Rev Bras Fisiol Exerc 2020;19(2):141-53
REVIEW
Kinesiotherapeutic
interventions in diaphragmatic mobility of patients with chronic obstructive
lung disease: systematic review
Intervenções cinesioterapêuticas na mobilidade diafragmática de
pacientes com doença pulmonar obstrutiva crônica: revisão sistemática
Gilson Rosa de Jesus1,
Milena Santos Peixoto1, Sidney de Souza Oliveira1,2,3
1Faculdade de Ciências
Empresariais (FACEMP), Santo Antônio de Jesus, BA Brazil
2União Metropolitana de
Educação e Cultura (UNIME), Lauro de Freitas, BA Brazil
3Escola Bahiana de Medicina e Saúde Pública, Salvador, BA Brazil
Received
on 2020, February10; accepted on 2020, April 16.
Corresponding author: Sidney de Souza
Oliveira, Praça Renato Machado, 10 Centro 44573-045 Santo Antônio de Jesus BA
Gilson Rosa de
Jesus: gilsonfisio123@gmail.com
Milena SAntos Peixoto: milena.peixoto.12@hotmail.com
Sidney
de Souza Oliveira: sid_ney2011@hotmail.com
Abstract
This
study analyzed the pathophysiological impacts of Chronic Obstructive Pulmonary
Disease (COPD) on the respiratory system and the benefits of kinesiotherapeutic interventions on diaphragmatic mobility
in patients affected by COPD. Systematic literature review carried out in the Scielo, Medline, VHL, Lilacs and PEDro
databases, using the following keywords: Chronic Obstructive Pulmonary Disease,
Respiratory Rehabilitation, Kinesitherapeutic
Interventions and Diaphragmatic Dysfunction. Only original articles published
between 2009 and 2019, about the benefits of different respiratory physical
therapy intervention programs were included. Two examiners analyzed the
qualities and evidence of the articles using the PEDro
scale. Twelve manuscripts make up the discussion of this work. The present
study confirms the beneficial effects of different Kinesiotherapy Intervention
programs on physical health and quality of life, reduction of respiratory
symptoms and risk of mortality, increased mobility of the rib cage, diaphragmatic
functionality, functional capacity and respiratory muscle strength of patients
affected by COPD.
Keywords: chronic obstructive pulmonary disease; respiratory rehabilitation; kinesiotherapeutic interventions; diaphragmatic
dysfunction.
Resumo
Este estudo analisou os
impactos fisiopatológicos da Doença Pulmonar Obstrutiva Crônica (DPOC) no
sistema respiratório e os benefícios das intervenções cinesioterapêuticas
na mobilidade diafragmática em pacientes acometidos pela DPOC. Revisão
sistemática de literatura, realizada nas bases de dados Scielo,
Medline, BVS, Lilacs e PEDro,
utilizando em cruzamentos os seguintes descritores: Doença Pulmonar Obstrutiva
Crônica, Reabilitação Respiratória, Intervenções Cinesioterapêuticas
e Disfunção Diafragmática. Incluídos apenas artigos originais, publicados entre
2009 e 2019, que versassem sobre os benefícios de diferentes programas de
intervenções fisioterapêuticas respiratórias. Dois examinadores analisaram as
qualidades e evidências dos artigos por meio da escala PEDro.
Doze manuscritos compõem a discussão deste trabalho. O presente estudo confirma
os efeitos benéficos de diferentes programas de Intervenções Cinesioterapêuticas sobre a saúde física e qualidade de
vida, redução dos sintomas respiratórios e do risco de mortalidade, aumento na
mobilidade da caixa torácica, funcionalidade diafragmática, capacidade
funcional e da força muscular respiratória de pacientes acometidos pela DPOC.
Palavras-chave: doença pulmonar
obstrutiva crônica, reabilitação respiratória, intervenções cinesioterapêuticas,
disfunção diafragmática.
