Rev Bras Fisiol Exerc 2021;20(1):3-16
doi: 10.33233/rbfex.v20i1.4144
RECOMMENDATIONS
General
recommendations for health care and physical activity vs. COVID-19 pandemic
Recomendações gerais de
cuidado à saúde e de prática de atividade física vs. pandemia da COVID-19
Rodrigo
Luiz Vancini1, Ana Paula Lima Leopoldo1, Luciana Carletti1,
Lucas Guimarães-Ferreira1, André Soares Leopoldo1,
Richard Diego Leite1, Natália Madalena Rinaldi1, Márcia
Regina Holanda da Cunha1, Danilo Sales Bocalini1
1Universidade Federal do Espírito Santo,
Vitória, ES, Brasil
Received:
em 20 de maio de 2020; accepted em 30 de maio de
2020.
Correspondence: Núcleo de Pesquisa e Extensão em Ciências do Movimento
Corporal (NUPEM), Centro de Educação Física e Desportos (CEFD), Universidade
Federal do Espírito Santo (UFES), Campus Universitário, Av. Fernando Ferrari,
514 Goiabeiras 29075-810 Vitória ES. nupem.cefd.ufes@hotmail.com
Rodrigo Luiz Vancini:
rodrigoluizvancini@gmail.com
Ana Paula Lima Leopoldo: ana.leopoldo@ufes.br
Luciana Carletti:
lucianacarletti@gmail.com
Lucas Guimarães-Ferreira: lgtrainer@yahoo.com.br
André Soares Leopoldo: andre.leopoldo@ufes.br
Richard Diego Leite: rdleite@gmail.com
Natália Madalena Rinaldi: natalia.rinaldi@ufes.br
Márcia Regina Holanda da Cunha: cunha.mrh@gmail.com
Danilo Sales Bocalini: bocaliniht@hotmail.com
Abstract
The Center for Research and Extension in Body Movement
Sciences (NUPEM) of CEFD/UFES, represented by professors and researchers,
jointly prepared an open letter to the community. The group saw the importance
of publishing management and strategies for maintaining physical activity and
health care and prevention during the coronavirus pandemic (COVID-19). The
pandemic has alarmed the sports community and physical activity practitioners
for its potential for transmission, dissemination, hospitalization, and
lethality, especially in more vulnerable populations, such as those with
chronic diseases and the elderly. In addition to general information about the
pandemic caused by COVID-19, the purpose of this document is to provide
information and recommendations related to the practice of physical activity
(PA) for the clarification of health professionals and people related to sport
and PA. Thus, we intend to assist in education and health promotion through
prevention strategies related to the pandemic and the practice of PA. In this
perspective, according to current guidelines, it is recommended to avoid
physical downtime and sedentary behaviors as much as possible. Still, it is
recommended to practice 150-300 min/week of moderate intensity aerobic PA and 2
sessions of activities involving muscle strength training, contributing to the
maintenance of health status. However, a lower volume of PA also produces
health benefits, that is, performing some PA is better than none and moving
more and resting less as well.
Keywords: viral disease; coronavirus;
sport; physical activity; prevention.
Resumo
O
Núcleo de Pesquisa e Extensão em Ciências do Movimento Corporal (NUPEM) do
CEFD/UFES, representado por professores e pesquisadores elaborou conjuntamente
uma carta aberta à comunidade. O grupo vislumbrou a importância de publicar
estratégias de gerenciamento e manejo para a manutenção da atividade física e
de cuidados de saúde e prevenção durante à pandemia do coronavírus(COVID-19).
A pandemia tem alarmado a comunidade esportiva e praticantes de
atividade física por seu potencial de transmissão,
disseminação, hospitalização
e letalidade, principalmente em populações mais
vulneráveis, como aquelas com
doenças crônicas e idosos. Além de
informações gerais sobre a pandemia causada
pelo COVID-19, o objetivo deste documento é fornecer
informações e recomendações
relacionadas à prática de atividade física (AF)
para o esclarecimento de
profissionais de saúde e pessoas ligadas ao esporte e da AF.
Pretendemos assim
auxiliar na educação e promoção da
saúde por meio de estratégias de prevenção
relacionadas à pandemia e à prática de atividade
física. Nesta perspectiva, de
acordo com as diretrizes atuais, recomenda-se evitar ao máximo o
tempo de
inatividade física e comportamentos sedentários. Ainda,
é recomendada a prática
de 150-300 min/semana de AF aeróbia de intensidade moderada e 2
sessões de
atividades que envolvam treinamento de força muscular,
contribuindo com a
manutenção do estado de saúde. No entanto, um
volume menor de AF produz também
benefícios à saúde, ou seja, realizar alguma AF
é melhor que nenhuma e movimentar
mais e repousar menos também.
Palavras-chave: doença viral; coronavírus;
esporte; atividade física; prevenção.
Introduction
Key points
-
COVID-19 is a major problem for public health systems and has a high potential for dissemination in sports/physical activity facilities, as these are often crowded environments.
