Fisioter
Bras 2021;22(6):871-80
ORIGINAL
ARTICLE
Expiratory positive airway
pressure on oxygenation and hemodynamics in patients submitted to coronary
artery bypass grafting
Pressão
positiva expiratória das vias aéreas sobre a oxigenação e hemodinâmica em
pacientes submetidos a revascularização do miocárdio
André
Luiz Lisboa Cordeiro*, Jammille Barreto Andrade**,
Luiza Teixeira dos Santos**, Ana Tereza Alves Silva**, Arethuza
Evangelista dos Santos Pedreira**, André Raimundo França Guimarães***
*Escola
Bahiana de Medicina e Saúde Pública, Salvador/BA, Faculdade
Nobre, Feira de Santana/BA, **Faculdade Nobre, Feira de Santana/BA,
***Instituto Nobre de Cardiologia, Feira de Santana/BA
Received: September
25, 2021; Accepted: December
6; 2021.
Correspondence: André Luiz Lisboa Cordeiro,
Departamento de Fisioterapia, Centro Universitário Nobre, Av. Maria Quitéria,
2116, 44001-008 Feira de Santana BA
André
Luiz Lisboa Cordeiro: andrelisboacordeiro@gmail.com
Jammille Barreto Andrade: jabandrade@outlook.com
Luiza
Teixeira dos Santos:
luizamm2610@gmail.com
Ana
Tereza Alves Silva: ana_tereza28@hotmail.com
Arethuza Evangelista dos Santos Pedreira:
are_fisio@outlook.com
André
Raimundo França Guimarães: andremed@bol.com.br
Abstract
Introduction: Expiratory
Positive Airway Pressure
(EPAP) is the application of an expiratory resistance
to maintain positive airway pressure and has been
widely used to prevent possible
complications in the postoperative period of cardiac surgery.
Objective: To describe the behavior
of oxygenation and hemodynamics during the use of EPAP in patients undergoing coronary artery bypass grafting
(CABG). Methods: This
was a cross-sectional study that evaluated
peripheral oxygen saturation (SpO2), heart
rate (HR), respiratory rate (RR), systolic
(SBP), diastolic (DBP) and mean (MAP) blood pressure, arterial oxygen pressure (PaO2), arterial carbon
dioxide pressure (PaCO2)
and oxygenation index that was calculated
by dividing PaO2
by inspired oxygen fraction (FiO2),
patients were evaluated at rest
and in the first postoperative day. The EPAP was performed with the patient in the armchair sedation,
and an arterial blood gas analysis
was collected and analyzed to
verify the PaO2,
PaCO2, SaO2 and PaO2/FiO2
values. The mask on the patient's
face was verbally stimulated to breathe
normally while applying an expiratory
resistance of 12 cmH2O
for ten minutes. Immediately
after the application of EPAP, the patients had
new blood gas analysis performed and the hemodynamics
analyzed. Results: We evaluated 58 patients for research, 41 (71%)
male and with a mean age of 54 ± 8 years. The use of EPAP in the postoperative period led to
improvement of all blood gas
variables except PaCO2.
There was an improvement in SaO2
(%) pre-EPAP 94 ± 3 and
post-EPAP 98 ± 2, PaO2/FiO2 pre-EPAP
279 ± 10 and post-EPAP 346 ± 8, PaO2
(mmHg) pre-EPAP 78 ± 8 and
post-EPAP 97 ± 7. Conclusion: We concluded that
the application of EPAP had a positive impact on oxygenation
in patients undergoing CABG
without generating adverse effects on hemodynamics.
Keywords: myocardial revascularization; respiratory function tests; intrinsic positive-pressure respiration.
