Fisioter
Bras 2021;22(6):881-894
ORIGINAL
ARTICLE
Distance from home to rehabilitation center did not influence
adherence to pulmonary rehabilitation program: a retrospective study
A
distância entre o domicílio e o centro de reabilitação não influencia a adesão
ao programa de reabilitação pulmonar: um estudo retrospectivo
Juliana
Ribeiro Fonseca Franco de Macedo*, Giuseppe Liistro, D.Sc.**, Thierry Pieters, M.Sc.**, Gilles Caty, D.Sc.***, Gregory Reychler, D.Sc.****
*Doctorant at Université
Catholique de Louvain, Institut de Recherche Expérimentale et Clinique (IREC), Pôle
de Pneumologie, ORL & Dermatologie ;
Service de Pneumologie, Cliniques universitaires
Saint-Luc, **Institut de Recherche
Expérimentale et Clinique (IREC), Pôle
de Pneumologie, ORL & Dermatologie,
Service de Pneumologie, Cliniques universitaires
Saint-Luc, ***Service de Médecine Physique
et Réadaptation, CHwapi asbl, ****Institut de Recherche Expérimentale et Clinique
(IREC), Pôle de Pneumologie,
ORL & Dermatologie, Service de Pneumologie, Cliniques universitaires
Saint-Luc; Haute Ecole Leonard de Vinci, Institut d’Enseignement Supérieur Parnasse-Deux Alice
Received: October 10, 2021 ; Accepted : November 18, 2021.
Correspondence: Juliana Ribeiro Fonseca Franco de
Macedo, Service de Pneumologie, Cliniques Universitaires Sain-Luc, Avenue Hippocrate 10, 1200 Brussels, Belgium
Juliana
Ribeiro Fonseca Franco de Macedo: juliana.ribeiro@uclouvain.be
Giuseppe
Liistro: giuseppe.liistro@uclouvain.be
Thierry
Pieters: thierry.pieters@uclouvain.be
Gilles
Caty: gilles.caty@chwapi.be
Gregory
Reychler: gregory.reychler@uclouvain.be
Abstract
Background: Adherence to treatment is
critical when dealing with chronic
diseases. One of the difficulties
in maintain long-term adherence is the
distance from home to rehabilitation center. Objective: To determine the influence of
the distance from subjects’ residence to rehabilitation
center on adherence of a 12-week pulmonary rehabilitation program in chronic respiratory disease. Methods: This retrospective study analyzed patients’ medical records with chronic respiratory
diseases from a pulmonary rehabilitation center. Driving distance between patients’ home and rehabilitation center was calculated with Google maps. The home-rehabilitation center distances were classified in three levels: up
to 10, 10-30 and more than 30 km. Results: 280
medical records from patients with chronic
pulmonary diseases with medical indication to follow the pulmonary
rehabilitation program were found and
148 medical records were included in our study. Out of them,
the majority (n = 93) had chronic obstructive
pulmonary disease (COPD). Seventy percent of patients lived
up to 10 km, 24% lived between 10 and 30 km and 6% lived more than 30 km. No difference in adherence was found comparing
the three groups based on
the distance from home to rehabilitation
center. Conclusion: In this
study, distance between home and rehabilitation center did not influence adherence
to pulmonary rehabilitation program.
Keywords: treatment adherence; rehabilitation; pulmonary disease; chronic obstructive.
Resumo
Introdução: A adesão ao tratamento é um aspecto
crítico quando se lida com doenças crônicas. Uma das dificuldades para manter a
adesão a longo prazo é a distância entre o domicílio do paciente e o centro de
reabilitação. Objetivo: Determinar a influência da distância na adesão a
um programa de reabilitação pulmonar de 12 semanas para pacientes com doenças
respiratórias crônicas. Métodos: Este estudo retrospectivo analisou os
registros médicos dos pacientes com doenças respiratórias crônicas de um centro
de reabilitação pulmonar. A distância foi calculada com o Google mapas e foram
classificadas em três níveis: até 10 km, entre 10 e 30 e mais de 30 km.
Resultados: Foram encontrados 280 registros médicos de pacientes com indicação
para acompanhar o programa de reabilitação pulmonar e 148 foram incluídos em
nosso estudo. Destes, a maioria (n = 93) tinha doença pulmonar obstrutiva
crônica (DPOC); 70% dos pacientes viviam até 10 km, 24% viviam entre 10 e 30 km
e 6% viviam mais de 30 km. Não foi encontrada diferença na adesão comparando os
três grupos com base na distância. Conclusão: A distância entre o
domicílio do paciente e o centro de reabilitação não influenciou a adesão ao
programa de reabilitação pulmonar.
