Fisioter Bras. 2023;24:(5):647-60
ORIGINAL ARTICLE
Digital physical therapy intervention to treat female
urinary incontinence: a semi-experimental study
Intervenção
fisioterapêutica digital para o tratamento da incontinência urinária feminina:
um estudo semi-experimental
Marina Petter Rodrigues, Bárbara Soares Peterson, Suzana Mallmann, Luciana Laureano Paiva, José Geraldo Lopes Ramos
Universidade
Federal do Rio Grande do Sul, Porto Alegre, RS, Brasil
Received: 2023 April 19; accepted 2023 sept 26.
Correspondência: Marina Petter
Rodrigues, mpetterrodrigues@gmail.com
How to cite
Rodrigues MP, Peterson BS, Mallmann S, Paiva LL, Ramos JGL. Digital physical therapy intervention to treat female urinary incontinence: a semi-experimental study. Fisioter Bras. 2023;24(5):647-60. doi:
Abstract
Background: Urinary incontinence
affects 15-40% Brazilian women in rural areas, indicating the necessity of
treatment for people in remote regions. Digital technology could be an option,
but the evidence-based digital health intervention remains untapped. Objective:
To assess whether a group intervention by synchronous video call reduces the
severity of female urinary incontinence symptoms and to assess woman’s
perception on this modality. Methods: Incontinent women who had digital
access were invited to this semi-experimental study. An 8-week protocol was
conducted through video calls once a week. Lifestyle counseling and exercises
were performed. Pre- and post-evaluations were done exclusively by phone call. Results:
48 women were enrolled in the study and 40 concluded the protocol. They were
56.5 ± 12.0 years old and most of them had mixed urinary incontinence. The
impact on quality of life and the severity of urinary incontinence symptoms was
significantly improved and most of the participants were completely satisfied
with the intervention. A large effect size was observed (Glass’s delta = 0.83) Conclusion:
Our findings support a digital group approach for the treatment of female
urinary incontinence as an alternative to be further explored. Combining
digital service with group assistance brought satisfaction and clinical results
for the participants and it can be promising for public health services.
Resumo
Introdução: A incontinência urinária acomete entre
15-40% das mulheres que vivem em áreas rurais no Brasil, evidenciando a
necessidade de acesso a tratamentos adequados para indivíduos em regiões
remotas. Objetivo: Avaliar se uma estratégia fisioterapêutica realizada
em grupo e por vídeo-chamada síncrona pode reduzir a gravidade dos sintomas de
incontinência urinária feminina, além de analisar a percepção das mulheres
sobre essa modalidade. Métodos: Mulheres com queixa de incontinência
urinária e que tinham acesso a recursos digitais foram convidadas a participar
deste estudo semiexperimental. Um protocolo de 8
semanas foi conduzido através de videochamadas
realizadas uma vez por semana, que incluíam aconselhamento sobre estilo de vida
e treinamento dos músculos do assoalho pélvico. As avaliações pré e pós-tratamento foram realizadas exclusivamente por
chamada telefônica. Resultados: 48 mulheres foram incluídas no estudo e
40 delas concluíram o protocolo. A idade média das participantes foi de 56,5 ±
12,0 anos e a maioria apresentou sintomas de incontinência urinária mista.
Observou-se melhora significativa na qualidade de vida e na gravidade dos
sintomas, e a maioria das participantes ficou completamente satisfeita com a
intervenção. Além disso, um grande tamanho do efeito foi observado (delta de
Glass = 0,83). Conclusão: Os presentes resultados apoiam a abordagem
fisioterapêutica digital para o tratamento da incontinência urinária feminina
como uma alternativa promissora a ser explorada. A combinação de serviços
digitais com a assistência em grupo proporcionou satisfação e resultados
clínicos para as participantes, o que pode ser uma estratégia eficaz para o
tratamento dessa condição em serviços públicos de saúde.
Palavras-chave: incontinência urinária; treinamento
dos músculos do assoalho pélvico; telemonitoramento.
Introduction
Urinary incontinence (UI) is the
most common pelvic floor disorder (PFD) affecting approximately 26% of adult
female population in developing countries [1]. In Brazil, the prevalence is
also high [2,3,4,5,6], and studies have indicated that 15 to 40% of Brazilians in
rural areas suffer from UI [7,8,9]. This highlights the necessity for
establishing treatment resources targeting populations in remote regions,
within which telehealth emerges as a viable consideration.
