Fisioter Bras 2023;24(1):1-12
ARTIGO ORIGINAL
Impact of COVID-19 on the emotional health and work routine of oncology
physiotherapists in Brazil
Impacto da COVID-19 na
saúde emocional e na rotina de trabalho de fisioterapeutas oncológicos no
Brasil
Universidade Federal do
Ceará, Fortaleza, CE, Brazil
Received: December 24, 2021; Accepted: November 20, 2020.
Correspondence: Daniela Gardano Bucharles Mont’Alverne, E-mail:
daniela.gardano@ufc.br
How to cite
Mont’Alverne DGB, Rodrigues LRS, Bedê
JMS, Silva AKA, Abreu BO, Fernandes TG, Silva RLC, Moura AF. Impact of
COVID-19 on the emotional health and work routine of oncology physiotherapists
in Brazil. Fisioter Bras 2023;24(1):1-12 doi: 10.33233/fb.v24i1.5045
Abstract
Background: The COVID-19 epidemic has affected the emotional
health and work routine of healthcare professionals. Objective: Assess
the effect of COVID-19 on the emotional health and work routine of oncology
physiotherapists in Brazil. Methods: Anonymous cross-sectional online
study, in which 102 oncology physiotherapists were recruited from different
regions of the country, using snowball sampling on social media.
Sociodemographic data on participants’ training and their work in oncology were
assessed, as well as symptoms of depression, anxiety and stress (21 - item
Depression, Anxiety and Stress Scale - DASS-21). Results: Most of the
physical therapists were women (n = 89, 87.3%), with an average age of 33.8 ±
7.1 years and specializing in oncology physiotherapy (n = 84, 82.5%). The
younger the professionals, the greater their stress levels (p = 0.022). Most
continued to provide in-person care (n = 89, 87.3%) and stress was the symptom
that scored highest (6.9 ± 4.4). Longer working hours and transfers to other
units resulted in more symptoms of anxiety (p = 0.016) and stress (p = 0.011). Conclusion:
The COVID-19 pandemic has adversely affected the work routine and emotional
health of oncology physiotherapists in Brazil.
Keywords: COVID-19; SARS-COV-2; mental health; rehabilitation.
Resumo
Introdução: A pandemia da COVID-19 vem impactando
na saúde emocional e na rotina de trabalho dos profissionais de saúde. Objetivo:
O objetivo deste estudo foi avaliar o efeito da pandemia da COVID-19 na saúde
emocional e na rotina do trabalho dos fisioterapeutas oncológicos brasileiros. Métodos:
Estudo transversal online anônimo, no qual 102 fisioterapeutas oncológicos
foram recrutados de diferentes regiões do país, usando amostras de conveniência
de bolas de neve nas mídias sociais. Dados sociodemográficos, referentes à
formação e atuação profissional foram avaliados, além dos sintomas de
Depressão, Ansiedade e Estresse. Resultados: A maioria dos fisioterapeutas
era do sexo feminino (n = 89,87,3%), com média de idade de 33,8 ± 7,1 anos e
especialista em fisioterapia oncológica (n = 84,82,5%). Quanto mais jovens mais
estressados eram os profissionais (p = 0,022). A maioria manteve os
atendimentos presenciais (n = 89, 87,3%) e o sintoma de estresse apresentou
maior pontuação (6,9 ± 4,4). O aumento na jornada de trabalho e a transferência
para outras unidades de trabalho resultaram em maiores sintomas de ansiedade (p
= 0,016) e de estresse (p = 0,011). Conclusão: Concluímos que a pandemia
afetou negativamente a rotina de trabalho e a saúde emocional de
fisioterapeutas oncológicos no Brasil.
Palavras-chave: COVID-19; SARS-COV-2; saúde mental; rehabilitação.
Introduction
The COVID-19 pandemic has posed a significant
challenge for health services worldwide. As an unknown disease in terms of
effective prevention and treatment, most countries adopted social isolation as
a viable means of reducing the spread of the infection [1]. Another change put
in place was the reorganization of health services by reducing or suspending
elective procedures, except in the case of pathologies that may lead to greater
complications, such as cancer. Although services were not suspended in these
cases, the literature recorded an important decline in access by cancer
patients [2].
