Fisioter Bras.
2023;24(2):153-65
ARTIGO ORIGINAL
High versus low frequency transcutaneous acupoint
electrical stimulation as an adjunct therapy to prevent nausea and vomiting in
the first 24 hours after infusion of high-grade emetic chemotherapy: a
randomized controlled trial
Estimulação
elétrica transcutânea de alta versus baixa frequência como terapia adjuvante
para prevenir náuseas e vômitos nas primeiras 24 horas após a infusão de
quimioterapia emética de alto grau: um estudo controlado randomizado
Rafael
Ailton Fattori1, Júlia Schlöttgen1, Fernanda Laís Loro1,
Pauline Lopes Carvalho1, Rodrigo Orso2, Fabricio Edler Macagnan1
1Universidade Federal de Ciências da
Saúde de Porto Alegre, RS Brasil
2Pontifícia Universidade Católica do Rio
Grande do Sul
Received: 2022,dec 22;
accepted 2023, feb 25.
Correspondence: Fabricio Edler Macagnan,
fabriciom@ufcspa.edu.br
How to cite
Fattori RA,
Schlöttgen J, Loro FL, Carvalho PL, Orso R, Macagnan FE. High versus low frequency transcutaneous acupoint electrical stimulation
as an adjunct therapy to prevent nausea and vomiting in the first 24 hours
after infusion of high-grade emetic chemotherapy: A randomized controlled
trial. Fisioter Bras 2023;24(2):153-65. doi: 10.33233/fb.v24i2.5136
Abstract
Background: Transcutaneous
acupoint electrical stimulation (TAES) has been tested as antiemetic therapy. Objective:
Evaluation of the effectiveness of two different frequencies of the electrical
current as adjunctive therapy in the prevention of nausea and vomiting. Methods:
This placebo-controlled clinical trial compared the incidence of nausea and
vomiting (within the first 24 hours after high-grade emetic chemotherapy
infusion) of 61 women (54 ± 11 years) with breast cancer undergoing three modes
of TAES: high frequency (HF:150 Hz), low frequency (LF:10 Hz), and placebo (P).
Electrodes were fixed at the acupuncture point PC6 and a symmetric bipolar
current (pulse width 200 µs) was applied in a single 30-minute session prior to
the start of chemotherapy infusion. All patients receive fixed antiemetic
treatment infusions (ondansetron 8 mg) and rescue medication instructions, if
necessary, according to the routine for infusions of cyclophosphamide
associated with anthracycline. Results: The incidence of nausea was 47%
in P, 45% in HF and 26% in LF. Although not significant, the intervention with
LF-TAES at PC6 acupoint reached relevant values in reducing the relative risk
of developing nausea (RR = 0.51; CI 95% = 0.18 to 1.44; p = 0.18) and a trend
toward improved reported well-being (p = 0.06) and a lower Edmonton Symptom
Rating Scale score (p = 0.08). The incidence of vomiting and the consumption of
rescue antiemetic doses were very similar between the groups. Conclusion:
New studies with LF and HF of TAES as adjuvant therapy for the prevention of
nausea and vomiting should be carried out to confirm this hypothesis.
Keywords: Antineoplastic combined
chemotherapy protocols; antiemetic agents; electrical stimulation therapy;
acupuncture.
Resumo
Introdução: A estimulação elétrica transcutânea em
pontos de acupuntura (TAES) foi testada como terapia antiemética.
Objetivo: Avaliar a eficácia de duas frequências diferentes de corrente
elétrica como terapia adjuvante para a prevenção de náusea e vômito. Métodos:
Este ensaio clínico controlado por placebo comparou a incidência de náusea e
vômito (nas primeiras 24 horas após a infusão de quimioterapia emética de alto
grau) em 61 mulheres (54 ± 11 anos) com câncer de mama em três modos de TAES:
alta frequência (HF:150 Hz), baixa frequência (LF:10 Hz) e placebo (P). Os
eletrodos foram fixados no ponto de acupuntura PC6 e uma corrente bipolar
simétrica (largura de pulso 200 µs) foi aplicada em uma única sessão de 30
minutos antes do início da infusão de quimioterapia. Todos os pacientes recebem
infusões fixas de tratamento antiemético (ondansetrona
– 8 mg) e orientação de uso de medicação de resgate, se necessário, conforme
rotina para infusões de ciclofosfamida associada à antraciclina.