Digital health practice has emerged
as a potential solution to overcome all restrictive measures that were
instituted during the Coronavirus Disease 2019 (COVID-19) pandemic [10]. Those
technologies were on the sideline of most health care services, but even before
the COVID-19 outbreak, the World Health Organization (WHO) had already talked
about a Global Strategy on Digital Health to promote wellbeing and health care
for everyone and everywhere [11]. Technology evolution has great potential to
accelerate human progress and to enhance health outcomes, but the promotion of
evidence-based digital health intervention remains largely untapped [11].
The International Continence
Society (ICS) recommends that initial treatment for women with UI should
include lifestyle education, bladder training and pelvic floor muscle training
(PFMT) for eight to 12 weeks [12]. In addition to being able to be taught
one-on-one, PFMT can also be practiced in groups as a lower cost alternative
[13,14,15,16]. Also, according to recent systematic reviews, it is possible to adapt
those intervention from a conventional face-to-face method to a digital basis
and also get improvement in urinary symptoms, in pelvic floor muscle (PFM)
function and on UI-related QoL [17,18].
Despite the promising results, the
strategies are quite heterogeneous ranging from traditional communication
methods such as phone calls, to more interactive and innovative approaches as
video calls and smartphone applications [17,19]. However, synchronous
supervision from the physiotherapist is not part of most of the protocols and
usually they are delivered on an individual basis [17,18,20]. Combining
supervised group care with digital practice could improve patients’
accessibility and optimize service and cost savings in the assistance field.
Therefore, the purpose of this
study was to assess whether a digital group physiotherapy intervention by
synchronous video call could be developed in a public hospital as a strategy to
reduce the severity of UI symptoms in females. Also, we aimed to evaluate the
participants' perception on this modality of treatment.
Methods
This was a semi-experimental study
following the TREND recommendations [21]. It was developed from December 2020
to April 2022, at Hospital de Clínicas de Porto
Alegre (HCPA), a public teaching hospital in southern Brazil. The study was
approved by the HCPA Ethics Committee (CAAE: 43638721.5.0000.5327 –
registration number 4.977.180) and followed the Circular Letter of the National
Commission for Research Ethics of the Ministry of Health about Guidelines for
virtual research (Carta Circular 1/2021-CONEP/SECNS/MS). Recommendations for
digital physiotherapy practices, provided by the Brazilian Federal Council of
Physical Therapy and Occupational Therapy (COFFITO) [22] and by the Brazilian
Association of Physical Therapy in Women's Health (ABRAFISM) [23,24], were
carefully followed. During the pandemic, digital interventions have been
supported by the COFFITO Resolution No 516 from March 2020.
Outcomes
The primary outcomes were the UI
symptoms severity and the impact on quality of life (QoL) evaluated by the
International Consultation on Incontinence Questionnaire Short Form (ICIQ-SF)
[25] and the secondary outcome was participants’ perception on the treatment
assessed through a custom survey.
Sample
In the mentioned period, patients
who underwent a gynecological appointment complaining of UI and who had
indication for conservative treatment were referred to pelvic floor physical
therapy by the HCPA Gynecology Outpatient Clinic team. Women were prescreened
by telephone to be informed about the intervention and to check for eligibility.
Inclusion criteria were females with UI, ≥ 18 years and who had digital
access to join a videocall weekly. Exclusion criteria were being in
physiotherapeutic treatment or have undergone a rehabilitation program in the
past 6 months. Medical records were checked to rule out conditions such as
pelvic organ prolapse ≥ grade 2, neurological diseases and abdominopelvic
surgery/childbirth in the past year.
A pilot study was developed with
eleven women to determine a proper sample to detect a four-point reduction in
the ICIQ-SF, suggested as a clinically significant improvement for women
undergoing non-surgical treatments for UI [26]. Those participants were not
included in the main study. Power and Sample Size for Health Researchers (PSS
Health) software - online version was used. Considering a power of 95%, a
significance level of 5%, and adding 30% for possible losses, the sample size
resulted in 20 participants.
Data collection
Participants received the Consent
Form on WhatsApp messaging app. They were instructed to read it carefully and
write back "I voluntarily agree to participate in this study", if
that was the case, to then be referred for the first evaluation. This method of
consent was defined by the HCPA Ethics Committee.