-
The current pandemic has frightened the sports and physical activity community (health professionals, technicians, spectators, practitioners, etc). This caused a chain reaction, with cancellations of competitions and sporting events and closure of sports and physical activity facilities worldwide.
-
We must develop strategies to prevent COVID-19 infection among athletes, hobbyists, and health professionals, as well as to manage practice in a safe environment.
-
The general recommendation by different health authorities, following the guidelines of the World Health Organization (WHO), so far, has been to wash and sanitize the hands, use disinfectants (with 70% alcohol), avoid public environments and agglomerations, and social distancing. This includes the entire community, that is, both spectators and practitioners.
Problematization
According to the
World Health Organization (WHO) [1], viral diseases pose a serious problem
for local and global public health systems, as they have a high potential to
cause epidemics (regional) and pandemics (global) [1,2]. In this context, viral
infections have high potential for dissemination in physical activity and
sporting facilities (gyms, clubs, arenas, championships, and competitions) due
to close contact between people and sharing of equipment [3].
The risk for
viral infections, including that caused by COVID-19, may be elevated under the
environment’s conditions (agglomerations) and, mainly, in immunodepressed
individuals with chronic diseases [4]. Thus, older adults are more vulnerable
due to the presence of comorbidities, immunodepression, and low functional
capacity. The immunosenescence includes lower responses to vaccination, lower
ability to mediate anticancer responses, increased inflammation, tissue damage,
and loss of control of persistent infections [5]. In fact, particularly for
COVID-19, older adults are at the top of the mortality rate. According to the
WHO [1], 95% of COVID-19 deaths occurred in individuals aged 60 or older.
Furthermore, adults aged 80 or older account for 50% of all deaths. An alarming
point of data indicates that eight out of ten deaths occur in individuals with
at least one comorbidity, particularly those with cardiovascular disease,
hypertension, and diabetes, but also with several other underlying chronic
conditions.
The COVID-19
pandemic has already caused thousands of deaths in Brazil and around the world
and continues to alarm the sports community and PA practitioners for its
potential for transmission, dissemination, hospitalization, and lethality in
the most vulnerable populations.
One of the most
important conducts for the control of the pandemic, according to the most
renowned public health entities in the world [1,6], is the adoption of social
distance and avoiding crowds of people. Wilder-Smith and Freedman [7] point out
that the terms distancing, isolation and quarantine are not synonymous. Within
this context, social distancing is the minimization of interaction between
people in a community to reduce the speed of transmission of the virus since
there are asymptomatic infected individuals still unaware of the condition. In
contrast, isolation is the measure that aims to separate individuals affected
with COVID-19 (symptomatic, suspected or confirmed cases) from non-patients,
avoiding the spread of the virus. Finally, quarantine means the
separation of people, as well as the restriction of their activities, that were
probably exposed to a contagious disease, but not yet present the symptoms,
either because they have not been infected or because they are in the
incubation period. The authorities' behaviors and decisions, however, vary
according to the reality of each country, being updated dynamically [1,6]. The
period of aggressive quarantine and social isolation was gradually being
overcome with the implementation of safety and sanitary measures, such as, for
example, respecting social distance and avoiding crowds, when leaving home,
constant use of facial masks in internal and external environments, wash your
hands with soap and water and use 70% alcohol frequently and avoid putting.
By using data
obtained during previous epidemic crises, the total time of social distancing
or quarantine can be predicted, since the habits assumed during this period
have an extremely negative impact on the physical and mental health of the
population. For example, during the epidemic of severe acute respiratory
syndrome (SARS) in 2004, it was observed that people who were quarantined in
Toronto, Canada had a high prevalence of psychological problems. Data obtained
through online form [8] indicated that 28.9% and 31.2% of these people had
symptoms of post-traumatic stress disorder and depression, respectively. Recent
data already indicate that the COVID-19 pandemic is also associated with many
negative psychological consequences such as depression and anxiety disorders
[9]. Furthermore, in addition to the negative consequences on the general state
of health during the pandemic, we must also consider the economic consequences
and their future impacts.
Epidemiological aspects and the context of physical
activity and sport
The disease
caused by betacoronavirus, COVID-19, is characterized by respiratory disorder
resulting from infection and leading to SARS [10]. Initially it promotes a
typical picture of cold and flu, involving signs and symptoms such as fever,
muscle pain, nasal congestion, headache, malaise, dry cough, sputum and shortness
of breath, which are commonly mild, but may generally impair physical
performance. In the most severe cases, it may progress to pneumonia and severe
lower respiratory tract infection, which increases the risk of morbidity and
mortality, leading to the need for mechanical ventilation and hospitalization
in the Intensive Care Unit (ICU) [1,2,11].
In general,
fatal and more severe cases are associated with older people. However, younger
adults between 30 and 59 years have also become fatal victims of the disease,
especially those with comorbidities. Approximately 50% of critical cases are
people affected with cardiovascular diseases, diabetes, chronic respiratory
diseases (asthma and chronic obstructive pulmonary disease (COPD)) and
oncological diseases [2].