Resumo
Introdução: A pressão positiva expiratória nas
vias aéreas (EPAP) é a aplicação de uma resistência expiratória para manter a
pressão positiva nas vias aéreas e também tem sido amplamente utilizada para
prevenir possíveis complicações no pós-operatório de cirurgia cardíaca. Objetivo:
Descrever o comportamento da oxigenação e hemodinâmica durante o uso de EPAP em
pacientes submetidos à cirurgia de revascularização do miocárdio (RM). Métodos:
Estudo transversal que avaliou saturação periférica de oxigênio (SpO2),
frequência cardíaca (FC), frequência respiratória (FR), pressão arterial
sistólica (PAS), diastólica (PAD) e média (PAM), pressão arterial de oxigênio
(PaO2), pressão arterial de dióxido de carbono (PaCO2) e
índice de oxigenação calculado dividindo a PaO2 pela fração
inspirada de oxigênio (FiO2), os pacientes foram avaliados em
repouso, no primeiro dia de pós-operatório. A EPAP foi realizada com o paciente
em sedestação na poltrona e uma gasometria arterial
foi coletada e analisada para verificar os valores de PaO2, PaCO2,
SaO2 e PaO2/FiO2. Foi aplicada uma resistência
expiratória de 12 cmH2O por dez minutos. Imediatamente após a
aplicação do EPAP, os pacientes tiveram nova análise gasométrica e a
hemodinâmica analisada. Resultados: 58 pacientes, 41 (71%) do sexo
masculino e com idade média de 54 ± 8 anos foram avaliados. O uso de EPAP no
pós-operatório levou à melhora de todas as variáveis gasométricas, exceto PaCO2.
Houve uma melhora na SaO2 (%) pré-EPAP 94
± 3 e pós-EPAP 98 ± 2, PaO2/FiO2 pré-EPAP
279 ± 10 e pós-EPAP 346 ± 8, PaO2 (mmHg) pré-EPAP
78 ± 8 e pós-EPAP 97 ± 7. Conclusão: Concluiu-se que a aplicação do EPAP
teve um impacto positivo na oxigenação em pacientes submetidos à RM sem gerar
efeitos adversos na hemodinâmica.
Palavras-chave: revascularização do miocárdio; testes
de função respiratória; respiração por pressão positiva intrínseca.
Introduction
Cardiovascular
diseases represent a serious public health problem in developing countries, being characterized as an epidemic due to
the rapid growth of morbidity
and mortality resulting from its occurrence [1]. Deaths from
cardiovascular diseases in Brazil
represent 32.6% of deaths, reaching 20 million in 2030 and deaths per year from cardiovascular diseases [2].
Some
conditions such as population aging, obesity, smoking, physical inactivity and systemic arterial hypertension
are important factors that predispose to the increased
incidence of these diseases [3]. One of the
alternatives to alleviate the symptoms
of these diseases is cardiac
surgery (CC), which aims to increase
survival and improve quality of life
[4].
Factors such as anesthesia, cardiopulmonary bypass (CPB), and postoperative drainage may lead to a decline in pulmonary function that causes physiological changes that affect
oxygenation [4]. Respiratory
physical therapy is essential to
this patient profile using techniques and exercises that
help reverse this condition.
Depending on the type of
patient and surgery, breathing patterns, incentive spirometry and positive end-expiratory pressure (PEEP) can be used or
associated with other types of
exercises for patient optimization [5].
PEEP
is the application
of resistance in the expiratory phase in order to maintain positive airway pressure. It is used in both
mechanical ventilation and spontaneous breathing patients. Pulmonary expansion technique with the use of positive pressure impacts the improvement of gas exchange,
optimizing oxygenation and reducing the
arterial lactate level of postoperative cardiac surgery patients [6].
Positive
Expiratory Airway Pressure (EPAP) has been widely used
in the prevention of some possible postoperative complications of cardiac surgery
with the objective of recruiting
alveoli, improving oxygen exchange and thus reducing
respiratory distress. However, its application can impact the
hemodynamics of these patients [7].
Therefore, the aim of this
study was to describe the
behavior of oxygenation and hemodynamics during the use of EPAP in patients undergoing myocardial revascularization.
Methods
This is a cross-sectional study. It was carried out at a cardiology referral hospital in the city of Feira de Santana, Bahia, from September 2017 to November 2018. The study was approved
by the Ethics
Committee of the Noble Faculty
of Feira de Santana, under the opinion number
2,002,971. All participants
signed an Informed Consent Form.
Inclusion criteria were individuals of both sexes,
aged 18 years and over and submitted
to myocardial revascularization via median sternotomy and cardiopulmonary bypass. As an exclusion factor:
intubated patients with severe pulmonary
disease, hemodynamically unstable (mean blood pressure < 70 mmHg and > 100 mmHg, systolic blood pressure < 100 mmHg, fracture or surgery
on the face that prevented mask placement, claustrophobia, arrhythmias,
medical contraindication for the
procedure and individuals who did not
cooperate or did not understand
the proposed technique.