From the start of the pandemic until July 30, 2020,
more than 668,000 people have died from COVID-19 worldwide. In Brazil, this
figure reached more than 91,000 (“Coronavirus Disease (COVID-19) Pandemic”
2020). Moreover, both cancer patients and healthcare professionals have faced
significant adversity in recent months. In addition to attempting to understand
the effects of the virus on patients with cancer and preventing contact during
hospital visits, the study area was also contained in order to prevent the
spread of COVID-19, despite its importance in contributing to clinical decision
under different conditions [3].
Clinical management of cancer within the healthcare
system during the pandemic was based, worldwide, on the current status of the
disease. While some countries advocated reducing or suspending
immunosuppressant drugs, others adopted telemedicine as a means of limiting
exposure and continuing treatment remotely [2,4]. In fact, in some cases, the
resulting changes in health services led to discontinued treatment and an
urgent need for public policies to address these types of situations and
reorganize the management of chronic pathologies [2,4,5].
These changes, adjustments and uncertainties regarding
how best to manage cancer patients during this time have affected both patients
and multiprofessional teams alike. Thus, the pandemic
has challenged the mental health of healthcare professionals in general,
promoting greater tendencies to depression, anxiety, insomnia and anguish, and
potentially interfering in follow-up care for patients [6,7,8].
This drastic change in services for cancer patients
can also cause significant stress for the physiotherapists responsible for
monitoring the patients on a day-to-day basis at clinics, hospitals or in
home-care settings. As such, this study aimed to assess the effect of COVID-19
on the emotional health and work routine of oncology physiotherapists in
Brazil.
Methods
Study design and participants
An anonymous cross-sectional online study was
conducted with oncology physiotherapists in Brazil. It was approved by the
Research Ethics Committee of the Federal University of Ceará
(4.084.326) and followed the STROBE recommendations for the reporting of
cross-sectional studies [9]. Inclusion criteria were ≥ 18 years, both
sexes, being a physiotherapist resident in Brazil and registered with the
relevant Regional Board of Physiotherapy and Occupational Therapy, working in
the field of oncology physiotherapy at public, private or philanthropic
hospitals, clinics or home-based care, and not having been on professional
leave in the last 60 days.
Data collection
Individuals were recruited over a three-week period
(June 12 to July 3, 2020) using snowball sampling on social media. Research
items included demographic data on the training of the physiotherapists and
their work in oncology during the COVID-19 pandemic, as well as the Depression,
Anxiety and Stress Scale (DASS-21).
The DASS was originally developed in English, with 42
items that yield three factors (depression, anxiety and stress). However,
considering situations in which a shorter instrument is desirable, the authors
opted to use the 21-item version denominated DASS-21. This version has been
applied in different countries and translated and validated for Portuguese
[10]. DASS-21 is a set of three self-reported 4-point Likert subscales, each
consisting of 7 items that evaluate the emotional states of depression,
anxiety, and stress.
Statistical analysis
The data were analyzed using SPSS software version
23.0. Participants’ characteristics and answers were summarized using
descriptive statistics, standard deviation and absolute and relative
frequencies. Associations between the working conditions of physiotherapists
and anxiety, depression and stress were examined with the independent t-test.
Correlations were analyzed using Spearman’s test for the numerical variables
and the chi-squared test for their categorical counterparts. Multivariate
linear regression was subsequently performed, using the stepwise backward
method and selecting variables with a correlation of up to 20% (p < 0.020)
in the bivariate analysis
Results
A total of 106 physiotherapists answered the
questionnaire, but 4 were excluded as duplicates, leaving a final sample of
102. Most were women (n = 89, 87.3%), with an average age of 34 (29 - 38) years
and married (n = 51, 50%). Additionally, 44 (43.1%) worked in the Southeast, 66
(64.7%) held a specialty as their highest academic degree, 84 (82.4%) were
oncology physiotherapists, and 48 (47.1%) had worked in the field for more than
5 years (n = 48, 47.1%) (Table I).
With respect to where the participants worked, 61
(59.8%) reported they worked at hospitals, 54 (52.9%) in outpatient
facilities/clinics and 30 (29.4%) provided home care.
