Fisioter Bras 2022;23(2): 206-19
ORIGINAL ARTICLE
Alternative therapy for respiratory muscle training using breath
stacking
Terapia alternativa
para o treinamento dos músculos respiratórios utilizando o breath
stacking
Fabrício Edler
Macagnan*, Bianca Andrade Martha**, Inaiá Miranda Lourenzon***,
Anderson Sartor Pedroni**,
Adriana Kessler****
*Departamento de Fisioterapia, Universidade
Federal de Ciências da Saúde de Porto Alegre, Programa
de Pós-Graduação em Ciências da Reabilitação da Universidade Federal de
Ciências da Saúde de Porto Alegre, RS, Brazil, **Programa de Pós-Graduação em Ciências da
Reabilitação da Universidade Federal de Ciências da Saúde de Porto Alegre,
Brazil, ***Acadêmica, Faculdade de
Medicina, Universidade do Vale do Taquari, Lajeado, RS, Brazil, ****Departamento
de Fisioterapia, Universidade Federal de Ciências da Saúde de Porto Alegre, Brazil
Received: August 25, 2021; Accepted: March 3, 2022.
Correspondence: Fabrício Edler Macagnan, Av. Itajaí 368/301 Petrópolis 90470-140
Porto Alegre RS
Fabrício Edler Macagnan:
fabriciom@ufcspa.edu.br
Bianca
Andrade Martha: bianca.martha@acad.pucrs.br
Inaiá Miranda Lourenzon: inalou5@me.com
Anderson Sartor Pedroni:
anderson.pedroni@ufcspa.edu.br
Adriana Kessler: adrianak@ufcspa.edu.br
Abstract
Objective: To evaluate the effectiveness of the breath-stacking
technique as a method of ventilatory muscle training. Methods:
Thirty-eight healthy youngsters were included in the study. The maximum
respiratory pressures were evaluated in cmH2O by a digital manovacuometer. The breath-stacking system (face mask
attached to a T-tube with a unidirectional inspiratory valve) was used as an
overload method in a 4-week 12-session ventilatory muscle training program. Results:
Both maximal inspiratory and expiratory pressures increased significantly after
ventilatory muscle training for all. Positive peak pressure also increased
significantly at the end of the program. Conclusion: Breath-stacking
generates sufficient overload to ventilatory muscles to consistently increase
maximal respiratory pressures when used in a ventilatory muscle training
protocol. The technique was well tolerated, although it needs to be tested in
clinical situations involving muscle weakness and other organic dysfunctions.
Keywords: breathing exercises; maximal respiratory pressures;
ventilatory muscles; respiratory mechanics; inspiratory capacity; physical
therapy techniques.
Resumo
Objetivo: Avaliar a efetividade da técnica de breath-stacking como método de treinamento dos músculos
ventilatórios. Métodos: Trinta e oito jovens saudáveis foram incluídos
no estudo. A pressão respiratória máxima foi avaliada em cmH2O em um manovacuômetro digital. O sistema de breath-stacking
(máscara facial conectada a um tubo T acoplado a uma válvula unidirecional
inspiratória) foi o método utilizado para gerar a sobrecarga ao longo de 12
sessões do programa de treinamento da muscular (4 sessões/semana). Resultados:
Ambas pressões inspiratórias e expiratórias máximas aumentaram
significativamente após o treino dos músculos ventilatórios. O pico de pressão
positiva aumentou significativamente ao final do programa. Conclusão: O breath-stacking gera sobrecarga suficiente para os músculos
ventilatórios promovendo aumento consistente das pressões respiratórias máximas
quando utilizado em um protocolo de treino da musculatura ventilatória. A
técnica foi bem tolerada, mas permanece a necessidade de testes em situações
clínicas que envolvam fraqueza muscular e outras disfunções orgânicas.
Palavras-chave: exercícios respiratórios; pressão
respiratória máxima; músculos ventilatórios; mecânica respiratória; capacidade
inspiratória; modalidades de fisioterapia.
Introduction
The respiratory muscles are
responsible for mobilizing a satisfactory air volume into the lungs at a large
range of metabolic rates. To move the ribcage during inspiratory and expiratory
cycles, all resistive forces must be overcome by these muscles. Respiratory
muscle strength is fundamental to ventilatory bump particularly when some
restrictive, obstructive or both disorders are present [1,2,3,4].
