Fisioter Bras 2022;23(4):633-44
REVIEW
Effects of aquatic physical therapy on balance in post-cerebrovascular
accident patients: an integrative review
Efeitos da
fisioterapia aquática no equilíbrio de pacientes pós-acidente vascular
encefálico: uma revisão integrativa
Antonia Cristina Silva dos Santos*, Bárbara Bernabé Pratti*, Deisiane Pereira de Lima*, Larissa Torquato de Carvalho*, Taynara Esperança Silva Santos*, Elivelton
Sousa Montelo*, Jardeson Rocha Filgueiras*,
Jaqueline Fernandes do Nascimento**, Tassiane Maria
Alves Pereira***, Jéssica Inara de Brito Siqueira***,
Lucas da Silva Nascimento***, Ariel Soares Teles****, Marco Orsini*****,
Janaína de Moraes Silva******, Nélio Silva Souza*******, Ariela
Thaís Albuquerque da Silva***, Silmar
Teixeira********, Victor Hugo do Vale Bastos*********
*Universidade Federal do
Delta do Parnaíba (UFDPAR), Parnaíba, Brazil,
**Universidade
Iguaçu (UNIG), RJ, ***UFDPAR, Laboratório de Mapeamento
Cerebral e
Funcionalidade (LAMCEF/UFDPAR), ****Professor associado do Instituto
Federal do Maranhão (IFMA), *****Professor associado e
coordenador do Mestrado de Neurologia
da Universidade Severino Sombra, RJ, professor da UNIG,
******Laboratório de
Mapeamento Cerebral e Funcionalidade, LAMCEF/UFDPAR,
Pós-Doutorado em Ciências
Biomédicas, UFDPAR, *******Professor assistente na Centro
Universitário Serra
dos Órgãos (UNIFESO), ********Professor Associado da
UFDPAR, Laboratório de Neuroinovação Tecnológica & Mapeamento Cerebral (NitLab) UFDPAR, *********Laboratório de Mapeamento Cerebral
e Funcionalidade, LAMCEF/UFDPAR, Associated Professor associado da UFDPAR
Received: May 10, 2022; Accepted:
July 6, 2022.
Correspondence: Victor Hugo Bastos, Universidade
Federal do Delta do Parnaíba (UFDPAR), Avenida São Sebastião, 2819, UFPI / CMRV
- LAMCEF - Block 16, Room 6, 64202-020 Parnaíba PI, Brazil
Antonia
Cristina Silva dos Santos: antoniacristinaacss@gmail.com
Bárbara
Bernabé Pratti: barbarabrpratti@gmail.com
Deisiane
Pereira de Lima: deysianne.lima56@gmail.com
Larissa
Torquato de Carvalho: larissatorquatodcarvalho@gmail.com
Elivelton Sousa Montelo:
elvtonmont@outolook.com
Jardeson Rocha Filgueiras: jardesonrocha2@gmail.com
Jaqueline
Fernandes do Nascimento: jac.fn@hotmail.com
Tassiane Maria Alves Pereira:
tassiane.alves07@gmail.com
Jéssica Inara de Brito Siqueira: jessicainarabrito@hotmail.com
Lucas da
Silva Nascimento: lucas_silvaphb@hotmail.com
Ariel
Soares Teles: ariel.teles@ifma.edu.br
Marco
Orsini: orsinimarco@hotmail.com
Sergio
Nader: sergionader@yahoo.com.br
Janaína de
Moraes Silva: fisiojanainams@gmail.com
Nélio
Silva Souza: neliosds@gmail.com
Ariela Albuquerque:
ariela.thais@gmail.com
Silmar Teixeira:
silmarteixeira@ufpi.edu.br
Victor
Hugo do Vale Bastos, victorhugobastos@ufpi.edu.br
Abstract
Introduction: Stroke can be characterized as ischemic or
hemorrhagic, and in individuals with this condition there is a decrease in
their functional independence, which reproduces a decrease in quality of life.