Resultados: A incidência de náusea foi de 47% no P, 45% na HF e 26% na
LF. Embora não significativa, a intervenção com LF-TAES no ponto de acupuntura
PC6, alcançou valores relevantes na redução do risco relativo de desenvolver
náuseas (RR = 0,51; IC 95% = 0,18 a 1,44; p = 0,18) e tendência de melhora na
sensação de bem estar (p = 0,06) e pontuação mais baixa na Edmonton Symptom Rating Scale (p = 0,08).
A incidência de vômitos e o consumo de doses antieméticas
de resgate foram muito semelhantes entre os grupos. Conclusão: Novos
estudos com LF e HF de TAES como terapia adjuvante na prevenção de náuseas e
vômitos devem ser realizados para confirmar essa hipótese.
Palavras-chave: protocolos combinados de quimioterapia
antineoplásica; agentes antieméticos; terapia de estimulação elétrica;
acupuntura
Introduction
The Multinational Association of
Supportive Care in Cancer (MASCC) cites that nausea and vomiting incidence in
antineoplastic protocols that combine anthracycline with cyclophosphamide can
reach 90% [1], but antiemetic drugs can reduce this incidence to values close
to 50% [2]. Nevertheless, non-pharmacological techniques such as transcutaneous
electric nerve stimulation (TENS) were proposed as complementary therapies to
support in the control of nausea and vomiting in these patients [3,4] as well
during postoperative period [5,6,7].
The last meta-analysis that
evaluated the effect of electric stimulating a specific acupuncture point (PC6)
associated with antiemetic drugs showed that the association of these
interventions is more effective in preventing postoperative vomiting when
compared to the exclusive use of drugs (RR = 0,56, CI 95% = 0,35 to 0,91; 9
trials, 687 participants). This therapy combination was not effective for the
prophylaxis of nausea (RR = 0,79, CI 95% = 0,55 to 1,13; 8 trials, 642
participants), but there was a reduction in the necessity for antiemetic drugs
in the postoperative period (RR = 0,61, CI 95% = 0,44 to 0,86; 5 trials, 419
participants) [7].
The mechanisms of action were
studied in an animal model [8] and some clinical trials, conducted in cancer
patients, have measured the effect of electrical stimulation under different
isolated or associated acupuncture points that are traditionally used in the
treatment of nausea and vomiting [3,4,8,9,10,11]. In an overview, there are many
discrepancies between these studies, but the PC6 was the most frequently
acupuncture point mentioned. The clinical characteristics of the patients
allocated were quite variable. The interventions also expose a quite different
between treatment time, weekly frequency and duration of the session. The
parameters used in electrical stimulation showed important differences, such as
the frequency of the electrical pulse, which in some studies was applied high
frequency others low frequency. Another aspect observed in these studies is a
tendency to applied electroacupuncture by transcutaneous acupoint electrical
stimulation (TAES) to avoid the risk of infection, inherent to the invasive
procedures. The results showed a favorable effect of TAES for the management of
nausea and vomiting, but there are many variations in these responses and
important discrepancies between the protocols.
The frequency of the electric pulse
is one of the main variables that make up the electric current, but there is no
consensus on whether high or low frequency is more effective. On the other
hand, the rate of incidence for nausea and vomiting is treatment-depended. Some
anticancer protocols are classified as high-grade emetic chemotherapy (HEC).
One of the most used HEC protocols combines anthracycline with
cyclophosphamide. This combination can induce nausea and vomiting up to 90% in
the first 24 hours after the infusion [12] and this specific characteristic
induced by the pharmacological association of the antineoplastic protocol
frequently used in the treatment of breast cancer, may be appropriate as a
clinical trial model to study antiemetic agents. Therefore, this study aims to
evaluate the acute effect of two frequencies of TAES on the incidence of nausea
and vomiting in volunteers undergoing a fixed regimen of HEC associated with
antiemetics usually prescribed in the care service.