Introduction
According to the Informatics Department of the Brazilian Unified Health
System [1], three individuals die every hour due to Chronic Obstructive
Pulmonary Disease (COPD), which corresponds to approximately 40,000 deaths per
year in the country. Due to the increase in tobacco consumption mainly in
developing countries and the aging population in high-income countries, the
prevalence is expected to increase worldwide, with the expectation of 4.5
million annual deaths in 2030, however, currently under diagnoses impact the
accuracy of pathology-related mortality data [2].
COPD is a preventable and treatable disease, characterized by persistent
respiratory symptoms and limited airflow due to abnormalities of the airways or
alveolar airways usually caused by significant exposure to harmful particles or
gases, that cause a chronic inflammatory response and that can produce changes
in the bronchi resulting in chronic bronchitis (defined as the presence of
cough and mucus production for at least three months in two consecutive years)
and pulmonary emphysema (characterized by destruction of the alveolus) [2,3].
The increase in airway resistance may cause, throughout the evolutionary
process of the disease, other pulmonary changes identified by the increase in
static lung volumes. This progressive process is recognized as air trapping and
has been considered an important limiting factor in diaphragmatic function in
patients with COPD [4]. The respiratory system has some muscles, the diaphragm
being the main muscle for ventilation and anatomically separates the chest from
the abdominal cavity, with differences between the diaphragmatic domes, the
right being higher than the left [5]. Craniocaudal movement of this muscle
promotes the perfect performance of pulmonary mechanics, making morphological
and functional changes in the thoracic and abdominal cavity, resulting in air
entering the lungs. It is essential that the diaphragm moves in its entirety
and with the ideal length-tension relationship for synergy to occur with the
abdominal muscles [6,7].
Over the years, studies have shown that the decrease in diaphragmatic
mobility (DM) occurs by reducing this relationship in the apposition zone and
in the radius of curvature of the diaphragmatic muscle [8], in addition to
promoting changes in volumes and lung capacity, interfere with performance,
mobility and conformity of the diaphragm, which loses its dome shape and tends to
rectify, reducing its apposition zone and limiting the ventilatory action,
normally more evident in the lower portion of the rib cage, which may lead the
patient to paradoxical breathing due to the disorder between the thoracic and
abdominal compartments [9].
In some studies, it was observed that patients classified as mild COPD
had a higher DM when compared to patients classified as severe. The same
authors also observed relationships between DM with functional vital capacity
(FVC) and slow vital capacity (SVC). These results support the hypothesis that
the reduction in DM may be related to the severity of COPD [10]. The acting of Kinesiotherapeutic Interventions is of fundamental
importance, helping in recovery and rehabilitation, seeking to interfere in
these mechanisms, improving the functional capacity of the patient and
restoring his independence [11].
Based on this information, this review sought scientific evidence to
demonstrate and/or prove the benefits of Kinesiotherapeutic
Interventions in improving diaphragmatic mobility in patients affected by COPD,
justified by the high incidence of individuals affected by COPD, taking into
account the pathophysiological impacts caused by respiratory system and the
need for physiotherapeutic approaches that are better elucidated and
scientifically proven as to their effectiveness, thus facilitating the
compliance and rehabilitation of these patients.
Methods
The present study is characterized as a systematic literature review,
carried out with original articles published in scientific journals indexed in
the databases Pubmed, Scielo,
Medline, BVS, PEDro and Lilacs, in the period from
2009 to 2019, using health descriptors: chronic obstructive pulmonary disease,
respiratory rehabilitation, kinesiotherapeutic
interventions and diaphragmatic dysfunction and their correlates in English.
The studies that fit the inclusion criteria were selected: a) Original
studies; b) Studies in which the participants presented only the diagnosis of
COPD; c) Clinical studies that applied physical therapy intervention programs
as a form of intervention; Studies were excluded: a) Whose participants had a
chronic disease in addition to COPD; b) Studies that described only clinical
recommendations; c) Studies that did not describe the intervention performed
with the participants; d) Duplicate studies; e) Case reports, doctoral thesis
and master's dissertation. Data selection and extraction.