Although there
is still no consensus, the main hypothesis is that the first cases of COVID-19
disease were related to direct exposure of humans in the Wuhan Seafood
Wholesale Market in China [1,2]. Since then, facilitated by the large transit
of people between countries, cases of COVID-19 infection have increased
exponentially worldwide, turning into a pandemic. To prevent the spread and
transmission of the virus on a large scale, measures to control public health
infection, risk management and education and health promotion are required.
Social and economic support is also needed, as well as investments in health
and science. These actions should involve all civil society, state and federal
governments, public and private institutions, and non-governmental organizations,
with the aim of containing the outbreak and spread of the disease [1,2,6].
The pandemic
associated with COVID-19 [1,2,6] generated great concern in the international
sporting community, including associations, institutions, federations, and sports
leagues due to the potential for transmission of the virus in its events,
spaces and sports arenas. In this context, the American College of Sports
Medicine [12] officially issued a position on COVID-19. The entity points out
that:
"Personal trainers, exercise
physiologists and fitness and wellness professionals should be aware of
COVID-19 and seek information about conducts. Due to the frequency and physical
proximity with which you interact with your customers and athletes, as well as
potentially infected surfaces and materials, it is necessary to change the
conduct of physical activity practice indoors and outdoors for you and your
customers to remain safe" [12].
A letter written
by scientists toward the public, published on March 17, 2020 in the British
Journal of Sports Medicine [13] contained the following guidelines:
"If possible, exercise
outdoors! You might want to jog in rural areas if those are available. And if
you live in a city where there is no way to avoid contact with other people,
try doing a workout at home. It is important to maintain a healthy lifestyle
with regular exercise, which will benefit your immune system"[13].
Regarding this
letter [13], “exercising outdoors” might take some deliberation, as it can
increase the risk of infection by the virus.
The theme of
COVID-19 has gained prominence in the scientific community, including the
sports and physical activity community. For example, Jiménez-Pavón et al.
[14] in a recently published article, highlight the need to reduce the negative
consequences of diseases that can be amplified with social distancing and
physical inactivity, such as diabetes, hypertension, cardiovascular and
respiratory diseases, and also the changes inherent to aging, such as
sarcopenia, dementia and psychological effects. They also encourage the
practice of physical exercises, even if it is not possible to meet the minimum
proposed in the prescription guidelines [14].
Considering this
change in everyday life worldwide as a result of COVID-19, Hall et al.
[15] suggest that this health crisis has a relevant impact on the pandemic of
physical inactivity and sedentary behavior, since we have not resolved this
issue for several years. The authors also question whether the pandemic is
making the world's population move less, and the answer to that question is
yes. It is noteworthy that there is no literature that evaluated the lasting
effect of pandemics on physical practice and sedentary behavior.
Another relevant
aspect is that positive efforts to keep the individual physically active should
continue during the COVID-19 pandemic, however researchers highlight the
concern with individuals who have not previously been involved in a regular
exercise routine and have a sedentary lifestyle. The study [15] suggests that
they are unlikely to increase their daily physical activity during the pandemic
and, in fact, may be moving less than before. This situation can generate a
cycle in which current patterns of physical inactivity as well as sedentary
behavior can worsen the impact of future pandemics [15].
What to do?
From the
perspective of public health management, the main concern has been with the
acceleration of COVID-19 transmission. This is because it has the potential to
collapse the health system, so that people could die due to the impossibility
of medical intervention, including other diseases or traumas. This has happened
around the world. In this sense, the collective effort to stop this propagation
is fundamental.
Places with
circulation of many people such as airports, shopping malls, gymnasiums and
educational institutions (such as Universities and Schools), as well as
cultural and sporting events held mainly indoors (and involving health
professionals and practitioners) have high transmission potential, due to
crowding and close contact between people.
Given the
proportion and effects (number of infected, hospitalizations and deaths) of the
current pandemic, the recommendations for social distancing have been radical.
In principle, during the first wave of transmission of the virus, the
recommendation has been adopted to leave home only when extremely necessary
[1]. However, the information and guidelines are updated daily. Therefore, it
is important to frequently monitor the positioning of respected entities, that
is, those that have a scientific advisory body. In addition, it is important to
emphasize that the distancing effort may postpone the peak of the pandemic to
autumn, with consequent increase in transmissibility in the winter [16].
Precautionary and hygiene measures
There are
essential measures for infection prevention and control that should be
implemented by all professionals working in community services avoiding or even
reducing the transmission of microorganisms, mainly because there are still no
vaccines or antiviral drugs specific to the treatment of COVID-19 [1,2].
Therefore, it is necessary for our community to be guided towards precautionary
measures and safe use of personal protective equipment, in order to prevent the
spread of the disease, in addition to preventing the transmission of the virus
in infected people, with or without symptoms.
