
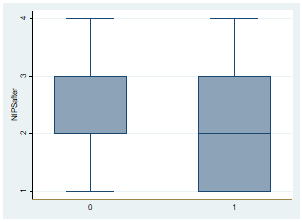
Graph 1 - Box plots
comparisons of NIPS after CP (0) and RTA method (1), Rio de Janeiro, Brazil,
2020 (n = 49)
After CPT,
overall relative risk for pain decreased and RTA method had no influence on
pain, compared to CP (Table 3).
Table III - Pain
evaluation comparisons between CP (n = 20) or RTA method (n = 29) before and
after CPT and risk for pain. Rio de Janeiro, Brazil, 2020 (n = 49)
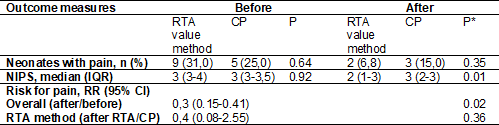
RR = relative risk. *p
= value associated to Mc Nemar, Kruskal-Wallis or Poisson regression
Risk factors for
pain after CPT and associated factors were calculated. Birth weight (RR 1,0;
95% CI 0.99-1.00; p value 0.49), gestational age (RR 1,0; 95% CI 0.95-1.06; p
value = 0.78), male sex (RR 4,3; 95% CI 0.45-42.49; p value = 0.20) were not
associated to pain, as observed in Figure 2. Age was considered not associated
to pain, as its RR was near the null value and 95% CI included the null value
(RR 1,06; 95% CI 1.00-1.13; p value = 0.04).
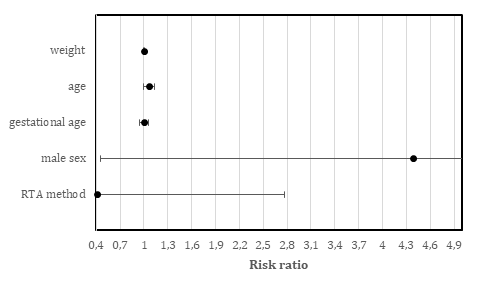
RTA method =
Rebalancing Thoraco-abdominal method
Figure 2 - Forest plot of relative risk for pain after
chest physiotherapy and factors (n = 49)
Discussion
The results of
this study show that RTA method did not increase the risk for pain in neonates
with transitory tachypnea. RTA intervention was associated to a lower NIPS
evaluation. CPT reduced risk of pain, NIPS evaluation and the proportion of
neonates with pain. Reduced respiratory frequency and enhanced peripheral
oxygen saturation was observed after CPT. It is important to evaluate whether
these benefits are of clinical importance. It seems that a respiratory rate
reduction has a clear clinical importance. A 18.4% reduction of pain also seems
to have a strong clinical impact, as less neonates had pain after CPT.
This study also
showed that neonate characteristics had no influence in pain after CPT. Most of
neonates were ≥ 7 months gestational age, birthweight > 2,500 g, not
intubated and aged less than 24 hours. Also, neonates were not routinely
aspirated. These characteristics are important as it has been suggested in
other study that preterm neonates after CPT and airway aspiration, had more
pain. In that scenario both procedures were applied to neonates, and it is
difficult to assure that pain was caused by CPT, airway aspiration or both. CPT
was considered by those authors as a painful stimulus [16].
In the present
study, physiological parameters suggested a better clinical condition after
CPT, as respiratory rate decreased, and peripheral oxygen saturation increased.
We must emphasize that all neonates were treated before and after CPT in the same
and calm ambient and this can have influenced results. A previous study
comparing clinical parameters after CPT in preterm neonates showed an immediate
increase in heart rate and pain scales with posterior return to baseline in 15
minutes [12]. Also, Nicolau et al. [17]
suggested that physiological parameters did not correlate with pain and should
not be used alone to measure pain.
Reduced NIPS
scale after CPT, independent to the physiotherapy method, revealed that CPT
seems to be safe in neonates with transitory tachypnea. We must emphasize that
in the present study, the magnitude of this effect was high as both RR and 95%
IC were far from the benefit thresholds. Noteworthy, pain scale was applied
immediately after the intervention, in the peak moment for pain assessment. It
has been previously suggested that in preterm neonates, immediately after CPT
and after airway aspiration, pain evaluation was worse [12,16]. Also, it has
been suggested that there is no sufficient evidence to recommend one pain
evaluation scale over another [12].
The familiarity
with a scoring seems to be very important for pain assessment [18]. Pain scores
are necessary as pain cannot be directly measured in neonates and behavioral
items are very informative of pain, such as calmness, alertness, and facial
tension [19]. We must emphasize that in the present study, all neonates were in
supine position and in a calm ambient. Also, airway suction was not routine.
So, this does not seem to have influenced the results. Prone position is
comfortable to the neonate, and it has been suggested as part of
non-pharmacological pain treatment [18,20].
The present
study has strengths and limitations. The same observer evaluated neonates
before and after CPT and this evaluation was not blinded. We had no loss of
follow-up, as all neonates included received the interventions and contributed
to outcome measures. Although groups were not balanced, randomization worked,
as groups were comparable at baseline parameters, demographic characteristics,
and initial pain assessment.
Conclusion
The results of
this study indicate that RTA does not influence pain and CPT applied in a calm
ambient reduced NIPS immediate evaluation in neonates with transitory
tachypnea, was effective on reducing respiratory frequency and enhanced
peripheral oxygen saturation. Therefore, CP and RTA can safely be integrated to
other clinical practices in neonatal units.
