Fisioter Bras. 2023;24:(5):718-28
REVISÃO
Effects of ozone therapy on joint rehabilitation in
patients with osteoarthritis: a systematic review
Efeitos
da ozonioterapia na reabilitação articular de
pacientes com osteoartrite: uma revisão sistemática
Priscilla
Abreu Barbosa, Lays Brito Dias de Araújo, André Luiz
Lisboa Cordeiro
1Unidade de Ensino Superior de Feira de
Santana, Feira de Santana, Bahia, Brasil
Received 2023 may 1th; accepted 2023 sept 20
Correspondence: André Luiz Lisboa Cordeiro, andrelisboacordeiro@gmail.com
How to cite
Barbosa PA, Araújo LBD, Cordeiro ALL. Effects of ozone therapy on joint rehabilitation in patients with osteoarthritis: a systematic review. Fisioter Bras. 2023;24(5):718-28. doi: 10.33233/fb.v24i5.5469
Abstract
Introduction: Osteoarthritis
is a comorbidity of chronic and multifactorial pain, characterized by a
degenerative joint process that compromises functionality. Ozone therapy has
proven to be a good rehabilitation strategy in view of its regenerative and
antioxidant effects. Objective: To describe the effects of ozone therapy
on tissue recovery, with regard to pain and functionality, impacting the joint
rehabilitation of patients with osteoarthritis. Methods: Refers to a
systematic review guided by the PICO strategy, the search was performed in the
Lilacs, Pubmed, and CENTRAL databases, with the
descriptors: osteoarthritis, degenerative arthritis, cartilage, damaged
cartilage, arthritis, joint, ozone, ozone therapy, ozone therapy, ozone
injection, pain, arthralgia, chronic pain, joint pain, mobility, mobility
limitation, range of motion and functionality, using the Boolean operators
"AND" and "OR", including articles from 2016 to 2021. Results:
After reading the title and abstract, 40 studies were found, 5 were selected
according to the inclusion criteria, which showed that ozone therapy is
effective in joint rehabilitation for pain and functionality markers. However,
with differences in duration of effects when compared to other therapies, being
more effective in the short term. Conclusion: Ozone therapy is effective
in reducing pain and inflammation, and in functional improvement, directly
impacting the joint rehabilitation of patients with osteoarthritis.
Keywords: ozone; cartilage;
articulation; inflammation.
Resumo
Introdução: A osteoartrite é uma comorbidade de
dor crônica e multifatorial, caracterizada por um processo articular
degenerativo que compromete a funcionalidade. A ozonioterapia
tem provado ser uma boa estratégia de reabilitação tendo em conta os seus
efeitos regenerativos e antioxidantes. Objetivo: Descrever os efeitos da
ozonioterapia na recuperação tecidual, no que diz
respeito à dor e funcionalidade, impactando na reabilitação articular de
pacientes com osteoartrite. Métodos: Revisão sistemática orientada pela
estratégia PICO; a busca foi realizada nas bases de dados Lilacs,
Pubmed e Central, com os descritores: osteoartrite,
artrite degenerativa, cartilagem, cartilagem danificada, artrite, articulação,
ozônio, terapia de ozônio, ozonioterapia, injeção de
ozônio, dor, artralgia, dor crônica, dor articular, mobilidade, limitação de
mobilidade, amplitude de movimento e funcionalidade, utilizando os operadores
booleanos “AND” e “OR”, incluindo artigos de 2016 a 2021. Resultados:
Após leitura do título e resumo, foram encontrados 40 estudos, e 5 foram
selecionados de acordo com os critérios de inclusão, que mostraram que a ozonioterapia é eficaz na reabilitação articular para
marcadores de dor e funcionalidade. Porém, com diferenças na duração dos
efeitos quando comparado a outras terapias, sendo mais eficaz em curto prazo. Conclusão:
A ozonioterapia é eficaz na redução da dor e
inflamação, e na melhora funcional, impactando diretamente na reabilitação
articular de pacientes com osteoartrite.
Palavras-chave: ozônio; cartilagem; articulação;
inflamação.
Introduction
Osteoarthritis (OA) is
characterized by a degenerative process of the joint, with morphological
changes, especially in cartilage, generating joint incongruence, reducing
functionality, impacting the quality of life and mental health of the
individual. In this context, ozone therapy has been consolidating its
regenerative effectiveness, thus favoring mobility, biomechanics, and joint
functionality [1,2].