Methods
This randomized, placebo-controlled
clinical study was conducted at the chemotherapy outpatient clinic after
approval by the local ethics committee (CAAE: 07489019.8.0000.5335) and
registered on the clinicaltrials.gov platform (NCT03145727). The study was
carried out in accordance with the ethical standards elaborated in the
Declaration of Helsinki 1964 and later amendments. Informed consent was
obtained from all individual participants included in the study (Form number:
3.265.023).
Sixty-one women (54 ± 11 years)
with breast cancer assigned to the HEC constituted by anthracycline combined
with cyclophosphamide were included. A fixed 8 mg ondansetron infusion (5-HT3
receptor antagonist) was administered prior to the chemotherapy session and
rescue doses of ondansetron and/or antihistamines and/or antidopaminergics were
instructed to use at home as needed. Only women with good functional capacity (Karnofsky score ≥ 70 points) and without previous (72
hours) nausea/vomiting symptoms were included. Patients with cognitive
limitations, undergoing concomitant radiotherapy, gastrointestinal and/or brain
metastases, cardiac pacemaker, or skin changes that did not allow electrical
stimulation to be performed were excluded.
Clinical evaluation
All participants received guidance
and training to record nausea and vomiting in the first 24h post-infusion of
HEC. The intensity/severity of nausea (visual analog scale 0-10) and vomiting
were recorded as recommended by the European Society of Medical Oncology (ESMO)
and the MASCC [12]. Home use of antiemetic drugs has been strictly controlled.
Telephone contact was maintained to answer questions and request form
(photographic) submission. The Edmonton Symptom Rating Scale (ESRS) was
incorporated into the form to control adverse symptoms [13].
Treatments
Eligible patients were randomized
into three groups: placebo (P); high frequency (HF) and low frequency (LF) of
the TEAS. An independent researcher used a random sequence generated at
randomizer.org to make opaque envelopes that were sealed and kept completely
confidential until the volunteers were assigned to one of the three
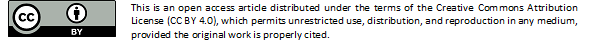
interventions. Neurodyn® III electro stimulator (Ibramed, Brazil) was applied 30-90 minutes before
chemotherapy. Reusable adhesive electrodes were positioned at the acupuncture point
PC6 on the contralateral infusion arm. One electrode was attached to two "tsuns" proximal to the flexion groove of the wrist in
the middle of the anterior surface of the forearm between the tendons of the
palmar muscles and radial flexors of the carpus, and the second electrode was
placed 5 cm above the CP6 towards the elbow (figure 1). For group P, the
electric current was adjusted with 75 Hz/200µs and intensity at the lower limit
of sensitivity. After 10 s, the intensity was reduced to zero, but the
electrodes were kept fixed for 30 minutes. In the LF and HF groups, the
currents were adjusted at the frequencies of 10 Hz and 150 Hz (respectively)
and both at the 200 µs pulse width. The stimulation time was 30 minutes and the
intensity was constantly increased to keep the
electric current at the upper tolerance limit.
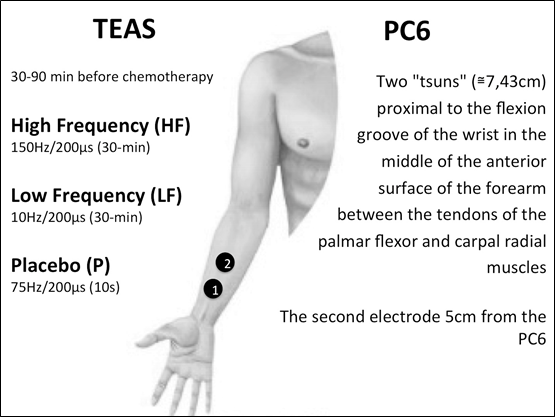
Fig. 1 - The PC6 acupuncture point is
represented by the anatomical location demarcated by the first black circle
(1). The second black circle (2) indicates the position where the second electrode
was connected to complete the electrical circuit. The intervention by
transcutaneous electrical stimulation (TEAS) was performed in the arm opposite
to the chemotherapy infusion
Statistical analysis
An independent researcher used
Shapiro-Wilk, Fisher's exact, G (Williams), chi-square, relative risk (RR),
relative risk reduction (RRR), absolute risk reduction (ARR) to test the acute
effect of TEAS on the incidence of nausea and vomiting. Mann-Whitney was
conducted to analyze the intensity of nausea and vomiting as well the systemic
symptoms (ESRS) between interventions and placebo.
