Rev Bras Fisiol Exerc 2020;19(4):301-11
doi: 10.33233/rbfex.v19i4.4249
REVIEW
Exercise
as early mobilization in patients using vasoactive drugs
Exercício como
mobilização precoce em pacientes com uso de drogas vasoativas
Amanda Mariano Morais1,
Daiane Naiara da Penha1, Danila Gonçalves
Costa1,
1Hospital e Maternidade
São Cristóvão, São Paulo, SP, Brasil
2Hospital ENCORE,
Aparecida de Goiânia, GO, Brasil
Received
on: July 5, 2020; Accepted on: August 10, 2020.
Corresponding author: Giulliano
Gardenghi, Rua Gurupi, Quadra 25, Lote 6 a 8 Vila
Brasília 74905-350 Aparecida de Goiânia GO, Brasil
Amanda Mariano Morais:
amanda.c.mariana@hotmail.com
Daiane Naiara da Penha:
daianepnaiara@gmail.com
Danila Gonçalves Costa: dgoncalves081@gmail.com
Vanessa Beatriz
Aparecida Fontes Schweling:
vanessafontes.fisio@gmail.com
Jaqueline Aparecida
Almeida Spadari: jaque.spadari@gmail.com
Giulliano Gardenghi:
ggardenghi@encore.com.br
Abstract
Introduction:
The functional benefits of Early Mobilization (EM) capable of
minimizing limitations and deformities are obvious, but many
barriers exist to conduct EM as a routine practice in the Intensive
Care Unit (ICU), including the use of vasoactive drugs
(VAD), directly related to weakness acquired in the ICU, in
addition to the resistance
of the multidisciplinary team to mobilize the patient using VAD. Objective:
The objective of this review was to raise a scientific basis in the
management of critically ill patients using VADs for EM in the ICU. Methods: This
is an integrative review, with research in the databases PEDro, Pubmed, Lilacs of
articles published between 2011 and 2018, in Portuguese and English, using the
terms: vasoactive drugs, early mobility, exercise in UCI, vasopressor and its
equivalents in Portuguese. Results: Nine studies were included that
analyzed the EM intervention in patients using VAD, with or without ventilatory
support. There was no homogeneous treatment among the researched works, varying
between exercises in bed and outside, with passive and/or active action.
However, regardless of the conduct, the
cardiovascular response improved without relevant changes regarding the use of VAD. Conclusion:
EM is not contraindicated for patients in the ICU with use of VAD, and
is effective and safe without promoting relevant hemodynamic and
cardiorespiratory changes, which would determine its absolute
contraindication.
Keywords: vasodilator agents; early ambulation; intensive care units; physical
therapy specialty.
Resumo
Introdução: São claros os
benefícios funcionais da mobilização precoce (MP) capaz de minimizar limitações
e deformidades diante do imobilismo, porém são muitas as barreiras para
conduzir a MP como prática de rotina na unidade de terapia intensiva (UTI), entre
elas, o uso de drogas vasoativas (DVA), visto que está diretamente relacionado
à fraqueza adquirida na UTI, além da presença da resistência da equipe
multidisciplinar em mobilizar o paciente em uso de DVA. Objetivo: O
objetivo desta revisão de literatura é levantar embasamento científico no
manejo do paciente crítico em uso de DVA para MP em UTI. Métodos: É uma
revisão integrativa da literatura, com pesquisa nas bases de dados: PEDro, Pubmed, Lilacs, com artigos publicados entre 2011 e 2018, em
português e inglês, utilizando os termos: vasoactive drugs, early mobility,
exercise in ICU, vasopressor e seus equivalentes em português.
Resultados: Foram incluídos nove trabalhos que analisaram a intervenção
de MP em pacientes com uso de DVA, com ou sem suporte ventilatório. Não houve
um tratamento homogêneo entre os trabalhos pesquisados, variando entre
exercícios no leito e fora, de ação passiva e/ou ativa. Porém, independente da
conduta, houve melhora da resposta cardiovascular sem alterações relevantes quanto
ao uso da DVA. Conclusão: A MP não é contraindicada para pacientes em
UTI com uso de DVA e mostrou-se eficaz e segura sem promover alterações
hemodinâmicas e cardiorrespiratórias relevantes, que determinassem sua
contraindicação absoluta.
Palavras-chave: vasodilatadores;
deambulação precoce; unidades de terapia intensiva; Fisioterapia.