As for
dissemination, it is known, to date, that the new coronavirus is transmitted
through droplets that are expelled during speech, coughs or sneezes, direct
contact with infected people or even by indirect contact through the hands. In
addition, contact with contaminated objects or surfaces can then generate
contact with the mouth, nose or eyes, in a very similar way to the spread that
occurs in other diseases transmitted by the airway (influenza, diphtheria,
tuberculosis). In this sense, both PAHO and WHO [1] as well as other
organizations issued the following general prevention recommendations:
-
Wash your hands using soap and water or alcohol-based sanitizer (70%), frequently, especially after contact with infected people or the environment to eliminate microorganisms that may be in your hands; repeat this act before coming into contact with the mucous regions of the body, such as the mouth, eyes and nose;
-
Make sure that you and the people around you follow good respiratory hygiene. This means covering the mouth and nose with the inner part of the elbow or with a tissue when coughing or sneezing (then discard the used handkerchief immediately) and washing your hands afterwards. When someone coughs or sneezes, liquid droplets are sprayed from the nose and/or mouth, possibly containing the virus.
-
When leaving home, keep at least an one-meter distance between you and anyone else; people with symptoms of acute airway infection should keep away from other people and redouble care with hand washing in addition to using masks, to prevent the spread of viral particles;
-
The use of disposable surgical masks is indicated for people with respiratory symptoms (cough or difficulty breathing), as well as for health professionals who provide care to individuals with respiratory symptoms. Regarding surgical masks, proper use and disposal are essential to ensure its effectiveness and avoid increased risk of transmission associated with incorrect practices.
-
Stay at home if you have a fever (temperature above 37.5°C); if you have a cough and difficulty breathing, seek medical attention.
-
Travelers returning from affected areas should monitor their symptoms for 14 days and follow the national protocols of the receiving countries; and if symptoms occur, they should contact a doctor and report on their travel history and symptoms.
-
Avoid unprotected contact with farm animals or wild animals.
-
There is no evidence that domestic animals can transmit the disease to humans, but it is recommended to isolate them when contamination is suspected or avoid contact with the animal when the owner is contaminated.
-
Current evidence suggests that the new coronavirus may remain viable for hours and even days on certain surfaces, depending on the type of material. Therefore, the cleaning of objects and surfaces, followed by disinfection, are recommended measures for the prevention of COVID-19 and other viral respiratory diseases in community environments.
According to
technical note 34/2020 of ANVISA [17], for the disinfection of external
environments, it is correct to use alcohol 70% in addition to products based on
sodium or calcium hypochlorite, at a concentration of 0.5%. Commercial bleach
has a sodium hypochlorite concentration between 2.0 and 2.5% and is a toxic
product in contact with eyes or skin. It is interesting to note that this
chemical is unstable after dilution and can be deactivated by light, so care is
recommended in its handling and immediate use after dilution. It should not be
mixed with other products, as sodium hypochlorite can react violently with many
chemical substances, producing toxic compounds or even losing its effectiveness
as a disinfectant [17,18].
What can physical activity and exercise do for people?
Although the
association between physical inactivity and mortality be a consensus recognized
worldwide, according to recent data 31% of individuals aged 15 years or older
are physically inactive and approximately 3.2 million deaths per year are
attributed to this harmful behavior to the lifestyle and the practice of
physical activity in leisure time could change this scenario [19]. Although
social distancing in a specific context of viral pandemic is temporary, we
understand that it is important to raise awareness about physical inactivity
and sedentary behavior. In this sense, there is evidence that links high risk
of chronic diseases when the individual is physically inactive, with consequent
sedentary lifestyle [20,21,22].
Although
there is no direct evidence, there is an assumption that people who exercise
regularly may be less vulnerable to viral diseases, since non-communicable
diseases (obesity, hypertension, diabetes, etc) and risk factors associated
with lifestyle (physical inactivity and smoking) are less prevalent in physical
practitioners. Furthermore, generalized physical exercise for the older
population promotes improvements in physical function, as well as in the
cognitive aspects [23,24].
Systematic
physical practice can complement therapy for a variety of chronic diseases,
including cardiovascular diseases, neurological and psychiatric disorders,
metabolic syndrome, oncological and respiratory diseases [25]. In addition,
there is a lot of scientific evidence available indicating that the practice of
regular physical exercise, mainly of moderate intensity, has a positive effect
on immunity [26,27,28,29]. It is also worth mentioning in this context that older
people apparently benefit more than young people in relation to protection
against all-cause mortality and some diseases [30,31,32], although we do not have
evidence in relation to COVID-19. Mazioli et al. [33] demonstrated that
in addition to presenting better immune response, mice submitted to regular
physical exercise (30 min/day) with moderate intensity had a lower mortality
rate after infection with influenza virus. However, long-term physical exercise
(approximately 2.5h/day) resulted in more severe symptoms, with no influence on
mortality when compared to sedentary animals. The same researchers found that
in humans, moderate physical activity prolongs the protective effect of annual
vaccination against influenza virus. However, no studies have yet been found
with COVID-19 to confirm the transposition of these results.
Although there
is still no research on COVID-19, in other respiratory tract disorders (e.g.,
asthma and COPD) the practice of moderate physical exercise has a positive
impact on immunity, besides being associated with the adoption of other
positive life habits, such as adequate sleep, reduced alcohol intake, smoking
cessation and adequate nutrition and hydration [26,27,29]. In addition, the
current literature shows that moderate physical activity improves the function
of defense cells, reducing the risk of infectious diseases as well as
increasing stress hormones with consequent reduction of excessive inflammation
[34]. Thus, individuals who perform moderate levels of physical activity in
their daily life have a 20-30% reduction in upper respiratory tract infections.