Aquatic physical therapy is an approach that stands out in the rehabilitation
of these patients, mainly due to the increase in treatment due to the
environment. Subjects: Patients with stroke. Objective: To update the
literature on the effects of aquatic therapy on the balance of post-stroke
patients, verifying the most used evaluation methods. Methods: The
literature search was performed in 6 Pubmed, Web of
Science, Scopus, Medline, PEDro and Cochrane
databases, using the association of descriptors, keywords and Boolean operators
“Stroke” AND “Hydrotherapy” OR “Hydrokinesiotherapy”
OR “Aquatic Physiotherapy” AND “Balance”, stipulating inclusion and exclusion
criteria. Results: Of the 259 studies identified, 14 were selected for
analysis and qualitative synthesis. Overall, the results showed significant
differences in the balance of individuals with cerebral vascular accident after
aquatic therapy. Conclusion: When compared to conventional
neurofunctional physical therapy techniques, aquatic physiotherapy has superior
efficacy. The most used evaluative means are the Berg Balance Scale and Timed
Up and Go, as they are tools that are quick and easy to apply, in addition to
being highly effective, demonstrating the relevance of the study in aspects of
functional recovery in the midst of dysfunctions arising from neurological
impairments.
Keywords: stroke; hydrotherapy; physical therapy modalities;
postural balance; quality of life.
Resumo
Objetivo: Atualizar a literatura sobre os
efeitos da terapia aquática no equilíbrio de pacientes pós-AVE e verificar os métodos
avaliativos mais empregados. Métodos: A busca na literatura foi
realizada em 6 bases de dados Pubmed, Web of Science, Scopus, Medline, PEDro
e Cochrane, utilizando a associação de descritores, palavras-chave e operadores
booleanos “Stroke” AND “Hydrotherapy”
OR “Hydrokinesiotherapy” OR “Aquatic
Physiotherapy” AND “Balance”, estipulando critérios
de inclusão e exclusão. Resultados: Dos 259 estudos identificados, foram
selecionados 14 para análise e síntese qualitativa. No geral, os resultados
evidenciaram diferenças significativas no equilíbrio de indivíduos com AVE após
terapia aquática. Conclusão: Quando comparada às técnicas de
fisioterapia neurofuncional convencionais, a
fisioterapia aquática apresenta superioridade de eficácia. Os meios avaliativos
mais utilizados são a Berg Balance Scale e a Timed Up and
Go por se tratarem de ferramentas de rápida e fácil aplicação, além de alta
eficácia, demonstrando a relevância do estudo em aspectos de reabilitação
funcional em meio a disfunções advindas de comprometimentos neurológicos.
Palavras-chave: hidroterapia; acidente vascular
encefálico; equilíbrio postural; fisioterapia; qualidade de vida.
Introduction
The cerebral vascular accident (CVA), more commonly
known as "stroke", is widely classified as ischemic or hemorrhagic.
In either category, the result is a loss of blood flow, nutrients, and oxygen
to a region of the brain, resulting in neuronal damage and subsequent
neurological deficits [1]. There are numerous etiologies that can cause a CVA and
one of the most common causes is the formation of a plaque due to the
accumulation of low-density lipoprotein (LDL) cholesterol. The most common risk
factors are hypertension, diabetes mellitus and smoking [2].
The CVA harms the descending neural pathways due to
injuries of the superior motor neurons, if it occurs in the middle cerebral
artery, the most common site for this type of injury, corticospinal and
corticocerebellar tract connections will be affected [3]. In post-CVA
individuals, impairments in gait and balance will lead to decreased functional
independence, limited mobility and social interaction, in addition to
presenting weakness, spasticity, lack of coordination and deficiencies, which
can lead to costly complications [4,5,6,7]. Through the exposed complications,
physical therapy can contribute to reducing the limitations and quality of life
of these individuals [8].
Regarding the therapeutic strategies for CVA, aquatic
physical therapy is widely used in the treatment of these individuals. The
aquatic environment is suggested as the ideal medium due to its physical
properties, buoyancy, hydrostatic pressure, density, viscosity and
thermodynamics, optimizing the effects of rehabilitation [9]. Hydrotherapy cover traditional approaches, such as the Halliwick Method and Bad Ragaz,
and complementary medicine techniques [10,11], which have shown promising
effects on balance, strength and mobility after CVA [12,13]. There are several
clinical studies addressing hydrotherapy in post-CVA rehabilitation, however,
there is a shortage in the analysis of evaluative measures. Thus, the aim of
this study is to update the literature on the effects of aquatic therapy on the
balance of post-CVA patients and verify the most used evaluation methods.