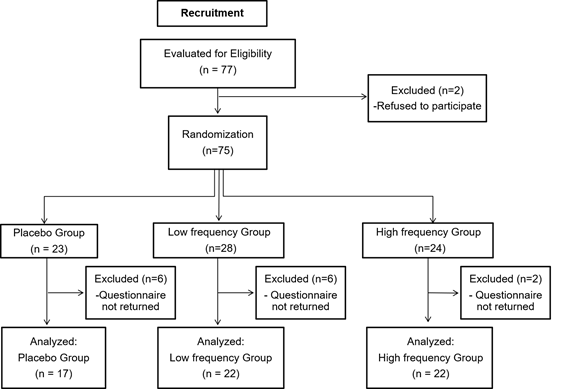
Fig. 2 - Study procedures flowchart
(CONSORT -2010)
Results
At baseline, 77 volunteers met the
eligibility criteria, but 75 patients agreed to participate in the study and
were randomized. However, only 61 completed and returned the nausea and
vomiting registering form (Figure 2). The total loss rate of the study sample
was 18%. There was homogeneity between the groups for age, type and phase of
chemotherapy cycles (Table I).
Table I - Clinical characteristics and
nausea symptoms and vomiting episodes in the first 24 hours after infusion of
high-grade emetic chemotherapy
The results were summarized using
values expressed in absolute terms and percentages, as well as mean and
standard deviation. The comparison between independent samples was performed
using Shapiro-Wilk, Chi-Square, G-test (Willians) and
Fisher’s exact tests
The incidence rate of nausea and
vomiting was statistically similar between groups. The total notifications of
nausea and vomiting were also similar between interventions. The same results
were found between interventions regarding the intensity of nausea symptoms.
Controlling the use of antiemetics in the domestic environment demonstrates
that the need for additional pharmacological management was very balanced
between interventions. The number of rescue doses of antiemetics was similar
between interventions, although the mean number of doses consumed in the LF and
HF groups represented 75% and 58%, respectively, of the mean number of doses
ingested in the placebo group.
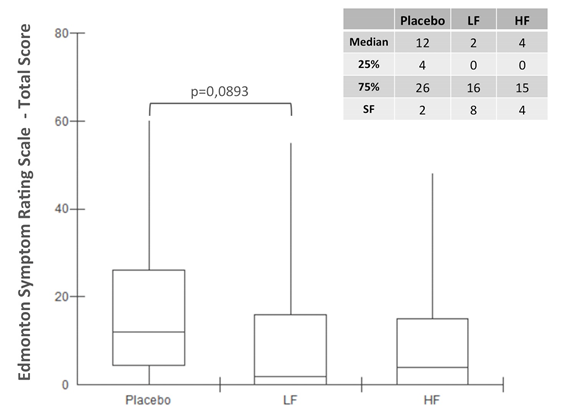
Fig. 3 - Edmonton Symptom Rating Scale
(ESRS) total score for placebo and low-frequency (LF) and high-frequency (HF)
TAES interventions. The box plot presents data through the median and maximum
and minimum values and interquartile range (25%-75%). The effect of LF and HF
was compared individually to placebo using the Mann-Whitney test. SF = symptom
free is the number of volunteers who remained asymptomatic during the first 24
hours after infusion of high-grade emetic chemotherapy
The relative risk of nausea was
very close between HF-TAES and placebo (RR = 0.97; p = 0.41; CI 95% = 0.49 to
1.91; RRR = 3%; ARR = 1.6%; NNT = 63), but when comparing LF-TAES with placebo,
the relative risk reduction was much more expressive. There is a high
probability of error in this estimation, but the magnitude of the relative risk
was substantially high (RR = 0.58; p = 0.17; CI 95% = 0.25 to 1.35; RRR = 42%;
ARR = 18%; NNT = 6).