Two meta-analyses have
demonstrated the beneficial impact of respiratory muscle training (RMT) in
healthy sedentary [5] and athletic [6] populations. Moreover, patients with low
functional capacity have also demonstrated substantial increase in inspiratory
performance [7,8]. Recently, inspiratory muscle training (IMT) has been used to
prevent pulmonary complications in post operatory stages [9,10,11]. IMT seems to
be beneficial to several clinical conditions [12,13,14,15,16,17], reinforcing the central
role of inspiratory muscle strength on physical performance [18] and
rehabilitation programs [7,8].
Respiratory muscle
adaptations have been described in the literature through diverse training
arrangements and overload techniques [19,20]. Some protocols deliver overload
only to inspiratory muscles while others focus on inspiratory and expiratory
training (RMT). In the literature, descriptions of muscle overload level,
training program structure and equipment employed are highly diverse
[5,7,8,17,18,19,20].
Breath-stacking (BS) is a
breathing technique used to induce higher alveolar ventilation through
pulmonary expansion [21] and is particularly helpful for poorly collaborative
patients. Due to using a unidirectional valve (expiratory occlusion) [22], the
BS incites a clinical situation that may correspond to dynamic
hyperventilation. This occurs following repetitive sequential inspirations that
promote considerable air retention, conducting the patient’s tolerance to their
limit for pulmonary hyperinflation [23]. When performing the maneuver
repeatedly, lung volume expansion and subsequent peripheral air distribution
are incited [21,22,23]. However, as the volume of air trapped increases with
sequential inhalation, it is assumed that the muscle overload progresses in
parallel with hyperinflation. The additional muscle effort imposed by changes
in ventilatory mechanics (due to hyperinflation) may act as an overload
stimulus and provide the respiratory muscles with functional adaptations. This
effect has not yet been fully described. Therefore, the main objective of this
study was to evaluate the efficacy of BS intervention as an alternative
respiratory therapy on respiratory muscle training in healthy young
individuals.
Methods
In this preclinical
single-arm study, young healthy and non-athlete volunteers participated in a
training program to investigate the viability, safety, and potential
therapeutic use of the Breath-Stacking technique as a respiratory muscle
training. Thirty-eight individuals (18-24 years old) were included in the
study. Considering the high standard deviations between the maximal inspiratory
pressure (MIP) and maximal expiratory pressure (MEP) in this population (MIP =
17.3 cmH2O) [24,25] and the expected increase of one standard
deviation after the ventilatory muscle training (VMT) program, the sample size
calculation resulted into 26 subjects; however, 40 individuals were recruited
in order to balance for possible dropouts. Participants reporting claustrophobia,
tympanic membrane rupture, MIP and MEP exceeding the normal range, and those
who were competitive athletes, wind instrumentalists, and singers were
excluded.
Procedures
After being informed about
the study procedures, eligible individuals signed a consent form and underwent
an educational session regarding the assessment tests and methods of
respiratory muscle strength training. An experienced independent researcher
assessed both MIP and MEP (72 hours following the educational session).
Assessment of ventilatory muscle strength
MIP and MEP were measured
and recorded on a digital manovacuometer (MVD 300®
model, Sao Paulo, Brazil). MIP was measured by performing a maximum
inspiration, while MEP was measured by performing a maximum expiration
according to the Pulmonary Function Test Guidelines [26].
Respiratory muscle training
RMT was conducted using a
silicone facemask attached to a T-tube, which was connected to a one-way
inspiratory valve (Figure 1). Participants were instructed to remain seated
with their elbows resting on a table and hands holding the mask firmly against
their face to minimize air leakage. Training sessions were conducted three
times a week, over a period of four weeks (twelve sessions in total). In every
training session, three sets of RMT (three-minute long each) were performed,
with two recovery intervals (three minutes each) between sets (15 minutes in
total). In the second set of each session, the BS system was coupled to the manovacuometer to monitor the positive pressure peak (PPP)
generated at the tolerance limit (maximum pulmonary expansion).
