Fisioter Bras. 2023;24(6):896-907
ORIGINAL ARTICLE
The influence of muscle variables on delivery route
after perineal preparation in primiparous women
Influência
das variáveis musculares na via de nascimento após preparação perineal em
primíparas
Leticia
Rodrigues Silva, Natasha Morena Bazílio Silva, Alana
Leandro Cabral, Sissi Sisconeto de Freitas, Rogério
de Melo Costa Pinto, Vanessa Santos Pereira-Baldon
Universidade
Federal de Uberlândia, MG, Brazil
Received: August 21, 2023; Accepted: November 28,
2023.
Correspondence: Leticia
Rodrigues Silva, leticiars22@hotmail.com
Como citar
Silva LR, Silva NMB, Cabral AL, Freitas SS, Pinto RMC, Pereira-Baldon VS. The influence of muscle variables on delivery route after perineal preparation in primiparous women. Fisioter Bras. 2023;24(6):896-907. doi: 10.33233/fb.v24i6.5534
Abstract
Introduction: Many pregnant
women seek vaginal delivery, as a healthier and more respectful mode of
delivery, and perineal massage and instrument-assisted perineal stretching
techniques aim to bring better postpartum outcomes. Despite this, some
deliveries may not occur as expected and conclude with interventions or
surgical delivery. Objective: To analyze the influence of muscle
variables on the mode of delivery of women undergoing perineal preparation. Methods:
This is a secondary analysis of a clinical trial in which primiparous women
with a gestational age of 33 weeks were included. Evaluations were performed
before and after eight intervention sessions using perineal massage and
stretching assisted by the Epi-No Delphine Plus® instrument. Perineal
distensibility muscle variables were evaluated using the Epi-No Delphine Plus®
equipment and the peak and mean strength of pelvic floor muscles (PFM) using
the PeritronTM vaginal manometer. After delivery, the
method of delivery performed was determined by telephone contact. For
statistical analysis, univariate logistic regression was performed with a
significance level of 0.05. Results: Sixty-one primiparous women were
included in the study (mean age: 30 years; SD: 4.8). None of the muscle
variables examined were predictors for vaginal delivery (p > 0.05). Conclusion:
Muscle variables did not influence the final delivery route of women undergoing
perineal preparation.
Keywords: cesarean section; natural
childbirth; pelvic floor; perineum; physical therapy specialty.
Resumo
Introdução: Muitas gestantes buscam o parto
vaginal, como uma via mais saudável e respeitosa, e as técnicas de massagem
perineal e alongamento perineal assistido por instrumento tem como objetivo
trazer melhores desfechos no pós-parto. Apesar disso, alguns partos podem não
ocorrer como o esperado e finalizarem com intervenções ou parto cirúrgico. Objetivo:
Analisar a influência das variáveis musculares no tipo de parto de mulheres
submetidas a preparação perineal. Métodos: Trata-se de uma análise
secundária de um ensaio clínico em que foram incluídas primíparas com idade
gestacional de 33 semanas. Foram realizadas avaliações antes e após oito
sessões de intervenção por meio de massagem perineal e alongamento assistido
pelo instrumento Epi-No Delphine
Plus®. Foram avaliadas as variáveis musculares distensibilidade perineal com
uso do equipamento Epi-No Delphine
Plus® e a força pico e média dos músculos do assoalho pélvico (MAP) por meio do
manômetro vaginal Peritron. Após o parto foi
questionado por contato telefônico o tipo de parto realizado. Para a análise
estatística foi realizada a regressão logística univariada
com nível de significância de 0,05. Resultados: Sessenta e uma primíparas foram incluídas no estudo (média de idade: 30
anos; DP: 4,8). Nenhuma das variáveis musculares examinadas foram preditores
para o parto vaginal (p > 0,05). Conclusão: As variáveis musculares
não influenciaram na via de parto final de mulheres submetidas a preparação
perineal.
Palavras-chave: assoalho pélvico; Fisioterapia; parto
normal; períneo; cesárea.
Introduction
In recent years, many women have
sought the vaginal route, with the minimum of interventions, as a more
respectful, healthy, and faster recovery mode of birth [1,2]. For the baby to
pass through the vaginal route, the pelvic floor musculature (PFM) must stretch
approximately 2.5 times its original size, which can result in perineal trauma
[3]. Thus, to improve the delivery experience, perineal preparation techniques
have been developed, such as perineal massage and instrument-assisted perineal
stretching, aiming for better childbirth and postpartum outcomes [4,5]. These
techniques aim to reduce muscle endurance and improve extensibility, allowing
perineal tissue to expand more easily during the baby's passage [5,6].