Then, they underwent a prescheduled
phone call to check for demographic data, UI symptoms and to answer the
ICIQ-SF, which is a three-scored questions questionnaire concerning frequency,
amount of leakage, and overall discomfort from 0-10. A fourth unscored question
helps in classifying the UI subtype. The score grades from 0 to 21, with higher
score indicating greater severity [25].
At the end of treatment, another
phone call was scheduled to reassess UI symptoms and to reapply the ICIQ-SF questionnaire.
Participants’ perception on the treatment was assessed through a 7-question’
custom satisfaction survey, adapted from Hui et al. [27], with answers
on a scale from 0 to 10. The answers were categorized into groups, as it is
shown in Table I.
Table I – Patients’ perception of
improvement
Phone calls were performed by a
student who was not involved in the videocalls so participants would feel
comfortable giving their opinion. All data collection was carried out
exclusively digitally due to the pandemic restrictions adopted at the time of
data collection.
Intervention
WhatsApp groups with no more than 5
participants (plus one physiotherapist) were organized. Groups were created to
enable a good communication between the participants and the researcher. Women
received a reminder 30 minutes before every meeting to encourage adherence to
treatment.
An 8-week digital group physical
therapy intervention was done once a week, in a 30-minute synchronous video
call, supervised by a physiotherapist with expertise in PFDs. All sessions
started with a conversation about lifestyle habits (around 20 minutes),
followed by exercises (around 10 minutes). A chatting space was stimulated, and
women were encouraged to share their experiences and ask questions. For
reference at home, all provided information was forwarded in digital files in
the end of each meeting, according to what was discussed. The intervention’
protocol is shown in Figure 1.
The exercise protocol was created
based on Ferreira et al. [28] recommendations, having breathing and
pelvic mobility exercises, PFMT and stretching exercises. Breathing exercises
were based on inhaling through the nose and exhaling through the mouth, with
awareness and concentration, in the lying, sitting, and standing posture.
Pelvic mobility had lateral legs’ movement in a lying position, pelvic
ante/retroversion in a sitting position and pelvic circumduction and lateral
mobility in a standing position. PFMT series consisted of slow and fast PFM
contractions in lying, sitting, and standing, and executing a bridge, a
sitting/standing exercise, and walking steps. Stretching of the spine and lower
limbs were also performed. As well as lifestyle orientations, the exercise
protocol was sent to the participants digitally.
To provide even better support,
YouTube videos were uploaded in the WhatsApp groups after the first, second and
last meeting. The first was about the PFM and its relationship to women’s
health, the second one was about basic PFMT exercises and the last one about
advanced PFMT. These videos were created by our research group, in a previous
study.
Analysis
Data were tabulated by the
double-key entry method and analyzed in IBM® SPSS® Statistics. Normality of the
data was defined by the Shapiro–Wilk test. Parametric quantitative data were
expressed as mean and standard deviation and nonparametric as median and
minimum and maximum. Comparisons was done through paired t tests and Wilcoxon
tests, according to the normality of the data. Categorical variables were
expressed as absolute and relative frequencies. The significance level was set
at 5% for all analyses. The effect size for the ICIQ final score was calculated
using Glass’s delta:
mean pre-mean post
SDpre
and common language effect size [29]. To evaluate the
participants’ perception about the treatment, a frequency analysis was
performed.
Results
One hundred and eleven women were
referred to the Pelvic Floor Physiotherapy service in the meantime. Of these,
23 did not answer our phone calls and two were not contacted because they had
only pelvic organ prolapse and no urine leakage. From the 86 participants who
were invited to participate in the study, 19 were excluded due to multiple
reasons and after undergoing the first assessment, only 48 were enrolled in the
intervention. Some women did not attend any session or withdrew along the
protocol, being 40 included in the final analysis. The CONSORT flow diagram is
shown in Figure 2.