However, prolonged high-intensity physical activity can lead to impaired immune
system, leading to increased susceptibility to infections [34,35,36].
General recommendations for the practice of physical
activity during the COVID-19 pandemic
Given the
difficulty of individualizing the orientation of physical activity at the moment,
the general and conservative recommendation of physical practice may be those
presented by the WHO [1], the American College of Sports Medicine (ACSM) [12]
and the Brazilian Society of Sports Medicine (SBME) [36,37]. Figure 1
summarizes the main actions to be taken during the pandemic.
These documents
recommend 150-300 min per week of aerobic exercise (e.g., walking indoors and
stationary cycling) of moderate intensity and two sessions of activities
involving muscle strength training. In addition, they recommend avoiding
physical downtime and sedentary behaviors such as sitting, using a mobile
device or watching TV for a long time.
The guidance for
moderate PA is based on the fact that this type of modality improves /
preserves the general health status, including the improvement of immunity, and
the reduction of anxiety and emotional stress, very common in the condition of
social distance and isolation. Thus, domestic programs using safe, simple and
easily implementable exercises are suitable to preserve fitness levels,
including aerobic exercises (walking indoors), strengthening, stretching and
balancing, or combinations of these [38,39]. On the other hand, intense
physical exercise can be harmful to health depending on the profile of the
practitioner and the level of intensity [39,40].
With the closure
of gyms and clubs, individuals involved in strength training programs were
unable to access a wide variety of equipment, dumbbells and weights. In the
home environment, access to equipment and a variety of weights is restricted to
most of the population. Thus, the use of smaller loads, using dumbbells,
elastic bands and the weight of the body itself, for example, become valid
alternatives. Kikuchi and Nakazato [40] demonstrated that a training program
using exercise with the weight of one's own body (push-ups) with a load
proportional to 40% of 1RM resulted in a significant increase in strength.
Therefore, it is
recommended that during the period of social distancing, individuals adapt
their strength training programs using low-cost equipment such as furniture and
household items as well as the weight of the body itself [14].
Considering the
declarations of health agencies, so far, we can highlight the following
practical guidelines [1,6].
-
The regular practice of physical exercise/physical activity is associated with improved immune function in humans, optimizing the body in the fight against infectious agents. Although there is no evidence of this improvement with the fight against COVID-19, an optimized immune system could fight infectious agents.
-
Physically active individuals have lower risk in the development of chronic non-communicable diseases.
-
Older adults, at higher risk, should be encouraged to maintain active habits, especially in an adapted fashion considering the place of practice, as well as social relations.
-
The recommendations of the WHO and the Brazilian Ministry of Health point out that people should avoid staying indoors with large amount of people, especially in gyms, sports clubs and the like.
-
The possibility of outdoor physical activity should consider guidelines from the Ministry of Health and municipal, state and federal governments, given the risk of contamination among people; and the minimum social distancing, according to the modality practiced. According to the WHO, in the case of cycling or walking outdoors, always practice physical distance and wash your hands with soap and water before leaving, when you get to where you are going and as soon as you get home. If soap and water are not available immediately, alcohol-based cleaning products are recommended.
-
There are no recommendations now regarding limitation of physical activity if you are asymptomatic, however, do not exercise if you have fever, cough and difficulty breathing. Stay at home and rest and seek medical attention. Follow the instructions of your local health authority.
-
Everyone should be careful with exercises of high intensity and volume, it can impair the immune system, especially of individuals not yet accustomed.
-
Engage in activities in which children and the family, who are living in the same environment of social distancing, can participate simultaneously.
-
If you are not regularly active, start with low intensity activities such as walking and low-impact exercises. Start with amounts of short exercises, such as 5 to 10 minutes, and gradually increase up to 30 minutes or more during the weeks. It is better and safer to stay active for short periods more often than trying to stay active for long periods when you are not adapted.
-
Sports activities such as interactive video games (EXERGAMES – dance games, for example) and walking in the home environment are recommended.
-
It is noteworthy that quarantined individuals (with a positive diagnosis for the disease) should remain in complete isolation to avoid the spread of the virus. This disease still has unknown repercussions that can lead to the development of cardiac and pulmonary complications; as such, individuals presenting symptoms should refrain from physical activity until complete recovery.
-
It is important to raise awareness not only of hygiene, but of all parameters of self-care.
-
Try to reduce your sitting, lying or motionless time, i.e. sedentary habits. Take advantage of the architecture (e.g. stairs) and furniture of the residence as tools to assist physical activity.
Are we going to move during the pandemic and social
distance?
Use your free time
to move around, avoiding sedentary behaviors. Some specific strategies:
-
Perform indoor activities (work and domestic) while listening to music. Take the opportunity to experience dances in general, climb stairs frequently, (two to three times daily, 10 to 15 minutes), skip rope - as long as you have no osteomyoarticular and/or cardiac problems. In these cases, appropriate recommendation and medical follow-up are necessary.