Methods
A systematic search was performed in 6 databases: Pubmed, Web of Science, Scopus, Medline, PEDro and Cochrane. In this sense, an association of
descriptors, keywords and Boolean operators was used: “Stroke” AND
“Hydrotherapy” OR “Hydrokinesiotherapy” OR “Aquatic
Physiotherapy” AND “Balance”. As inclusion criteria, only randomized clinics
published in English in the period from 2016 to 2021 and available in full were
delimited, which addressed aquatic physical therapy techniques in the balance
of individuals with CVA with different therapies or no intervention as a
comparison. In this study, studies on animals, systematic reviews or
meta-analyses are excluded.
Five authors selected the articles, following the
process of choosing the title, reading the abstracts and lastly the reading of
the full text. The studies that met the inclusion criteria were analyzed and
the following data extracted: author, year of publication, population design,
evaluative measures, interventions and results (Table I). The PICOS strategy
(P-Population; I-Intervention; C-Comparison; O-Outcomes; S-Study type) was used
to search the databases and guide the research question (Chart 1). According to
the established “PICOS” strategy, the guiding question of the research was: “What
is the effect of aquatic physical therapy techniques on the balance of
individuals with CVA?” The assessment of the methodological quality of the
included studies was performed using the PEDro scale
(Physiotherapy Evidence Database) (Table II), which qualifies clinical trials
following 11 criteria with scores from 1 to 10, with the first criterion not
being scored.
Table I - Characteristics of the selected studies
Chart 1 - Elements of the PICOS strategy
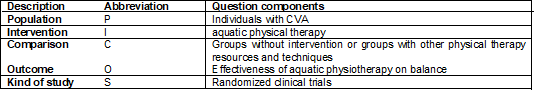
Source: Own Authorship (2021).
Table II - Analysis of the methodological quality of the
included studies
Results
Based on the search strategies, 259 articles were
identified in the databases, of which 58 were excluded because they were
duplicates. After the reading, 14 studies were selected for the specific
analysis of methodological quality and for the qualitative synthesis, this to
compose the structural framework of this study, but other articles were
selected. These were intended to support stages of the study such as
introduction and discussion. This new selection of studies was blindly
performed by 3 other authors and a fourth author selected what was in common
among the first 3 authors. Thus, we ended up with 36 articles in total, with
the 14 specific articles selected by the criteria established for quality
analysis already in these. The selection process is shown in figure 1.
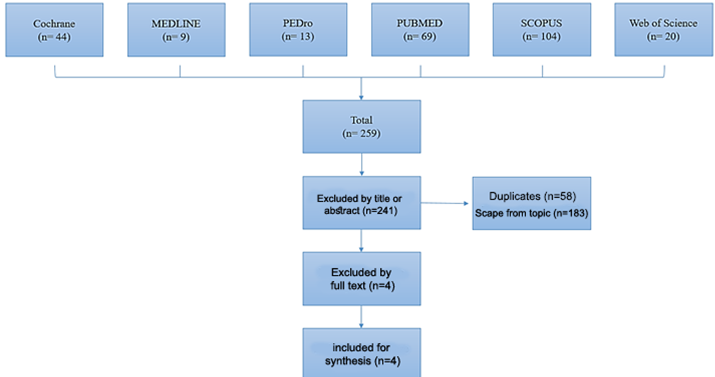
Source: Own Authorship (2021)
Figure 1 - Study selection process
The study investigated 430 participants aged 20 to 85
years who were diagnosed with CVA. All surveys included had balance as one of
the outcomes, using several evaluative scales, such as the Berg Balance Scale
(BBS), Sit Up Test (TSL), Timed Up and Go (TUG), Tinetti Test, Test of
Stability Limit, Functional Range Test (TAF) and Barthel Index.
