Fisioter Bras 2022;23(5);701-17
ORIGINAL ARTICLE
Effect of a training of pelvic muscles in group for women with urinary
incontinence: a randomized clinical test
Efeito de um
treinamento de músculos pélvicos em grupo para mulheres com incontinência
urinária: um ensaio clínico randomizado
Lia Ferla,
D.Sc.*, Caroline Darski, D.Sc.**, Luciana Laureano Paiva, D.Sc.***,
José Geraldo Lopes Ramos, D.Sc.****
*Professora no Curso de
Fisioterapia da Centro Universitário Ritter dos Reis e Pós-Graduação em
Fisioterapia Pélvica da FisioWork, Fisioterapeuta
Pélvica na CLAPA, **Professora no Curso Pós-Graduação online Fisioterapia
Obstétrica da Aprimore, Fisioterapeuta Pélvica na CLAPA, ***Professora no Curso
de Fisioterapia da Universidade Federal do Rio Grande do Sul, ****Professor no
Curso de Medicina da Universidade Federal do Rio Grande do Sul
Received: December 13,
2021; Accepted: August 31, 2022.
Correspondence: Lia Ferla,
Rua Caracas, 55 Jardim Lindóia 91050-160 Porto Alegre RS, Brazil
Lia Ferla: liaferlafisio@gmail.com
Caroline Darski: carolinedarski@outlook.com
Luciana
Laureano Paiva: lucianalaureanopaiva@gmail.com
José
Geraldo Lopes Ramos: jramos@hcpa.edu.br
Abstract
Introduction: Urinary incontinence (UI) is a problem that is often
underestimated, not receiving proper attention. Among the possibilities for
conservative treatment of UI, supervised pelvic floor muscle training (PFMT)
should be recommended as a first line of treatment for women. PFMT can be
developed in groups, individually and at home. Objective: There are
still few studies in the literature involving group PFMT with defined protocols
that can be easily understood and reproduced by the patients. The aim of this
study is to identify the effect of a group PFMT protocol compared to a PFMT
protocol at home for women with UI. Methods: This experimental blinded
randomized controlled trial followed CONSORT recommendations. The evaluation
instruments were the PERFECT scale, ICIQ-SF and PISQ-12. The main outcome was
improvement in pelvic floor muscle (PFM) function, and secondary outcomes were
improvement in quality of life (QOL) and sexual function (SF). Results:
With twelve weeks of treatment, the PFMT group protocol presented as a more
effective form of treatment for UI, since it showed improvement in the Power
and QV items. When observing the effect of the protocols, after twenty-four
weeks, both were effective only when referring to the secondary outcomes, QOL
and SF. Conclusion: It can be assumed that the group intervention, used
in this specific sample, constitutes a feasible and viable physiotherapeutic
intervention strategy, able to benefit many women with UI, besides being a tool
that is easy for patients to understand and follow.
Keywords: pelvic floor disorders; physical therapy
modalities; quality of life; sexual health; urinary incontinence, women.
Resumo
Introdução: A incontinência urinária (IU) é um
problema muitas vezes subestimado, não recebendo a devida atenção. Dentre as
possibilidades de tratamento conservador da IU, o treinamento dos músculos
do assoalho pélvico (TMAP) supervisionado deve ser recomendado como primeira
linha de tratamento para as mulheres. O TMAP pode ser
desenvolvido em grupos, individualmente e em casa. Objetivos: Ainda há
poucos estudos na literatura envolvendo TMAP em grupo com protocolos
definidos que possam ser facilmente compreendidos e reproduzidos pelos
pacientes. O objetivo deste estudo é demonstrar a eficácia de um protocolo
de TMAP em grupo comparado a
um protocolo de TMAP domiciliar para mulheres com IU. Métodos: Este foi
um estudo experimental controlado randomizado cego que seguiu as recomendações
do CONSORT. Os instrumentos de avaliação foram a
escala PERFECT, ICIQ-SF e PISQ-12. O
principal resultado foi a melhora da função dos músculos do assoalho
pélvico (MAP) e os resultados secundários foram a melhora da
qualidade de vida (QV) e da função sexual (FS). Resultados: Com
doze semanas de tratamento o protocolo do grupo TMAP apresentou-se
como uma forma de tratamento mais eficaz
para IU, pois apresentou melhora nos itens
potência e QV. Ao observar a efetividade dos protocolos, após vinte e
quatro semanas, ambos foram efetivos apenas no que se refere aos desfechos
secundários, QV e FS. Conclusão: Pode-se supor que a
intervenção em grupo, utilizada nesta amostra específica, constitui uma
estratégia de intervenção fisioterapêutica factível e viável, capaz
de beneficiar muitas mulheres com IU, além de ser uma ferramenta de fácil
compreensão e acompanhamento pelos pacientes.