However, even with the preparation
of the perineum and the desire of the pregnant women for the vaginal route,
some deliveries may not occur as expected. Many pregnant women may undergo
vaginal delivery interventions or are referred for cesarean delivery [2,7]. In
view of these unexpected outcomes, some studies have identified predictive
factors for delivery routes. Advanced maternal age [8], high body mass index
(BMI) [9], advanced gestational age (over 40 weeks) [10] and newborn weight
(over 4,500 g) [11] have been indicated as risk factors for cesarean section.
It is known that the pelvic floor
(PF) muscles play a fundamental role during labor, allowing the passage of the
fetus during the expulsive period [3,12]. However, little is known about the
participation of variables related to the PF muscles in the final method of
delivery. The extensibility of the perineal muscles seems to be extremely
important during delivery, as this region needs to be able to stretch
sufficiently to allow the passage of the fetus through the vaginal canal and
ensure the integrity of the perineum in the postpartum period [3,12,13].
According to Zanetti et al. [13], a circumference larger than 20.8 cm
achieved by a balloon introduced into the vaginal introitus was a predictor of
perineal integrity in parturients. However, in a
systematic review, the authors found no effects of the instrument-assisted
perineal stretching technique on perineal outcomes at delivery [14].
PFM strength also seems to be
important for labor and birth. Although some studies have reported that a
strong musculature could be associated with failures in labor [15], new studies
and systematic reviews reports positive effects of muscle strength [16,17]. Sobhgol et al. [16] found in their systematic review
that antenatal PFM training may be effective in shortening labor and did not
affect the instrumental delivery rate and cesarean section rate. In addition,
another study showed that the strength of the pelvic floor has no negative
effects on vaginal delivery [17].
Despite the influence of muscle
tissue in the passage of the fetus through the birth canal, no studies have
analyzed the possible contribution of muscle variables as predictors of method
of delivery birth. Variables such as PFM extensibility and strength are widely
discussed in the literature, but their relationship with the final outcome of
the delivery route has not yet been studied. Thus, considering the importance
of PFM in the vaginal delivery process and the absence of studies that analyzed
the relationship between the PFM strength and extensibility with the final
birth path, the objective of this study was to analyze the influence of muscle
variables on the type of delivery route of women undergoing perineal
preparation.
Methods
Study design
This study is a secondary analysis
of an unpublished clinical trial, approved by the Ethics and Research Committee
at the Federal University of Uberlândia (no.
3.402.205) and registered in the Brazilian Registry of Clinical Trials (ReBEC - no. RBR-387ntq). All study participants were
informed about the procedures and signed the informed consent form.
The research was carried out at the
Faculty of Physiotherapy at the Federal University of Uberlândia.
Recruitment took place through dissemination on social media, totaling 65
eligible volunteers recruited for evaluation.
Inclusion and exclusion criteria
The study included women over 18
years old, gestational age of 33 weeks, primiparous, who had medical
authorization to perform the intervention, and who wanted vaginal delivery.
The non-inclusion criteria were: multiple
pregnancy, presence of bone deformities, important muscle and nervous
disorders, presence of high gestational risk, unusual fetal position or risks
that preclude vaginal delivery (placenta previa), risk of ascending infection
like vaginal infection, presence of unhealed lesions in the vaginal region,
presence of vaginal bleeding, presence of cervical cancer, inability to
contract the pelvic floor muscles, intolerance to vaginal palpation, presence
of neurological and/or cognitive disabilities that make it impossible to
understand the proposed procedures, use of prenatal methods of preparing the
pelvic floor before taking part in the study, and being visibly under the
influence of illegal drugs or alcohol.
The volunteers who missed two
consecutive interventions or who had a medical request to interrupt the
sessions were excluded.
Assessments
The study participants were
evaluated before and after the intervention regarding the variables perineal
distensibility and PFM strength, by two trained and experienced evaluators.
After delivery, telephone contact was made and the method of delivery and the
type of delivery assistance performed were determined.
During the initial evaluation, the
eligible pregnant women, with 33 gestational weeks, were submitted to a
standard interview with questions about their urogynecological
and obstetric history and their life habits. Next, in the dorsal decubitus
position, with hips and knees semi-flexed and feet supported on the examination
table, vaginal palpation was performed to verify if the volunteer could perform
satisfactory voluntary muscle activation. Satisfactory activation was defined
as a muscle contraction equal or bigger than 2 by the Modified Oxford scale.