This pathology is considered
chronic and multifactorial, of non-genetic character, not linked to aging and
gender, but a higher percentage in women and the elderly stands out. It is the
most common cause of disability and affects up to 15% of the population over
60. According to the United Nations (2004), by the year 2050 this figure will
increase to 20%, that is, 130 million people will be affected [3,4].
Osteoarthritis is a chronic pain
comorbidity that can affect any joint, however, with greater incidence in hips,
knees, hands, feet and spine. Through which, the inflammatory process in the
synovial fluid causes deterioration of the cartilage and adjacent structures,
such as muscles, tendons, and ligaments, causing bone deformities, pain, edema,
stiffness, and loss of function [5].
Ozone therapy promotes the
synthesis of antioxidant enzymes, inhibits the action of pro-inflammatory
cytokines, and stimulates anabolism. These processes favor angiogenesis and
stimulation of cells that are directly linked to the maintenance of the matrix
and healing of connective tissue. Thus, enabling an effective action on the
symptoms and repair of tissues degenerated by osteoarthritis [6].
The use of
ozone as a therapy is still recent; the time of discovery of its
pharmacodynamics in human blood is less than half a century. For this reason,
the number of studies discussing the effects of ozone therapy on
musculoskeletal disorders is, in fact, small. Thus, the present study aims to
describe the effects of ozone therapy on tissue recovery, with regard to pain
and functionality, impacting the joint rehabilitation of patients with OA.
Methods
Study design
This systematic review was
completed in accordance with the Preferred Reporting Items for Systematic
Reviews and Meta-Analyses (PRISMA) guidelines [7].
Eligibility criteria
To perform this systematic review,
the PICO strategy was used, whose Population was patients affected by
osteoarthritis, having ozone therapy as Intervention. The control group were
patients who received placebo treatment, conservative physical therapy, or other
invasive interventions. In the endpoints, the search was related to pain and
functionality.
Information sources
The search for articles was
conducted in the Latin American and Caribbean Literature on Health Sciences
(LILACS), Pubmed, and Cochrane Central Register of
Systematic Review (CENTRAL) databases. Reference lists of previous systematic
reviews and of the clinical trials eligible for this review were also searched.
The search for articles ended in September 2021.
Search
The search was based on the
previously described PICO strategy and the Boolean operators AND and OR. The keywords were extracted from the Health
Sciences Descriptors (Decs), and for the population:
osteoarthritis, degenerative atritis, cartilage,
damaged cartilage, arthritis, and joint. As for the intervention: ozone, ozone
therapy, ozone therapy, ozone injection. The results were: pain, arthralgia,
chronic pain, joint pain, mobility, mobility limitation, range of motion, and
functionality. Randomized clinical trials, clinical trials and controlled
trials were used as descriptors for the study design.
Study Selection
Randomized clinical trials from the
last 5 years, in English, Portuguese and Spanish, involving patients with
osteoarthritis were included in this systematic review. To be eligible, the
clinical trial had to have assigned patients with osteoarthritis to an ozone
therapy treatment group. Studies with adults (18 years and older), regardless
of gender, were also included. Ozone therapy refers to the medicinal use of the
triatomic oxygen molecule, produced from a medical generator, for the treatment
of various conditions. It is possible by several routes of administration, such
as intra-articular, periarticular, subcutaneous, rectal, venous, auricular, and
vaginal. And as exclusion criteria were listed studies that involved tests on
animals and related to the use of drugs.
Data collection process
For the extraction of the selected
articles, titles (first step), abstracts (second step), and complete reading
(third step) were checked. Then, an exploratory reading of the selected studies
was performed, followed by a selective and analytical reading. The data
extracted from the articles were summarized in authors, year, title,
population, gender, mean age, sample size, type of interventions, number of
sessions, O3 concentration used, diagnostic method, follow-up, and
scales used to obtain important information for the research.
Data Items
Two authors independently extracted
the data from the published reports using standard data extraction considering:
(1) aspects of the study population, such as mean age, gender, number of
patients, method of diagnosis; (2) aspects of the intervention performed
(sample size, type of intervention, number of sessions, O3
concentration used); (3) follow-up; (4) variables analyzed; and (5); scales
used.
Quality of studies
The methodological quality was
evaluated according to the criteria of the PEDro
scale, which scores 11 items, namely: 1 - Eligibility criteria, 2 - Random
allocation, 3 - Hidden allocation, 4 - Baseline comparison, 5 - Blinded, 6 -
Blinded therapists, 7 - Blinded assessors, 8 - Adequate follow-up, 9 -
Intention to treat analysis, 10 - Inter-group comparisons, 11 - Point estimates
and variability. Items are scored as present (1) or absent (0), generating a
maximum sum of 10 points, not counting the first item8.