Palavras-chave: distúrbios do assoalho pélvico;
modalidades de fisioterapia;
qualidade de vida; saúde
sexual; incontinência urinária, mulheres.
Introduction
Urinary incontinence (UI) is a problem that is often
underestimated, not receiving proper attention, since urinary loss can be
considered a normal condition, a result of the aging process [1]. Considering
the negative impact of UI on people's lives, and the increase in the prevalence
of this condition, it is necessary to implement actions aimed at raising
awareness, prevention, diagnosis and management of this situation, since it is
a public health problem, often accompanied by a social stigma [2].
Initial treatment for women with SUI (stress urinary
incontinence), UUI (urgency urinary incontinence) and MUI (mixed urinary
incontinence) should include appropriate lifestyle counseling, physical
therapy, a programmed urination regime, behavioral therapy, and medication [3].
Among the possibilities for conservative treatment of UI, supervised pelvic
floor muscle training (PFMT) should be recommended as a first line of treatment
for women with SUI, UUI and MUI symptoms. However, the effect of this long-term
training needs to be researched further [3,4].
FMT can be developed in groups, individually and at
home. Group and individual training are commonly supervised by a
physiotherapist. Recently Paiva et al. [5] have shown in a systematic
review that group PFMT is as effective as individual PFMT for UI, but when
compared to at-home PFMT, it is more effective [5]. Considering that group PFMT
is effective in reducing UI and is a type of intervention that may benefit a
greater number of people, it becomes a viable option to be implemented and
developed as a first line of treatment for users of the public health system.
However, there are still few studies in the literature involving group PFMT
which have well-defined protocols and are easily understood and followed by
patients. In this sense, the present study aims to identify the effect of a
group PFMT protocol compared to an at-home PFMT protocol, for women with UI.
Methods
This study presents an experimental design of the type
randomized blinded trial and follows the recommendations of CONSORT [6]. Women
between 30 and 70 years of age with UI who had had intercourse in the last 6
months were eligible for the study. In addition to not having undergone pelvic
radiotherapy and/or chemotherapy, not having delivered in the last 12 months,
not having participated in group or individual PFMT in the last 6 months,
agreeing to participate in the study and signing the Term of Informed Consent.
Patients were excluded if they had latex allergy, did not understand the
instruments used in the research and had pelvic floor muscle (PFM) contraction
at grade zero (0).
The sample was non-probabilistic by convenience, and
patients from the Gynecology and Obstetrics Outpatient Clinic of the Hospital
de Clínicas de Porto Alegre (HCPA), where the
activities of pelvic physical therapy were performed, in the city of Porto
Alegre/RS/Brazil, that met the inclusion criteria of the research were invited
to participate.
Initially, the examiner used an anamnesis form to
collect personal data. She then applied two self-administered questionnaires:
International Consultation on Incontinence Questionnaire-Short Form (ICIQ-SF)
and Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12)
[7,8]. A physical examination was performed to assess the functionality of the
pelvic floor muscles (PFM) through pressure biofeedback and vaginal palpation.
Also, at this time the participants were advised on the correct voluntary
contraction of the PFM.
Participants randomized to the PFMT group protocol
performed the exercises with a group of women once a week for one hour under
the supervision of a physical therapist for twelve weeks. They were also
instructed to perform the exercises at home. After twelve weeks, they followed
the same protocol, now at home. At the end of the 12th and 24th weeks, they
were re-evaluated. On the other hand, the participants randomized to the home
PFMT protocol received the exercise protocol on the day of the initial
evaluation and were instructed to perform the exercises daily for a period of
twenty-four weeks. After the 12th and 24th weeks, they were re-evaluated as
well. Figure 1 demonstrates the sequence of protocols in a 24 weeks follow-up.
In both groups the participants received an exercise
protocol with images showing the postures, that could be performed alternately
(lying down, sitting and standing), including activation of phasic and tonic
fibers. The sustained contractions were 5 seconds of contraction and ten
seconds of relaxation, ten repetitions in total. Phasic contractions were one
contraction and three relaxation periods, ten repetitions in total. In the home
PFMT protocol, participants could lie down, which was not possible in the group
PFMT due to the physical space of the outpatient clinic. In the group
intervention, a minimum number of eight weeks stay was considered for the
study. Figure 2 shows the protocols used in group and at home.