Discussion
The present study aimed to update the literature on
the effects of aquatic therapy on the balance of post-CVA patients, verifying
the most used evaluative methods. In this sense, it was observed in the
literature that post-CVA individuals have decreased functional independence,
limited mobility, resulting from deficits in gait and postural balance,
generating difficulties in the process of functional recovery [4,5]. Functional
recovery after CVA has been shown to be very important in function recovery and
there are many tools that can be used [14]. The popularity of aquatic physical
therapy has increased among neurological physiotherapists and researchers due
to the benefits that water provides [15]. The aquatic environment acts as a
partial support to the body, allowing the mobilization of joints and, in addition,
provides motor and sensory stimuli that can induce plasticity [16] and presents
itself as an alternative for training in balance, gait and weight transfer, due
to its physical characteristics [5]. Therefore, it is essential to carry out a
more focused assessment of such impairments in post-CVA patients.
A water exercise technique that has been growing among
neurological patients is Ai Chi, which is composed of movements that address
characteristics of postural stability training. Some studies demonstrate the
effectiveness of Ai Chi, as can be seen in Ku et al. [19], who showed
positive effects during excursion speed and movement in the stability limit
test in the group treated with the Ai Chi technique. Similar to the previous
study [19], Pérez-De la Cruz [17], in two studies, evaluated the effects of Ai
Chi compared to two other interventions over a 12-week period: dry land therapy
and associated aquatic therapy with dry land therapy [28]. In Pérez-De la Cruz
[28], Ai Chi was associated with calming activity, in which significant
differences were observed for the combined therapy group in BBS, TSL, Tandem
Posture Test and TUG. In Pérez-De la Cruz [17] the technique was associated
with a cooling program, in which the group of therapy on land and aquatic
therapy obtained significant results in EVA, total Tinetti, 360-degree rotation
and TSC -30.
Temperoni et
al. [18] performed two therapeutic approaches in their study that lasted 4
weeks, comparing a sequential postural change training with a standard aquatic
therapy plus warm-up, stretching, recruiting and walking exercises, noting
benefits in both groups, but with superiority in the combined therapy group in
the BBS and EQVE-AVE scales. This study was characterized as the first to use
sequential training. Babaeipour et al. [22]
programmed two aquatic interventions to compare with a control group without
intervention. The first program included supervised exercises in shallow water;
the second applied supervised exercises in deep water, both with load
progression, with a significant difference in the two interventional groups in
the BBS scores compared to the control group, which demonstrates the
effectiveness of aquatic training whatever the depth.
Saleh et al. [31] compared terrestrial training
with aquatic training, showing significant effects in patients treated in the
aquatic environment compared to terrestrial, with superiority in the OASI, APSI
and MLSI parameters. Corroborating these results, Noh [33] and Montagna [34] demonstrated in their studies that when
compared to the conventional therapy group, the aquatic therapy group had
significant changes in BBS scores, forward and backward weight bearing skills,
limbs and knee flexor strength, with positive effects on postural balance [33,34]
as well as Berger [35]. Cha et al. [24] compared rehabilitation on
conventional soil with aquatic therapy associated with rehabilitation on
conventional soil, obtaining significance in the TUG balance index [29],
similar to the findings of Chan et al. [26] and Eyvaz
et al. [23] who also obtained significant values in the balance
parameters assessed in the combination therapy group.
Lim [32] in their study applied a conventional
physical therapy program in two groups, both of which performed gait training
on an underwater treadmill with different resistances, in which group 1
performed with jet resistance against the anterior region of the leg, and in
group 2, an anklet weighing 5% of the participant's body weight was applied.
Both groups showed benefits, however, the jet resistance group had significance
in static and dynamic balance skill scores, which can be explained, according
to the authors, as resistance at the ankle level limiting other areas,
preventing buoyancy in all areas below the knee.
Franciulli [21]
applied an intervention lasting 9 weeks, divided into a group that performed
aerobic training (walking on the ground, treadmill and relaxation) and the
other aerobic training in water, in which both interventions positively affected
the TUG scores and BBS. A recent meta-analysis by Veldema
and Jansen [36] demonstrated that aquatic therapy has superior efficacy in
balance, walking, muscle strength, proprioception, health-related quality of
life, physiological indicators, and cardiorespiratory fitness. However, they
concluded that methods such as Halliwick, Ai Chi,
Watsu or Bad Ragaz Ring are the most effective in the
variables mentioned and that walking on a treadmill is less effective than
them, thus outlining a more effective treatment.