Where possible, PEDro
scores were extracted from its own database. When articles were not found in
the database, a trained independent reviewer evaluated the article with the PEDro scale. Studies were considered of high quality if
they scored 8, and excellent quality if they scored 9 to 10.
Results
Forty articles were excluded after
reading the titles and abstracts. Eight articles were selected, three of which
succeeded to exclusion because they were related to the use of medications,
thus remaining five studies by the inclusion criteria. The flowchart in figure
1 shows the criteria and databases used to select the articles.
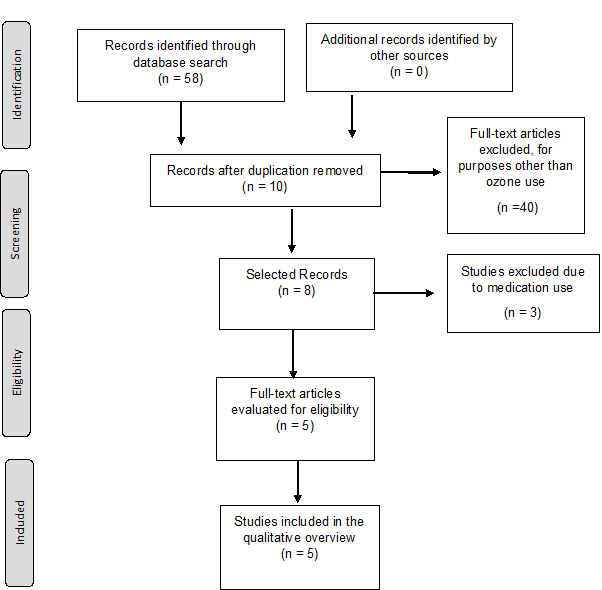
Figure 1 - Flow chart for obtaining
randomized clinical trials based on the effects of ozone therapy in patients
with osteoarthritis
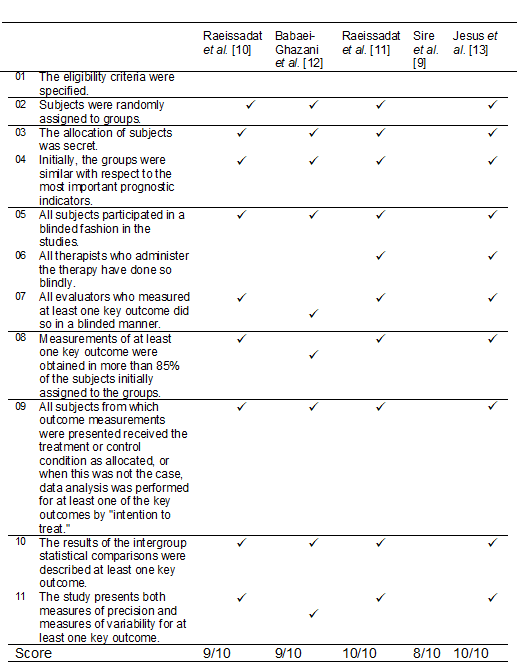
The methodological quality evaluated by the Pedro
scale is shown in Table I. Being that the 5 studies included in this systematic
review discuss the effects of ozone therapy on patients with osteoarthritis.
Only the study by Sire et al. [9] showed good methodological quality
while the studies by Raeissadat et al.
[10,11], Babaei-Ghazani et al. [12] and Jesus et
al. [13] were rated at excellent methodological quality.
Table I - Methodological quality
assessment of the studies included in this review, using the Pedro database
scale
The summary of the methods used and clinical results
are presented in Table II. The scales used to evaluate functionality were the
Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Lequesne Index (LEQ), Oxford Knee Questionnaire (OKQ),
Timed up and go (TUG) and Physical Component Summary (PCS). Those that evaluate
pain are the Visual Analog Pain Scale (VAS) and the Geriatric Pain Measurement
(GPM).
Table II - General data from the
randomized clinical trials included, looking for the effects of ozone therapy
in patients with osteoarthritis
Discussion
The results obtained in the studies
prove the effectiveness of ozone use for joint rehabilitation, since its
efficacy is statistically significant for pain and function markers. However,
they show differences in the duration of the effects when compared to other
therapies, being more effective in short protocols of up to 6 months.
The authors, Jesus et al. [13],
Sire et al. [9], Raeissadat et al. [11], Babaei-Ghazani et al.