-
Watch interactive videos on social networks; but remember, consider their functional limitations, as well as the intensity recommended by institutions with scientific support. In this sense, try to interact with materials that are guided by health professionals and entities. Consult before choosing for more safety.
-
If you have equipment such as treadmills and stationary bikes it is a great opportunity to use them.
-
Muscle strength activities using dumbbells, free weights, elastic bands, or the body weight itself are good options. But be prudent and be careful. Pay attention to the correct posture and technique during the execution of the movements.
-
Consider activities renowned for reducing anxiety and depression (alternative therapies) such as meditation, yoga, tai chi and lian gong.
-
The recommendation of outdoors practices such as walking, running, and biking is still relevant for the better functioning of the immune system and general health. However, current recommendations are to avoid indoor activities (gyms) and take care in the practice of outdoor activities (walking and running in outdoor environments should respect the social distance) to prevent local and community transmission of the virus and not to overload local health systems;
-
Pay attention to the situation in your city, as in some places there are local rules for all citizens and rules regarding the use of indoor and outdoor environments.
-
Additionally, we recommend gardening in general; in rural areas or even in the urban environment, if possible, stimulated mainly among the older population.
-
Household chores are welcome to increase energy expenditure (laundry, sweeping the house etc.).
-
If you have difficulty performing the activities yourself, seek health professionals.
-
If you want to develop a specific physical exercise program, contact a Physical Education professional. It is worth noting that the Federal Council of Physical Education allows Physical Education teachers to work through an online consulting service. This can represent a great opportunity for accompaniment by a trained professional, even during the period of social distance and isolation and in the impossibility of crowds of people as it happens in gyms. However, PA practice sites have instituted safety measures (distance of at least 1 meter between practitioners) and sanitary measures (use of face masks and 70% alcohol) in order to make the use of spaces safer.
In this context,
there are national and international scientific approaches and reflections on
the recommendations of physical exercise in the domestic environment during the
period of social distancing. The guidelines aim to improve adherence and
maintenance of physical exercise programs and to contribute to the promotion of
health during the COVID-19 pandemic and the necessary measures of social
distance and avoiding crowds. Jiménez-Pavón et al. [14] point out that
if possible, considering the reduction in the level of physical activity caused
by social distancing, the weekly volume of physical exercise should be raised
to about 200 to 400 min, 5 to 7 days a week. In addition, Oliveira Neto et
al. [41] suggested a model of prescription of physical exercise in a
domestic environment of strength exercises (strength training program based on
calisthenics) for the main muscle groups. The authors also guide the use of
tools that allow monitoring the quantity and quality of physical exertion
(subjective effort perception scale), as well as personal satisfaction (scale
of sensation and motivation for practice).
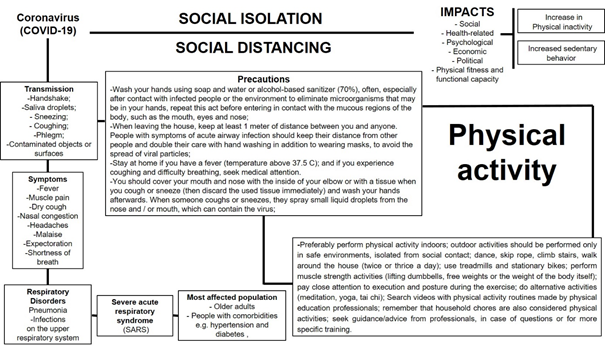
Figure 1 - General recommendations for
healthcare and physical activity
Conclusion
Taking into
account the current scenario, the best strategy to reduce community
transmission during the COVID-19 pandemic still continues to respect social
distancing and sanitary measures (wearing face masks, washing hands and hygiene
with alcohol 70% frequently).
Thus, promotion
of prevention strategies and dissemination of accurate information are
necessary to prevent infection by the disease among athletes, physical activity
practitioners, health professionals and other people involved in the context.
It is important to stimulate physical activity as well as the reduction of
sedentary behavior during this delicate period. The guidelines for the practice
of physical exercises should be available to the population, while respecting
the guidelines of social distancing.
This article
brought some practical recommendations, supported by scientific evidence and
aiming at health promotion and attenuation of injuries associated with sedentary
behavior. It is also necessary to reinforce that the general hygiene
recommendation involves: washing hands with soap and water frequently; using
hand sanitizer (alcohol 70%); avoiding hand-to-face contact after interacting
with a potentially contaminated environment; respecting the minimum distance of
2m when in establishments classified as essential, including supermarkets and
pharmacies. Therefore, it is time to stay alert and follow the guidelines of
public and health authorities.
Acknowledgments
The authors RLV, NMR, DSB thank CNPQ and FAPES for
their support. To all health professionals and scientists who donate their
knowledge and experience to save lives. To all people, victims, patients,
family, parents, friends... who have lost loved ones. RLV is a productive fellowship at the
Fundação de Amparo à Pesquisa e Inovação do Espírito Santo (FAPES) agency
(Edital Nº 18/2018-Bolsa Pesquisador Capixaba).
Conflict of interest
The authors declare no conflict of interest.