The occurrence of symptoms assessed
by the ESRS was evenly distributed among the interventions (data not shown).
Symptom intensity was also equivalent between groups for pain, tiredness,
drowsiness, nausea, appetite, shortness of breath, depression and anxiety.
However, when compared to the placebo the LF-TAES showing a trend towards
improvement in the perception of well-being (p = 0.06) and in the total ESRS
score (p = 0.09) (Fig. 3). The number of volunteers who remain asymptomatic in
the first 24 hours after HEC infusion also tends to be smaller in the LF group
compared to placebo (RR = 0.72; p = 0.08; IC 95% = 0.50 to 1.03; RRR = 28%; ARR
= 24%; NNT = 5).
Discussion
TEAS applied to a unilateral PC6
acupuncture point, as proposed in this protocol, showed an uncertainly effect
in preventing nausea and vomiting in the first 24 hours after HEC infusion. The
incidence of nausea in placebo and HF-TAES interventions was proportionally
equivalent to the rates described by Roiola et al.
[12], but with a LF-TAES, there was almost half and, additionally, there was a
strong tendency to less intense manifestations. However, even with this
reduction in the proportion of the incidence of nausea, we cannot consider it
appropriate to attribute to LF-TEAS the effect of reducing the incidence of
nausea in the first 24 hours due to the high level of type I error observed.
The variability of the distribution reinforced the statistical requirement of
expanding the sample size. However, omitting this information would be an even
bigger mistake.
Nausea and vomiting can be
controlled by serotonin receptor inhibitors, antihistamines and
antidopaminergics [1,2] however, after cisplatin infusion, electroacupuncture
(applied to the acupuncture point VC12) showed lower plasma serotonin
concentration in animal [8]. This finding links the action of acupuncture's
antiemetic mechanism to state-of-the-art pharmacological therapies that involve
the serotonin-signaling pathway [14,15]. This connection between acupuncture
and pharmacological therapies became more unequivocal after the latest review
published by Lee et al. [7], PC6 acupoint stimulation was compared with
six different types of antiemetic drugs (metoclopramide, cyclizine,
prochlorperazine, droperidol, ondansetron and
dexamethasone), and no difference was found in the incidence of nausea (RR
0.91, 95% CI 0.75 to 1.10; 14 trials, 1.332 participants), vomiting (RR 0.93,
95% CI 0.74 to 1.17; 19 trials, 1.708 participants), or the need for rescue
antiemetic drugs (RR 0.87, 95% CI 0.65 to 1.16; 9 trials, 895 participants).
The review included clinical trials that tested the effect of various types of
PC6 acupuncture point stimulation (acupuncture, electro-acupuncture,
transcutaneous electrical acupoint stimulation, transcutaneous nerve
stimulation, laser stimulation, capsicum plaster, acu-stimulation
device, and acupressure) as a way to prevent postoperative nausea and vomiting
[5,6,7].
Another interesting result appeared
when Lee et al. [7] analyzed clinical trials that compared the effect of
PC6 stimulation combined with antiemetic drug and antiemetic drug alone. This
assessment showed that stimulation of acupuncture points as an adjunctive
therapy reduces the incidence of vomiting (RR 0.56, 95% CI 0.35 to 0.91; 9
trials, 687 participants) and the necessity for rescue antiemetic drugs (RR
0.61, 95% CI 0.44 to 0.86; 5 trials, 419 participants) but not nausea (RR 0.79,
95% CI 0.55 to 1.13; 8 trials, 642 participants). Our findings have progressed
in a slightly different direction. The incidence of vomiting and the
consumption of rescue antiemetic doses were very similar between the groups,
but the few occurrences of vomiting made the analysis unfeasible.