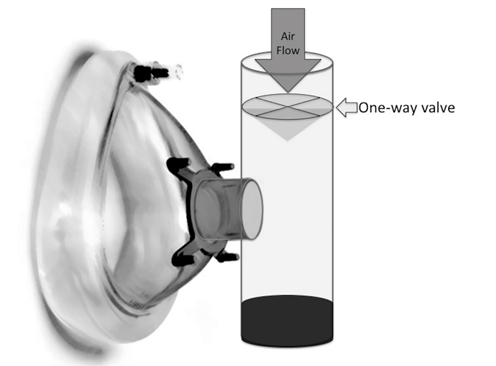
Fig. 1 - Respiratory muscle training device for
breathing-staking protocols
Participants were instructed
to fractionate inspiration in at least three parts. In the interval between
each inhalation, air should be maximally forced into the mask (with the
expiratory valve occluded) generating successive PPP. After each expiration
attempt, a new inspiratory cycle should be started successively until the
hyperinflation tolerance limit was reached. This limit was defined as a drastic
decrease or absence of inspiratory flow. After that, the mask was removed to
allow pulmonary emptying and the start of a new repetition. MIP and MEP were
reevaluated at the end of each week and reports of discomfort and/or
difficulties to properly perform exercises were constantly recorded. To
continue in the study, adherence to the program should be full. Any absence was
later recovered; therefore, no exclusion due to lack of adherence occurred.
Statistical analysis
Data are expressed as
absolute (mean, standard deviation, standard error) and relative values
(percentage variation between pre and post-test). The effect of RMT on MIP and
MEP was analyzed through Student's t-test (paired) and repeated measure
analysis of variance for time and sex factors were performed. Tukey's test was
used for multiple comparisons, and effect size was assessed by Cohen's d
coefficient for dependent t-test, as preconized by Lenhard W and Lenhard A
[27]. A significance level of 5% (p < 0.05) and an observed power of 80% (OP
> 80%) were assumed.
Results
Forty healthy young
individuals (Table I) were invited to participate, although one declined due to
time restriction and another one quit the program due to intolerance to the BS
RMT protocol (ear pain provoked during PPP). The remaining 38 participants (26
females) completed the study. As expected, MIP and MEP were significantly
higher in males (MIP: f = 84.60 and p = 0.0001; MEP: f = 71.28 and p = 0.0001).
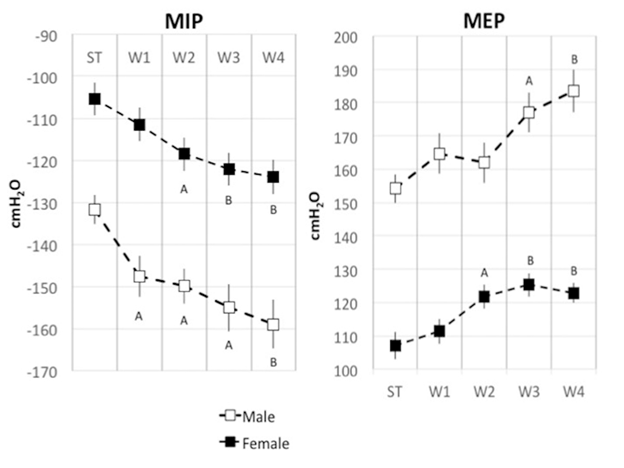
There was a significant increase in respiratory muscle strength (Figure 2) but
no interaction between time and sex was found (MIP: p = 1.0; MEP: p = 0.7).
This indicated that functional adaptations induced by muscle overload occurred
regardless of sexual characteristics (Figure 3). The relative increase in
muscle strength was equivalent between males and females (approximately 4%
higher in men for both MIP and MEP) (Table I). On the other hand, the effect of
time on strength increment was significant (MIP: p = 0.002; MEP: p = 0.02) and
progressive throughout the program.