The screening process of the studies was carried out initially by reading
the titles. Posteriorly, duplicate articles were excluded, and titles and
abstracts were read to verify that they met the eligibility criteria of the
present study. The articles that met the established criteria were retrieved
for reading the full text, reassessment of the eligibility criteria and data
extraction regarding a) the author and year of publication, (b) objectives, (c)
sample and method of assessing muscle strength, (d) intervention and (e)
results of muscle strength (Table I). Lastly, the references of the main
studies included in this review were evaluated, in order to verify the
existence of unidentified eligible articles in the searches in the selected
databases (Figure 1). Resume the process of screening and selecting studies.
The selected studies were submitted by two examiners to a qualitative
evaluation of the methodology used through the PEDro
scale and were evaluated according to the quality indicators shown on the
scale. The application of the PEDro scale in the
evaluation of each article results in a final score that can vary from 0 (zero)
to 10 (ten), and only the articles that obtained a score equal to or greater
than 3 (three) points were used in the present study (Table I).
The information available in the articles included in this review was
extracted and summarized in a standardized manner, based on the following
topics: authors/year of publication, Qualis score,
study title, type of study/sample number, type of intervention, total
intervention time and a brief description of the results obtained. After being
extracted, the data were allocated in a summary table to facilitate the
analysis of the results (Table II).
Results
The search in the databases initially identified 561 studies of which
207 were excluded because they were review articles, doctoral thesis, master's
thesis and case report, 122 articles were excluded because they addressed other
pathologies besides COPD, 188 articles were excluded because they did not
directly address the topic and 32 studies were excluded because they did not
describe applied physical therapy interventions, leaving 12 articles as
potentially relevant for this review, as shown in the flowchart below (Figure
1).
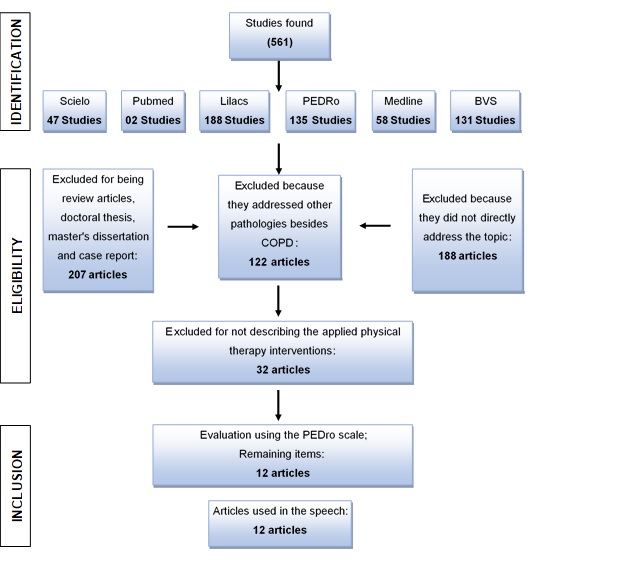
Figure
1 - Flowchart of screening and selection of studies
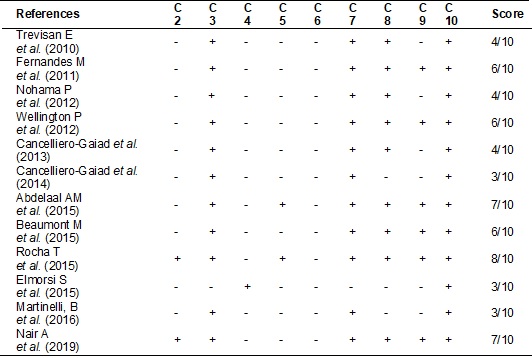
The 12 selected articles were evaluated on the PEDro
scale according to the following quality indicators of the evidence presented:
1. specification of the inclusion criteria (item not scored); 2. random
allocation; 3. secrecy in the allocation; 4. Similarity of the groups in the
initial or baseline phase; 5. masking the subjects; 6. masking those
responsible for the intervention; 7. masking the evaluator; 8. measurement of
at least one primary outcome in 85% of the allocated subjects; 9. analysis of
the intention to treat; 10. comparison between groups of at least one primary
outcome; and 11. reporting of variability measures and estimating parameters
for at least one primary variable, who received an assigned point (in relation
to presence) or no assigned point (in relation to absence) of the indicators.