Palavras-chave: adesão ao tratamento; reabilitação;
doença pulmonar obstrutiva crônica.
Introduction
The
chronic obstructive pulmonary disease (COPD) is the most
prevalent chronic respiratory disease [1] with global prevalence around 12.16% [2]. The COPD was responsible by 3.23 million of death worldwide in 2019 [2]. An essential component of the integrate
care of patients
with chronic respiratory diseases is the pulmonary
rehabilitation program
(PRP) which has as benefits the reduction
of patients’ symptoms and hospitalizations,
the improvement of exercise capacity,
limb muscle strength and endurance,
emotional function, quality of life
and the enhancement
of knowledge and self-efficacy [3,4,5,6,7,8,9,10,11,12].
Despite these important benefits, many patients do not follow the program [7,9,13,14,15,16,17]. Adherence is defined as “the extent to
which a patient’s behavior coincides with medical advice” [18,19] and is influenced by
a set of personal and environmental determinants that enables the free
choice of people to adopt
certain recommendations, thus becoming co-responsible
on their treatment [20,21]. Adherence to treatment is
critical for managing a chronic disease. Adherence to general long-term care in developed countries is around 30 to 50% and in developing countries,
rates are even smaller
[22,23,24,25]. The success of rehabilitation programs depends on the
assessment of barriers that interfere with adherence [13,22,26,27].
These barriers are classified into five domains: intra-
or interpersonal, logistical, barriers related to the
rehabilitation program and to the
health system [28]. Intrapersonal
barriers include self-reported
health [23,28,29], health beliefs, lack of
time [28], motivation [28,30], recurrent
hospital admissions [31] and
religious reasons [28,32]. Interpersonal barriers include lack of family
or social support [28,30] and work conflicts
[28]. Logistical barriers
are related to transport [3,13,28,33], distance
[28,31,34], availability of
personal or community resources [28]. Barriers related to the rehabilitation
program include services offered, group format, exercise component and perceptions
about the rehabilitation program
[28,33,35,36]. Health system barriers include lack of referral,
cost [25,28], negative experiences
with health system and language [28].
The
distance from home to rehabilitation center has been many
time suggested as one of the difficulties
in maintain long-term
(i.e.: > 12 weeks [37]) adherence
[31,33,34]. We hypothesized
that this distance may influence
the adherence to a 12-week pulmonary rehabilitation program in chronic respiratory diseases.
The
aim of this
study was to verify the
influence of the distance from
patients’ home to rehabilitation center on adherence of a 12-week pulmonary rehabilitation program in chronic respiratory diseases.
Methods
This retrospective
study analyzed all medical records from patients with
chronic respiratory diseases from the
pulmonary rehabilitation
center in Cliniques universitaires
Saint-Luc (Brussels, Belgium)
for a pre-established period
of 45 months. The study was approval
by local ethical committee (2020/12OCT/502).
The
pulmonary rehabilitation
center is easily accessible by public
transport and has parking facilities. The indications to be part of
the program are all chronic respiratory
diseases with reduced exercise tolerance and restriction
in daily live activities, and future or recent lung
surgery. The program is tailored to
the patients’ capacities and objectives are identified during the initial
assessment. The patients are accompanied
by a team including physician, pulmonologist, physiotherapist, occupational therapist, social worker, psychological and nutritional therapists. The rehabilitation program lasts six
months with three weekly sessions
of one hour. Educational sessions are included once a month.
All patients who
started and completed 12 weeks of PRP were included
in this retrospective study and were
divided in three groups considering the home-rehabilitation distance (up to
10 km, between 10 and 30 km
and more than 30 km). Patients who presented
exacerbation and were hospitalized during the PRP period were excluded
from the study. The adherence rate was determined based on the
frequency with which the patients
attended the 12 weeks of rehabilitation
program, i.e.:
[(number of attended sessions
/ number of planned sessions of treatment) * 100] [24,38]
Then the rate was compared between
each group. Data on lung function
and functional exercise capacity were correlated with adherence.
Descriptive analysis was performed
for patients’ background (age, weight,
height, lung function volumes and six-minute walk test (6MWT)) using mean and standard deviation. The means were compared by
an analysis of variance. Tukey-Kramer
method was used for post-hoc comparisons. Correlations were analyzed by the
Pearson correlation coefficient.