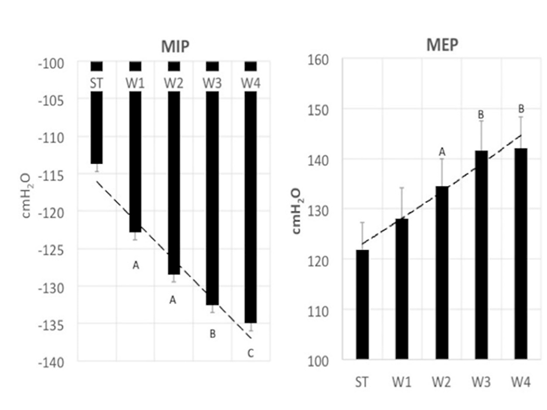
ST = start training; W = week; A = significant
difference when compared to the ST; B = significant difference when compare to
the A; C = significant difference when compared to the B. Data represent
average and standard error; the effects of respiratory muscle training were
available by repeated measure analysis of variance
Fig. 2 - Maximal inspiratory pressure (MIP) and maximal
expiratory pressure (MEP) development during the respiratory muscle training
program
Table I - Increase in muscle strength in the respiratory muscle
training program
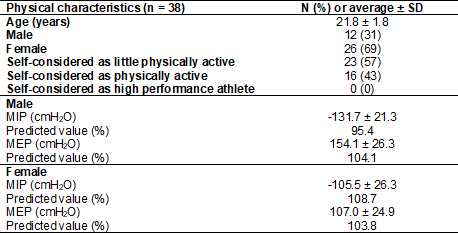
MIP = maximal inspiratory pressure; MEP = maximal
expiratory pressure
ST = start training; W = week; A = significant
difference when compared to the ST; B = significant difference when compare to
the A. Data represent average and standard error; the effects of respiratory
muscle training were available by repeated measure analysis of variance
Fig. 3 - Maximal inspiratory pressure (MIP) and maximal
expiratory pressure (MEP) development during the respiratory muscle training
program
PPP also increased linearly
and progressively until the end of the RMT (Figure 4). In the fifth session,
PPP significantly exceeded the values recorded on the first day of training (p
< 0.05). In the seventh session, PPP reached values higher than the fifth
session and the values of the eleventh session were even higher when compared
to the seventh session. The pattern of PPP increment was comparable between
sexes while no interaction between sex and time was found (p = 0.98).
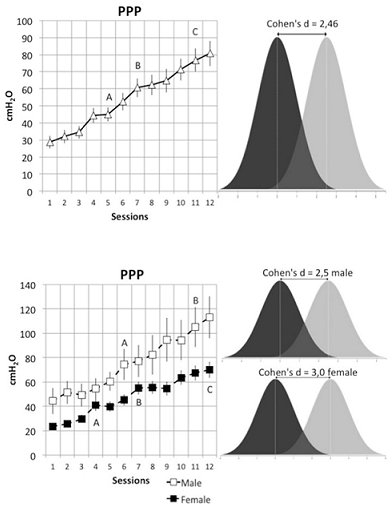
ST = start training; W = week; A = significant
difference when compared to the ST; B = significant difference when compare to
the A; C = significant difference when compare to the B Data represent average
and standard error; the effects of respiratory muscle training were available
by repeated measure analysis of variance, effect size estimate for Cohen’s d
test
Fig. 4 - Positive pressure peak (PPP) development during
the respiratory muscle training program
Considering baseline values
as normality pattern, it could be assumed that baseline values represent data
from a control group of healthy young individuals. Thus, it was possible to
rearrange the data to perform effect size calculation (Cohen's d) and the
number needed to treat (NNT). It was observed that the effect size was
relatively large for MIP and MEP, but larger for PPP (Table II). At the end of
training, it was possible to expect increases in MIP, MEP and PPP of 76%, 73%
and 281% in healthy young individuals, respectively, regardless of sex. The NNT
suggested that one therapeutic success could be achieved for each 4.1 (MIP),
4.9 (MEP) and 1.3 (PPP) healthy youngers treated (respectively).
Table II – Differences before and after training
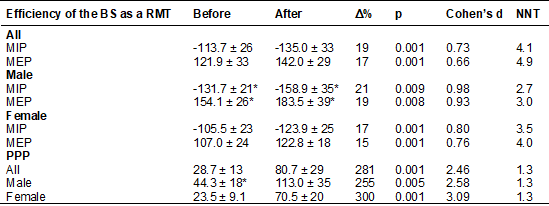
MIP = maximal inspiratory pressure; MEP = maximal expiratory
pressure, PPP = positive pressure peak, * = p < 0.0001 when compared with
female
Discussion
This study has been the
first so far to evaluate the effectiveness of Breath Stacking as a therapeutic
method of respiratory muscle training in young and healthy individuals. The
results were consistent and demonstrated that adaptations occurred regardless
of sex. Even with slight differences between sexes, the expectation of
enhancing the performance of the respiratory muscles is quite high for this population.
In general, the changes started from the second week of training and kept on
progressing towards the end of the twelfth session. Since healthy individuals
have shown to improve their respiratory muscle strength, it may be assumed that
those presenting reduced respiratory muscle strength will benefit from more
significant improvements.