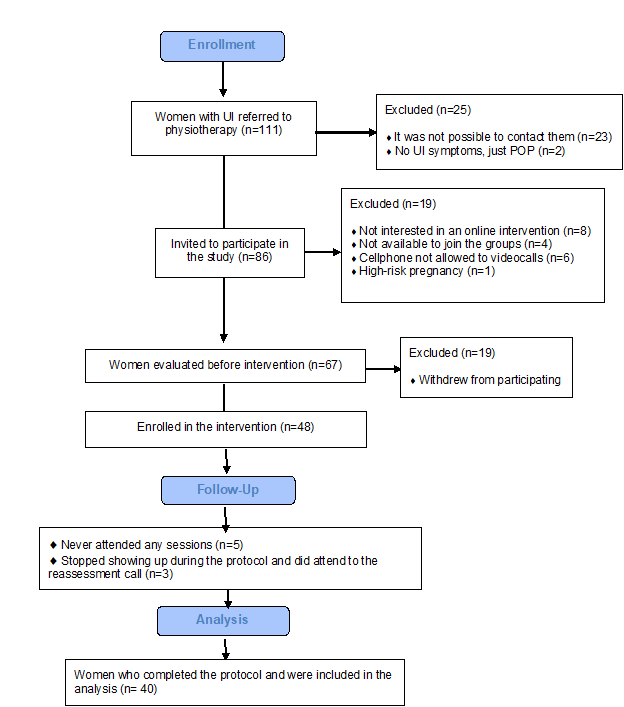
Figura 2 – Flowchart
The mean age was 56.5 ±12.0 years, the most prevalent subtype of UI was mixed UI (MUI) (57.5%) and there
was a wide range on the duration of symptoms (from 3 months to 30 years). More
than half of the sample did not live where the reference hospital of the study
was located (57.5%). The characterization of the sample is demonstrated on
Table II.
Tabela II – Characterization
of the sample
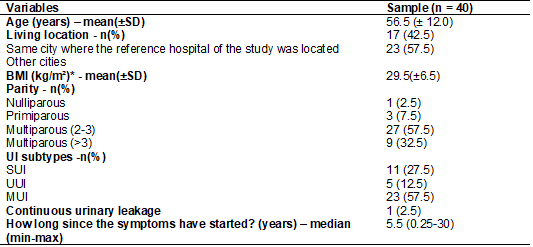
n = absolute frequency; SD =
standard deviation; BMI = body mass index; UI = urinary incontinence; SUI =
stress urinary incontinence; UUI = urgency urinary incontinence; MUI = mixed
urinary incontinence. Parametric and nonparametric quantitative variables are
presented as mean and standard deviation and median and minimum (min) and
maximum (max) values respectively. Categorical variables are presented as total
number and percentage. *Data available from 36 participants
The impact on QoL and the severity
of the UI were significantly improved after the intervention (Table III). These
two outcomes were evaluated by the ICIQ-SF third question and by the final
score, respectively. The ICIQ-SF final score dropped from 14.5 ± 3.0 (a severe
UI) [30] to 12.0 ± 5.0 (a moderate UI) [30]. Also, the effect size calculated
by the Glass’s delta formula was large for this variable (0.83) [31] and the
common language resulted in 72.2% probability of superiority with the treatment
[29], considering the ICIQ-SF final score.
Tabela III – Comparison
between pre and post intervention regarding the impact on quality of life and
the severity of UI symptoms
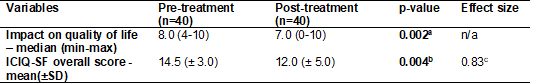
n = absolute frequency; ICIQ-SF =
International Consultation on Incontinence Questionnaire = Short Form.
Nonparametric quantitative variables are presented as median and minimum and
maximum values and the parametric quantitative variables in mean and standard
deviation. aWilcoxon test for quantitative
non-parametric variables. bPaired-t test for
quantitative parametric variables. cMeasure of effect
size calculated by Glass’s delta. Statistical significance was p ? 0.05 for the analyses. The overall score ranges from 0
to 21, with greater values indicating increased severity of UI symptoms. The impact on quality of life is assessed through question 5
of the questionnaire, with a score from 0 to 10 (greater values indicating
worst impact)
About participants’ perception on
the treatment, 65% were completely satisfied, 25% were satisfied and 80% would
strongly recommend the digital group for other people. The support materials
were considered very useful and most of them (62.5%) followed all behavioral
instructions exactly as recommended. The participants’ perception questionnaire
and the complete data are presented in Table I.
Discussion
Our findings support a digital
group physical therapy intervention as an alternative to reduce UI severity and
to improve QoL in women from a public health service. Self-reported
satisfaction on this modality was also high, suggesting an alternative to enhance
patients’ access and content to UI health care, corroborating previous studies
[20,27].