The cutoff points used to interpret Pearson's
correlation were: negligible correlation (0.00 –
0.10); weak correlation
(0.10 – 0.39); moderate (0.40 – 0.69); strong (0.70 – 0.89) and very strong correlation
(0.90 – 1.00) [39].
All statistical analyses
were performed using SPSS 25.0 (IBM Software, Minneapolis, Arizona). A significance level of 5% probability was established.
Results
Two hundred eighty
chronic subjects presented a clinical indication to follow the PRP. One hundred
forty-eight medical records
were included in the study. Sixty-two
medical records did not fulfill the
inclusion criteria (to start and to
follow a minimum of twelve weeks of
PRP). Seventy medical records
were excluded due to medical problems (exacerbations, hospitalizations) during the PRP period. The recruitment process is shown in figure 1.
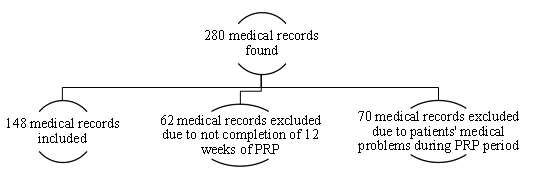
Figure
1 - Flowchart describing the included and excluded
medical records
Sample
characteristics are shown
in table I. Out of the 148 subjects, 93 subjects had chronic
obstructive pulmonary disease (COPD); 21 interstitial lung diseases; 2 diaphragmatic paralysis; 1 bronchiectasis; 9 obstructive sleep apnea syndrome;
4 pulmonary arterial hypertension;
4 lung cancer without surgery; 3 lobectomy due to
lung cancer; 2 hypoventilation related to obesity; 2 neuromuscular disease; 4 asthma; 1 lung transplant; 1 respiratory failure; 1 acquired immune deficiency syndrome.
Table
I - Characterization
of the sample
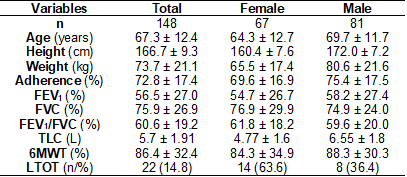
Values expressed as mean ± standard deviation; L = liters; FEV1 = forced expiratory volume in one second; FVC = forced vital capacity; TLC = total lung capacity; 6MWT = six-minute walk test; LTOT = long-term oxygen therapy
The
functional exercise capacity in admission was good with
the walked distance covered in the 6MWT over 80% of the predicted value
[40] in our general sample (shown
in table I). It was not different depending
on the group
based on the distance from
the subjects’ residence to the
rehabilitation center (shown
in table II).
The
mean age, adherence, forced expiratory volume in one second (FEV1), 6MWT and the number
of long-term oxygen therapy for each group based
on distance from subjects’ residence to rehabilitation
center are shown in table
II.
Table
II - Comparison between the distance from
patients’ residence to rehabilitation center and age, adherence, FEV1, 6MWT and LTOT
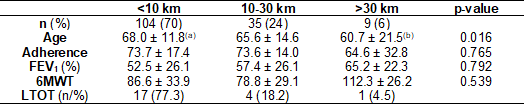
Values expressed as mean ± standard deviation; km = kilometers; FEV1 = forced expiratory volume in one second; 6MWT = six-minute walk test; LTOT = long-term oxygen therapy; p-value between (a) and (b) = 0.011
Most of them (70%) lived up to 10km distance
from the rehabilitation center. The number
of patients decreased as the driving distance increased. The driving distance did not
influence the adherence (p = 0.77) in this group of patients.
Neither the walked distance during the 6MWT (p = 0.54) nor FEV1 (p = 0.79) were different between groups based on
the driving distance.
There was a significant difference when comparing the age between the groups (p = 0.016). This difference was present among
patients living more than
30 km away (60.7 y.o. ±
21.5) compared to patients living up to 10 km away (68.0 y.o. ± 11.8) (p = 0.016), patients
living further away were younger. There
was no significant difference when comparing the age between the groups
living up to 10 km away with those
living between 10-30 km (p = 0.76) as well as those living between 10-30 km with those living more than 30 km (p =
0.15) (table II).
The
adherence rate was neither correlated to the distance
from patients’ home to rehabilitation center (r =
0.028; p = 0.74), 6MWT (r = -0.069; p = 0.44) nor
FEV1 (r = 0.020; p = 0.82) (figure 2).