[12] highlight the degeneration factor as the key point in joint
destruction, which generates a range of symptoms that have the consequence of
disabling the individual, leading to joint incongruity, causing pain, absence
of function and decreased quality of life.
In this context, it is believed
that ozone therapy is effective in tissue recovery by promoting moderate
oxidative stress, being a vehicle for endogenous immune responses, with reduction
of pro-inflammatory cytokines and activation of regeneration factors. Thus, it
becomes a hope for treatment, besides the low cost, and it can be more
accessible to the population, besides making it less costly for the country.
The pain in osteoarthritis is one
of the main symptoms experienced by patients affected, since the degeneration
is part of a multifactorial inflammatory process, which leads to the
destruction of the articular cellular matrix. This triggers a series of
problems that accompany the entire process, and increases as the pathology
evolves. It is worth pointing out that pain and function are directly related,
for the individual with joint pain necessarily has a deficit in function.
Functionality, on the other hand,
reflects the biomechanical alignment and joint fluency, which allows stable
synergic movements, keeping the individual active throughout life. However, in
OA, due to the chronic inflammatory process of the joint structures, especially
the cartilage, there is formation of osteophytes and deformities, compromising
functionality as a result of incongruity.
Following this reasoning, Raeissadat et al. [10] prove the effectiveness and
safety of O3 and HA in pain management and functionality. Although
both techniques were effective in relieving symptoms, O3 was
slightly better in the context of pain and stiffness, and HA in the aspect of
functionality, but without statistical relevance in the results. Thus, the
authors suggest ozone therapy over HA, due to the primary cost-benefit factor.
It is known that ozone therapy is
still relatively recent, but it is already used in several painful conditions,
as well as in other pathologies, and according to the suggestion of Raeissadat et al. [10] regarding cost-benefit,
currently the market values of the two therapies oscillate, with the
application of O3 being around one third of HA. In fact, ozone
therapy is a better option, allowing a larger fraction of the population to
have access to a promising treatment for OA.
Similarly, Sire et al. [9],
6 months after intra-articular application, found that ozone and HA are
effective therapies for pain relief. However, they show that in the short term,
that is, within one-month, hyaluronic acid is more effective for this symptom.
These results may be explained by the absence of a description of the HA
concentration in the protocol proposed in this study.
On an opposing side, Raeissadat et al. [11] and Jesus et al. [13]
converge their results to the same reasoning, that O3 is more
effective in the short term, around two months regarding pain, function and
stiffness. Possibly, the blockade of pro-inflammatory cytokines has a direct
action in reducing pain and consequently improving function.
This condition is explained by the
ozone action mechanism, since it has the potential to paralyze the inflammatory
process, as well as activating growth factors, in addition to greater
vascularization and local O2 supply. These events trigger an
endogenous response from the immune system, which receives the stimulus for the
production of antioxidants, which happens quickly, due to the high solubility
and short half-life of this gas.
The results found in the studies by
Raeissadat et al. [11] and Babaei-Ghazani
et al. [12], support the theory that the effects of ozone may only
persist for up to 6 months. For up to three months after applications, Babei-Ghazani et al. [12] elucidated the superiority
of ozone in improving pain and functionality when compared to corticosteroid therapy.
Raeissadat et al. [11], on the other hand,
found that the effects of ozone begin to decline after 6 months and at 12
months it is not effective in tissue repair or analgesia.
Throughout the development of the
present research, some limitations were experienced, in particular the lack of
articles aligned with the search and screening plan. However, they did not
affect the results, since the guidelines and methods defined in this systematic
review allowed the work to be carried out without generating negative impact,
emphasizing in this sense, the high methodological quality of the studies
addressed.
Conclusion
Based on the results it is possible
to conclude that ozone therapy is a powerful tool for the treatment of
osteoarthritis. However, despite being an approved complementary therapy, new
studies are still needed, with greater robustness, especially in the percentage
of samples, treatment time, dosages, number and interval of applications, as
well as the ideal stage of the pathology for intervention with ozone. Thus, it
could become accessible to the entire population in a safe and effective way,
aligning the cost-benefit of the treatment with the rehabilitation itself, with
regard to the return of joint functionality and, consequently, the individual's
physical and emotional well-being.