The articles selected in this study are shown in Table I.
Table
I - Presentation of the score of the selected
articles, according to the PEDro scale. C Scoring
Criteria
Table
II - Clinical characteristics of the studies selected
for this review. (see PDF annexed)
Discussão
According to studies, the reduction in diaphragmatic mobility (MD) is
one of the main risk factors for increased mortality in patients with COPD.
Thus, interventions that encourage the use of specific techniques that aim to
increase the mobility of the diaphragm and rib cage should be prioritized [9].
The results found in this systematic review point to the acute and chronic
benefits of the various techniques of Kinesiotherapeutic
Interventions in the diaphragmatic mobilization of patients with COPD, showing
the immense importance it has for the rehabilitation of these patients [12].
Studies have shown that techniques such as diaphragmatic breathing
[19-21,23,24] electrical stimulation [13-15] and inspiratory muscle training
[16-18] promoted improvements in diaphragmatic mobility [14,20,22,24] among
other benefits such as increased inspiratory muscle strength [13,14,16,17].
On electrical stimulation techniques, the study by Nohama
et al. [13], showed that after 10 sessions lasting 20 minutes of
synchronized transcutaneous diaphragmatic stimulation, an electrical
stimulation system controlled by the respiratory signal, generated an increase
in inspiratory muscle strength in all patients, improved quality of life and
decreased symptoms. Similarly, Cancelliero-Gaiad et
al. [14] evaluated 8 patients with COPD, using transcutaneous electrical
diaphragmatic stimulation, showing that after 12 sessions lasting 30 minutes
each, there was an increase in MIP, MEP and thoracoabdominal expandability
without interfering with spirometric variables, also
showing that these increases were maintained for four weeks after the
completion of the intervention. Corroborating with the studies above,
Martinelli et al. [15] aiming to identify changes after transcutaneous
electrical diaphragmatic stimulation by the Russian current in 13 patients with
COPD, it was found that after 30 sessions lasting 30 minutes, patients showed
improvement in minute volume, BODE index (Body Mass Index, Airflow Obstruction,
Dyspnea and Exercise Capacity) which is a multigrade
system used primarily as a predictor of mortality risk in COPD patients and in
the distance covered in the 6-minute Walk Test (6MWT). Although these are
studies without a control group, it is possible to infer that
electrostimulation may be a viable therapeutic alternative to recover the
clinical condition of inspiratory muscle weakness and limitations in
thoracoabdominal mobility observed in patients with COPD.
Another technique that can be used to improve diaphragmatic mobility in
patients with COPD, it is inspiratory muscle training (IMT) that may or may not
be associated with lower limb muscle training (lower limbs). In this sense, Trevisan et al. [16] verified the effectiveness of
respiratory muscle and quadriceps training on the functional performance of 9
individuals with COPD, noting that after 16 sessions, patients showed
improvement in MIP, distance covered on the 6MWT, quadriceps muscle strength,
functional capacity and quality of life. The training of the inspiratory
muscles and quadriceps proved to be beneficial to the functional performance of
individuals with COPD, suggesting the use of respiratory and peripheral muscle
strengthening as a supporting resource in the treatment of these individuals.