Digital strategies used on the
management of UI are diverse [17,18,32] but, to our knowledge, this is the
second study to propose a group video call intervention for UI and the first
one to propose it for women in a public hospital. A randomized clinical trial
comparing an 8-week intervention protocol through videoconferencing with
face-to-face sessions was published in 2006 [27], showing a reduction in the number
of daily incontinence episodes and improvement in PFM strength in both groups.
A face-to-face first assessment was done, affording necessary guidance for the
participants on PFM awareness. However, it was a completely different global
health context, and the protocols were conducted by nurses and not by
physiotherapists.
Our study was conducted in a period
when vaccination wasn’t fully widespread and the recommendations for social
distancing were strong [33]. Proposing a remote service was an alternative to
meet the waiting lists but performing it in a group was also a way to encourage
socialization. Besides the social isolation context, a group intervention
collaborates with the environment for learning by allowing real time
interaction between patients and health-care professionals [27] and it has a
significant difference in mean cost comparing to an individual treatment [14].
Paiva et al. [13]
demonstrated in their metanalysis no difference when comparing PFMT in groups
vs individual PFMT intervention. When comparing PFMT in groups vs PFMT at home,
the group intervention was more efficient, probably due to physiotherapeutic
supervision [15,34]. Poor patient compliance has been investigated in PFDs and
assumptions converge with our thoughts regarding the lack of ongoing support
[35]. Poor motivation, forgetting to perform the exercises, disinformation on
PFM and UI were identified as impact factors [35,36]. Supervised and shared
treatment with other people can be a motivating factor and we do consider that
the practices chosen in our protocol comprise a good part of these points.
PFMT has grade A recommendation by
ICS, but beyond it, lifestyle interventions and bladder training are also
highly recommended [12]. We made a strong use of these approaches proposing an
even more complete assistance. Given the time that physiotherapists spend
weekly with the patients, they contribute to patient's comprehension on
behavioral practices. The same strategy was adopted by Santiago et al.
[20] and a good adherence to behavioral measures and changes in the
participants' lifestyle was seen.
As access to pelvic floor
physiotherapists is not a reality everywhere, a digital program can be an
alternative to manage UI in remote areas. In our study, more than half of the
sample (57.5%) did not live in the same city where the reference hospital was
located. The literature also provides data on high prevalence of UI in rural
areas of Brazil [7,8,9]. To attend face-to-face appointments, these patients would
have costs regarding transport and other expenses related to the time away from
home, such as food. This approach may contribute to the choice of a low-cost
intervention, especially in referral hospitals where patients from other
locations are admitted.
Another interesting way of using
digital health strategies in this context is the hybrid-telerehabilitation
intervention proposed by Santiago et al. [20]. A randomized controlled
trial was performed comparing a 12-week hybrid program versus a conventional
face-to-face one. UI-related quality of life and UI severity significantly
improved in both groups, highlighting the potential and diverse use of digital
intervention in health care. A hybrid service can improve accessibility,
without giving up on face-to-face appointments when necessary.
Some limitations in our study
warrant mention. The design did not present a control group and a randomized
sample. This small sample reflects the pandemic period when few elective
appointments were being performed. Since face-to-face appointments were not
allowed, a proper physical evaluation to check for pelvic floor awareness, and
objective methods to quantify the severity of urine leakage, like a pad test,
were missed.
However, despite the limitations, a
digital physical therapy intervention to treat UI has been developed and we aim
to keep studying it to ensure a more affordable form of treatment for women in
the Unified Health System in Brazil. In 2020, 52.000 teleconsultations in
different areas were performed at our hospital, increasing almost 30% in 2021
[37]. An important health strategy has emerged and can no longer be left
behind, though further investigation is still required.
Conclusion
Our findings support a digital
group physical therapy intervention for the treatment of female UI as an
alternative to be further explored. UI affects thousands of women around the
world and PFMT has strong evidence for UI treatment, so distance should not be
a limiting factor.
Combining digital service
accessibility with group assistance brought satisfaction and good clinical
results for the participants, but it can also be promising for public health
services as it does not require much physical space and absorbs greater demand
in a shorter time. The COVID-19 pandemic has given a significant boost to the
use of digital health, and more robust data through rigorous methods are
necessary to consolidate these practices beyond the pandemic.
Conflicts of interest
The authors report no competing
interests to declare.
Funding
This work was supported by
Coordination for the Improvement of Higher Education Personnel (CAPES).