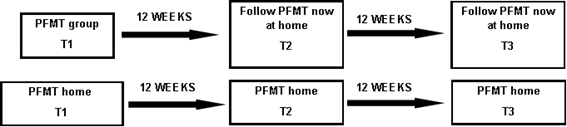
PFMT = Pelvic Floor Muscle Training); T1 (Time 1):
Initial assessment; T2 (Time 2) = Evaluation after twelve weeks; T3 (Time 3) =
Final evaluation
Figure 1 - Sequence of protocols in a twenty-four-week
follow-up
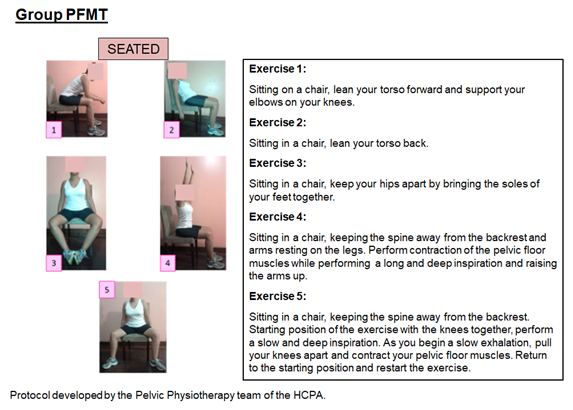
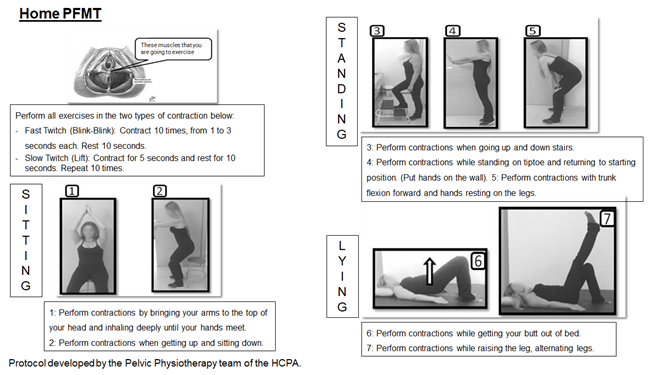
Figure 2 - Protocols
The primary outcome was improvement of PFM
functionality. In this study, it was evaluated by measuring the pressure
through pressure biofeedback and by vaginal palpation. Pressure biofeedback is
a device with a vaginal catheter containing a pressure gauge, which measures
the PFM pressure by assessing the maximum peak muscle contraction of the pelvic
floor in cm H2O. This study used the device "Vaginal probe
transducer" (VPT) developed at HCPA. The transducer consists of a silicone
probe attached to a pressure sensor and to the computer which, upon being
inflated, measures the PFM pressure according to its dynamic response as soon
as the patient performs a MVC (maximum voluntary contraction) [9]. The PERFECT
Scale was used during vaginal palpation. It is an acronym, composed of seven
items, that was developed and validated by Laycock and Jerwood [10], to
evaluate the contractility of the PFM and to enable professionals to plan
patients’ treatments. The PERFECT Scale used in the present study was the
updated version described by Laycock, Whelan & Dumoulin [11].
For the secondary outcomes, the two self-administered
questionnaires, ICIQ-SF and PISQ-12, were used to assess the impact of UI on
quality of life (QOL) and sexual function (SF), respectively. The ICIQ-SF is a
questionnaire validated for the Portuguese language, which proposes to assess
the impact of UI on the QOL of women/men. It consists of four items that check
the frequency of urinary loss, the amount of urinary loss, how much this loss
interferes with daily life and the situations in which urinary losses occur.
The results are based on the sum of the answers given to each item, with points
varying of 0 to six. The maximum score to be reached is 21, with higher scores
indicating a worse QOL [7]. PISQ-12 was used to assess sexual function, a
questionnaire validated for the Portuguese language, which assesses sexual
function in women with UI and pelvic organ prolapse (POP). It has four items:
emotional concerns, physical aspects, and relationship with the partner. The
results are based on the sum of the individual questions, consisting of answers
like "never" to "always", with points of 0 to four. The
maximum score of 48, where higher scores indicate better SF [8].
The sample calculation considered, following a study
by Felicíssimo et al. [12], a minimum
difference of 2.9 points to be detected in the QOL (ICIQ-SF) in addition to a
standard deviation of 4.35. The level of significance and statistical power
were set at 5% and 80%, respectively, and thus the sample size was at least 28
individuals for each group. The sample calculation was performed on the
software G*Power, version 3.0.10.
Participants were randomly assigned to the group PFMT
protocol or the home PFMT protocol according to a random list generated by the
software WinPepi, version 4.0. Participants were
allocated in eight blocks of eight, as suggested in the literature [13]. The
allocation sequence was concealed using numerically sequenced, opaque sealed
envelopes opened after inclusion of patients in the study. One researcher,
blind to treatment, was responsible for assigning, registering, evaluating and
monitoring individuals.