For the measurement of PFM strength,
vaginal manometry was performed, with the aid of the PeritronTM
electronic manometer. The vaginal probe was initially coated with a
non-lubricated condom and lubricated with a water-based gel. Then it was
introduced until its center reached approximately 3.5 cm in the volunteer's
vaginal introitus. The device was calibrated to zero before starting the
measurements and the researcher instructed the performance of three maximal
contractions, with duration of 5 seconds each, with a 30-second interval in
between. The arithmetic mean of the mean values and arithmetic mean of the peak
values of the three contractions were used for the statistical analysis of the
manometry data.
The perineal distensibility was
evaluated using Epi-No Delphine Plus® equipment (Starnerg
Medical, Tecsana, Munich, Germany). The equipment was
coated with a non-lubricated condom and lubricated with water-based gel, and
then introduced into the volunteer's vaginal introitus so that 2 cm of the
equipment base was visible. The pregnant woman was informed that she should
keep the PFM relaxed throughout the procedure. The equipment was inflated to
the pregnant woman's tolerance, for a 1-minute interval. After the interval,
this procedure was repeated two more times and finally, the volunteer was
instructed to expel the equipment, still inflated, during exhalation. With the
equipment still inflated, the condom was removed, and the examiner measured the
balloon at its largest circumference, using a metric tape measure [18].
Intervention
Eight interventions were performed,
from the 34th to the 38th gestational week, with a frequency of twice a week.
Perineal massage and instrument-assisted perineal stretching techniques were
performed by two researchers experienced in the use of these techniques during
pregnancy.
Initially, the perineal massage was
performed for about 10 minutes. With the pregnant woman in the dorsal decubitus
position, with hips and knees semi-flexed and feet supported on the examination
table, the researcher introduced two fingers, lubricated with almond oil, about
3 to 5 cm into the vaginal introitus. The technique consisted of performing an
internal massage in lateral semicircles, towards the anus, for 20 to 30 seconds
(repeating the procedure four times). Soon after, the physiotherapist put
pressure on each lateral wall of the vagina, for 2 minutes, and then down. At
the end, the vagina was massaged in motion simulating the letter U [19].
Instrument-assisted perineal
stretching was performed using the Epi-No Delphine Plus® device (Tecsana GmbH, Munich, Germany). For this, the equipment was
coated with a non-lubricated condom and lubricated with water-based gel. With
the pregnant woman still in the same position as the perineal massage, the
equipment was inserted into the vaginal introitus and inflated to maximum
tolerance for 15 minutes, with the device being able to be inflated again
within this period. At the end, the researcher instructed the volunteer to
expel the equipment during exhalation [13].
Data analysis
For the sample calculation, the Bioestat 5.0 software was used. Considering the sample size
so that it can be identified, with 95% confidence (error α = 0.05) and a
test power of 80% (error β = 0.20), a significant model in logistic
regression with a pseudo R2 significant above 23%, the minimum sample size
would be 50 patients [20].
Statistical analyses were performed
using the SISVAR software. The normality of the data was tested by the
Shapiro-Wilk test. Univariate logistic regression was used to determine odds
ratios (OR) and significant associations between muscle variables predictors
and vaginal birth. The t-test was applied to compare variables between
participants with vaginal and cesarean delivery. The level of significance
adopted was 0.05.
Results
Sixty-five primiparous volunteers
were assessed, aged between 21 and 43 years and gestational age of 33 weeks.
Four pregnant women were excluded, three because they were unavailable for the
visits and one for presenting a medical request for interruption (Figure 1).
The 61 included volunteers were in the data analysis. Table 1 shows the sample
characterization.

Figure 1 - Study participants
Table I - Sample characterization
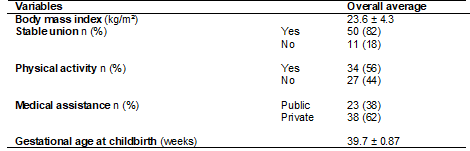
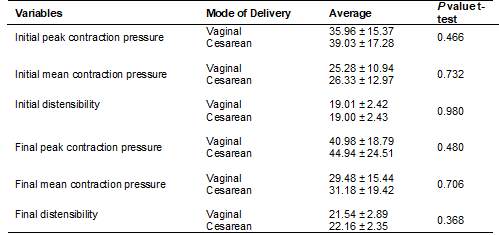
Regarding the mode of delivery, 31
(50.8%) of the deliveries were vaginal and 30 (49.2%) were cesarean sections.