Following this reasoning, Elmorsi et al. [17]
assessed the effectiveness of inspiratory muscle training as part of physical
training in 60 male patients with COPD, divided into 3 groups. After 8 weeks of
intervention, it was noted that the IMT associated with peripheral muscle
training led to a significant improvement in MIP, MEP and distance covered in
the 6MWT compared to isolated peripheral muscle exercise training. However,
both improved dyspnea, the BODE index (Body Mass-Index, Airflow Obstruction,
Dyspnea and Exercise Capacity) which is a multigrade
system used primarily as a predictor of mortality risk in COPD patients and the
SGRQ-C (St George's Respiratory Questionnaire for COPD Patients) a version
shorter derived from the original version SGRQ (St George's Respiratory
Questionnaire) after detailed analysis of data from large studies in COPD and
addresses aspects related to three domains: symptoms, activity and psychosocial
impacts that respiratory disease inflicts on the patient without significant
differences between the two groups. The study showed that IMT offers additional
benefits when associated with peripheral muscle training for patients with COPD
and with weakness of inspiratory muscles. However, in patients without
inspiratory muscle weakness (MIP ≥ 60 cmH2O) when assessing
dyspnea, MIP and 6MWT, Beaumont et al. [18], compared IMT with aerobic exercise
associated with upper and lower muscle training in 34 patients divided into 2
groups, with COPD and without inspiratory muscle weakness (MIP ≥ 60 cmH2O),
after 15 30-minute sessions, the IMT improved FEV1 <50% of the predicted
value, while no benefit was seen in patients with FEV1 > 50% predicted. IMT
did not improve dyspnea or the functional parameter in COPD patients with PImax ≥ 60 cmH2O, However, in the subgroup
of patients with FEV1 < 50% predicted, these items have been significantly
improved. Thus, we can suggest that IMT is more effective in improving dyspnea
and exercise tolerance when used in patients with COPD and MIP < 60 cmH2O.
Diaphragmatic breathing (DB) is also a technique widely used in
pulmonary rehabilitation of patients with COPD, with the aim of improving
abdominal movement and reducing chest excursion time and the activity of
respiratory muscles in the rib cage, however, it has been little studied in the
scientific literature. Thus, when addressing the breathing patterns that aim to
raise awareness of the abdominal thoraco breathing
movements, improve the movement of the rib cage, optimize the functionality of
the respiratory muscles and promote the improvement of pulmonary ventilation,
Fernandes et al. [19] investigated the effects of diaphragmatic
breathing on pulmonary ventilation and on the breathing pattern of 44 patients
with moderate and severe COPD. The authors applied DB every day (4 minutes of
natural breathing + 2 minutes of DB + 4 minutes of natural breathing) and after
4 sessions, DB was associated with a significant increase in tidal volume (VC)
and reduction in respiratory rate (RR), providing greater ventilation and
oxygen saturation (SPO2), reduction in ventilation of dead space and
the ventilatory equivalent of carbon dioxide. Despite the small number of
sessions, diaphragmatic breathing was able to improve breathing pattern and
ventilatory efficiency without causing dyspnea in patients with severe and
moderate COPD whose respiratory muscular system is preserved. Following this
idea, Wellington et al. [20] aiming to identify the benefits of
diaphragmatic breathing training in abdominal mobility, evaluated 30 patients
divided into 2 groups. The results showed that after 12 sessions, the
intervention group when compared to the control group, showed greater abdominal
movement during natural breathing, reduction in the relationship between the
rib cage and abdominal movement, increase in the distance covered in the 6MWT,
improvement in SGSQ-C. The diaphragmatic breathing training program for
patients with COPD induced increased participation of the diaphragm during
natural breathing, resulting in an improvement in the patients' functional
capacity. These results underscore the importance of DB as a kinesiotherapeutic intervention for adjuvant treatment for
patients with COPD. In order to compare ventilatory parameters during DB and pilates breathing (PB), Cancelliero-Gaiad
et al. [21] evaluated 15 patients affected by COPD and 15 healthy,
performing natural breathing, DB and PB. The results showed that DB had
positive effects, such as increased lung volumes, respiratory movement and SpO2
and reduced respiratory rate. Although there were no changes in volume and time
measurements during PB in COPD, this breathing pattern increased volumes in
healthy individuals and increased oxygenation in both groups. In this context,
the acute benefits of DB are emphasized as a supportive treatment in
respiratory rehabilitation programs.