Initially the Shapiro-Wilk test was performed to
verify the distribution of the data. Symmetric variables were expressed as mean
and standard deviation, or by median and 95% Confidence Interval [95% CI].
Categorical variables were described as absolute (n) and relative (n%)
frequencies. To compare means between intergroups, Student’s t test for
independent samples was applied. In asymmetry cases, the Mann-Whitney test was
used to perform comparisons. The Chi-Square test with standardized residuals
was applied for determining the association between two nominal variables. To
compare means between intragroups, t-test of Paired
Samples was applied. In asymmetry cases, the Wilcoxon test was used to perform
comparisons. The Chi-Square test with standardized residuals was applied for
determining the association between two nominal variables.
For assessing intervention type (PFMT group or PFMT
home) and the outcomes involving the primary and secondary outcomes between and
within groups, simultaneously, the model of Generalized Estimating Equations
(GEE) adjusted by Bonferroni was applied. All data were evaluated using the
SPSS, version 18.0. (SPSS Inc., Released in 2009, PASW Statistics for Windows,
Version 18.0. Chicago). The significance level adopted for all analyses was set
at 5%. This study was approved by the Ethics Committee of the Hospital de Clínicas de Porto Alegre (no. 150316) and was registered at
Clinical Trials (no. NCT03500185).
Results
One hundred and ninety women diagnosed with UI were
selected to participate in the study. Of these, one hundred and twenty-six were
excluded because they did not meet the inclusion criteria. Sixty-four were
randomized to one of the two treatment groups. Thirty-two women were treated
according to the group they were allocated. Fourteen and twelve women were
removed from the analysis, missing their follow-up, after twelve weeks of
treatment, respectively in the group PFMT and the home PFMT. The results
according to protocol were analyzed in 17 participants in each group at the end
of the 24 weeks of treatment (Figure 3). The baseline data of the studied
sample are described in Table I and Table II, with categorical and numerical
variables, respectively.
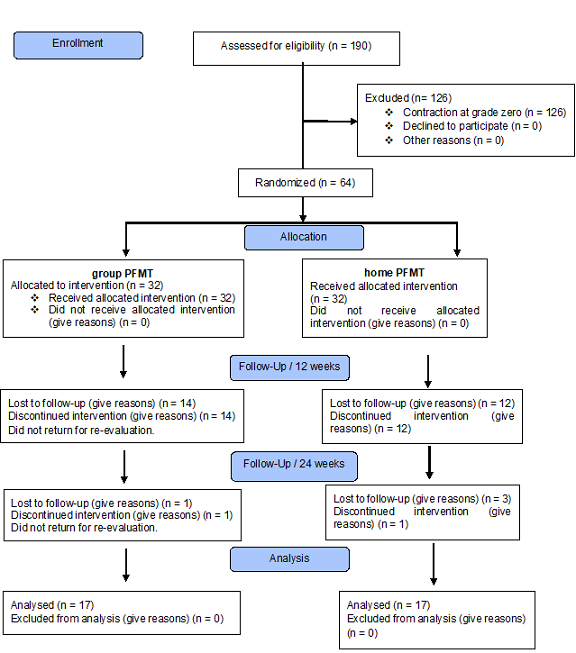
Figure 3 - Flowchart of the study population randomized to
two treatment groups
Table I - Characterization of the sample - categorical
variables
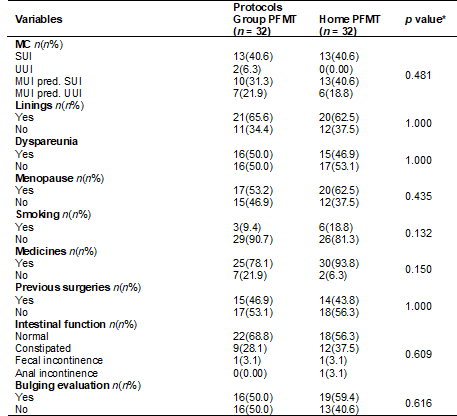
N = absolute frequency; n% = relative frequency; MC =
main complaint; SUI = Stress urinary incontinence; UUI = Urgency urinary
incontinence; MUI = Mixed urinary incontinence; MUI pred. SUI = MUI predominance SUI; MUI pred. UUI = MUI predominance
UUI; p = statistical significance.