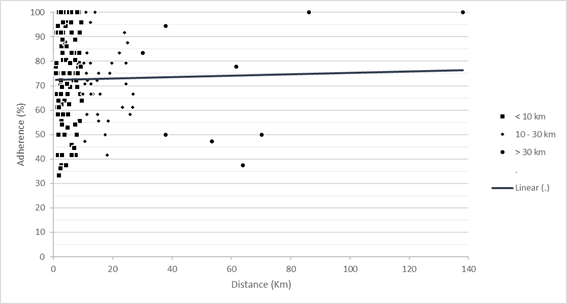
Figure
2 - Correlation
between adherence and distance
Discussion
The
literature has indicated that most dropouts in rehabilitation programs occur during the
first three months with dropout
rate ranging from 30 to 50% [22,31], with similar results in all age groups, regardless of gender [41]. It can be explained
by the fact
that we considered
only subjects who attended at
least 12 weeks of rehabilitation program. Then, patients who had
clinical indication of pulmonary rehabilitation,
but who did
not start the program, were not
considered in our study.
In
this retrospective analysis, it was demonstrated that there is no relationship
between adherence to the pulmonary
rehabilitation program and distance from
home to the rehabilitation center. Of the 148 patients included in this study, nine (6%) lived more than 30 km away. We think, then,
probably subjects who live far
from the rehabilitation center and accept to follow the program are, then, adherent. Probably, those who hesitate due
to distance do not even start the program. To
verify whether this hypothesis is confirmed, it was decided to
analyze the distances from home to the rehabilitation
center of the 62 patients who did
not meet the inclusion criteria,
i.e., did not complete the 12 weeks of
the rehabilitation program to be
included in this study. Our intention
was to verify
if these 62 patients lived far enough away
to abandon the rehabilitation program and the
distance would then be an
influential factor of adherence by
doing these subjects not even
starting the program or abandoning
it in the first sessions. When we analyzed these
patients, it was seen that most
of them (81%) lived up to
10 km from the rehabilitation center and only 6.4% lived more than 30 km away. This means that
the distance does not explain the
non-adherence of these patients to the rehabilitation
program.
In
this study, the driving distance
did not influence
the adherence to the program,
as we did not find difference
between groups according to the
distances. This finding is in accordance
with previous studies [22,26,31]. One study [22] compared adherence and distance
by analyzing 796 medical records of patients
in general rehabilitation programs.
Their medical conditions included cardiorespiratory diseases, cancers, obesity and/or
diabetes. The rehabilitation program
was similar to our study regarding
the frequency (three to six
times a week) and patients had freedom
of choice of days and
times to attend the sessions. In this study, distance
also did not influence adherence
(p = 0.41). Other study [31] investigated
which physiological or environmental factors could predict
the participation in a pulmonary rehabilitation program. It was also a retrospective analysis with 243 patients (204 COPD; 28 COPD and asthma and 11 had
asthma) who followed two kinds
(short and long) of rehabilitation program. The short one included three sessions per week for 6 weeks and the
long one, one session per week for 18 weeks. Long and short programs had identical
content and format, each session
lasting for approximately two hours and included
educational activities, individualized exercise prescription, and educational sessions addressing the psychological aspects of chronic disability.
In this study, distance also did
not influence adherence (p = 0.55).
One study [25] retrospectively
identified variables related to adherence
in a lung rehabilitation program in Argentina. The authors
analyzed 388 medical records
and found a significant relationship between adherence and distance (p = 0.002). They considered the cut-off point of the distance
of 10 km, then analyzed the adherence
of patients who lived more or less than
10 km from the hospital. Patients who lived
more than 10 km to reach the hospital were less adherent,
the authors suggested that this non-adherence may also be
related to socioeconomic factors. The socioeconomic profile of our patients was
not analyzed because data to perform such analysis
was not available.
A possible explanation for the difference in the results between
our study and the Boim’s
et al. study [25] is
that our patients had higher
lung function values (FEV1 - 56.5% ± 27.0) when
compared to that of their
study (39.6% ± 17) and also the duration
of rehabilitation program was different.
We analyzed the adherence for 12 weeks and then,
for 16 weeks, these 4 extra
weeks may have made the
difference in this case.