In the study by Zhu [24] they compared two
interventions in their study: the first consisted of water therapy with
stretching of joints and major muscle groups, strengthening and balance
exercises for upper limbs, lower limbs and training on a water treadmill, while
the second therapy land with stretching, exercises for strengthening and
mobility of the trunk, training on a treadmill. The results were positive in
both groups, due to trunk mobility movements and lower limb strengthening
exercises, however, the aquatic therapy group obtained significance in the TAF
and 2-min walk test due to water buoyancy and buoyancy training challenging the
balance even more.
Bobath's
approach is a method that involves the regulation of muscle tone and allows the
restoration of functional movement through motor learning principles,
characterized as a neurodevelopmental treatment. Kim et al. [25]
compared the neurodevelopment intervention associated with dual-task aquatic
training with individuals who underwent only the neurodevelopmental treatment,
in which they demonstrated effects that are more significant after treatment in
all balance and gait tests in the group of combination therapy. Park et al.
[20] also presented differences in the scale of trunk impairment, postural
assessment and functionality.
Regarding the evaluative tools, most of the studies
included for synthesis more than one instrument to assess balance and
functional capacity. The BBS was present in 10 of the 14 articles [17,18,19,20,21,22,23,24,25,26], as
it is an easy and quick scale to apply, in addition to having high reliability
[27], followed by the TUG which was present in 8 of the 14 articles [21,22,23,24,25,26,28,29], as it is a reliable, valid and easy-to-administer clinical tool to
assess advanced functional mobility after a CVA [30].
This integrative review has relevant points, some
limitations found may be related to the heterogeneity of objectives, the
duration of the protocols, effects found in each study, and despite these
limitations, the evidence found suggests that aquatic physical therapy is an
effective treatment for balance in post-CVA patients. A strong point found is
that most studies according to the PEDro
methodological quality scale (Physiotherapy Evidence Database) have grades with
quality ranging from moderate to high.
Conclusion
As for the facts described, we can conclude that
aquatic physical therapy produces significant effects in the treatment of
balance disorders in post-CVA patients, showing greater effectiveness when
compared to conventional neurofunctional physical therapy techniques. Regarding
the evaluative measures of balance, the BBS and the TUG proved to be the gold
standard, given that they were the most used scales for being easy and quick to
apply. With regard to the most suitable techniques, there was heterogeneity
between the studies, which made our comparison difficult. Thus, it is necessary
research that seeks results more accurate to define a linear and standardized
therapeutic approach.
Conflict of interest
The authors do not have any conflicts of interest.
Financing source
There were no external funding sources for this study.
Authors’ contribution
Conception and design of the research: Santos ACS, Pratti BB, Lima DP; Data collection: Carvalho
LT, Santos TES, Albuquerque A, Nader S; Data analysis and interpretation:
Montelo ES, Filgueiras JR, Nascimento JF; Writing the manuscript: Santos
ACS, Pratti BB, Lima DP, Carvalho LT, Santos TES; Critical review of
the manuscript for important intellectual content: Pereira TMA,
Siqueira JIB, Nascimento LS; Silva JM, Orsini M, Souza NL, Teles AS, Teixeira
S, Bastos VHV
References
- Zafar F, Tariq W, Shoaib R, Shah A, Siddique M, Zaki
A, et al. Frequency of ischemic stroke subtypes based on toast classification
at a tertiary care center in Pakistan. Asian J Neurosurg
2018;13(4):984-9. doi: 10.4103/ajns.AJNS_365_16 [Crossref]
- Hankey GJ. Stroke. Lancet 2017;389(10069):641-54. doi: 10.1016/S0140-6736(16)30962-X [Crossref]
- Lundy-Ekman L. Neuroscience: Fundamentals for rehabilitation. London: WB
Saunders; 1998. doi: 10.1016/S0964-3397(98)80696-4 [Crossref]
- Koch G, Bonnì S, Casula EP, Iosa M, Paolucci S, Pellicciari MC, et al. Effect of cerebellar stimulation on gait and balance recovery in patients with hemiparetic stroke: a randomized clinical trial. JAMA Neurol 2019;76(2):170. doi: 10.1001/jamaneurol.2018.3639 [Crossref]
- Chae CS, Jun JH, Im S, Jang Y, Park G. Effectiveness of hydrotherapy on balance and paretic knee strength in patients with stroke: a systematic review and meta-analysis of randomized controlled trials. Am J Phys Med Rehabil 2020;99(5):409-19. doi: 10.1097/PHM.0000000000001357 [Crossref]
- Donkor ES. Stroke in the 21st century: a snapshot of the burden, epidemiology, and quality of life. Stroke Res Treat 2018;2018:1-10. doi: 10.1155/2018/3238165 [Crossref]
- Francisco GE, McGuire JR. Poststroke spasticity management. Stroke 2012;43(11):3132-6. doi: 10.1161/STROKEAHA.111.639831 [Crossref]
- Verbeek JM, van Wegen E, van Peppen R, van der Wees PJ, Heniks E, Rietberg M, et al. What is the evidence for physical therapy poststroke? A systematic review and meta-analysis. PloS One 2014;9(2):e87987. doi: 10.1371/journal.pone.0087987 [Crossref]
- Becker BE. Aquatic therapy: scientific foundations and clinical rehabilitation
applications. PM R 2009;1(9):859. doi: 10.1016/j.pmrj.2009.05.017
- Martin J. The Halliwick Method. Physiotherapy
1981;67(10):288. PMID: 6460262.