Postoperative nausea and vomiting
are clinically distinct from chemotherapy-induced nausea and vomiting,
particularly when HEC is infused, but there is some
evidences that acupoint therapy could be useful to prevent nausea and vomiting
induced by chemotherapy [16,17]. In patients under chemotherapy for lung
cancer, the acupoint stimulation drastically decreased the nausea and vomiting
at Grade II-IV when compared to the control group (RR, 0.46; 95% CI, 0.37-0.51;
P = 1E-5, 8 studies, 501 patients). In addition, increases in hemoglobin,
platelets and immunomodulatory response markers were also observed (increase of
IL-2, CD3+ and CD4+ T cells and NK cells) [18]. Some studies showed an
advantage in the improvement of performance status and quality of life
(EORCT-QLQ-C30) [19].
The overall score of the main
symptoms evaluated in our study showed a strong favorable trend for LF-TEAS.
The benefits of LF-TAES on cancer-related symptoms open an opportunity for
clinical studies on the effect of electro stimulation on the quality of life of
patients undergoing anticancer treatment. The feeling of well-being was the
best scored aspect by patients undergoing LF-TAES. In this sense, another
important finding was the substantial number of volunteers who remained
asymptomatic after the intervention with LF-TAES.
Nonetheless, our results indicate
the possibility that the frequency used in the TAES may have a relevant role in
the effects size of the intervention. This hypothesis was described before, but
Xie et al. [9] found no statistical
significant differences between placebo and low frequency (4Hz) applied under
multiple acupuncture points simultaneously stimulated (PC6, E36 and LI4; with
electrode patch placed on the skin surface, and intensity between 7-15 mA;
twice a day, for 30 min to 60 min by six consecutive days) combined with a
fixed dose of an antagonist of serotonin (palonosotron,
0.25 mg). The patients (active acupuncture, n = 72 or placebo acupuncture, n =
70) were followed for 5 days after cisplatin infusion (60 mg) and no significant
differences were found.
Interpersonal variations play an
important role in the development of anticancer chemotherapy-induced
nausea/vomiting. As described by McKeon et al. [10], chemotherapy side
effects worsen after the first infusion cycle. In this regard, it is worth
noting that 56% of the volunteers who participated in our study had completed
the first cycle of chemotherapy treatment. For prophylaxis purposes, evaluating
the effect of antiemetic strategies in volunteers free of cumulative effects is
the best scenario, but the interpersonal variations described in the literature
bring with them the need for studies with large samples, especially when the
incidence rate of symptoms is low, as observed in our study in relation to
episodes of vomiting. An interesting alternative would be to evaluate the
adjuvant effect of TAES in the management of nausea and vomiting in patients
who suffer recurrently from these disorders. Including only patients with
nausea and vomiting refractory to antiemetic therapies could be useful to
increase the accuracy of detection of the antiemetic effect of TAES. With more
occurrences of symptoms, the consistency of the adjuvant effects of TAES could
be explored in future clinical trials. In addition, the hypothesis of the
existence of other antiemetic action pathways of acupuncture could be tested.
On the other hand, we must consider
that the antiemetic mechanism of TAES is the same as that of some antiemetic.
Duplicating or intensifying the same antiemetic pathway may be ineffective in
preventing symptoms of nausea and vomiting, as this could be achieved simply by
increasing drug doses. Therefore, it is possible that TAES involves other
signaling pathways, but this hypothesis still needs to be confirmed. Our
results may be contributing to this possibility, whether the recommended dose
in routine cancer care is in fact the best dose established by the evidence
described in the literature.
Even though our results were
inconclusive due to intergroup variations and small sample size, this clinical
trial supports the possibility of using TEAS as an adjuvant therapy for the
management of undesirable effects of antineoplastic treatment and brings
additional information that reinforces the role of stimulation frequency in the
action pathway.