Based on the results, the
use of BS as proposed in this study can be classified as a respiratory muscle
training due to the significant increases in the performance of the ventilatory
(both inspiratory and expiratory) muscle groups. Although the Breath Stacking
technique has been originally used as a therapeutic resource to promote
increased lung volume [21,22,23], this study showed that muscle overload generated
by the artificial dynamic hyperventilation is sufficient to induce gains in
ventilatory strength performance - even in the absence of mechanical or
pathological airflow resistance during inspiration processes. When comparing
the relative increase in maximum pressures (MIP ~ 19% and MEP ~ 17%), it is
reasonable to assume that BS imposes an equivalent overload to both inspiratory
and expiratory muscles.
Measurement of positive
pressure peak (PPP) during the isovolumetric expiration phase allowed to monitor
the degree of effort produced by the expiratory muscles throughout the program.
In the first session, PPP corresponded to 26% of basal MEP. Interestingly, the
relative increase in PPP (281%) at the end of the program was substantially
higher than the relative increase in MPE (17%). This indicates that
participants began to develop higher muscle capacity (56% of the post training
MEP), which may represent the effect of learning in improving the performance
of the technique.
When analyzed separately by
sex, PPP reached 61% and 57% of MEP (male and female, respectively). This
muscle requirement is very close to the highest muscle overload values
recommended in the literature, which generally do not exceed 60% of the maximum
pressure for expiratory muscle training [6,7,8,9,10,11]. Regarding expiratory overload,
BS can be considered an effective expiratory muscle training technique since
the achieved overload rate is substantially high. RMT using BS protocol may
also be useful for pulmonary expansion therapy or atelectasis reversion due to
the significant increase in PPP achieved at the end of training. However, this
mechanism must be studied through new trials recruiting patients with pulmonary
disorders.
Considering the size of the
effect obtained after training, our findings strongly support the therapeutic
potential that this technique offers as an RMT modality. It is also important
to consider the relevant influence of motivation for physical training since in
this method the degree of muscle demand is influenced by each individual
determination. Thus, the applicability of BS as RMT in clinical situations has
yet to be evaluated. Another important aspect to consider is related to the
degree of strength increase that is intended to be obtained with training. In
athletes, for instance, equipment that uses airflow resistance (springs)
generates very high workloads, and, consequently, greater training potential.
In fact, BS is a much more feasible technique for treating clinical
dysfunctions than for high performance training, although similar gains to ours
were reported in healthy young people (17%) [19]. Nonetheless, flow resistors
achieve much greater gains [28] than those found with BS, especially over MIP,
reinforcing the recommendation that high-performance physical training should
prioritize more robust overloading techniques as a first option.
The results show statistical
importance and bring light to a new alternative therapy for RMT since BS has
been studied and applied for other purposes other than the one proposed and
proved by the results in this study. The size effect found is relatively large
for MIP, MEP and PPP regardless of sex. Moreover, the small number needed to
treat (NNT) demonstrates this therapy must be explored in new trials, with
other populations and specific pathologies (NNT: MIP = 4.1; MEP = 4.9; PPP =
1.3).
Finally, the upward behavior
of respiratory muscle strength (inspiratory and expiratory) performance
observed throughout the proposed training period (4 weeks) suggests that the
physiological adaptations promoted by BS may reach values higher than those
observed in this study, since there was no accommodation (plateau pattern) in
the MIP and MEP curves. Therefore, the maximum potential of BS as RMT has not
been found yet, and our data support the hypothesis that the apex of functional
development of ventilatory muscles should occur over a 4-week training period.
Conclusion
In conclusion, BS can be a
feasible choice for RMT aiming at the recovery of muscle strength. However,
exposure to training periods longer than 12 sessions will be required to
elucidate the physiological peak of ventilatory muscle adaptation when
overloaded by this technique. In addition, BS must be tested under different
clinical conditions of ventilatory muscle weakness to unravel the likelihood of
success of this therapeutic resource for rehabilitation of ventilatory muscles
functions. The BS protocol as a RMT may also be useful for pulmonary expansion
therapy, due to the significant increase in PPP achieved at the end of
training, but clinical trials with different lung disorders should be conducted
to further confirm our findings.
Acknowledgements
We thank André Dias Bueno for his constant effort in
the search for viable therapeutic methods for clinical practice. We thank the
support of Júlio Brunelli, Vitório
Ortiz Reolon, Alessandro Pereira Spigolon
e Roberta Ribeiro Gonçalves for their assistance in the initial phases of the
study. We are also grateful to all study participants for contributing their
time.