Introduction
Early mobilization (EM) is understood to mean physical therapy performed
on the critical patient, in the first 48 hours of an installed disease, as a process
of improving functionality and reducing time in Intensive Care Units (ICU)
[1,2].
The functional benefits of EM are clear [3], capable of minimizing
limitations and deformities [3-5]. It has better results when started early
[4], with a positive effect on improving quality of life and longevity after
discharge [6].
The prolonged stay in the ICU is associated with bed immobilization,
which is responsible for the development of weakness acquired in the ICU due to
the loss of skeletal muscle of 1-1.5% per day at rest [3,7] this loss may reach
3% [8] and still last for five years after hospital discharge [5,7]. Even with
these data, immobility is considered a public health problem, since less than
10% of critical patients in Brazil are mobilized in a hospital environment,
which impacts on the increase comorbidities and mortality [3,9].
Because it is little practiced, there are few national studies that
demonstrate such a practice [9-11], however we know that patients who are most
commonly mobilized early, are on mechanical ventilation [1,2,4-6,8,10-13], and
a part, under the effect of several medications, due to the severity of the
clinical scenario. In agreement with this data, in the United States of America
it was observed that non-mechanically ventilated patients were less likely to
be mobilized and, in addition, the exercises performed were limited to the bed
[14].
There are many barriers to conduct EM as a routine practice in the ICU,
ranging from the poorly prepared and untrained multiprofessional
team, lack of equipment, instability of the patient's clinical condition,
sedation and use of vasoactive drugs (VADs), and it is also necessary constant
monitoring of hemodynamic repercussions. [7,15]
The literature states that VADs are among the most widely used drugs in
all intensive care centers [16]. Many critically ill patients use these to
optimize cardiac output and systemic and pulmonary vascular tone, due to their
peripheral, pulmonary, cardiac and renal effects, with vasoconstriction,
inotropism, chronotropism, bronchodilation and others. They can reestablish
blood flow in vital organs in states of circulatory shock [17-19] for having
fast and powerful action, improving the prognosis and survival of patients.
However, the use of VADs is associated with weakness acquired in the ICU
regardless of other factors, so that this loss of muscle strength will be more
pronounced when associated with bed immobilization. Therefore, it should be
used with caution and with hemodynamic and laboratory monitoring [20,21]
because the response in alpha and beta receptors is directly related to the
dose applied [19,21].
Resistance is perceived among physicians regarding the mobilization of
patients using mechanical ventilation and drugs (sedation and vasoactive),
which we fear often extends to the multidisciplinary team [5,22,23]. They use
the risk of changes as a justification to the risk of cardiovascular criteria
(mean arterial pressure, cardiac output and blood flow), since during EM there
is an increase in oxygen consumption due to muscle activation, which can result
in adverse events, especially if the team is not adequately prepared to perform
this procedure [23].
A better understanding of the risks when mobilizing patients who are
using VADs can reduce the distance between research and clinical practice.
Having knowledge of the barriers that imply in performing EM and the
concomitant use of VADs, the purpose of this literature review is to raise
scientific basis in the management of critically ill patients using VADs for EM
in the ICU.
Methods
This study is an integrative literature review and research was carried
out through the databases: PEDro, Pubmed,
Lilacs, with articles published between 2011 and 2018, in Portuguese and
English, using the terms: vasoactive drugs, early mobility, exercise in ICU,
vasopressor and its equivalents in Portuguese. The articles were evaluated
according to the recommendation of “Oxford Center for Evidence-Based Medicine”:
A) Systematic review (with homogeneity) of controlled and randomized clinical
trials. Controlled and randomized clinical trial with narrow confidence
interval. Therapeutic results of the “all or nothing” type; B) Systematic
review (with homogeneity) of cohort studies. Cohort study (including randomized
trial of lower quality). Observation of therapeutic results / Ecological study.
Systematic review (with homogeneity) of case-control studies. Case-control
study; C) Case reports (including lower quality cohort or case-control); D)
Expert opinion without critical evaluation or based on basic subjects
(physiological study or study with animals). In all the databases consulted, 63
articles were found and only nine were selected that fit the inclusion criteria,
who underwent motor physiotherapeutic intervention in patients using VADs.
Narrative / integrative or systematic review articles and studies that did not
make clear the use of VADs were excluded. The selection flowchart follows
below, in figure 1.