A
relationship between FEV1 and adherence was
not found. The FEV1 ranged from 52% of the predicted
value for patients living up to 10 km to
65% for patients living over 30 km (p = 0.79). This means that
our patients did not have
a high degree of airway obstruction. Similar to ours, four previous
studies [25,29,31,42] were carried out with most COPD patients. One of them
[31] was a retrospective analysis with 243 patients (COPD and/or asthma) who
followed a short (6 weeks) or a long (18 weeks)
rehabilitation program. The
program was similar to our program,
except the duration of each
session which was approximately two hours, twice as much as ours. The mean FEV1 of patients
in this study was 39.1% ± 17 for adherents and 36.4% ± 15 for non-adherents,
they also found no significant difference in correlating FEV1 with adherence (p = 0.39). Another study [42] was similar to our study in terms
of duration of each session,
length of the program and
exercise types. They included only
patients with COPD (n =
217). In our sample this pathology affected 58% of our sample. General parameters of disease
severity, such as FEV1 did not differ
among patients who complete the entire program compared to those
who stopped the program (p = 0.44).
Conversely, Sahin et Naz [13] and Heerema-Poelman
[43] found a relationship between FEV1 and adherence. The first study [13] aimed to determine the reasons why patients
with COPD completed or failed to
complete the pulmonary rehabilitation program. They included 359 patients with COPD and out of them,
147 did not complete the program. The group of patients
who did not
complete the program had significantly lower FEV1 (p = 0.024) and significantly lower walked distance (p = 0.001). The second one [43] analyzed the adherence
of 70 patients with COPD during a one-year rehabilitation program. They found
a significant difference between FEV1 values from adherents’ patients comparing to non-adherents (p = 0.37). In both studies, the
patients had worse lung function
(FEV1 = 39% [13] and 35% [43] when
compared to our patients (FEV1 = 56%).
In
this study, the functional exercise capacity measured by the
6MWT was greater than 78% of the
predicted value regardless of the
group. Two studies [29,42] conducted with 1218 [29] and 217 [42] COPD patients also did
not find a significant relationship between adherence and 6MWT (p = 0.90 [29]; p = 0.53 [42]). One study [13] aimed to compare demographic and clinical characteristics of patients with
COPD who complete and fail to complete pulmonary rehabilitation program. They found
a statistically significant
difference between adherence and the
walk distance measured by the
6MWT (p = 0.001). The number of
subjects receiving long-term oxygen treatment in this study was higher
(n = 80) than in our study (n = 22), this may probably explain
the differences between our studies.
We decided to
analyze FEV1 and 6MWT values of the
62 patients who did not complete the 12 weeks of
rehabilitation to be included in the study. Our
intention was to verify whether
the functional exercise capacity and/or level
of obstruction of these patients
could explain the non-participation or abandonment before the first
twelve weeks of the program.
Regarding FEV1, subjects who lived more than 30 km away had higher FEV1 (81.4 ± 17.0) when compared to
subjects living up to 10 km away (61.2 ± 23.3). Regarding physical capacity, subjects who lived more than 30 km also presented higher values in the 6MWT (103.1 ± 2.4) when compared to
those who lived up to
10 km away (71.7 ± 36.1).
The
limitation of this research was
the use of data coming only from
the medical records of the patients
followed in our hospital, therefore, we do not have data if
they have been absent from
the program due to hospitalization
in other hospitals than ours. To
minimize the risk of bias in patients not included in the study, we
analyzed the distance traveled, the FEV1, and the
6MWT. The patients of this study have
several pathologies where the degree
of commitment may differ and
influence or not the adherence.
Although we had zip code data to calculate the
distance, we did not have
information about the socioeconomic profile of subjects, this
factor may influence adherence. We considered the
distance in relation to the length
in kilometers, we did not consider
the time required to cover this distance,
which may influence adherence. However, the advantage
of this retrospective
methodology is linked to the
fact that the subjects does not know that
their presence or absence is
being verified and therefore, the adherence is
not influenced by the fact
that he knows
that he is
part of a research on adherence.
Conclusion
The
results of this study indicate
that for such a program (12 weeks with fixed exercising
schedule), the distance between the subjects’
residence and the rehabilitation center had no effect on
adherence to pulmonary rehabilitation program when they
accept to participate.
Statement of
ethics
The
study was approval by Comité d’Ethique Hospitalo-Facultaire
Saint-Luc – UCLouvain (2020/12OCT/502).
Conflict of
interest statement
The
authors declare no conflict
of interest.