Patients were evaluated at rest
and at the
time of intervention on the first
postoperative day. With the patient
in armchair sedation, preferably before the diet, an arterial blood gas analysis
was collected and analyzed to
verify the PaO2,
PaCO2, SaO2 and PaO2/FiO2
values, and all patients wore
a 28% venturi mask. In addition, they were monitored for evaluation of hemodynamic
variables. At this time, the mask was
placed on the patient's face, which were verbally
stimulated to breathe normally while applying an expiratory resistance
of 12 cmH2O for ten
minutes. Immediately after the application of EPAP, the patients
had new blood gas analysis and
the hemodynamics analyzed.
Before, during and after the
procedure, patients who presented signs of respiratory distress, SpO2 decrease
(< 90%), RR elevation (> 30 bpm),
HR elevation (> 130 bpm),
MAP alteration (< 70 or
> 100 mmHg) and / or agitation were excluded from the
study.
For
data analysis, the SPSS 20.0 software was used. Normality was assessed using
the Shapiro-Wilk test. Numerical
variables were expressed as mean and standard deviation or median and
interquartile range. For comparison
of blood gas and hemodynamic
values before and after EPAP application was performed using the paired Student's
t test. It was considered significant when p < 0.05.
Results
During the research period, 70 patients were admitted
for cardiac surgery, 8 of whom were
excluded because three did not
understand the therapy and 4 had
a medical contraindication. 58 patients
were included in the study, 41 (71%) male and mean age 54 ± 8 years. The other clinical and surgical
data in table I.
The
application of EPAP in the postoperative period resulted in improvement of all blood gas
variables except PaCO2
(Table II).
The
application of positive pressure caused a change in hemodynamic variables, but without statistical significance and not related to
adverse events. The values
are shown in table III.
Table
I - Clinical
and surgical data of the studied
patients
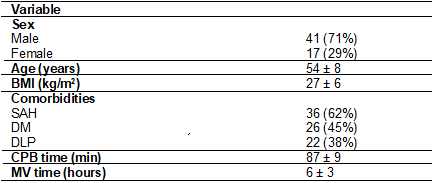
BMI
= Body Mass Index; MR = Myocardial
Revascularization; TV = Valve
Exchange; SAH = Systemic Arterial Hypertension;
DM = Diabetes Mellitus; DLP = dyslipidemia; CPB = Extracorporeal Circulation; VM = Mechanical Ventilation
Table II - Behavior of oxygenation variables in patients undergoing EPAP
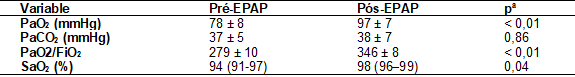
A
= Paired Student's t-test; PaO2 - Arterial Oxygen
Pressure; PaCO2 - Carbon
Dioxide Blood Pressure; SaO2 - Arterial Oxygen
Saturation
Table III - Hemodynamic behavior of patients
submitted to EPAP application
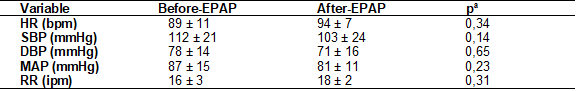
A
= Paired Student's t-test; HR - Heart Rate; SBP = systolic
blood pressure; DBP = Diastolic Blood Pressure; MAP = Mean Arterial Pressure; bpm = beats per minute;
mmHg = millimeters of mercury
Discussion
In
the present study, it was observed
that the effects of Expiratory
Positive Pressure (EPAP) on
the airways on oxygenation in patients undergoing cardiac surgery improved all postoperative
oxygenation variables, including partial oxygen pressure (PaO2)
and oxygen saturation (SaO2), but
without impact on hemodynamics.
Haeffner et al. [8], who
evaluated the use of ventilatory-associated EPAP in
patients undergoing myocardial revascularization surgery, reported that by analyzing
the pulmonary variables studied, there was a significant
improvement in pulmonary function within 30 days in the group
using the EPAP mask, when compared
to baseline values, whereas in the control group there
was no restoration of pulmonary function
after surgery. In general, the use of EPAP promotes, at the
physiological level, improvement of gas exchange due
to the recruitment
of collapsed alveoli, leading to increased pulmonary
expansion, so its application in bedridden patients accelerates the restructuring of pulmonary function,
decreasing the time in
hospital beds as well as the repercussions related to this
state.