When questioned about the impact that COVID-19 had on
their work routine, 52 (51%) reported shorter working hours and 13 (12.7%) were
transferred to another facility to meet demand (Table II).
In regard to patient care, most respondents continued
in-person appointments at both outpatient/clinic and hospital level. When asked
about remote monitoring for cancer patients during the pandemic, most (46.8%)
participants who worked at outpatient facilities/clinics or provided home care
stated that their workplace provided the necessary means for them to monitor
their patients (Table II).
In relation to the type of remote monitoring used, 38
(48.1%) contacted their patients only once and provided general guidance, and
27 (34.2%) compiled educational material and emailed it to patients after
initial telephone contact.
Assessment of the symptoms of depression, anxiety and
stress by DASS-21 indicated that stress obtained the highest score, with an
average value of 6.9 (4 - 10). Average scores for depression and anxiety were
4.2 (1 - 6) and 3.9 (1 - 7), respectively.
Analysis of the association between working conditions
and depression, anxiety and stress scores indicated that physiotherapists who
worked at outpatient facilities/clinics obtained lower depression scores (p =
0.038). Additionally, longer working hours were associated with higher levels
of anxiety (p = 0.016) and stress (p = 0.011), and being transferred to another
oncology unit resulted in greater stress (p = 0.021) (Table III).
Analysis of the correlations between age, anxiety,
depression and stress demonstrated a positive moderate correlation between
depression and anxiety (r = 0.546 p = 0.000) and depression and stress (r =
0.678 p = 0.000), as well as a strong correlation between stress and anxiety (r
= 0.835 p = 0.000). Age exhibited a weak inverse correlation with stress (r =
-0.227 p = 0.022), that is, the younger the individual, the higher their stress
score.
No associations were observed between length of
service or sex and anxiety, depression and stress (p ≥ 0.05).
In multivariate analysis using stress as the outcome
variable, only anxiety and depression influenced the stress of physiotherapists
(Table IV).
Table I - Sociodemographic characteristics of oncology
physiotherapists in Brazil during the COVID-19 pandemic
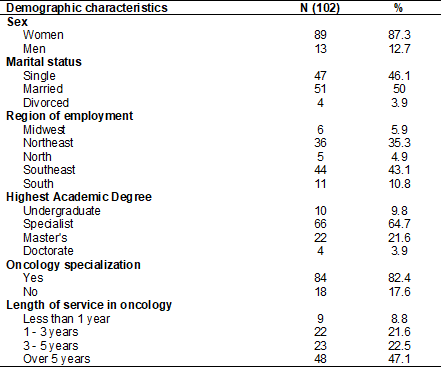
Table II - Working conditions of oncology physiotherapists during the COVID-19
pandemic
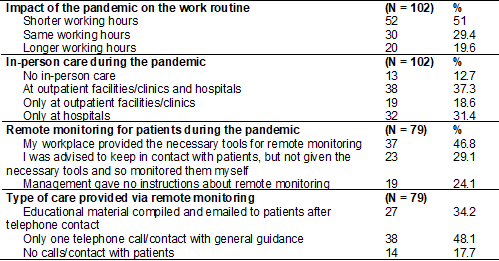
Table III - Association between the working conditions of physiotherapists and
anxiety, depression and stress

DASS =
Depression, Anxiety and Stress Scale; *p < 0.05
Table IV - Multivariate analysis between
stress and the variables work routine, age, anxiety and depression
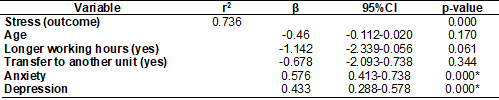
95% CI = 95% Confidence Interval; r2
= adjusted Pearson’s correlation; *p < 0.05, variables of the final model by
multivariate linear regression
Discussion
The present study demonstrated that the COVID-19
pandemic altered the work routine of physiotherapists in the form of shorter
working hours and transfers to other units in order to meet demand. This has
led to emotional disturbances correlated with greater stress in professionals
who were transferred to another facility as well as those with longer working
hours. Telerehabilitation was used by a large part of the physiotherapists
studied here as a means of circumventing the reduced therapist-patient contact
in place during the pandemic.
Several studies have been conducted to scientifically
prove the impact of COVID-19 on all aspects of cancer treatment [3,11,12].