Funding sources
One of the authors received
a grant from the Institut de Recherche Expérimentale et Clinique (Université Catholique de Louvain – Brussels, Belgium).
Authors’ contributions
Development of
the research design and concept: Macedo JRFF, Reychler G; Data collection:
Macedo JRF; Data analysis: Reychler
G; Revised for intellectual
content: Liistro G, Caty G, Pieters T. All authors approved the final version to be published.
References
- Karakaya G, Lona M, Bruyneel
L. Etude sur les maladies chroniques
en Belgique - Evolution
entre 2010 et 2018. Brussel: Mutualités Libres ;2020.
32p.
- WHO. Chronic obstructive pulmonary disease (COPD)
[Internet]. 2021. [cited 2021 Dec
7]. Available from:
https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(COPD)
- Rochester
CL, Vogiatzis I, Holland
AE, Lareau SC, Marciniuk
DD, Puhan MA, et al. An Official American Thoracic
Society/European Respiratory
Society Policy Statement: enhancing implementation, use, and delivery of pulmonary rehabilitation. Am J Respir Crit
Care Med
2015;192(11):1373-86. doi: 10.1164/rccm.201510-1966ST [Crossref]
- Hansen H, Bieler T, Beyer N, Kallemose T, Wilcke JT, Østergaard LM, et al. Supervised pulmonarytele-rehabilitation versus pulmonary rehabilitation in severe COPD: a randomised multicentre trial. Thorax 2020;75(5):413-21. doi: 10.1136/thoraxjnl-2019-214246 [Crossref]
- Vasilopoulou M, Papaioannou AI, Kaltsakas G, Louvaris Z, Chynkiamis N, Spetsioti S, et al. Home-based maintenance tele-rehabilitation reduces the risk for acute exacerbations of COPD, hospitalisations and emergency department visits. Eur Respir J 2017;49(5). doi: 10.1183/13993003.02129-2016 [Crossref]
- Collinsworth AW, Brown RM, James CS, Stanford RH, Alemayehu D, Priest EL. The impact of patient education and shared decision making on hospital readmissions for COPD. Int J Chron Obstruct Pulmon Dis 2018;13:1325-32. doi: 10.2147/copd.S154414 [Crossref]
- Barker RE, Jones SE, Banya W, Fleming S, Kon SSC, Clarke SF, et al. The Effects of a video intervention on posthospitalization pulmonary rehabilitation uptake. A randomized controlled trial. Am J Respir Crit Care Med 2020;201(12):1517-24. doi: 10.1164/rccm.201909-1878OC [Crossref]
- Güell MR, Cejudo P, Ortega F, Puy MC, Rodríguez-Trigo G, Pijoan JI, et al. Benefits of long-term pulmonary rehabilitation maintenance program in patients with severe chronic obstructive pulmonary disease. three-year follow-up. Am J Respir Crit Care Med 2017;195(5):622-9. doi: 10.1164/rccm.201603-0602OC [Crossref]
- Luhr K, Eldh AC, Theander K, Holmefur M. Effects of a self-management programme on patient participation in patients with chronic heart failure or chronic obstructive pulmonary disease: A randomized controlled trial. Eur J Cardiovasc Nurs 2019;18(3):185-93. doi: 10.1177/1474515118804126 [Crossref]
- Aboumatar H, Naqibuddin M, Chung S, Chaudhry H, Kim SW, Saunders J, et al. Effect of a hospital-initiated program combining transitional care and long-term self-management support on outcomes of patients hospitalized with chronic obstructive pulmonary disease: A randomized clinical trial. Jama 2019;322(14):1371-80. doi: 10.1001/jama.2019.11982 [Crossref]
- Rinaldo N, Bacchi E, Coratella G, Vitali F, Milanese C, Rossi A, et al. Effects of combined aerobic-strength training vs fitness education program in COPD patients. Int J Sports Med 2017;38(13):1001-8. doi: 10.1055/s-0043-112339 [Crossref]
- Benzer W, Rauch B, Schmid J-P, Zwisler AD, Dendale P, Davos CH, et al. Exercise-based cardiacrehabilitation in twelve European countries results of the European cardiac rehabilitation registry. Int J Cardiol 2017;228:58-67. doi: 10.1016/j.ijcard.2016.11.059 [Crossref]