The
period of effects of EPAP therapy on the
variables oxygen saturation, respiratory rate and heart rate was analyzed in nine patients with acute
myocardial infarction within 72 hours. In this study, with PEEP up to 10 cmH2O, the heart and
respiratory rates before and after the
use of EPAP both showed no clinical difference, but promoted increased oxygen saturation levels [9].
According to Cordeiro et
al. [7] the use of 12 cmH2O
pressure increased PaO2
without significance, and such significance
was only achieved when the
authors used a PEEP of 15 cmH2O. In our study, the 12 cmH2O
PEEP was sufficient to significantly increase this value,
this difference may be due
to the fact
that in the study this PEEP was used in noninvasive
ventilation.
During CPAP application
in patients, after cardiac surgery in the ward, evidenced
that PaO2 showed
a reduction when compared only with
oxygen utilization [10].
The difference may have been due
to the type
of environment, as the first study
was performed in the ward and
ours in the ICU. Another difference may have been
due to the
excessive use of oxygen used by
the oxygen therapy group [10].
Lima
et al. [11] found no gas
changes in myocardial revascularization surgeries, but significant changes were observed
in the present study. This difference
may or may
not be related
to the load
imposed on the PEEP, in the study by Lima et al. [11] the PEEP was 10 cmH2O,
in which 12 cmH2O was
used. The use of PEEP makes
sense primarily because it recruits unstable alveoli and improves gas exchange, but in a large clinical study using high PEEP (12 cmH2O)
and recruitment maneuvers during open abdominal surgery, no protection against postoperative pulmonary complications was found operative
[12].
Correlating similar studies,
it was evidenced by Setak-Berenjestanaki [13] research that the
use of 10 cmH2O PEEP in patients with mechanical
ventilation in the ICU after CC can lead to a significant reduction in the risk rate with incidence of atelectasis
taking into account alveolar recruitment and redistribution of extravascular fluid. Already in a second similar study [14] on the effect
of positive pressure, it
shows that the PEEP of 8 cmH2O and 5 cmH2O
had no significant effect on reducing
this incidence. In the related research
for improvement in all oxygenation variables, using PEEP of 12 cmH2O,
it is suggestive of a lower risk
rate in atelectatic conditions.
In
postoperative cardiac surgery patients, it was found that
the application of a 10 cmH2O EPAP was
associated with a small increase in mean and pulmonary
arterial pressures, pulmonary
artery occlusion pressure and central venous pressure [15]. In our study there
was an increase
in heart rate, while SBP,
DBP and MAP decreased, but without significance
even with the use of higher
pressures. Possibly, between studies, variations may be related to
the use of vasoactive drugs, although during the intervention there was no increase
in drugs, but the flow they
were using may have contributed
to the maintenance
of hemodynamic variables.
In
another study, 10 cmH2O
PEEP was used in postoperative cardiac surgery patients, in their results there
was a decrease in cardiac output, increased central
venous pressure and systolic volume variation, but had little effect
on blood pressure mean and
HR. In our study, we also observed
a slight decrease in hemodynamic parameters with higher PEEP. Theoretically, this decrease in CD may have been due
to the effect
of decreased venous return and
decreased right ventricular
preload that may limit hemodynamic
elevations [16].
Thofehrn et al. [17] applied,
in patients with congestive insufficiency, the six-minute walk test and
20 cmH2O EPAP, generating changes
in hemodynamic variables.
In our study, a lower pressure was used, which
caused a change in the variables. This result may
have been generated due to
the pressure level that was
not so high, that is, the
higher the applied pressure level, the greater
the volume of the alveolus reached
and the subsequent
increase in transpulmonary pressure and interalveolar pressure at the
end of expiration
[18,19].
In
our study, we used 12 cmH2O PEEP and no statistical significance was observed in hemodynamic parameters. These effects generated by the application
of EPAP, regardless of the blood
pressure level, can be explained
by increased intrathoracic pressure, compression of the superior and inferior vena cava, decreased atrial and ventricular filling and, consequently, reduced cardiac output [20].