Funding
National Council for scientific and technological
Development (CNPq) and Espirito Santo Research and Innovation Support
Foundation (FAPES)
Authorial contribution
All authors participated equally in the writing,
analysis, and publication of the document.
- World Health Organization (WHO). Coronavirus disease
(COVID-2019) situation reports. [cited
2020 Mar 17]. Available from:
https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports
- Cascella M, Rajnik M, Cuomo A, Dulebohn SC,
Di Napoli R. Features, evaluation and treatment coronavirus (COVID-19). Book chapter.
[cited 2020 Mar 19]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554776/
- Halabchi F,
Ahmadinejad Z, Selk-Ghaffari M. COVID-19 Epidemic:
exercise or not to exercise; that is the question! Asian J Sports Med 2020;11(1):e102630.
- Al-Hazmi A. Challenges
presented by MERS corona virus, and SARS corona virus to global health. Saudi J
Biol Sci 2016;23: 507-11. doi: 10.1016/j.sjbs.2016.02.019 [Crossref]
- Pawelec G. Age and immunity: What is "immunosenescence"? Exp Gerontol 2018;105:4-9. doi: 10.1016/j.exger.2017.10.024 [Crossref]
- Center for Disease Control and Prevention (CDC). How
to protect yourself. [cited 2020 Mar 18]. Available from:
https://www.cdc.gov/coronavirus/2019-ncov/prepare/prevention.html
- Wilder-Smith A, Freedman DO. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med 2020;27(2). doi: 10.1093/jtm/taaa020 [Crossref]
- Hawryluck L,
Gold WL, Robinson S, Pogorski S, Galea S, Styra R. SARS control and psychological effects of
quarantine, Toronto, Canada. Emerg Infect Dis
2004;10(7):1206-12.
- Li S, Wang Y, Xue J, Zhao N,
Zhu T. The impact of COVID-19 epidemic declaration on psychological
consequences: a study on active weibo users. Int J
Environ Res Public Health 2020;17:E2032
- Sohrabi C, Alsafib Z, O'Neilla Z, Kerwanc KA, Iosifidisa AAC, Aghad R. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19). Int J Surg 2020;76:71-6. doi: 10.1016/j.ijsu.2020.02.034 [Crossref]
- Van den Brand JM, Smits SL, Haagmans BL. Pathogenesis of Middle East respiratory syndrome coronavirus. J Pathol 2015;235:175-84. doi: 10.1002/path.4458 [Crossref]
- American College of Sports Medicine (ACSM). Personal
Trainers, Fitness Professionals and the Coronavirus
(COVID-19). [cited 2020
Mar 20]. Disponível:
https://www.acsm.org/read-research/newsroom/news-releases/news-detail/2020/03/09/personal-trainers-fitness-professionals-and-the-coronavirus-COVID-19
- British Journal of Sports Medicine (BJSM). Exercise
and Infectious Diseases Covid-19. [cited
2020 Marc 21]. Available from::
https://blogs.bmj.com/bjsm/2020/03/17/exercise-and-infectious-diseases-covid-19/
- Jiménez-Pavón D, Carbonell-Baeza A, Lavie CJ. Physical exercise as therapy to fight against the mental and physical consequences of COVID-19 quarantine: Special focus in older people. Prog Cardiovasc Dis 2020;63(3):386-88. doi: 10.1016/j.pcad.2020.03.009 [Crossref]
- Hall G, Laddu DR, Phillips SA, Lavie CJ, Arena R. A tale of two pandemics: How will COVID-19 and global trends in physical inactivity and sedentary behavior affect one another? Prog Cardiovasc Dis 2020; S0033-0620:30077-3. doi: 10.1016/j.pcad.2020.04.005 [Crossref]
- Kissler S, Tedijano C, Lipsitch M, Grad Y.
Social distancing strategies for curbing the COVID-19 epidemic. 2020.
http://dash.harvard.edu/handle/1/42638988
- Nota
técnica Nº 34/2020 SEI/COSAN/GHCOS/DIRE3/ANVISA
- Nota
técnica Nº 04/2020 GVIMS/GGTES/ANVISA
- Lee DC, Pate RR, Lavie CJ,
Sui X, Church TS, Blair SN. Leisure-time running reduces all-cause and
cardiovascular mortality risk. J Am Coll Cardiol
2014;64(5):472-81.