Changes in access to health care during this global emergency have resulted in
less patient contact in the treatment of different chronic diseases [12].
However, the possibility of metastasis, progression or other complications
means cancer treatment cannot be put on hold [13]. Although 51% of the
physiotherapists interviewed reported a decline in working hours, in-person
care continued in the outpatient sector, hospitals and via remote monitoring. A
study on multidisciplinary care provided to survivors of head and neck cancer
during the pandemic at a medical center affiliated with the University of
Pittsburgh (UPMC) also found that physiotherapists had to adjust their
assessment and treatment services via telemedicine [14].
Telemedicine emerged about 25 years ago, but the
pandemic has been a major milestone for its use in a number of countries.
However, its application in oncology to monitor patients before or after
surgery or during other treatments is not well described in the literature
[12]. In the present study, approximately 48% of the sample monitored their
patients remotely and sent them educational material. Additionally, their
workplaces were willing to supply the necessary resources for telemedicine,
indicating that this technology can be used for cancer patients during the
pandemic to help healthcare professionals monitor these individuals.
This emergency measure has been adopted by several
institutions to meet needs resulting from the pandemic and is guaranteed
nationwide by the Federal Board of Physiotherapy and Occupational Therapy
(COFFITO) via Ordinance 155 of March 20, 2020 [15] which governs the creation
of a National Teleconsulting Committee for the COFFITO/CREFITOS System in Physiotherapy
and Occupational Therapy to address the crisis caused by the COVID-19 pandemic.
However, it is important to note that telemedicine is a challenging strategy
for physiotherapy, given the hands-on nature of the profession and the lack of
results proving its effectiveness in oncology or well-structured guidelines for
professionals.
A study with healthcare professionals in the United
States and United Kingdom found no significant increase in absenteeism during
the first 100 days of the COVID-19 pandemic in these countries. The results
indicate that about 30% of healthcare personnel were unable to do their jobs
effectively, with fear of infection and the lack of personal protective
equipment (PPE) as decisive factors [16].
From another perspective, scientific evidence shows a
correlation between outbreaks or pandemics and psychological problems in
healthcare professionals. Some studies indicate that, among public health
workers aged 30 to 50 years, living with older adults or children below 6 years
old, having a previously diagnosed health condition and inexperience in public
health emergencies are risk factors for high scores on scales that assess
depression, anxiety, insomnia and obsessive-compulsive symptoms in COVID-19
frontline health workers [17,18,19].
Another study also demonstrated a possible correlation
between psychological problems and frontline healthcare workers during the
pandemic [7]. Moreover, a recent study found a high prevalence of anxiety and
depression among oncologists in the United States despite not being on the
frontline of COVIID-19, caused by their inability to adequately treat their
patients [8].
The SARS (Sudden Acute Respiratory Syndrome) and Ebola
outbreaks caused psychosomatic symptoms in healthcare professionals, with
sequelae including pain, fatigue, weakness, anxiety, lethargy and chronic
symptoms of the infections they came into contact with during their work day.
It is important to investigate associations between these symptoms because they
may result in prolonged periods of absenteeism and health workers care for
highly vulnerable patients [20,21,22,23].
A multinational and multicenter study applied the
DASS-21 questionnaire to multiprofessional teams
involved in caring for patients with COVID-19 and found that anxiety was the
most common symptom, particularly among less experienced professionals. This
anxiety was caused by the fear of contamination or contaminating colleagues of
family members, since asymptomatic individuals can transmit the infection [20].
Similarly, in our sample, the age of healthcare
workers was inversely related to stress, with younger professionals reporting
higher stress levels, possibly due to less experience. As such, it is important
for managers of healthcare facilities to provide personnel with psychological
support in order to safeguard their mental health. Some authors have
demonstrated the benefits of implementing different mental health care
platforms, whereby the less access medical staff had to these platforms, the
higher their levels of anxiety, depression and insomnia [24,25].
Thus, it can be inferred that the COVID-19 pandemic
has adversely affected the work routine and emotional health of oncology
physiotherapists in Brazil. The pandemic has resulted in the reorganization of
health services, involving adjustments to the work routine of physiotherapists
in outpatient and intensive care sectors in the form of a reduced workload or
longer working hours as part of a new health team on the frontline.