Authors’ contribution
Research conception and design:
Rodrigues MP, Paiva LL, Ramos JGL; Data collection: Rodrigues MP, Peterson BS;
Data analysis and interpretation: Rodrigues MP, Mallmann
S; Statistical analysis: Rodrigues MP, Mallmann S;
Writing of the manuscript: Rodrigues MP, Mallmann S;
Critical review of the manuscript for important intellectual content: Paiva LL,
Ramos JGL.
References
- Mostafaei H, Sadeghi?Bazargani
H, Hajebrahimi S, Salehi?Pourmehr
H, Ghojazadeh M, Onur R, et
al. Prevalence of female urinary incontinence in the developing world: A
systematic review and meta?analysis—A Report from the
Developing World Committee of the International Continence Society and Iranian
Research Center for Evidence Based Medicine. Neurourol Urodyn
[Internet]. 2020 Apr 3;39(4):1063–86. Available from:
https://onlinelibrary.wiley.com/doi/10.1002/nau.24342
- Guedes
TSR, Guedes MBOG, de Oliveira HKM, Soares RL, da Cunha VL, Lopes JM, et al. Urinary
Incontinence in Physically Active Older Women of Northeast Brazil. Int J
Environ Res Public Health [Internet]. 2021 May 30;18(11):5878. Available from:
https://www.mdpi.com/1660-4601/18/11/5878
- Ting HY, Cesar JA. Urinary incontinence among pregnant
women in Southern Brazil: A population-based cross-sectional survey. Spradley
FT, editor. PLoS One [Internet]. 2020 Jun 8;15(6):e0234338. Available from:
https://dx.plos.org/10.1371/journal.pone.0234338
- Oriá
MOB, Mitchell EM, Vasconcelos CTM, de Oliveira TDA, Lopes LG, de Menezes PR, et
al. Prevalence of lower urinary tract symptoms and social determinants in
primary care users in Brazil. Int
Urogynecol J [Internet]. 2018 Dec
24;29(12):1825–32. Available from:
http://link.springer.com/10.1007/s00192-018-3635-1
- Magnani
PS, Bettiol H, da Silva AAM, Barbieri MA, de Carvalho
Cavalli R, Brito LGO. Urinary incontinence between 12 and 24 months
postpartum: a cross-sectional study nested in a Brazilian cohort from two
cities with different socioeconomic characteristics. Int Urogynecol J [Internet]. 2019 Jun 26;30(6):1003–11. Available from: http://link.springer.com/10.1007/s00192-019-03907-y
- Paiva
LL, Rodrigues MP, Bessel T. Prevalência de incontinência urinária em idosos no
brasil nos últimos 10 anos: uma revisão sistemática. Estud
Interdiscip sobre o Envelhec
[Internet]. 2019 Oct 28;24. Available
from:
https://seer.ufrgs.br/RevEnvelhecer/article/view/97762
- Weschenfelder AJ, Strelow
C, de Arruda GT, Froelich MA, Foletto
Pivetta HM, Braz M. Prevalência de incontinência
urinária e seu impacto sobre a qualidade de vida de idosos: estudo comparativo
entre meio urbano e meio rural. Rev Kairos Gerontol.
2016;19(3):67–77.
- Dziekaniak AC, Meucci
RD, Cesar JA. Incontinência urinária entre idosos residentes em área rural de
município do sul do Brasil. Geriatr Gerontol Aging [Internet]. 2019 Mar;13(1):4–10. Available
from:
http://www.ggaging.com/details/508/pt-BR/incontinencia-urinaria-entre-idosos-residentes-em-area-rural-de-municipio-do-sul-do-brasil
- Tavares
DMS, Santos LL, Dias FA, Pollyana, Ferreira C dos S,
Feliciano EA de O, et al. Comparação das características sociodemográficas de
saúde e qualidade de vida de idosos rurais segundo sexo. Rev
Enferm e Atenção à Saúde. 2013;2(1):32–46.