- Wen CP, Wu X. Stressing harms of physical inactivity to promote exercise. Lancet 2012;380(9838):192-3. doi: 10.1016/S0140-6736(12)60954-4 [Crossref]
- Pratt M, Ramirez Varela A, Salvo D, Kohl III HW, Ding D. Attacking the pandemic of physical inactivity: what is holding us back? British J Sport Med 2019. doi: 10.1136/bjsports-2019-101392 [Crossref]
- Bauer UE, Briss PA, Goodman RA, Bowman BA. Prevention of chronic disease in the 21st century: elimination of the leading preventable causes of premature death and disability in the USA. Lancet 2014;384(9937):45-52. doi: 10.1016/S0140-6736(14)60648-6 [Crossref]
- Booth FW, Roberts CK, Thyfault JP, Ruegsegger GN, Toedebusch RG. Role of inactivity in chronic diseases: evolutionary insight and pathophysiological mechanisms. Physiol Rev 2017;97:1351-402. doi: 10.1152/physrev.00019.2016 [Crossref]
- Lavie CJ, Ozemek C, Carbone S, Katzmarzyk PT, Blair SN. Sedentary behavior, exercise, and cardiovascular health. Circulation Research 2019;124(5):799-815. doi: 10.1161/CIRCRESAHA.118.312669 [Crossref]
- Falck RS, Davis JC, Best JR, Crockett RA, Liu-Ambrose T. Impact of exercise training on physical and cognitive function among older adults: a systematic review and meta-analysis. Neurobiol Aging 2019;79:119-30. doi: 10.1016/j.neurobiolaging.2019.03.007 [Crossref]
- Pedersen BK, Saltin B. Exercise as medicine - evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand J Med Sci Sports 2015;25 Suppl 3:1-72. doi: 10.1111/sms.12581 [Crossref]
- Simpson RJ, Kunz H, Agha N, Graff R. Exercise and the regulation of immune functions. Prog Mol Biol Transl Sci 2015;135:355-80. doi: 10.1016/bs.pmbts.2015.08.001 [Crossref]
- Roberts JA. Viral illnesses and sports performance. Sports Med 1986;3:298-303. doi: 10.2165/00007256-198603040-00006 [Crossref]
- Paffenbarger Junior RS, Hyde RT, Wing AL, Hsieh CC. Physical activity, all-cause mortality, and longevity of college alumni. N Engl J Med 1986;6(314):605-13. doi: 10.1056/NEJM198603063141003 [Crossref]
- Löllgen H, Böckenhoff A, Knapp G. Physical activity and all-cause mortality: an updated meta-analysis with different intensity categories. Int J Sports Med 2009;3:213-24. doi: 10.1055/s-0028-1128150 [Crossref]
- Samitz G,
Egger M, Zwahlen M. Domains of physical activity
and all-cause mortality: systematic review and dose–response meta-analysis of cohort
studies. Int J Epidemiol 2011;5:1382-400. doi: 10.1093/ije/dyr112 [Crossref]
- Mazioli RCF, Santos JP, Silva VL, Lunz W, Perez AJ, Lima-Leopoldo AP, et al. Marcadores hematológicos de corredores amadores do município de Vitória/ES. ConScientiae Saúde 2015;14(3):394-401. doi: 10.5585/conssaude.v14n3.5772 [Crossref]
- Harris MD. Infectious disease in athletes. Curr Sports Med Rep 2011;10(2):84-9. doi: 10.1249/JSR.0b013e3182142381 [Crossref]
- Ahmadinejad Z, Alijani N, Mansori S, Ziaee V. Common sports-related infections: a review on clinical pictures, management and time to return to sports. Asian J Sports Med 2014;5(1):1-9. doi: 10.5812/asjsm.34174 [Crossref]
- Sociedade
Brasileira de Medicina do Esporte. Informe da Sociedade Brasileira de Medicina
do Exercício e do Esporte (SBMEE) sobre exercício físico e o coronavírus (COVID-19). [cited 2020 Mar 24]. Available from:
http://www.medicinadoesporte.org.br/wp-content/uploads/2020/03/sbmee_covid19_final.pdf
- Sociedade Brasileira de Medicina do Esporte. Informe 2 da Sociedade Brasileira de Medicina do Exercício e do Esporte (SBMEE) sobre exercício físico e o coronavírus (COVID-19). [cited 2020 mar 24]. Available from: http://www.medicinadoesporte.org.br/wp-content/uploads/2020/03/sbmee_covid_informe2.pdf
- Chen P, Mao L, Nassis GP,
Harmer P, Ainsworth BE, Li F. Wuhan coronavirus (2019-nCoV): The need to
maintain regular physical activity while taking precautions. J Sport Health
Sci 2020;9(2):103-4.
- Lavie CJ, O’Keefe JH, Sallis RE. Exercise and the heart - the harm of too little and too much. Curr Sports Med Rep 2015;14(2):104-9. doi: 10.1249/JSR.0000000000000134 [Crossref]
- Schnohr P, O'Keefe JH, Marott JL, Lange P, Jensen GB. Dose of jogging and long-term mortality: the Copenhagen City Heart Study. J Am Coll Cardiol 2015;10(65):411-9. doi: 10.1016/j.jacc.2014.11.023 [Crossref]
- Kikuchi N, Nakazato K. Low-load bench press and push-up induce similar muscle hypertrophy and strength gain. Journal of Exercise Science and Fitness 2017;15(1):37-42. doi: 10.1016/j.jesf.2017.06.003 [Crossref]
- Oliveira Neto L, Elsangedy HM, Tavares VDO, Teixeira CVLS, Behm DG, Silva-Grigoletto ME. Training at home during the COVID-19 (SARS-COV2) pandemic: physical exercise and behavior-based approach. Rev Bras Fisiol Exerc 2020;19(2):S9-S19. doi: 10.33233/rbfe.v19i2.4006 [Crossref]