It
was analyzed in our study that
the use of PEEP in patients in the postoperative period of CHD is a safe and well-tolerated technique, since it did not cause any
adverse events or hemodynamic repercussions. The effects caused by PEEP are integrated responses
in the central nervous
system, triggering the activation of the
sympathetic and parasympathetic systems, which modulate the cardiovascular
system, especially BP and
HR [21,22].
Conclusion
We concluded that
the application of EPAP had a positive impact on oxygenation
in patients undergoing myocardial revascularization without adverse effects on hemodynamics.
Potencial
conflict of interest
No
potential conflicts of interest relevant
to this article
have been reported.
Financing source
There were no external funding sources for this study.
Authors´contribution
Conception and
research design: Cordeiro ALB, Andrade JB, Santos LT,
Silva ATA, Pedreira AES; Data collection:
Cordeiro ALB, Andrade JB, Santos LT, Silva ATA, Pedreira AES; Data analysis and interpretation:
Cordeiro ALB; Writing of
the manuscript: Cordeiro
ALB, Andrade JB, Santos LT, Silva ATA, Pedreira AES; Critical
review of the manuscript for important intellectual content: Cordeiro
ALB, Guimarães ARF, Ferreira GVD, Soares LO
References
- Santos
JAA, Calles ACN. Uso da realidade virtual na
reabilitação de pacientes submetidos à cirurgia cardíaca: uma revisão. Ciências
Biológicas e de Saúde Unit 2017;2(edição):83-96. Available
from: https://core.ac.uk/download/pdf/230434476.pdf
- Beccaria LM, Cesarino
BC, Werneck AL, Correio NCG, Correio KSS, Correio MNM. Complicações
pós-operatórias em pacientes submetidos à cirurgia cardíaca em hospital de
ensino. Rev Arq Ciênc Saúde 2015;22(3):37-41. doi: 10.17696/2318-3691.22.3.2015.216 [Crossref]
- Cordeiro
ALL, Amorim NM, Andrade PH, Esquivel MS, Guimarães AR, Melo TA, et al.
Alterações fisiológicas da caminhada e tempo de internamento no pós-operatório
de cirurgia cardíaca. Int J Cardiovasc
Sci 2015;28:480-6. doi: 10.5935/2359-4802.20150068 [Crossref]
- Soares
JL, Souza AMB, Medeiro JS. Physiotherapeutic treatment at the
postoperative cardiac surgery: integrative review.
Revista Ciência e Saberes [Internet]. 2017 [cited
2021 Dec 6];3:624-9. Available from: https://www.facema.edu.br/ojs/index.php/ReOnFacema/article/view/191
- Graetz JP, Moreno MA. Efeito da aplicação da pressão positiva expiratória final no pós-operatório de revascularização do miocárdio. Fisioter Pesqui 2015;1:17-22. doi: 10.590/1809-2950/12525722012015 [Crossref]
- Oliveira SS, Neto M, Junior RA. Expansion pulmonary therapy in blood oxygenation and lactate serum level in postoperative cardiac surgery. Int J Cardiovasc Sci 2018;1:63-70. doi: 10.5935/2359-4802.20170092 [Crossref]
- Cordeiro ALL, Gruska CA, Ysla P, Queiroz A, Nogueira SCO, Leite MC, et al. Effect of different levels of PEEP on oxygenation during non-invasive ventilation in patients submitted to CABG surgery: randomized clinical trial. Braz J Cardiovasc Surg 2017;4:295-300. doi: 10.21470/1678-9741-2016-0038 [Crossref]
- Haeffener MP, Ferreira GM, Barreto SSM, Arena R, Dall’Ago P. Incentive spirometry with expiratory positive airway pressure reduces pulmonary complications, improves pulmonary function and 6-minute walk distance in patients undergoing coronary artery bypass graft surgery. Am Heart J 2008;156(5):900. doi: 10.1016/j.ahj.2008.08.006 [Crossref]
- Spigolon N, Ambrozin
A, Carvalho G, Caminha P. Aplicação do EPAP em pacientes com infarto agudo do
miocárdio. Rev Bras Fisioter 2004;Supl185.