- Smith
AC, Thomas E, Snoswell CL, Haydon
H, Mehrotra A, Clemensen J,
et al. Telehealth for global emergencies: Implications for
coronavirus disease 2019 (COVID-19). J Telemed
Telecare [Internet]. 2020 Jun 20;26(5):309–13. doi: 10.1177/1357633X20916567 [Crossref]
- Organization WH. Global Strategy on Digital Health
2020-2025. Geneva World Heal Organ. 2021;
- Abrams P, Andersson K-E, Apostolidis A, Birder L, Bliss D, Brubaker L, et al. 6th International Consultation on Incontinence. Recommendations of the International Scientific Committee: Evaluation and treatment of urinary incontinence, pelvic organ prolapse and faecal incontinence. Neurourol Urodyn [Internet]. 2018 Sep;37(7):2271–2. doi: 10.1002/nau.23551 [Crossref]
- Paiva LL, Ferla L, Darski C, Catarino BM, Ramos JGL. Pelvic floor muscle training in groups versus individual or home treatment of women with urinary incontinence: systematic review and meta-analysis. Int Urogynecol J [Internet]. 2017 Mar 9;28(3):351–9. doi: 10.1007/s00192-016-3133-2 [Crossref]
- Lamb S, Pepper J, Lall R, Jørstad-Stein E, Clark M, Hill L, et al. Group treatments
for sensitive health care problems: a randomised
controlled trial of group versus individual physiotherapy sessions for female
urinary incontinence. BMC Womens Health [Internet].
2009 Dec 14;9(1):26. Available from:
https://bmcwomenshealth.biomedcentral.com/articles/10.1186/1472-6874-9-26
- Figueiredo VB,
Nascimento SL, Martínez RFL, Lima CTS, Ferreira CHJ, Driusso
P. Effects of individual pelvic floor muscle training vs individual training
progressing to group training vs group training alone in women with stress
urinary incontinence: A randomized clinical trial. Neurourol
Urodyn [Internet]. 2020 Jun 30;39(5):1447–55.
Available from: https://onlinelibrary.wiley.com/doi/10.1002/nau.24370
- Brennen R, Frawley HC, Martin J, Haines TP.
Group-based pelvic floor muscle training for all women during pregnancy is more
cost-effective than postnatal training for women with urinary incontinence:
cost-effectiveness analysis of a systematic review. J Physiother
[Internet]. 2021 Apr;67(2):105–14. Available from:
https://linkinghub.elsevier.com/retrieve/pii/S1836955321000217
- da Mata KRU, Costa RCM, Carbone É dos SM, Gimenez MM, Bortolini MAT, Castro RA, et al. Telehealth in the
rehabilitation of female pelvic floor dysfunction: a systematic literature
review. Int Urogynecol J [Internet]. 2021 Feb
11;32(2):249–59. Available from:
http://link.springer.com/10.1007/s00192-020-04588-8
- Huang Z, Wu S, Yu T, Hu A. Efficacy of telemedicine
for urinary incontinence in women: a systematic review and meta-analysis of
randomized controlled trials. Int Urogynecol J
[Internet]. 2020 Aug 31;31(8):1507–13. Available from:
https://link.springer.com/10.1007/s00192-020-04340-2
- Bernard S, McLean L, Boucher S, Hébert LJ, Plante M,
Grégoire J, et al. An in-home rehabilitation program for the treatment of
urinary incontinence symptoms in endometrial cancer survivors: a single-case
experimental design study. Int Urogynecol J
[Internet]. 2021 Nov 25;32(11):2947–57. Available from: https://link.springer.com/10.1007/s00192-021-04981-x
- Santiago M, Cardoso-Teixeira P, Pereira S, Firmino-Machado J, Moreira S. A Hybrid-Telerehabilitation
Versus a Conventional Program for Urinary Incontinence: a
Randomized Trial during COVID-19 Pandemic. Int Urogynecol
J [Internet]. 2022 May 21; Available from:
https://link.springer.com/10.1007/s00192-022-05108-6
- Des Jarlais DC, Lyles C, Crepaz N. Improving the Reporting Quality of Nonrandomized
Evaluations of Behavioral and Public Health Interventions: The TREND Statement.
Am J Public Health [Internet]. 2004 Mar;94(3):361–6. Available from:
http://ajph.aphapublications.org/doi/10.2105/AJPH.94.3.361
- COFFITO.
Teleconsulta, Telemonitoramento
e teleconsultoria. Resolução N 516, 20 março 2020.
- Associação
Brasileira de Fisioterapia em Saúde da Mulher. Recomendações da Abrafism sobre fisioterapia em uroginecologia
e coloproctologia em tempos de COVID-19. 2020.
- Associação
Brasileira de Fisioterapia em Saúde da Mulher. Recomendação geral Abrafism fisioterapia por meio digital/teleconsulta
e telemonitoramento na fisioterapia em saúde da
mulher e uro-proctologia. 2020.