When talking about manual techniques, the manual release technique
improves diaphragmatic mobility, inspiratory capacity and exercise capacity in
people with COPD, that said, Rocha et al. [22] evaluated the
effectiveness of the manual release technique of the diaphragm in 10 patients
with COPD and compared it with 10 patients who underwent simulated treatments,
for a total of 6 sessions. After the intervention, the manual release technique
of the diaphragm showed a significant increase in diaphragmatic mobility with
difference between groups. The manual release diaphragm group had a significant
increase in PEmax and PImax.
The study suggests that the manual release technique improves diaphragmatic
mobility, exercise capacity and inspiratory capacity in people with COPD. In
another study, Abdelaal et al. [23]
investigated the benefits of diaphragmatic and rib manipulation in ventilatory
functions (VF) and functional capacity (FC) in patients with COPD. 195 men were
randomly divided into (GA = 46 patients) who underwent diaphragmatic
manipulation and (GB = 53 patients) performing rib elevation, (CG = 50
patients) who performed both procedures and (DG = 46 patients as control), all
participants received drug treatments. After the intervention that lasted 24
sessions, the results showed that there was a significant increase in the mean
values of the 6MWT in Groups A, B and C, with Group C having more significant
differences. Thus, diaphragmatic and costal manipulations are effective
therapeutic techniques to improve VF and HR in COPD patients, especially if
applied together.
In parallel with these techniques, respiratory muscle stretching is
another kinesiotherapy intervention used to break the
shortening-contraction-shortening cycle, of the diaphragm muscle, present in
COPD patients. In a recent randomized study, Nair et al. [24], in which
20 patients were allocated in GA = 10 patients undergoing the diaphragmatic
stretching technique and GB = 10 patients undergoing the manual diaphragm
release technique, showed that both groups showed significant improvement in
diaphragmatic excursion and chest expansion, meantime, there was no
statistically significant difference between the techniques. This result
indicates that both can be effective in improving diaphragmatic mobility. It
would be better if the authors included a placebo group to assess whether there
was a difference between kinesiotherapy interventions and the placebo group.
Although the results are positive, some points must be listed. 1) The
evaluation of interventions in adult patients may not adequately represent
young people and the elderly; 2) the lack of standardization of the techniques
makes the protocols fluctuate and cannot be compared properly; 3) analyzing the
results based only on statistical precepts, limits clinical inferences and,
therefore, the applicability of results in clinical practice; 4) the protocols
follow-up period may not have been sufficient to promote responses from a
clinical point of view, studies are needed with a longer follow-up time; and 5)
the descriptors referring to diaphragmatic mobilization and its synonyms showed
low sensitivity and specificity, limiting searches in electronic databases.
Although the aspects described need to be further discussed, they do not
diminish the importance of the results found.
Therefore, even in the face of the above limitations, we can understand
that kinesiotherapy interventions bring benefits to patients affected by COPD,
due, because, considered effective as an adjunctive treatment for this disease,
especially about diaphragmatic mobility. Even so, we do not rule out the need
for more robust studies such as clinical trials with a control group, to better
assess the benefits of each kinesiotherapy intervention.
Conclusion
The results indicate that kinesiotherapeutic
interventions lead to a significant improvement in diaphragmatic mobility in
individuals with COPD. Other benefits include reduced respiratory symptoms and
the risk of mortality, significant improvement in quality of life related to
physical health, increased mobility of the rib cage, functionality,
functional
capacity and respiratory muscle strength.
This work corroborates the importance of incorporating regular breathing
programs into conventional COPD treatment, as examples: manual release
techniques, respiratory incentive devices, electrostimulation and breathing
pattern techniques, directed at increasing the mobility of the rib cage improve
chest expansion and exercise capacity in these patients.