Conclusion
The results were inconclusive and
reinforce the need to increase the sample size. However, there is no evidence
to exclude the possibility of an antiemetic benefit from the use of TEAS as
adjunctive antiemetic therapy. Keeping the proportion of reduction in the
incidence of nausea observed in the intervention with LF-TEAS, it is perfectly
expected that in studies with larger sample sizes, this finding will indeed be
confirmed. The relevance of further studies is centered on the high number of
patients undergoing anticancer therapies who may benefit from this therapeutic
modality.
Acknowledgements
Eliane Goldberg Rabin, providing acupuncture knowledge support and article
review.
Conflict of interest
The authors have no conflict of
interest.
Study funding
This study was awarded the National
Multiprofessional Residency Scholarship Program of
the Ministry of Education of the Federal Government of Brazil, obtaining
financial support for conducting research in public health.
Authors' contributions
Concepção
e desenho da pesquisa:
Fattori RA; Macagnan FE; Obtenção
de dados: Fattori RA; Schlöttgen
J; Loro FL; Carvalho PL; Análise e interpretação dos dados: Fattori RA; Macagnan FE; Análise
estatística: Macagnan FE; Redação do
manuscrito: Fattori RA; Macagnan
FE; Schlöttgen J; Loro FL; Carvalho PL; Orso R; Revisão crítica do manuscrito quanto ao conteúdo
intelectual importante: Fattori RA; Macagnan FE
References
- Herrstedt J, Roila F, Warr D, Celio L, Navari RM, Hesketh PJ, Chan A, Aapro MS. 2016 Updated MASCC/ESMO Consensus
Recommendations: Prevention of Nausea and Vomiting Following High Emetic Risk
Chemotherapy. Support Care Cancer. 2017 Jan;25(1):277-88. doi: 10.1007/s00520-016-3313-0 [Crossref]
- Rapoport B, Schwartzberg L, Chasen M, Powers D, Arora S, Navari R, Schnadig I. Efficacy and safety of rolapitant for prevention of chemotherapy-induced nausea and vomiting over multiple cycles of moderately or highly emetogenic chemotherapy. Eur J Cancer. 2016 Apr;57:23-30. doi: 10.1016/j.ejca.2015.12.023 [Crossref]
- Ozgür TM, Sandıkçı Z, Uygur MC, Arık AI, Erol D. Combination of transcutaneous electrical nerve stimulation and ondansetron in preventiOzgür TM, Sandıkçı Z, Uygur MC, Arık AI, Erol D cisplatin-induced emesis. Urol Int. 2001;67(1):54-8. doi: 10.1159/000050945 [Crossref]
- Dou P-H, Zhang D-F, Su C-H, Zhang X-L, Wu Y-J. Electrical stimulation on adverse events caused by chemotherapy in patients with cervical cancer: A protocol for a systematic review of randomized controlled trial. Medicine (Baltimore). 2019 Feb;98(7):e14609. doi: 10.1097/MD.0000000000014609 [Crossref]
- Lee A, Done ML. Stimulation of the wrist acupuncture point P6 for preventing postoperative nausea and vomiting. The Cochrane database Syst Rev. 2004;(3):CD003281. doi: 10.1002/14651858.CD003281.pub3 [Crossref]
- Lee A, Fan LT. Stimulation of the wrist acupuncture point P6 for preventing postoperative nausea and vomiting. Cochrane database Syst Rev. 2009;(2):CD003281. doi: 10.1002/14651858.CD003281.pub3 [Crossref]
- Lee A, Chan SKC, Fan LTY. Stimulation of the wrist acupuncture point PC6 for preventing postoperative nausea and vomiting. Cochrane database Syst Rev. 2015(11):CD003281. doi: 10.1002/14651858.CD003281.pub4 [Crossref]