Conclusion
The COVID-19 pandemic has prompted the need to
reorganize health services, including treatment for cancer patients. As a
result, oncology physiotherapists have experienced changes in their work
routine that may be associated with emotional difficulties such as stress.
Stress was also related to anxiety and depression, demonstrating that emotional
aspects during the pandemic directly affect the daily lives of these
professionals.
Conflict of interest
The authors report no conflicts of interest.
Funding source
No funding.
Author’s contribution
Conception and design of the research: Mont’Alverne DGB, Rodrigues LRS, Bedê JMS, da Silva AKA, Abreu BO, Fernandes TG, Silva RLCA,
Moura AF ; Data collection : Bedê
JMS, da Silva AKA, Silva RLCA; Data analysis and interpretation:
Rodrigues LRS, Abreu BO, Fernandes TG; Statistical analysis : Mont’Alverne DGB, Moura AF ; Manuscript writing :
Bedê JMS, da Silva AKA, Silva RLCA,Rodrigues
LRS, Abreu BO, Fernandes TG; Critical review of the manuscript for important
intellectual content : Mont’Alverne DGB,
Moura AF
References
- Ismael J, Losco F, Connor OJ, Quildrian S,
Sanchez P, Pincemin I, Lastiri
J, et al. Abordaje multidisciplinario
de COVID-19 y cáncer? Consenso Intersociedades
Científicas de Argentina. Fundación Oncológica de La
Patagonia Sociedad 2020;1-33; 2020. doi: 10.3332/ecancer.2020.1044 [Crossref]
- Peña E, Hernández V, Guijarro A, Castro A, Losa JE, Martel J, et al. Recomendaciones
sobre el manejo del
carcinoma de vejiga en situación de pandemia por Covid-19. Experiencia aprendida y
preparación para el futuro.
Arch Esp Urol [Internet]. 2020 [cited 2023 Jan
4];73(5):374-83. Available from:
https://pesquisa.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov/resource/pt/covidwho-1016834
- Moujaess E, Kourie HR, Ghosn M. Cancer patients and research during COVID-19 pandemic: a systematic review of current evidence. Crit Rev Oncol Hematol. 2020;22:102972. doi: 10.1016/j.critrevonc.2020.102972 [Crossref]
- Zhang WR, Wang K, Yin L, Zhao WF, Xue Q, Peng M, et al. 2020. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom. 2020;89(4):242-50. doi: 10.1159/000507639 [Crossref]
- Macedo FO, Costa RM, Ferreira FO,Torres DM, Bergmann A, Fabro EAN. Linfedema secundário ao tratamento do câncer de mama: abordagem fisioterapêutica em tempos de pandemia. Rev Bras Cancerol. 2020;66(TemaAtual):2-5. doi: 10.32635/2176-9745.RBC.2020v66nTemaAtual.1043 [Crossref]
- Leones LMB, Berba CMP, Chua AV, Sandoval-Tan J. Caring for the carers: safeguarding oncologists’ mental health in the time of COVID-19. Ecancer medical science. 2020;14:1-4. doi: 10.3332/ECANCER.2020.1057 [Crossref]
- Chou YJ, Hsuan JK, Shiow CS. 2018. Cancer prehabilitation programs and their effects on quality of life. Oncol Nurs Forum. 2018;45(6):726=36. doi: 10.1188/18.ONF.726-736 [Crossref]
- Thomaier L, Teoh D,
Jewett P, Beckwith H, Parsons H, Yuan J, et al. Emotional health concerns of
oncology physicians in the United States: Fallout during the COVID-19 pandemic.