- Tamanini JTN, Dambros
M, D’Ancona CAL, Palma PCR, Rodrigues Netto Jr N. Validação para o português do
“International Consultation
on Incontinence Questionnaire - Short Form”
(ICIQ-SF). Rev Saude
Publica [Internet]. 2004 Jun;38(3):438–44. Available from:
http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0034-89102004000300015&lng=pt&tlng=pt
- Lim R, Liong ML, Lim KK,
Leong WS, Yuen KH. The Minimum Clinically Important Difference of the
International Consultation on Incontinence Questionnaires (ICIQ-UI SF and ICIQ-LUTSqol). Urology [Internet]. 2019 Nov;133:91–5.
Available from: https://linkinghub.elsevier.com/retrieve/pii/S0090429519307125
- Hui E, Lee PSC, Woo J. Management of urinary
incontinence in older women using videoconferencing versus conventional
management: a randomized controlled trial. J Telemed
Telecare [Internet]. 2006 Oct 1;12(7):343–7. Available from:
http://journals.sagepub.com/doi/10.1258/135763306778682413
- Ferreira
CHJ, Driusso P, Haddad JM, Pereira SB, Fernandes
ACNL, Porto D, et al. A guide to physiotherapy in urogynecology for patient
care during the COVID-19 pandemic. Int Urogynecol J
[Internet]. 2021 Jan 28;32(1):203–10. Available from: https://link.springer.com/10.1007/s00192-020-04542-8
- Lakens D.
Calculating and reporting effect sizes to facilitate cumulative science: a
practical primer for t-tests and ANOVAs. Front Psychol [Internet]. 2013;4.
Available from: http://journal.frontiersin.org/article/10.3389/fpsyg.2013.00863/abstract
- Klovning A,
Avery K, Sandvik H, Hunskaar S. Comparison of two
questionnaires for assessing the severity of urinary incontinence: The ICIQ-UI
SF versus the incontinence severity index. Neurourol Urodyn [Internet]. 2009 Jun;28(5):411–5. Available from:
https://onlinelibrary.wiley.com/doi/10.1002/nau.20674
- Sawilowsky SS.
New Effect Size Rules of Thumb. J Mod Appl Stat Methods [Internet]. 2009 Nov
1;8(2):597–9. Available from: http://digitalcommons.wayne.edu/jmasm/vol8/iss2/26
- Bernard S, Boucher S, McLean L, Moffet
H. Mobile technologies for the conservative self-management of urinary
incontinence: a systematic scoping review. Int Urogynecol J [Internet]. 2020 Jun 2;31(6):1163–74. Available from: http://link.springer.com/10.1007/s00192-019-04012-w
- Aquino
EML, Silveira IH, Pescarini JM, Aquino R, Souza-Filho
JA de, Rocha A dos S, et al. Medidas de distanciamento social no controle da
pandemia de COVID-19: potenciais impactos e desafios no Brasil. Cienc Saude
Colet [Internet]. 2020 Jun;25(suppl 1):2423–46. Available from:
http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1413-81232020006702423&tlng=pt
- Hay-Smith EJC, Herderschee
R, Dumoulin C, Herbison GP. Comparisons of approaches
to pelvic floor muscle training for urinary incontinence in women. Cochrane
Database Syst Rev [Internet]. 2011 Dec 7; Available from:
https://doi.wiley.com/10.1002/14651858.CD009508
- Paquette J, McDermott CD, Acquaviva
B, Faghani N, Lovatsis D.
Real-world effectiveness of pelvic floor muscle training for women with urinary
tract symptoms and/or prolapse. J Obstet Gynaecol Canada [Internet]. 2021 Nov;43(11):1247-1253.e1.
Available from: https://linkinghub.elsevier.com/retrieve/pii/S1701216321004163
- Frawley HC, McClurg D, Mahfooza
A, Hay-Smith J, Dumoulin C. Health professionals’ and patients’ perspectives on
pelvic floor muscle training adherence- 2011 ICS State-of-the-Science Seminar
research paper IV of IV. Neurourol
Urodyn [Internet]. 2015 Sep;34(7):632–9. Available from:
https://onlinelibrary.wiley.com/doi/10.1002/nau.22774
- HCPA. Produção assistencial HCPA [Internet]. [cited 2022 Nov 10]. Available from: https://www.hcpa.edu.br/institucional/institucional-apresentacao/institucional-apresentacao-principais-numeros