- Sahin H, Naz I. Why are COPD patients unable to complete the outpatient pulmonary rehabilitation program? Chron Respir Dis 2018;15(4):411-8. doi: 10.1177/1479972318767206 [Crossref]
- Benzo RP, Kramer KM, Hoult JP, Anderson PM, Begue IM, Seifert SJ. Development and feasibility of a home pulmonary rehabilitation program with health coaching. Respir Care 2018;63(2):131-40. doi: 10.1016/j.ijcard.2016.11.059 [Crossref]
- White P, Gilworth G, Lewin S, Hogg L, Tuffnell R, Taylor SJC, et al. Improving uptake and completion of pulmonary rehabilitation in COPD with lay health workers: feasibility of a clinical trial. Int J Chron Obstruct Pulmon Dis 2019;14:631-43. doi: 10.2147/copd.S188731 [Crossref]
- Kokturk N, Polatli M, Oguzulgen IK, Saleemi S, Al Ghobain M, Khan J, et al. Adherence to COPD treatment in Turkey and Saudi Arabia: results of the ADCARE study. Int J Chron Obstruct Pulmon Dis 2018;13:1377-88. doi: 10.2147/COPD.S150411 [Crossref]
- Rogliani P, Ora J, Puxeddu E, Matera MG, Cazzola M. Adherence to COPD treatment: Myth and reality. Resp Med 2017;129:117-23. doi: 10.1016/j.rmed.2017.06.007 [Crossref]
- Andrade MB, Cespedes CV. Adherencia al tratamiento en enfermedad cardiovascular: rediseño y validación de un instrumento. Enferm Univ 2017;14(4):226-76. doi: 10.1016/j.reu.2017.10.001 [Crossref]
- López-Campos JL, Quintana Gallego E, Carrasco Hernández L. Status of and strategies for improving adherence to COPD treatment. Int J Chron Obstruct Pulmon Dis 2019;14:1503-15. doi: 10.2147/COPD.S170848 [Crossref]
- Brawley LR, Culos-Reed SN. Studying adherence to therapeutic regimens: overview, theories, recommendations. Control Clin Trials 2000;21(5 Suppl):156s-63s. doi: 10.1016/s0197-2456(00)00073-8 [Crossref]
- Bourbeau J, Bartlett SJ. Patient adherence in COPD. Thorax 2008;63(9):831-8. doi: 10.1136/thx.2007.086041 [Crossref]
- Cabral-de-Oliveira AC, Ramos PS, Araujo CG. Distance from home to exercise site did not influence the adherence of 796 participants. Arq Bras Cardiol 2012;98(6):553-8. doi: 10.1590/s0066-782x2012005000039 [Crossref]
- Pierobon A, Sini Bottelli E, Ranzini L, Bruschi C, Maestri R, Bertolotti G, et al. COPD patients' self-reported adherence, psychosocial factors and mild cognitive impairment in pulmonary rehabilitation. Int J Chron Obstruct Pulmon Dis 2017;12:2059-67. doi: 10.2147/copd.S133586 [Crossref]
- Oates GR, Hamby BW, Stepanikova I, Knight SJ, Bhatt SP, Hitchcock J, et al. Social determinants of adherence to pulmonary rehabilitation for chronic obstructive pulmonary disease. Copd 2017;14(6):610-7. doi: 10.1080/15412555.2017.1379070 [Crossref]
- Boim C, Caberlotto
O, Storni M, Cortinaz M, Monti F, Khoury M. Adherence to interdisciplinary
pulmonary rehabilitation program. Medicina (B Aires) [Internet]. 2014 [cited 2021 Dec 7];74(2):104-9. Available from:
https://pubmed.ncbi.nlm.nih.gov/24736252/
- Leira EC, Viscoli CM, Polgreen LA, Gorman M, Kernan WN. Distance from home to research center: a barrier to in-person visits but not treatment adherence in a stroke trial. Neuroepidemiology 2018;50(3-4):137-43. doi: 10.1159/000486315 [Crossref]
- Nissen L, Lindhardt T. A qualitative study of COPD-patients' experience of a telemedicine intervention. Int J Med Inform 2017;107:11-7. doi: 10.1016/j.ijmedinf.2017.08.004 [Crossref]
- Resurrección DM, Motrico E, Rigabert A, Rubio-Valera M, Conejo-Cerón S, Pastor L, et al. Barriers for nonparticipation and dropout of women in cardiac rehabilitation programs: a systematic review. J Womens Health (Larchmt) 2017;26(8):849-59. doi: 10.1089/jwh.2016.6249 [Crossref]