PLoS One. 2020;15(11): e0242767. doi: 10.1371/journal.pone.0242767 [Crossref]
- Elm E, Altman DG, Egger M, Pocock ST, Gøtzsche PC, Vandenbroucke JP. 2008. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344-49. doi: 10.1016/j.jclinepi.2007.11.008 [Crossref]
- Vignola RCB, Tucci AM. Adaptation and validation of the Depression, Anxiety and Stress Scale (DASS) to Brazilian Portuguese. J Affect Disord. 2014;155:104-9. doi: 10.1016/j.jad.2013.10.031 [Crossref]
- Dai M, Liu D, Liu M, Zhou F, Li G, Chen Z, et al. Patients with cancer appear more vulnerable to SARS-CoV-2: A multicenter study during the COVID-19 outbreak. Cancer Discovery. 2020;10(6):783. doi: 10.1158/2159-8290.CD-20-0422 [Crossref]
- Daggubati LC, Eichberg DG, Ivan ME, Hanft S, Mansouri A, Komotar RJ, et al. Telemedicine for outpatient neurosurgical oncology care: lessons learned for the future during the COVID-19 pandemic. World Neurosurg. 2020;139:e859-63. doi: 10.1016/j.wneu.2020.05.140 [Crossref]
- Valenza F, Papagni G, Marchianò A, Daidone MG, De’Braud F, Colombo MP, et al. Response of a comprehensive cancer center to the COVID-19 pandemic: The experience of the fondazione IRCCS – Istituto Nazionale Dei Tumori Di Milano. Tumori. 2020;106(3):193-202. doi: 10.1177/0300891620923790 [Crossref]
- Nilsen ML, Clump DA, Kubik M, Losego K, Mrozek A, Pawlowicz E, et al. Prevision of multidisciplinary head and neck cancer survivorship care during the 2019 novel coronavirus pandemic. Head and Neck. 2020;42(7):1668-73. doi: 10.1002/hed.26256 [Crossref]
- COFFITO. 2020. Portaria No
155, de 20 de março de 2020 – Comissão Nacional de Teleconsultoria
[Internet]. 2020. [cited 2023 Jan 6]. Available from:
https://www.coffito.gov.br/nsite/?p=15843
- Batten K. The first 100 days: the effects of the COVID-19 pandemic on healthcare workers’ efficacy and absenteeism in the United States and the United Kingdom. SSRN Electronic Journal. 2020;1-22. doi: 10.2139/ssrn.3633537 [Crossref]
- Yang S, Kwak SG, Ko EJ, Chang MC. The mental health burden of the Covid-19 pandemic on physical therapists. Int J Environ Res Public Health 2020;17(10). doi: 10.3390/ijerph17103723 [Crossref]
- Zhang L, Zhu F, Xie L, Wang C, Wang J, Chen R,
P Jia P, et al. Clinical characteristics of COVID-19-infected cancer patients:
A retrospective case study in three hospitals within Wuhan, China. Ann Oncol.
2020;31(7):894-901.
- Cai W, Lian B, Song X, Hou T, Deng G, Li H. A cross-sectional study on mental health among health care workers during the outbreak of corona virus disease 2019. Asian J Psychiatr. 2020;51:102111. doi: 10.1016/j.ajp.2020.102111 [Crossref]
- Chew NWS, Lee GKH, Tan BYQ, Jing M, Goh Y, Ngiam NJH, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain, Behav Immun. 2020;88:559-65. doi: 10.1016/j.bbi.2020.04.049 [Crossref]
- Schmidt B, Crepaldi MA, Bolze SDA, Neiva-Silva L, Demenech M. Mental health and psychological interventions during the new coronavirus pandemic (COVID-19). Estudos de Psicologia (Campinas) 2020;37:1-13. doi: 10.1590/1982-0275202037e200063 [Crossref]
- Faro A, Bahiano MA, Nakano TC, Reis C, Silva BFP, Vitti LS. COVID-19 e saúde mental: a emergência do cuidado. Estudos de Psicologia (Campinas). 2020;37. doi: 10.1590/1982-0275202037e200074 [Crossref]
- Ito A, Ishioka T. Exploring the impact of the COVID-19 pandemic on the mental health of rehabilitation therapists. J Rehabil Neurosc. 2020;1-9. doi: 10.24799/jrehabilneurosci.200512 [Crossref]
- Walton M, Murray E, Christian MD. Mental health care for medical staff and affiliated healthcare workers during the COVID-19 pandemic. Eur Heart J Acute Cardiovasc Care. 2020;9(3):241-47. doi: 10.1177/2048872620922795 [Crossref]
- Kang L, Ma S, Chen M, Yang J, Wang Y, Li R, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav Immun. 2020;87:11-7. doi: 10.1016/j.bbi.2020.03.028 [Crossref]