- Boyle AM. The Bad Ragaz ring method.
Physiotherapy 1981;67(9):265.PMID: 7291338
- Mehrholz J, Kugler J, Pohl M, Mehrholz J. Water-based exercises for improving activities of daily living after stroke. Cochrane Database Syst Rev 2011;2011(1):CD008186. doi: 10.1002/14651858.CD008186.pub2 [Crossref]
- Iliescu AM, McIntyre A, Wiener J, Iruthayarajah J, Lee A, Caughlin S, et al. Evaluating the effectiveness of aquatic therapy on mobility, balance, and level of functional independence in stroke rehabilitation: a systematic review and meta-analysis. Clin Rehabil 2020;34(1):56-68. doi: 10.1177/0269215519880955 [Crossref]
- Makiyama TY, Battistella LR, Litvoc J, Martins LC. Estudo sobre a qualidade de vida de pacientes hemiplégicos por acidente vascular cerebral e de seus cuidadores. Acta Fisiátr 2004;11(3):106-9. doi: 10.5935/0104-7795.20040004 [Crossref]
- Salinet AS. Hidroterapia e reabilitação cardiorrespiratoria após acidente vascular cerebral. Rev Neurocienc 2012;20(2):183-4. doi: 10.34024/rnc.2012.v20.8270 [Crossref]
- Meneghetti CHZ, Carraro L, Leonello LA, Batistella ACT, Ferracini Júnior LC. A influência da fisioterapia aquática na função e equilíbrio no acidente vascular cerebral. Rev Neurocienc 2012;20(3):410-4. doi: 10.34024/rnc.2012.v20.8268 [Crossref]
- Pérez-de la Cruz S. Comparison of aquatic therapy vs. dry land therapy
to improve mobility of chronic stroke patients. Int J Environ Res Public Health
2020;17(13):4728. doi: 10.3390/ijerph17134728 [Crossref]
- Temperoni G, Curcio A, Iosa M, Mangiarotti MA, Morelli D, De Angelis S, et al. A water-based sequential preparatory approach vs. conventional aquatic training in stroke patients: a randomized controlled trial with a 1-month follow-up. Front Neurol 2020;11:466. doi: 10.3389/fneur.2020.00466 [Crossref]
- Ku P, Chen S, Yang Y, Lai T, Wang R. The effects of Ai Chi for balance in individuals with chronic stroke: a randomized controlled trial. Sci Rep 2020;10(1):1201. doi: 10.1038/s41598-020-58098-0 [Crossref]
- Park H, Lee H, Lee S, Lee W. Land-based and aquatic trunk exercise program improve trunk control, balance and activities of daily living ability in stroke: a randomized clinical trial. Eur J Phys Rehabil Med 2019;55(6):687. doi: 10.23736/S1973-9087.18.05369-8 [Crossref]
- Franciulli PM, Bigongiari A, Grilletti JVF, Mazuchi FAS, Amadio AC, Mochizuki L. The effect of aquatic and treadmill exercise in individuals with chronic stroke. Fisioter Pesqui 2019;26(4):353-9. doi: 10.1590/1809-2950/17027326042019 [Crossref]
- Babaeipour H, Sahebozamani M, Mohammadipour F, Vakilian A. The effect of training at different depths on the balance of chronic ischemic stroke patients. IJAEP 2018;7(3):68-78. doi: 10.30472/ijaep.v7i3.295 [Crossref]
- Eyvaz N, Dundar U, Yesil H. Effects of water-based and land-based exercises on walking and balance functions of patients with hemiplegia. Neuro Rehabilitation 2018;43(2):237-46. doi: 10.3233/NRE-182422 [Crossref]