Conflitos
de interesse
Sem
conflito de interesse
Fontes
de financiamento
Sem
financiamento
Contribuição
dos autores
Concepção
e desenho da pesquisa:
Barbosa PA, Araújo LBD, Cordeiro ALL; Coleta de dados: Barbosa PA,
Araújo LBD, Cordeiro ALL; Análise e interpretação dos dados: Cordeiro
ALL; Análise estatística: Cordeiro ALL; Redação do manuscrito:
Barbosa PA, Araújo LBD, Cordeiro ALL; Revisão crítica do manuscrito quanto
ao conteúdo intelectual importante: Barbosa PA, Araújo LBD, Cordeiro
ALL
References
- Anzolin AP, Bertol CD. Ozone therapy as an integrating therapeutic in osteoartrosis treatment: a systematic review. Br J Pain. 2018;1(2):171-5.
- Costa T,
Rodrigues-Manica S, Lopes C, Gomes J, Marona J,
Falcão S, Branco J. Ozonoterapia na osteoartrose do
joelho: revisão sistemática. Acta Med Port. 2018 Oct 31;31(10):576-80. doi: 10.20344/amp.10330 [Crossref]
- Ocampo PE, Vallejo VH, Canavese
Rahal S. Cartilagem articular, patogênese e tratamento da osteoartrite. RVZ
[Internet]. 2019 [citado 16 de janeiro de 2023];26:1-12. Disponível em: https://rvz.emnuvens.com.br/rvz/article/view/425
- Vina ER, Kwoh CK.
Epidemiology of osteoarthritis: literature update. Curr
Opin Rheumatol. 2018
Mar;30(2):160-67. doi: 10.1097/BOR.0000000000000479 [Crossref]
- Noori-Zadeh A, Bakhtiyari S, Khooz R, Haghani K, Darabi S. Intra-articular ozone therapy efficiently attenuates pain in knee osteoarthritic subjects: A systematic review and meta-analysis. Complement Ther Med. 2019 Feb;42:240-47. doi: 10.1016/j.ctim.2018.11.023 [Crossref]
- Seyam O,
Smith NL, Reid I, Gandhi J, Jiang W, Khan SA. Clinical utility of ozone therapy
for musculoskeletal disorders. Med Gas Res. 2018 Sep 25;8(3):103-110. doi: 10.4103/2045-9912.241075 [Crossref]
- Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009 Jul 21;6(7):e1000097. doi: 10.1371/journal.pmed.1000097 [Crossref]
- Maher CG, Sherrington C, Herbert RD, Moseley AM,
Elkins M. Reliability of the PEDro scale for rating
quality of randomized controlled trials. Phys Ther.
2003 Aug;83(8):713-21.
- de Sire A, Stagno D, Minetto MA, Cisari C, Baricich A, Invernizzi M. Long-term effects of intra-articular oxygen-ozone therapy versus hyaluronic acid in older people affected by knee osteoarthritis: A randomized single-blind extension study. J Back Musculoskelet Rehabil. 2020;33(3):347-54. doi: 10.3233/BMR-181294 [Crossref]
- Raeissadat SA, Rayegani SM, Forogh B, Hassan
Abadi P, Moridnia M, Rahimi Dehgolan
S. Intra-articular ozone or hyaluronic acid injection: Which one is superior in
patients with knee osteoarthritis? A 6-month randomized clinical trial. J Pain
Res. 2018 Jan 4;11:111-17. doi: 10.2147/JPR.S142755 [Crossref]
- Raeissadat SA, Ghazi Hosseini P, Bahrami MH, Salman Roghani R, Fathi M, Gharooee Ahangar A, Darvish M. The comparison effects of intra-articular injection of Platelet Rich Plasma (PRP), Plasma Rich in Growth Factor (PRGF), Hyaluronic Acid (HA), and ozone in knee osteoarthritis; a one year randomized clinical trial. BMC Musculoskelet Disord. 2021 Feb 3;22(1):134. doi: 10.1186/s12891-021-04017-x [Crossref]
- Babaei-Ghazani A, Najarzadeh S, Mansoori K, Forogh B, Madani SP, Ebadi S, Fadavi HR, Eftekharsadat B. The effects of ultrasound-guided corticosteroid injection compared to oxygen-ozone (O2-O3) injection in patients with knee osteoarthritis: a randomized controlled trial. Clin Rheumatol. 2018 Sep;37(9):2517-2527. doi: 10.1007/s10067-018-4147-6 [Crossref]
- Lopes de Jesus CC, Dos Santos FC, de Jesus LMOB, Monteiro I, Sant'Ana MSSC, Trevisani VFM. Comparison between intra-articular ozone and placebo in the treatment of knee osteoarthritis: A randomized, double-blinded, placebo-controlled study. PLoS One. 2017 Jul 24;12(7):e0179185. doi: 10.1371/journal.pone.0179185 [Crossref]