- Cui Y, Wang L, Shi G, Lui L, Pei P, Guo J. Electroacupuncture alleviates cisplatin-induced nausea in rats. Acupunct Med. 2016 Apr;34(2):120-6. doi: 10.1136/acupmed-2015-010833 [Crossref]
- Xie J, Chen L-H, Ning Z-Y, Zhang C-Y, Chen H, Chen Z, et al. Effect of transcutaneous electrical acupoint stimulation combined with palonosetron on chemotherapy-induced nausea and vomiting: a single-blind, randomized, controlled trial. Chin J Cancer. 2017;36(6). doi: 10.1186/s40880-016-0176-1 [Crossref]
- McKeon C, Smith CA, Gibbons K, Hardy J. Electro Acupuncture versus sham acupuncture and no acupuncture for the control of acute and delayed chemotherapy-induced nausea and vomiting: a pilot study. Acupunct Med. 2015 Aug;33(4):277-83. doi: 10.1136/acupmed-2015-010781 [Crossref]
- Chen B, Hu S, Liu B, Zhao T, Li B, Liu Y, et al. Efficacy and safety of electroacupuncture with different acupoints for chemotherapy-induced nausea and vomiting: study protocol for a randomized controlled trial. Trials. 2015 May;16:212. doi: 10.1186/s13063-015-0734-x [Crossref]
- Roila F, Herrstedt J, Aapro M, Gralla RJ, Einhorn LH, Ballatori E, et al. Guideline update for MASCC and ESMO in the prevention of chemotherapy- and radiotherapy-induced nausea and vomiting: results of the Perugia consensus conference. Ann Oncol Off J Eur Soc Med Oncol. 2010 May;21 Suppl 5:v232-43. doi: 10.1093/annonc/mdq194 [Crossref]
- Bruela E,
Kuehn N, Miller MJ, Selmser P, Macmillan K. The
Edmonton Symptom Assessment System (ESAS): a simple method of the assessment of
palliative care patients. J Palliat Care.
1991;2(7):6-9. https://pubmed.ncbi.nlm.nih.gov/1714502/
- Herrstedt J. The latest consensus on antiemetics. Curr Opin Oncol. 2018 Jul;30(4):233-39. doi: 10.1097/CCO.0000000000000450 [Crossref]
- Zhang Z, Zhang Y, Chen G, Hong S, Yang Y, Fang W, Luo F, Chen X, Ma Y, Zhao Y, Zhan J, Xue C, Hou X, Zhou T, Ma S, Gao F, Huang Y, Chen L, Zhou N, Zhao H, Zhang Li. Olanzapine-based triple regimens versus neurokinin-1 receptor antagonist-based triple regimens in preventing chemotherapy-induced nausea and vomiting associated with highly emetogenic chemotherapy: a network meta-analysis . Oncologist 2018 May;23(5):603-16. doi: 10.1634/theoncologist.2017-0378 [Crossref]
- Ezzo J, Vickers A, Richardson MA, Allen C, Dibble SL, Issell B, Lao L, Pearl M, Ramirez G, Roscoe AJ, Shen J, Shivnan J, Streitberger K, Treish I, Zhang G. Acupuncture-point stimulation for chemotherapy-induced nausea and vomiting. J Clin Oncol. 2005;23(28):7188-98. doi: 10.1002/14651858.CD002285.pub2 [Crossref]
- Ezzo JM, Richardson MA, Vickers A, Allen C, Dibble SL, Issell BF, Lao L, Pearl P, Ramirez G, Roscoe Ja, Shen J, Shivnan JC, Streitberger K, Treish I. Acupuncture-point stimulation for chemotherapy-induced nausea or vomiting. Cochrane Database Syst Rev. 2006;(2):CD002285. doi: 10.1002/14651858.CD002285.pub2 [Crossref]
- Han JS. Acupuncture: neuropeptide release produced by electrical stimulation of different frequencies. Trends Neurosci. 2003 Jan;26(1):17-22. doi: 10.1016/s0166-2236(02)00006-1 [Crossref]
- Chen H-Y, Li S-G, Cho WC, Zhang Z-J. The role of acupoint stimulation as an adjunct therapy for lung cancer: a systematic review and meta-analysis. BMC Complement Altern Med. 2013 Dec 17;13:362. doi: 10.1186/1472-6882-13-362 [Crossref]