- Fan VS, Giardino ND, Blough DK, Kaplan RM, Ramsey SD. Costs of pulmonary rehabilitation andpredictors of adherence in the National Emphysema Treatment Trial. Copd 2008;5(2):105-16. doi: 10.1080/15412550801941190 [Crossref]
- Arnold
E, Bruton A, Ellis-Hill C. Adherence
to pulmonary rehabilitation: A qualitative study. Respir Med
2006;100(10):1716-23. doi: 10.1016/j.rmed.2006.02.007 [Crossref]
- Sabit R, Griffiths TL, Watkins AJ, Evans W, Bolton CE, Shale DJ, et al. Predictors of poor attendance at an outpatient pulmonary rehabilitation programme. Respir Med 2008;102(6):819-24. [Crossref] doi: 10.1016/j.rmed.2008.01.019 [Crossref]
- George M, Bender B. New insights to improve treatment adherence in asthma and COPD. Patient Prefer Adherence 2019;13:1325-34. doi: 10.2147/PPA.S209532 [Crossref]
- Cox NS, Oliveira CC, Lahham A, Holland AE. Pulmonary rehabilitation referral and participation are commonly influenced by environment, knowledge, and beliefs about consequences: a systematic review using the Theoretical Domains Framework. J Physiother 2017;63(2):84-93. doi: 10.1016/j.jphys.2017.02.002 [Crossref]
- Almadana Pacheco V, Pavon Masa M, Gomez-Bastero Fernandez AP, Muniz Rodriguez AM, Tallon Moreno R, Montemayor Rubio T. Patient profile of drop-outs from a pulmonary rehabilitation program. Arch Bronconeumol 2017;53(5):257-62. doi: 10.1016/j.arbres.2016.06.010 [Crossref]
- Duarte-de-Araújo A, Teixeira P, Hespanhol V, Correia-de-Sousa J. COPD: Analysing factors associated with a successful treatment. Pulmonology 2020;26(2):66-72. doi: 10.1016/j.pulmoe.2019.05.012 [Crossref]
- Kjærgaard J, Juhl CB, Lange P, Wilcke T. Adherence to early pulmonary rehabilitation after COPD exacerbation and risk of hospital readmission: a secondary analysis of the COPD-EXA-REHAB study. BMJ Open Respir Res 2020;7(1). doi: 10.1136/bmjresp-2020-000582 [Crossref]
- Verrill D, Barton C, Beasley W, Lippard WM. The effects of short-term and long-term pulmonary rehabilitation on functional capacity, perceived dyspnea, and quality of life. Chest 2005;128(2):673-83. doi: 10.1378/chest.128.2.673 [Crossref]
- Carvalho D, Castro L, Merli M, Felcar J, Vidotto L, Fujisawa D, et al. Quali-quantitative analysis ofadherence and perceived satisfaction of individuals with COPD after high-intensity training on land and in water: additional analysis from a randomized clinical trial. Fisioter Pesqui 2021;28:126-35. doi: 10.1590/1809-2950/19000628022021 [Crossref]
- Schober P, Boer C, Schwarte LA. Correlation coefficients: appropriate use and interpretation. Anesth Analg 2018;126(5):1763-8. doi: 10.1213/ane.0000000000002864 [Crossref]
- Enright PL, Sherrill DL. Reference equations for the six-minute walk in healthy adults. Am J Respir Crit Care Med 1998;158(5 Pt 1):1384-7. doi: 10.1164/ajrccm.158.5.9710086 [Crossref]
- Marcus BH, Dubbert PM, Forsyth LH, McKenzie TL, Stone EJ, Dunn AL, et al. Physical activity behavior change: issues in adoption and maintenance. Health Psychol 2000;19(1s):32-41. doi: 10.1037/0278-6133.19.suppl1.32 [Crossref]
- Fischer MJ, Scharloo M, Abbink JJ, van't Hul AJ, van Ranst D, Rudolphus A, et al. Drop-out and attendance in pulmonary rehabilitation: the role of clinical and psychosocial variables. Respir Med 2009;103(10):1564-71. doi: 10.1016/j.rmed.2008.11.020 [Crossref]
- Heerema-Poelman A, Stuive I, Wempe JB. Adherence to a maintenance exercise program 1 year afterpulmonary rehabilitation: what are the predictors of dropout? J Cardiopulm Rehabil Prev 2013;33(6):419-26. doi: 10.1097/HCR.0b013e3182a5274a [Crossref]