*Statistical representation of the initial assessment
categorized distribution, as measured by the Chi-Square test. Statistical
significance was set at p ≤ 0.05 for all analyses. * Shapiro-Wilk
normality test
Table II - Characterization of the sample - numerical
variables
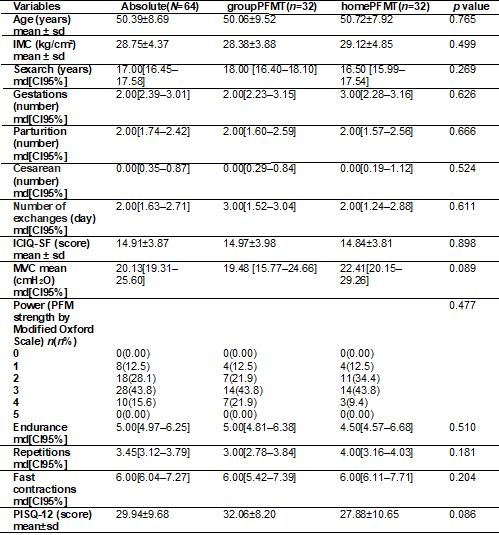
Md = median; CI = Confidence Interval; sd = standard deviation of the mean; PFMT = Pelvic Floor
Muscles Training. MVC = Maximum Voluntary Contraction; PFM = Pelvic Floor
Muscles. *Statistical representation of the categorized comparison
pre-intervention intergroups, measured by the Independent Samples t-test or
Mann-Whitney and Chi-square, when applicable. Statistical significance was set
at p ≤ 0.05 for all analyses. *Shapiro-Wilk normality test
Observing the intragroup variables after twelve weeks
of treatment, both protocols were not effective in improving PFM functionality,
measured by pressure biofeedback. When the PERFECT Scale was considered, the
group PFMT protocol was effective in improving the Power item (Chi-square, p =
0.042). The remainder of the items in the PERFECT Scale did not change. These
results are described in Table III.
Table III - Intergroup / intragroup comparison after 12
weeks
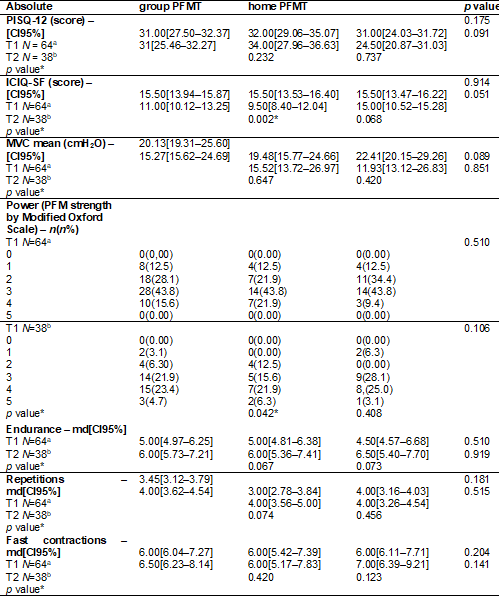
md = median; CI = Confidence Interval; sd = standard deviation of the mean; T1 = Initial evaluation;
T2 = Evaluation after 12 weeks; PFMT= Pelvic Floor Muscles Training; MVC =
Maximum Voluntary Contraction; PFM = Pelvic Floor Muscles. a PFMT group N=32 /
PFMT home N=32; bPFMT group N=18 / PFMT home N=20. *Statistical
representation of the intergroup categorized comparison after 12 weeks, as
measured by the Independent Samples t
test or
Mann-Whitney and Chi-Square, where applicable. Statistical significance
was set
at p ≤ 0.05 for all analyzes. *Shapiro-Wilk normality test.
*Statistical representation of the intragroup categorized comparison
after 12
weeks, as measured by the t-test of Paired Samples or Wilcoxon and
Chi-Square,
where applicable. Statistical significance was set at p ≤ 0.05 for
all
analyses. *Shapiro-Wilk normality test
After the twenty-four weeks, the average MVC,
Endurance and Fast contractions variables remained unchanged in both protocols.
The Power and Repetition items, however, were affected by time, but one should
be careful when analyzing these items. Despite this, the test was not able to
demonstrate the interaction, probably due to the large loss of follow-up
throughout the study and the proximity of the averages found in both groups.
The same occurs with the Power item, but in this case an additional test was
performed (Chi-square, p = 0.139), which confirmed that none of the protocols
were effective at the end of twenty-four weeks. These results are described in
Table IV.
Table IV - Group, time and interaction pairwise comparisons
using generalized estimating equations
Observing the intra-group variables after twelve weeks
of treatment, only the group PFMT protocol was effective in improving the QOL
variable (Wilcoxon, p = 0.002), while none of the protocols presented
difference in the SF variable. These results are described in Table III.
Time and protocol interactions
were observed for the ICIQ-SF and PISQ-12 variables. In the group PFMT, the
PISQ-12 variable already showed improvement from T2 until T3. In the home PFMT
protocol, the PISQ-12 variable worsens in T2 and from it until T3 presents an
evolution. Analyzing the variable in pairs, the group PFMT protocol was the
most effective (T2 and T3). The ICIQ-SF item in both protocols presents evolution
in T2. However, the home PFMT protocol in T3 is not shown to be more effective.