Authors’
contributions
Jesus GR, Oliveira SS conceived the study and research design. Jesus GR,
Oliveira SS, Peixoto MS analyzed and interpreted the data. Jesus GR, Oliveira
SS wrote the manuscript. Sacramento MS, Oliveira SS They made a critical review
of the manuscript as the important intellectual content.
Potential
conflict of interest
No potential conflict of interest relevant to this article was reported.
Funding
sources
There were no external funding sources for this study.
References
- Datasus. Sistema de
informações hospitalares – SIH/SUS. Ministério da Saúde; 2014.
- Global Strategy for the Diagnosis, (GOLD). Management
and Prevention of COPD, Global Iniciative for Chronic
Obstructive Lung Disease; 2018.
- Jardim JR, Oliveira JA,
Nascimento O. II Consenso Brasileiro sobre Doença Pulmonar Obstrutiva Crônica –
DPOC. J Bras Pneumol
2004;30(1):42.
- Yamaguti WPS, Paulin E, Shibao S, Chammas MC, Salge JM, Ribeiro M, Cukier A, Carvalho CRF. Air
trapping: The major factor limiting diaphragm mobility in chronic obstructive
pulmonary disease patients. Respirology
2008;13(1):138-144. https://doi.org/10.1111/j.1440-1843.2007.01194.x
- Nason LK, Walker CM, McNeeley
MF, Burivong W, Fligner CL,
Godwin JD. Imaging of the diaphragm: anatomy and function. Radiographics
2012;32(2):51-70. https://doi.org/10.1148/rg.322115127
- Lanzetti CEG, Mitsuya MMF, Lima AB. Análise da força muscular respiratória em pneumopatas crônicos participantes do programa de
reabilitação pulmonar. Revista Científica do Uni salesiano 2011;2(4):239-52.
http://www.salesianolins.br/universitaria/artigos/no4/artigo41.pdf
- Pupin MK, Riccetto AGL, Ribeiro JD, Baracat
ECE. Comparação dos efeitos de duas técnicas fisioterapêuticas respiratórias em
parâmetros cardiorrespiratórios pacientes com bronquiolite viral aguda. J Bras Pneumol 2009;35(9);860-7.
https://doi.org/10.1590/s1806-37132009000900007
- Cassart M, Pettiaux
N, Gevenois PA, Paiva M, Estenne
M. Effect of chronic hyperinflation on diaphragm length and surface area. Am J
Respir Crit Care Med 1997;156:504-8.
https://doi.org/10.1164/ajrccm.156.2.9612089
- Yamaguti WPS, Paulin E, Salge JM, Chammas MC, Cukier A, Carvalho
CRF. Diafragmatic dysfunction and mortality in patients with CPOD. J Bras Pneumol 2009;35(12):1174-81.
https://doi.org/10.1590/s1806-37132009001200003
- Davachi B, Lari
S, Attaran D, Tohidi M, Ghofraniha
L, Amini M, Salehi M, Eskandari
E, Yazdi E, Moosavi M, Sm L, Yazdi K. The relationship
between diaphragmatic movements in sonographic assessment and disease severity
in patients with stable chronic obstructive pulmonary disease. J Cardiothorac
Med 2014;(2):187-192.
- Zanchet RC, Viegas CAA,
Lima T. A eficácia da reabilitação pulmonar na capacidade de exercício, força
da musculatura inspiratória e qualidade de vida de portadores de doença
pulmonar obstrutiva crônica. J Pneumol
2005;31(2):118-24. https://doi.org/10.1590/s1806-37132005000200006
- Global
Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the
diagnosis, management and prevention of chronic pulmonary disease. AJR CCM 2011;187.