What was already
known on this topic: CPT is widely practiced in neonatal units. The existing
evidence suggested that neonates present a higher pain scale evaluation
immediately after CPT, but few studies explored RTA method.
What this study
adds: In neonates with transitory tachypnea, CPT was associated to a decrease
in pain and RTA was well tolerated and did not cause an increase in NIPS
evaluation.
Conflicts of interest
The authors declare no
conflicts of interest.
Financing
The present study had
no funding support.
Acknowledgments
We greatly thank all
neonates and participants involved in the project.
References
- Raja SN, Carr DB, Cohen M, et al. The
revised International Association for the Study of pain: concepts, challenges,
and compromises. Pain 2020 https://doi.org/10.1097/j.pain.0000000000001939 [Crossref]
- Anand KJ, Hickey PR. Pain and its effects in the human neonate and fetus. N Engl J Med 1987;317:1321-29, https://doi.org/10.1056/NEJM198711193172105 [Crossref]
- Balda RCX, Guinsburg R. Evaluation and treatment of pain in the neonatal period. Residência Pediátrica 2019;9(1):43-52. https://doi.org/10.25060/residpediatr [Crossref]
- Lawrence
J, Alcock D, McGrath P, et al. The
development of a tool to assess neonatal pain. Neonatal Netw 1993;12:59-66.
- Sposito NPB, Rossato LM, Bueno M, et al. Avaliação e manejo da dor em recém-nascidos internados em Unidade de Terapia Intensiva Neonatal: um estudo transversal. Rev Latino-Am Enferm 2017;25:e2931. https://doi.org/10.1590/1518-8345.1665.2931 [Crossref]
- Miyoshi
MH, Yada M. Síndrome do pulmão úmido. In: Kopelman BI, Santos AMN, Goulart AL, Almeida MFB, Myioshi MH, Guinsburg R. Diagnóstico e tratamento em
neonatologia. São Paulo: Atheneu; 2004.
- Kimura AF, Yoshitake APM, Bueno M, Belli MAJ. Assessment of the newborn respiratory function in the immediate neonatal period. Rev Bras Enferm 2009;62(6):850-55. https://doi.org/10.1590/s0034-71672009000600008 [Crossref]
- Etches PC, Scott B. Chest physiotherapy in the
newborn: Effect on secretions removed. Pediatrics 1978; 62:713-15.
- Finer NN, Boyd J. Postextubation atelectasis: A retrospective review and a prospective controlled study. J Pediatr 1979;94:110-113. https://doi.org/10.1016/s0022-3476(79)80371-6 [Crossref]
- Figuls MR, Giné-Garriga M, Rugeles CG, et al. Chest Physiotherapy for acute bronchiolitis in paediatric patients between 0 and 24 months. Cochrane Database Sys Rev 2016;2(2):CD004873. https://doi.org/10.1002/14651858.CD004873.pub5 [Crossref]
- Postiaux G, Maffei P, Villiot-Fanger JC, Dubus JC. La kinésitherapie respiratoire dans la bronchiolite virale aiguë du norrisson. Arguments pour/contre. Rev Mal Respir 2018;35(4):403-15. https://doi.org/10.1016/j.rmr.2017.08.003 [Crossref]
- Roussenq KR, Scalco JC, Rosa GJ, et al. Rebalancing thoracoabdominal movements in preterms infants: effects on cardiovascular parameters, in behavior, in pain and in the respiratory effort. Acta Fisiatr 2013;20(3):118-23. https://doi.org/10.5935/0104-7795.20130019 [Crossref]
- Tavares AB, Treichel L, Ling CC, et al. Chest physical therapy does not alter acute physiological parameters or pain levels in preterm infants with respiratory distress syndrome in intensive care unit. Fisioter Pesqui 2019;26(4):373-79. https://doi.org/10.1590/1809-2950/18020126042019 [Crossref]
- Zanelat CF, Rocha FR, Lopes GM, et al. The respiratory phisiotherapy causes pain in newborns? A systematic review. Fisioter Mov 2017;30(1):177-86. https://doi.org/10.1590/1980-5918.030.001.ar01 [Crossref]
- Shulz KF,
Altman DG, Moher D, CONSORT Group. CONSORT 2010 statement: updated guidelines
for reporting parallel group randomized trials. BMJ 2010;340:c332. https://doi.org/10.1136/bmj.c332 [Crossref]
- Fink, JB. Expiratory chest compression for atelectasia: No Harm,No
foul – oops! Respiratory Care 2004;49(8):894.
- Gimenez LG, Rodrigues RF, Oliveira MCF, et al. Temporal assessment of neonatal pain after airway aspiration. Rev Bras Ter Intensiva 2020;32(1):66-71. https://doi.org/10.5935/0103-507x.20200011 [Crossref]
- Nicolau CA, Modesto K, Nunes P, et al. Avaliação da dor no recém-nascido prematuro: parâmetros fisiológicos versus comportamentais. Arq Bras Cienc Saude 2008; 33(3):146-50. https://doi.org/10.5935/2595-0018.20200021 [Crossref]
- Carter BS, Brunkhorst J. Neonatal pain assessment. Seminars in Perinatology. 2017;41(2):111-116. https://doi.org/10.1053/j.semperi.2016.11.001 [Crossref]
- Välitalo PAJ, van Dijk M, Krekels EHJ, et al. Pain and distress caused by endotracheal suctioning in neonates is better quantified by behavioral than physiological items: A comparison based on Item Response Theory Modelling. Pain 2016;157(8):1611-17. https://doi.org/10.1097/j.pain.0000000000000485 [Crossref]