Analyzing the variable in pairs, the group PFMT protocol was the most effective
(T2 and T3). Figure 4 shows the evolution of the protocols. These results are
described in Table IV.
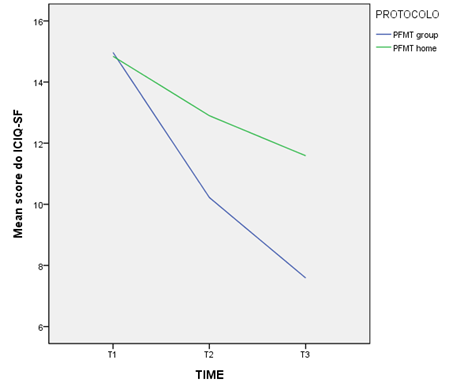
ICIQ-SF = Consultation on Incontinence
Questionnaire-Short Form); PFMT = Pelvic Floor Muscle Training
Figure 4 - ICIQ-SF Consultation on Incontinence
Questionnaire-Short Form)
Discussion
The objective of this study was to identify the effect
of a group PFMT protocol compared to a home PFMT protocol for women with UI,
with the main outcome being improvement of PFM functionality. With twelve weeks
of treatment, in a general context, it was observed that only the PFMT group
protocol was presented as a more effective form of treatment for UI because it
demonstrated improvement in the Power and QOL aspects. When we observed the
effect of the protocols after twenty-four weeks, both were effective only when
referring to the secondary outcomes, that is, quality of life and sexual
function.
According to Bo et al. [14], PFMs present a constant
level of rest tonus (except before and during urination and defecation),
symmetry and the ability to contract and relax voluntarily. The normal
contractile function of the PFM is verified by a movement of internal
constriction of the pelvic openings in the ventrocephalic
direction. The "Power" muscle variable is one of the characteristics
of muscle action, defined as the explosive aspect of force, the product of force
and moving speed (force × distance/time).
PFMT is a type of exercise whose goal is to improve
the strength, endurance, potency and relaxation of these muscles [14]. In
addition, it can alter the morphology of the muscles by increasing its thickness
and strength in the first six to eight weeks, being predominantly neural.
Hypertrophy occurs after six to eight weeks and can be prolonged for years. The
latter is general for all muscle fibers; however, the potential of hypertrophy
is greater in phasic fibers than in tonic ones. The success of this training
also depends on the ability to identify the PFM, awareness of correct
contraction, compliance, and motivation to perform the exercise protocol [15].
In the present study, the Power variable showed improvement only at twelve
weeks of the group PFMT intervention, which is consistent with what is
advocated by ICS (International Continence Society), that PFMT involves the
voluntary and repeated contraction of this striated muscle, and that this training
should be maintained for eight to 12 weeks [3].
After the twelve weeks, no change was observed for the
Power variable in the group treatment, probably because the participants were
unsupervised from this moment, and training adherence was not controlled [3].
This does not refer to the intervention itself, but the patients’ commitment to
change their behavior and adhere to the intervention [14].
In their systematic review, Dumoulin et al
demonstrated that individual PFMT protocols are better than no treatment,
placebo or inactive control for women with UI. However, follow-up (usually
twelve weeks) after the end of treatment is limited in most studies, thus
meaning that the long-term results of individual PFMT protocols remain unclear
[4].
Paiva et al. [5] opted to perform a systematic
review of the behavior of the group PFMT protocol. These authors demonstrated
that the group PFMT protocol is as effective as the individual PFMT for UI, but
when compared to the home PFMT it is more effective. However, the effect of
individual and group PFMT protocols is observed for up to twelve weeks. Thus,
the present study corroborates with Paiva et al. [5], since it
demonstrates that the group PFMT, considering twelve weeks, is more effective
than the home PFMT in relation to the Power aspect of PFM functionality and QOL
improvement, in the conservative treatment of UI.
On the other hand, observing the 24 weeks of
treatment, both protocols are effective regarding QOL and SF, but with specific
behaviors. Regarding QOL, it was observed that in 12 weeks both protocols were
already effective. QOL depends on the subjective perception of UI and on
treatments that target the social, physical and mental levels [16]. Thus, the
group PFMT protocol (in twelve weeks) relied on the interaction between the
participants and the physiotherapeutic supervision, which may benefit the three
levels mentioned. However, even without supervision, the home PFMT protocol was
also effective for QOL in this period. The fact that they received orientation
and education during the evaluation proved to be an important strategy capable
of initially modifying these women’s QOL. A good level of education and health
has an intrinsic value for people: education helps to improve health and good
health contributes to better education [17].