- Olper L, Bignami E, Di Prima AL, Albini S, Nascimbene S, Cabrini L, et al. Continuous positive airway pressure versus oxygen therapy in the cardiac surgical ward: a randomized trial. J Cardiothorac Vasc Anesth 2017;31(1):115-21. doi: 10.1053/j.jvca.2016.08.007 [Crossref]
- Lima RO, Borges DL, Costa MA, Baldez TE, Barbosa, Silva MG, et al. Relationship between pre-extubation positive end-expiratory pressure and oxygenation after coronary artery bypass grafting. Rev Bras Cir Cardiovasc 2015;30(4):443-8. doi: 10.5935/1678-9741.20150044 [Crossref]
- Bugedo G, Retamal J, Bruhn A. O uso de níveis altos de PEEP previne a lesão pulmonar induzida pelo ventilador? Rev Bras Ter Intensiva 2017;29(2):231-7. doi: 10.5935/0103-507X.20170032 [Crossref]
- Setak-Berenjestanaki M, Bagheri-Nesami
M, Baradari GA, Mousavinasab
SN, Ghaffari R, Darbeheshti
M. The prophylactic effect of different levels
of positive endexpiratory pressure on the
incidence rate of atelectasis after cardiac surgery: a randomized controlled trial. Med J Islam
Repub Iran [Internet] 2018 [cited
2021 Dec 6];10;32:20. Available from:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6108254/
- Manzano F, Fernández-Mondéjar E, Colmenero M, Poyatos ME, Rivera R, Machado J, et al. Positive-end expiratory pressure reduces incidence of ventilator-associated pneumonia in nonhypoxemic patients. Crit Care Med 2008;36(8):2225-31. doi: 10.1097/CCM.0b013e31817b8a92 [Crossref]
- Sena ACBS, Ribeiro SP, Condessa RL, Vieira SRR. Pressão expiratória positiva na via aérea por máscara facial na hemodinâmica de pós-operatórios cardíacos. Arq Bras Cardiol 2010;5:594-9. doi: 10.1590/S0066-782X2010005000128 [Crossref]
- Geerts BF, Aarts LPHJ, Groeneveld AB, Jansen JRC. Predicting cardiac output responses to passive leg raising by a PEEP-induced increase in central venous pressure, in cardiac surgery patients. Br J Anaesth 2011;2:150-6. doi: 10.1093/bja/aer125 [Crossref]
- Thofehrn C, Coutinho MSSA, Daros CB, Assis AV, Lima RM, Bonin CDB, Benetti M. Efeitos da aplicação da EPAP (expiratory positive airway pressure) sobre a tolerância ao esforço em pacientes portadores de insuficiência cardíaca. Rev Bras Med Esporte 2013;19(2). doi: 10.1590/S1517-86922013000200002 [Crossref]
- Arena R, Myers J, Aslam SS, Varughese EB, Peberdy MA. Technical considerations related to the minute ventilation/carbon dioxide output slope in patients with heart failure. Chest J 2003;2:720-7. doi: 10.1378/chest.124.2.720 [Crossref]
- Renault JA, Costa VR, Rosseti MB. Fisioterapia respiratória na disfunção pulmonar pós-cirurgia cardíaca. Rev Bras Cir Cardiovasc 2008;4:562-9. doi: 10.1590/S0102-76382008000400018 [Crossref]
- Pissinato IG, Karstenm
M, Neves LMT, Minatel V, Silva AB, Catai AM. Pressão expiratória positiva nas
vias aéreas não reproduz as respostas de frequência cardíaca à manobra de Valsalva em homens jovens saudáveis. Fisioter
Pesqui 2012;2:178-84. doi: 10.1590/S1809-29502012000200015 [Crossref]
- Marães VRFS, Santos MDB, Catai AM, Moraes FR,
Oliveira L, Gallo JL, et al. Modulação do sistema
nervoso autonômico na resposta da frequência cardíaca em repouso e à manobra de
Valsalva com incremento da idade. Rev
Bras Fisioter [Internet]
2004 [cited 2021 Dec 6];2:97-103. Available from:
https://pesquisa.bvsalud.org/portal/resource/pt/lil-384557
- Looga R. The Valsalva Manoeuvre – cardiovascular effects and performance technique: a critical review. Respir Physiol Neurobiol 2005;1(edição):39-49. doi: 10.1016/j.resp.2005.01.003 [Crossref]