- Zhu Z, Cui L, Yin M, Yu Y, Zhou X, Wang H, et al. Hydrotherapy vs. conventional land-based exercise for improving walking and balance after stroke: a randomized controlled trial. Clin Rehabil 2016;30(6):587-93. doi: 10.1177/0269215515593392 [Crossref]
- Kim K, Lee DK, Kim EK. Effect of aquatic dual-task training on balance and gait in stroke patients. J Phys Ther Sci 2016;28(7):2044-7. doi: 10.1589/jpts.28.2044 [Crossref]
- Chan K, Phadke CP, Stremler D, Suter L, Pauley T, Ismail F, et al. The effect of water-based exercises on balance in persons post-stroke: a randomized controlled trial. Top Stroke Rehabil 2017;24(4):228-35. doi: 10.1080/10749357.2016.1251742 [Crossref]
- Downs S. The Berg Balance Scale. J Physiother 2014;2015;61(1):46. doi: 10.1016/j.jphys.2014.10.002 [Crossref]
- Pérez-de la Cruz S. Comparison between three therapeutic options for the treatment of balance and gait in stroke: a randomized controlled trial. Int J Environ Res Public Health 2021;18(2):426. doi: 10.3390/ijerph18020426 [Crossref]
- Cha H, Shin Y, Kim M. Effects of the Bad Ragaz Ring Method on muscle activation of the lower limbs and balance ability in chronic stroke: A randomized controlled trial. Hong Kong Physiother J 2017;37:39-45. doi: 10.1016/j.hkpj.2017.02.001 [Crossref]
- Chan PP, Si Tou JI, Tse MM, Ng SS. Reliability and validity of the Timed Up and Go Test with a motor task in people with chronic stroke. Arch Phys Med Rehabil 2017;98(11):2213-20. doi: 10.1016/j.apmr.2017.03.008 [Crossref]
- Saleh MSM, Rehab NI, Aly SMA. Effect of aquatic versus land motor dual
task training on balance and gait of patients with chronic stroke: A randomized
controlled trial. Neuro Rehabilitation 2019;44(4):485-92. doi: 10.3233/NRE-182636 [Crossref]
- Lim C. Effect of underwater treadmill gait training with water-jet resistance on balance and gait ability in patients with chronic stroke: a randomized controlled pilot trial. Front Neurol 2020;10:1246. doi: 10.3389/fneur.2019.01246 [Crossref]
- Noh DK, Lim J, Shin H, Paik N. The effect of aquatic therapy on postural balance and muscle strength in stroke survivors - a randomized controlled pilot trial. Clin Rehabil 2008;22(10-11):966-76. doi: 10.1177/0269215508091434 [Crossref]
- Montagna JC, Santos BC, Battistuzzo CR, Loureiro AP. Effects of
aquatic physiotherapy on the improvement of balance and corporal symmetry in
stroke survivors. Int J Clin Exp Med 2014 [Internet];7(4):1182-7. [cited 2022 aug 5]. Available from: https://pubmed.ncbi.nlm.nih.gov/24955206/
- Berger L, Klein C, Commandeur M. Évaluation des effets immédiats et à moyen terme de la mobilisation en eau chaude thermale sur l’équilibre statique et dynamique de sujets âgés. Annales de Réadaptation et de Médecine Physique 2008;51(2):84-9. doi: 10.1016/j.annrmp.2007.10.007 [Crossref]
- Veldema J, Jansen P. Aquatic therapy in stroke rehabilitation: systematic review and meta-analysis. Acta Neurol Scand 2021;143(3):221-41. doi: 10.1111/ane.13371 [Crossref]