When the participants were divided by the mode of delivery, no statistically
significant differences were observed between them in the initial or final
muscle variables (Table II).
Table II - Variables when the sample was
divided by the type of vaginal delivery (n = 31) and cesarean section (n = 30)
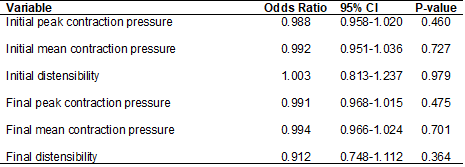
Logistic regression was performed
involving the predictor variables (initial and final mean contraction pressure,
initial and final peak contraction pressure and initial and final
distensibility) and considering vaginal delivery as the reference variable. The
results showed that none of the variables analyzed demonstrated statistical
significance as a predictor for the vaginal route in the initial or final
muscle variables (Table III).
Table III - Univariate logistic
regression using vaginal delivery as a reference
Discussion
The results of the present study
demonstrate that PF muscle variables are not predictors of the vaginal route,
either before or after the intervention. The importance of PFM during delivery
and expulsion of the fetus is known. During delivery, the PFM act in concert
with the uterine contractions and the contraction of the abdominal muscles and
mold themselves around the fetal head during descent through the vaginal canal.
For this action to happen, the perineal musculature is subjected to extreme
stretching [3,12,21].
The flexibility of the perineal
tissue is improved throughout pregnancy, thanks to hormonal changes and changes
in the concentration of collagen in the PFM. There is also an increase in the
length of muscle fibers, in response to the overload exerted on this
musculature during the gestational period, enabling greater muscle distension
during fetal passage [22,23]. Thus, the elastic capacity of the musculature to
achieve the necessary stretching, in addition to assisting in the passage of
the fetal head, allows vaginal delivery to happen with lower rates of perineal
trauma [12,21].
It is possible that there are
differences between the measurement of perineal extensibility at the end of
pregnancy and that performed during labor, due to the hormonal action during
the process. Zanetti et al. [13] evaluated the maximal distensibility of
the PFM of nulliparous and multiparous parturients
and concluded that a greater capacity of perineal distensibility is associated with
lower rates of trauma, with the cut-off point for perineal integrity of 20.8 cm
circumference of the Epi-No® equipment, same equipment used for measurement in
the present study. Thus, despite not being a predictor of the route of birth,
perineal extensibility seems to be important for perineal integrity after
vaginal delivery. However, in this study, the relationship between
distensibility and cesarean delivery was not analyzed.
The PFM strength also did not show
statistical significance as a predictor for vaginal delivery. This finding is
in agreement with the study carried out by Bø et
al. [17] who showed that PFM strength and endurance did not affect cesarean
rates, second stage of delivery, instrumental vaginal delivery, and third- and
fourth-degree perineal trauma. Thus, the authors concluded that the ability of
nulliparous women to contract or maintain maximum PFM contraction does not have
negative effects on childbirth.
In addition to no harm, studies
have demonstrated that strong and well-controlled muscles seem to facilitated
labor and reduce the need for instrumental delivery [24,25]. The effects of
antenatal PFM interventions results in improved muscle
control and strong, flexible muscle, which may contribute to the descent,
flexion, and rotational movements of the fetal head [16,25].
In the present study, an increase
in strength and extensibility was observed in both delivery routes, after the
intervention using perineal massage and instrument-assisted perineal
stretching. Although not the objective of this study, the finding that the
techniques can promote muscle benefits opens the way for further research on
possible neural gains with the performance of perineal preparation techniques
for childbirth.
This study is limited by the
impossibility of having all volunteers monitored by the same medical team in
the same hospital. It is known that, in Brazil, the obstetric care model still
presents a scenario quite marked by medical interventions during childbirth and
by high rates of operative deliveries [26], which may have influenced the route
of birth. As well as the lack of standardization and consensus between the
medical procedures performed during childbirth, they may also have influenced
the final outcome.
Another limitation of this study is
the difficulty in evaluating PFM distensibility. Pelvic floor stretching is not
related to joint movement, as in other muscle groups, which makes its assessment
more complex. Therefore, the Epi-No Delphine Plus® has been used by several
authors, as an evaluation and measurement method of pelvic floor stretching
[13,18,27].