- Nohama P, Jorge RF, Valenga MH. Efeitos da estimulação diafragmática
transcutânea sincronizada em pacientes com doença pulmonar obstrutiva crônica
(DPOC): um estudo piloto. Rev Bras
Eng Bioméd
2012;28(2):103-15. https://doi.org/10.4322/rbeb.2012.018
- Cancelliero-Gaiad KM, Ike D, Costa D. Efeito da estimulação diafragmática
elétrica transcutânea em parâmetros respiratórios de pacientes com Doença
Pulmonar Obstrutiva Crônica. Fisioter Pesqui 2013;20(4):322-9.
https://doi.org/10.1590/s1809-29502013000400004
- Martinelli B, Santos
LP, Barrile SR, Iwamoto HCT, Gimenes C, Cavalcanti
RDM. Estimulação elétrica transcutânea diafragmática pela corrente russa em
portadores de DPOC. Fisioter Pesqui 2016;23(4):345-51.
https://doi.org/10.1590/1809-2950/14854823042016
- Trevisan ME, Porto AS,
Pinheiro TM. Influência do treinamento da musculatura respiratória e de membros
inferiores no desempenho funcional de indivíduos com DPOC. Fisioter
Pesqui 2010;17(3):209-13.
https://doi.org/10.1590/s1809-29502010000300004
- Elmorsi AS, Eldesoky ME, Mohsen MAA, Shalaby
NM. Effect of inspiratory muscle training on exercise performance and quality
of life in patients with chronic obstructive pulmonary disease. Egyptian
Journal of Chest Diseases and Tuberculosis 2016;65:41-6.
https://doi.org/10.1016/j.ejcdt.2015.10.006
- Beaumont
M, Mialon P, Le Ber-Moy C, Lochon
C, Péran L, Pichon R, Gut-Gobert
C, Leroyer C, Morelot-Panzini
C, Couturaud F. Inspiratory muscle training during
pulmonary rehabilitation in chronic obstructive pulmonary disease: A randomized
trial. Chron Respir Dis 2015;12(4):305-12.
https://doi.org/10.1177/1479972315594625
- Fernandes
M, Cukier A, Feltrim MI.
Efficacy of diaphragmatic breathing in patients with chronic obstructive
pulmonary disease. Chron Respir Dis 2011;8(4):237-44.
https://doi.org/10.1177/1479972311424296
- Yamaguti WP, Claudino RC, Neto AP,
Chammas MC,
Gomes AC, Salge
JM, Moriya HT, Cukier A, Carvalho CRF. Diaphragmatic
breathing training program improves abdominal motion during natural breathing
in patients with chronic obstructive pulmonary disease: a randomized controlled
trial. Arch Phys Med Rehabil 2012;93(4):571-7.
https://doi.org/10.1016/j.apmr.2011.11.026
- Cancelliero-Gaiad KM, Ike D, Pantoni CBF, Borghi SA, Costa D.
Respiratory pattern of diaphragmatic breathing and pilates
breathing in COPD subjects. Braz J Phys Ther
2014;18(4):291-9. https://doi.org/10.1590/bjpt-rbf.2014.0042
- Rocha T, Souza H,
Brandão DC, Rattes C, Ribeiro L, Campos SL, Aliverti A, de Andrade AD. The
Manual Diaphragm Release Technique improves diaphragmatic mobility, inspiratory
capacity and exercise capacity in people with chronic obstructive pulmonar y disease: a randomised
trial. J Physiother 2015;61:182-9.
https://doi.org/10.1016/j.jphys.2015.08.009
- Abdelaal Ashraf AM, Ali Mohamed
MI, Hegazy Ibrahim M. Effect of diaphragmatic and
costal manipulation on pulmonary function and functional capacity in chronic
obstructive pulmonary disease patients: Randomized controlled study. Int J Med
Res Health Sci 2015;4(4):841-847.
https://doi.org/10.5958/2319-5886.2015.00167.8
- Nair
A, Alaparthi GK, Krishnan S, Rai S, Anand R, Acharya
V, Acharya P. Comparison of diaphragmatic stretch technique and manual
diaphragm release technique on diaphragmatic excursion in chronic obstructive
pulmonary disease: a randomized crossover trial. Pulm Med
2019:1-7. https://doi.org/10.1155/2019/6364376