Conflict of interest
The authors declare they have no conflict of interest.
Founding Source
Rio Grande do Sul Research Support Foundation (FAPERGS
- Fundação de Amparo à Pesquisa
do Rio Grande do Sul) provided financial support for the conduct of the
research.
Ethical approval
The study design was approved by a local Research
Ethics Committees of Porto Alegre, RS, Brazil (AN: 07/03874).
Authors' contributions
Statistical analysis, presentation and discussion of
results and writing the paper: Macagnan FE; Providing
extra methodological help, writing assistance and proof reading the article:
Martha BA, Lourenzon IM, Pedroni
AS, Kessler A
References
- Franco L, Tobin MJ. Disorders
of the respiratory muscles. Am J Respir Crit Care Med 2003;168(1):10-48. doi: 10.1164/rccm.2206020 [Crossref]
- Rondelli RR, Corso SD,
Simões A, Malaguti C. Métodos de avaliação da fadigabilidade
muscular periférica e seus determinantes energético-metabólicos na DPOC. J
Bras Pneumol 2009;35(11):1125-35. doi: 10.1590/s1806-37132009001100011 [Crossref]
- McConnell AK, Griffiths LA. Acute cardiorespiratory responses to inspiratory pressure threshold loading. Med Sci Sports Exerc 2010;42(9):1696-703. doi: 10.1249/mss.0b013e3181d435cf [Crossref]
- Turky K, Afify
AMA. Effect of preoperative inspiratory muscle training on alveolar-arterial
oxygen gradients after coronary artery bypass surgery. J Cardiopulm
Rehabil Prev
2017;37(4):290-4. doi: 10.1097/hcr.0000000000000234 [Crossref]
- Illi SK, Held U, Frank I, Spengler CM.
Effect of respiratory muscle training on exercise performance in healthy
individuals: a systematic review and meta-analysis. Sports Med
2012;42(8):707-24. doi: 10.1007/bf03262290 [Crossref]
- HajGhanbari B, Yamabayashi C, Buna TR, Coelho JD, Freedman KD, Morton TA, et al. Effects of respiratory muscle training on performance in athletes: a systematic review with meta-analyses. J Strength Cond Res 2013;27(6):1643-63. doi: 10.1519/jsc.0b013e318269f73f [Crossref]
- Lin SJ, McElfresh J, Hall B, Bloom R, Farrell
K. Inspiratory muscle training in patients with heart failure: a systematic
review. Cardiopulm Phys Ther
J 2012;23(3):29-36. doi: 10.1097/01823246-201223030-00005 [Crossref]
- Plentz RD, Sbruzzi
G, Ribeiro RA, Ferreira JB, Dal Lago P. Inspiratory muscle training in patients
with heart failure: meta-analysis of randomized trials. Arq Bras Cardiol 2012;99(2):762-71. doi: 10.1016/j.ijcard.2012.06.035 [Crossref]
- Katsura M, Kuriyama A, Takeshima
T, Fukuhara S, Furukawa TA. Preoperative
inspiratory muscle training for postoperative pulmonary complications in adults
undergoing cardiac and major abdominal surgery. Cochrane Database Syst Rev
2015;(10):CD010356. doi: 10.1002/14651858.cd010356 [Crossref]
- Mans CM, Reeve JC, Elkins MR.