To the authors’ knowledge, this
study is the first to examine the relationship between the strength and
extensibility of the AP with the final delivery route. The strengths of this
study are the previous sample size calculation, few withdrawals, high adherence
to the training protocol, blinded and experienced assessors, and physiotherapists
trained in the use of the applied techniques.
Conclusion
Based on this study, it can be
concluded that the muscle variables PFM strength and distensibility did not
influence the final delivery route of women undergoing perineal preparation.
Conflitos
de interesse
Nenhum
Fontes
de financiamento
Este
estudo foi financiado em parte pela Fundação de Amparo à Pesquisa do Estado de
Minas Gerais (FAPEMIG - APQ-01085-15) e pela Coordenação de Aperfeiçoamento de
Pessoal de Nível Superior (CAPES) – Código de financiamento 001.
Contribuição
dos autores
Concepção
e desenho da pesquisa:
Silva LR, Pereira-Baldon VS; Coleta de dados:
Silva LR, Silva NMB, Cabral AL, Freitas SS; Análise e interpretação dos
dados: Silva LR, Pinto RMC, Pereira-Baldon VS; Análise
estatística: Silva LR, Pinto RMC, Pereira-Baldon
VS; Redação do manuscrito: Silva LR, Pereira-Baldon
VS; Revisão crítica do manuscrito quanto ao conteúdo intelectual importante:
Silva LR, Silva NMB, Cabral AL, de Freitas SS, Pinto RMC, Pereira-Baldon VS
References
- World Health Organization. Who recommendations on
intrapartum care for a positive childbirth experience. World Health
Organization; 2018. [Internet]. [cited 2020 Sep 24]. Available from:
https://www.who.int/reproductivehealth/publications/intrapartum-care-guidelines/en/
- Arik RM, Parada CMGL, Tonete
VLP, Sleutjes FCM. Perceptions and
expectations of pregnant women about the type of birth. Rev Bras Enferm. 2019;72:41-9. doi: 10.1590/0034-7167-2017-0731
- Hoyte L, Damaser MS,
Warfield SK, Chukkapalli G, Majumdar A, Choi DJ.
Quantity and distribution of levator ani stretch
during simulated vaginal childbirth. Am J Obstet
Gynecol. 2008;199:198.e1-198.e5. doi:
10.1016/j.ajog.2008.04.027
- Beckmann MM, Stock OM. Antenatal perineal massage for
reducing perineal trauma. Cochrane Database of Systematic Reviews. 2013. doi: 10.1002/14651858.CD005123.pub3
- Kovacs GT, Heath P, Heather C. First Australian trial
of the birth-training device Epi-No: A highly significantly increased chance of
an intact perineum. Aust N Z J Obstet Gynaecol. 2004;44:347–8. doi: 10.1111/j.1479-828X.2004.00265.x
- Abdelhakim AM, Eldesouky E, Elmagd IA, Mohammed
A, Farag EA, Mohammed AE, et al. Antenatal perineal massage benefits in
reducing perineal trauma and postpartum morbidities: a systematic review and
meta-analysis of randomized controlled trials. Int Urogynecol J. 2020;31:1735–45.
doi: 10.1007/s00192-020-04302-8
- Weidle WG, Medeiros CRG, Grave MTQ, Dal Bosco
SM. Escolha da via de parto pela mulher: autonomia ou indução? Cad Saúde Colet. 2014;22:46–53. doi: 10.1590/1414-462X201400010008
- Rydahl E, Declercq
E, Juhl M, Maimburg RD. Cesarean
section on a rise—Does advanced maternal age explain the increase? A population
register-based study. PLoS ONE. 2019;14:e0210655. doi:
10.1371/journal.pone.0210655
- Chu SY, Kim SY, Schmid CH, Dietz PM, Callaghan WM, Lau
J, Curtis KM. Maternal obesity and risk of cesarean delivery: a meta-analysis. Obes Rev. 2007;8:385-94. doi: 10.1111/j.1467-789X.2007.00397.x
- Heffner L. Impact of labor induction, gestational age,
and maternal age on cesarean delivery rates. Obst
Gynecol. 2003;102:287–93. doi:
10.1016/S0029-7844(03)00531-3
- Macrosomia: ACOG Practice Bulletin, Number 216. Obstet Gynecol. 2020;135:
e18–e35. doi: 10.1097/AOG.0000000000003606
- Mendes
NA, Mazzaia MC, Zanetti MRD. Análise crítica sobre a
utilização do Epi-No na gestação e parto. ABCS
Health Sci. 2018;43. http://dx.doi.org/10.7322/abcshs.v43i2.1091
- Zanetti MRD, Petricelli CD,
Alexandre SM, Paschoal A, Araujo Junior E, Nakamura
MU, et al. Determination of a cutoff value for pelvic floor distensibility
using the Epi-no balloon to predict perineal integrity in vaginal delivery: ROC
curve analysis. Prospective observational single cohort study. Sao Paulo Med J.