After 12 weeks, only the group PFMT protocol remained
effective regarding QOL. Participants in the group PFMT are likely to remain
more engaged in treatment because of prior interaction with other women and
supervision, which has not occurred with the participants who performed home
PFMT. The sample of this study had a predominance of MUI and when comparing the
different types of UI, some studies indicate that MUI has a greater impact on
women's QOL [18,19]. Thus, probably the questionnaires were able to identify
the effect of both protocols in these outcomes due to the predominance of MUI
in this sample.
Regarding sexual function, the group and home
interventions showed different effects. While the group PFMT protocol was
effective for SF, as early as the 12th week, improving the PISQ-12 score, home
protocol behaved inversely, probably because the participants did not have
supervision. The presence of UI in women's lives causes feelings of low
self-esteem, restricting social contact and interferes with sexual life [1]. As
well as the impact that the different types of UI have on QOL, they also have
an impact on SF. Women with overactive bladder would be more prone to sexual
problems than women with SUI and MUI. Lower urinary tract symptoms, urgency and
urinary incontinence, are associated with sexual dysfunction in women [20].
After 12 weeks, both protocols presented an evolution in the PISQ-12 score,
probably because at this moment the home PFMT participants were re-evaluated
and received a new incentive to perform the exercises, a fact that may explain
the behavior change of the PISQ-12 variable.
Thus, group PFMT was an effective strategy in the
conservative treatment of female UI when compared to home treatment. And as
stated by Dumoulin et al. [21], if we consider demographic projections,
human resources, and health system limitations, there is an urgent need to
expand the evidence on the long-term benefits of low-cost interventions for UI
treatment in women, a condition that is often underestimated, as is the case of
group interventions.
We can cite as limitations of this study the great
loss of follow-up in both treatment groups, with 46.87% of loss in each group
after 24 weeks. This fact can be justified by the large number of patients from
outside the city who seek treatment at the HCPA. In addition, it was not
possible to control adherence to the exercises in any of the protocols,
especially in the home PFMT.
Conclusion
The group PFMT protocol used in the present study was effective
in improving the functionality of the PFM and QOL in women with UI when applied
under supervision for twelve weeks. After 24 weeks of intervention, in this
studied sample, the group and home protocols were effective in the secondary
outcomes, QOL and SF. It can be assumed that the group intervention constitutes
a feasible and viable physiotherapeutic intervention strategy, able to benefit
many women with UI, besides being a tool that is easy for patients to
understand and follow.
It is important to remember that group PFMT is a
strategy that has been used in the Outpatient Clinic of Pelvic Physiotherapy
developed in partnership with the Outpatient Clinic of Gynecology and
Obstetrics of the Hospital de Clínicas de Porto
Alegre for six years, and it is clinically possible to verify the improvement
of the patients in care. However, there was a need for scientific evidence on
the effect of group interventions. Thus, in addition to answering the question
of the effect, this study was able to identify that group PFMT protocol,
supervised by a physiotherapist, can be an easy and practical tool to be
applied as a basis for the treatment of female UI in the public health system.
Conflict of interest
There is no conflict of interest.
Funding source
No funding sources.
Authors' contributions
Research conception and design: Ferla
L; Data collection: Ferla L, Darski
C; Data analysis and interpretation: Ferla L,
Statistical analysis: Ferla L, Writing of the
manuscript: Ferla L; Critical review of the
manuscript for important intellectual content: Ferla
L, Darski C, Paiva LL, Ramos JGL
References
- Souza LC, Azevedo RCS,
Cardoso JDC, Alexandre RMS, Lima IF. Interferências e repercussões da
incontinência urinária na vida dos idosos. Brazilian
Journal of Health Review 2022;5(3):9792-804. doi: 0.34119/bjhrv5n3-150 [Crossref]
- Batmani S, Jalali R, Mohammadi M, Bokaee S. Prevalence and factors related to urinary incontinence in older adult women worldwide: a comprehensive systematic review and meta-analysis of observational studies. BMC geriatrics 2021;21(1):1-17. doi: 10.1186/s12877-021-02135-8 [Crossref]