Postoperative outcomes following preoperative inspiratory muscle training in
patients undergoing cardiothoracic or upper abdominal surgery: a systematic
review and meta analysis. Clin Rehabil
2015;29(5):426-38. doi: 10.1177/0269215514545350 [Crossref]
- Kendall F, Oliveira J,
Peleteiro B, Pinho P, Bastos PT. Inspiratory muscle training is
effective to reduce postoperative pulmonary complications and length of
hospital stay: a systematic review and meta-analysis. Disabil Rehabil
2017:1-22. doi: 10.1080/09638288.2016.1277396 [Crossref]
- Silva IS, Fregonezi GA, Dias FA, Ribeiro CT, Guerra RO, Ferreira GM. Inspiratory
muscle training for asthma. Cochrane Database Syst Rev 2013;(9):CD003792. doi: 10.1002/14651858.cd003792.pub2 [Crossref]
- Tamplin J, Berlowitz DJ. A systematic review and meta-analysis of the
effects of respiratory muscle training on pulmonary function in tetraplegia. Spinal Cord 2014;52(3):175-80. doi: 10.1038/sc.2013.162 [Crossref]
- Martín-Valero
R, Zamora-Pascual N, Armenta-Peinado JA. Training
of respiratory muscles in patients with multiple sclerosis: a systematic
review. Respir Care 2014;59(11):1764-72. doi: 10.4187/respcare.02881 [Crossref]
- Martín-Valero R, De La Casa Almeida M, Casuso-Holgado
MJ, Heredia-Madrazo A. Systematic review of
inspiratory muscle training after cerebrovascular accident. Respir Care
2015;60(11):1652-9. doi: 10.4187/respcare.03981 [Crossref]
- Gomes-Neto M, Saquetto MB, Silva CM, Carvalho VO, Ribeiro N, Conceição
CS. Effects of respiratory muscle training on respiratory function,
respiratory muscle strength, and exercise tolerance in patients poststroke: a
systematic review with meta-analysis. Arch Phys Med Rehabil
2016;97(11):1994-2001. doi: 10.1016/j.apmr.2016.04.018 [Crossref]
- Bissett BM, Leditschke A, Neeman
T, Boots R, Paratz J. Inspiratory muscle training to
enhance recovery from mechanical ventilation: a randomised
trial. Thorax 2016;71:812-9. doi: 10.1136/thoraxjnl-2016-208279 [Crossref]
- Strasser B, Siebert U, Schobersberger W. Effects
of resistance training on respiratory function in patients with chronic
obstructive pulmonary disease: a systematic review and meta-analysis. Sleep
Breath 2013;17(1):217-26. doi: 10.1007/s11325-012-0676-4 [Crossref]
- Romer LM, McConnell AK. Specificity and reversibility of inspiratory
muscle training. Med Sci Sports Exerc
2003;35(2):237-44. doi: 10.1249/01.mss.0000048642.58419.1e [Crossref]
- Verges S, Renggli AS, Notter
DA, Spengler CM. Effects of different respiratory muscle training regimes on
fatigue-related variables during volitional hyperpnoea.
Respir Physiol Neurobiol 2009;169(3):282-90. doi: 10.1016/j.resp.2009.09.005 [Crossref]
- Marini JJ, Rodriguez RM,
Lamb VJ. Involuntary breath-stacking. An alternative method for
vital capacity estimation in poorly cooperative subjects. Am Rev Respir Dis 1986;134:694-8. doi: 10.1164/arrd.1986.134.5.902 [Crossref]
- Sá Feitosa LA, Barbosa PA,
Pessoa MF, Rodrigues-Machado MG , de Andrade AD. Clinimetric properties of breath-stacking technique for
assessment of inspiratory capacity. Physiother Res Int 2012;17:48-54. doi: 10.1002/pri.512 [Crossref]
- Dias CM, Plácido TR,
Ferreira MFB, Guimarães FS, Menezes SLS. Inspirometria
de incentivo e breath stacking:
repercussões sobre a capacidade inspiratória em indivíduos submetidos à
cirurgia abdominal. Rev Bras
Fisioter 2008;12(2):94-9. doi: 10.1590/s1413-35552008000200004 [Crossref]
- Neder JA, Andreoni S, Lerario MC, Nery LE. Reference
values for lung function tests: II. Maximal respiratory pressures and voluntary
ventilation. Braz J Med Biol Res 1999;32(6):719-27. doi: 10.1590/s0100-879x1999000600007 [Crossref]
- Rodrigues A, Silva ML, Berton DC, Cipriano G Jr, Pitta F, O'Donnell DE, et al. Maximal
inspiratory pressure: does the choice of reference values actually matter? Chest 2017;152(1):32-9. doi: 10.1183/13993003.congress-2016.pa2251 [Crossref]
- Souza RB. Diretrizes para
teste de função pulmonar: pressões respiratórias estáticas máximas. J Pneumol 2002;28(supl3):155-65.
- Lenhard W, Lenhard A. Calculation of effect sizes. Dettelbach (Germany):
Psychometrica; 2016. [Internet] [cited 2022 March 8].
Available from: https://www.psychometrica.de/effect_size.html
- Forbes S, Game A, Syrotuik D, Jones R, Bell GJ. The effect of inspiratory and expiratory respiratory muscle training in rowers. Res Sports Med 2011;19(4):217-30. doi: 10.1080/15438627.2011.608033 [Crossref]