2015;134:97–102. doi:
10.1590/1516-3180.2014.8581009
- Schreiner L, Crivelatti
I, Oliveira JM, Nygaard CC, Santos TG. Systematic
review of pelvic floor interventions during pregnancy. Int J Gynecol
Obstet. 2018;143:10–18. doi: 10.1002/ijgo.12513
- Aran T, Aran T, Osmanagaoglu MA, Kart C, Guven S, Sahin
M, Unsal MA, et al. Failed labor induction in nulliparous women at term:
the role of pelvic floor muscle strength. Int Urogynecol
J. 2012;23:1105–10. doi:
10.1007/s00192-012-1754-7
- Sobhgol SS.
The effect of antenatal pelvic floor muscle exercises on labour
and birth outcomes: a systematic review and meta-analysis. Int Urogynecol J. 2020;15. doi:
10.1007/s00192-020-04298-1
- Bø K, Hilde G,
Jensen JS, Siafarikas F, Engh
ME. Too tight to give birth? Assessment of pelvic floor muscle function in 277
nulliparous pregnant women. Int
Urogynecol J. 2013;2065–70. doi:
10.1007/s00192-013-2133-8
- Freitas
SS, Cabral AL, Melo CPR, Resende APM, Pereira BVS. Effects of
perineal preparation techniques on tissue extensibility and muscle strength: a
pilot study. Int Urogynecol J. 2018;30:951–7.
doi: 10.1007/s00192-018-3793-1
- Labrecque M,
Eason E, Marcoux S, Lemieux F, Pinault JJ, Feldman P, Laperrière
L. Randomized controlled trial of prevention of perineal trauma by perineal
massage during pregnancy. Am J Obstet Gynecol.
1999;180. doi: 10.1016/S0002-9378(99)70260-7
- Hair Jr JF, Black WC, Babin
BJ, Anderson RE, Tatham RL. Análise
multivariada de dados. Bookman; 2009.
- Silva MET, Oliveira DA, Roza
TH, Brandão S, Parente MPL,
Mascarenhas T. Study on the influence of the fetus
head molding on the biomechanical behavior of the pelvic floor muscles, during
vaginal delivery. J Biomech. 2015;48:1600–5. doi: 10.1016/j.jbiomech.2015.02.032
- Moccellin AS, Rett MT, Driusso P. Existe alteração na função dos músculos do
assoalho pélvico e abdominais de primigestas no segundo e terceiro trimestre
gestacional? Fisioter Pesqui.
2016;23:136–141. doi:
10.1590/1809-2950/14156523022016
- Alperin M, Lawley DM,
Esparza MC, Lieber RL. Pregnancy-induced
adaptations in the intrinsic structure of rat pelvic floor muscles. Am J Obstet Gynecol. 2015;213:191.e1-191.e7.
doi: 10.1016/j.ajog.2015.05.012
- Salvesen, KÅ, Mørkved S. Randomised controlled trial of pelvic floor muscle training
during pregnancy. BMJ. 2004;329:378–80. doi: 10.1136/bmj.38163.724306.3a
- Du Y, Xu L, Ding L, Wang Y, Wang Z. The effect of
antenatal pelvic floor muscle training on labor and delivery outcomes: a
systematic review with meta-analysis. Int Urogynecol J. 2015;26:1415–27.
doi: 10.1007/s00192-015-2654-4
- Zanardo
GLP, Uribe MC, Nadal AHRD, Habigzang LF. Violência
obstétrica no Brasil: uma revisão narrativa. Psicol
Soc. 2017;29. doi: 10.1590/1807-0310/2017v29155043
- Nakamura MU, Sass N, Elito Júnior J, Petricelli CD, Alexandre SM, Edward Araujo Júnior E, et al. Parturient perineal distensibility tolerance assessed by EPI-NO: an observational study. Einstein. (São Paulo) 2014;12:22–6. doi: 10.1590/S1679-45082014AO2944