- Abrams P, Andersson K, Apostilidis A, Birder L, Bliss D, Brubaker L, et al. 6th International Consultation on Incontinence. Recommendations of the International Scientific Committee: evaluation and treatment of urinary incontinence, pelvic organ prolapse and faecal incontinence. Neurourol Urodyn 2018;37(7):2271-72. doi: 10.1002/nau.23551 [Crossref]
- Dumoulin C, Cacciari LP, Hay-Smith EJC. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women: a short version Cochrane Syst Rev 2015;34(4):300-8. doi: 10.1002/nau.22700 [Crossref]
- Paiva LL, Ferla L, Darski C, Catarino BM, Ramos JGL. Pelvic floor muscle training in groups versus individual or home treatment of women with urinary incontinence: systematic review and meta-analysis. Int Urogynecol J 2017;28(3):351-9. htps://doi.org/10.1007/s00192-016-3133-2 [Crossref]
- Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated
guidelines for reporting parallel group randomized trials. Ann Int Med
2010;152(11):726-32. doi: 10.7326/0003-4819-152-11-201006010-00232 [Crossref]
- Tamanini JTN, Dambros M, D’Ancona CAL, Palma PCR, Netto JR NR. Validação para o português do International Consultation on Incontinence Questionnaire-Short form (ICIQ-SF). Rev Saúde Pública 2004;38:438-44. doi: 10.1590/S0034-89102004000300015 [Crossref]
- Santana GWRM, Tsutomu A, Auge APF. The Portuguese validation of the short form of the pelvic organ prolapse/urinary incontinence sexual questionnaire (PISQ-12). Int Urogynecol J 2012;23(1):117-21. doi: 10.1007/s00192-011-1505-1 [Crossref]
- Sanches PRS, Silva Junior DP, Müller AF, Schmidt AP, Ramos JGL, Nohama P, et al. Vaginal probe transducer: Characterization and measurement of pelvic-floor strength. J Biomech 2009;42(15):2466-71. doi: 10.1016/j.jbiomech.2009.07.021 [Crossref]
- Laycock JO, Jerwood D. Pelvic floor muscle assessment: the PERFECT scheme. Physiotherapy 2001;87(12):631-42. doi: 10.1016/S0031-9406(05)61108-X [Crossref]
- Laycock J, Whelan MM, Dumoulin. C. Patient assessment. In: Haslam J, Laycock J, Eds. Therapeutic management of incontinence and pelvic pain. 2nd ed. London: Springer; 2007. p.57-66. doi: 10.1007/978-1-84628-756-5 [Crossref]
- Felicíssimo MF, Carneiro MM, Saleme CCS, Pinto RZ, Fonseca AMRM, Silva-Filho AZ, et al. Intensive supervised versus unsupervised pelvic floor muscle training for the treatment of stress urinary incontinence: a randomized comparative trial. Int Urogynecol J 2010;21(7):835-40. doi: 10.1007/s00192-010-1125-1 [Crossref]
- Bland JM. Statistics notes: how to randomise. BMJ 1999;319:703-4. doi: 10.1136/bmj.319.7211.703 [Crossref]
- Bo K, Frawley HC, Haylen BT, Abramov Y, Almeida FG, Berghmans B, Bortolini M, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for the conservative and nonpharmacological management of female pelvic floor dysfunction. Int Urogynecol J 2017;28(2):191-213. doi: 10.1007/s00192-016-3123-4 [Crossref]
- Ferreira M, Santos P.
Princípios da fisiologia do exercício no treino dos músculos do pavimento
pélvico. Acta Urológica [Internet].
2009 [cited 2022 Aug 24];26(3):31-8. Available from:
https://apurologia.pt/acta/3-2009/princ-fisio-ex-trei.pdf
- Whoqol Group. The World Health Organization quality of life assessment (WHOQOL): position paper from the World Health Organization. Social Sci Med 1995;41(10):1403-9. doi: 10.1016/0277-9536(95)00112-K [Crossref]
- Loureiro M. Promover a
Saúde - Dos fundamentos à acção. 3ª ed. Alfragide: Leya; 2019.
- Souza BR, Souza BR, Dantas IS, Souza JS, Alencar I, et al. A influência da incontinência urinária na qualidade de vida de mulheres jovens: uma revisão de literatura. Research, Society and Development 2021;(10):13:e23101321033. doi: 10.33448/rsd-v10i13.21033 [Crossref]
- Oliveira LGP, Tavares ATDVB, Amorim TV, Paiva ACPC, Salimena ACPC. Impacto da incontinência urinária na qualidade de vida de mulheres: revisão integrativa da literatura. Revista Enfermagem UERJ 2020;28:51896. doi: 10.12957/reuerj.2020.51896 [Crossref]
- Wang Y, Jiao W, Wang X, Zhang J, Shi G, et al. The correlation between severity of overactive bladder symptoms with female sexual dysfunction and sexual satisfaction of partners. Urologia Internationalis 2021;105:124-30. doi: 10.1159/000508764 [Crossref]
- Dumoulin CM, Morin M, Mayrand M, Tousignant M, Abrahamowicz M. Group physiotherapy compared to individual physiotherapy to treat urinary incontinence in aging women: study protocol for a randomized controlled trial. Trials 2017;18(1):544. doi: 10.1186/s13063-017-2261-4 [Crossref]