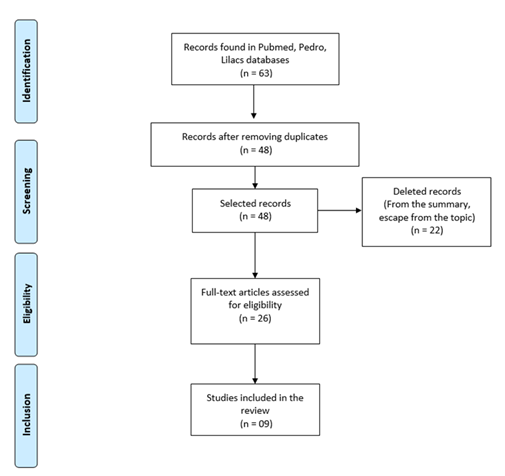
Figure
1 - Flowchart for selecting articles
Results
Nine articles were included, where patients were submitted to physical
therapy intervention, with or without the use of VADs, with constant
hemodynamic monitoring.
The results obtained through the selected studies are shown in tables I
and II. Table I shows the name of the author, year of publication, the degree
of evidence, the objective of the study and the conclusion obtained through the
observed results. Table II shows the name of the author, year of publication,
the sample of patients with their respective distribution and the
physiotherapeutic intervention. It is important to note that the interventions
described in Table II were different, but all were performed in a hospital environment.
The results show that the use of VADs was not an obstacle to the performance of
EM, as they did not cause hemodynamic instability, in addition to potentially
improving the cardiovascular response to muscle activation. In addition, there
were no adverse events that required an increase in the dose of VADs, showing,
therefore, that their presence is not a contraindication for physical therapy
interventions.
Table
II - Sample of patients with respective distribution
in groups and type of intervention performed on a patient using VAD. (ver Anexo em PDF)
Discussion
The literary survey carried out and demonstrated in the results provided
evidence that EM in the ICU, in the presence of VADs, can be a safe alternative
in the care of critical patients, seeking to minimize the negative repercussions
of bed immobilization.
The consensus of experts published in 2014 by Hodgson et al. [29]
was unable to reach an agreement regarding the dose of VADs that can be
considered safe to initiate early mobilization. However, Boyd et al.
[25] evaluated the safety limits for exercise in intensive care units in
patients using VADs, based on the same system of signs and colors as the
consensus mentioned above, in which green means low risk of adverse events,
yellow, when there are risks for mobilization, but the benefits overlap risks
as long as the team is qualified and trained in the processes and red, when
there is a potential risk of adverse events with serious consequences. In this
prospective cohort study, there were 91 patients, and the authors recorded the
most advanced form of exercise (that is, the exercise with the greatest muscle
activation) used each day, defining active exercises performed in or out of bed
as rehabilitation exercises. VADs were categorized, according to individual
dose, into low, moderate and high doses. Patients who used more than one VAD
were categorized according to the highest level of one of the medications [25].
In summary, there were 809 mobilization opportunities, with the
physiotherapist who made the decision on the indication of mobilization, in 260
(32.1%) of these opportunities rehabilitation did not occur because passive
mobilizations were performed, which for the authors was not considered a
rehabilitation intervention. In the total of mobilizations performed, on 299
occasions the patients were using inotropes or vasopressors, in 144 (48.16%) of
these occasions the exercise was not performed. The exercises in bed occurred
in 41 (13.71%) of these sessions, and in 114 (38.12%) occasions they were
performed out of bed. Of all these occasions, only one adverse event occurred
when patients were on VAD support. This adverse event was defined as
cardiovascular instability and occurred when using the tilt table in a patient
who was classified as receiving a moderate level of inotropic support (0.15 mcg
/ kg / min noradrenaline). At the conclusion of the study, they suggest that
addiction to vasoactive medication should not be considered a reason to retain
exercise rehabilitation [25].
Camargo et al. [2] performed a single passive cycle ergometer
exercise for lower limbs for 20 minutes in 19 hemodynamically stable patients,
deeply sedated and mechanically ventilated. Among those evaluated, 13 (68%)
were using noradrenaline. The hemodynamic, respiratory and metabolic variables
were evaluated minute by minute before, during and after exercise. The
variables analyzed included: cardiac output, systemic vascular resistance,
central venous oxygen saturation in the blood, respiratory rate and tidal
volume, oxygen consumption, carbon dioxide, blood lactate production and
levels. In conclusion, exercise was considered safe, not being associated with
significant changes in hemodynamic, respiratory conditions or metabolic
variables, even in those that required vasoactive agents.
Passive exercises (PE) are widely used in the treatment of unconscious
patients and an early start is recommended. Genc et
al. [28] aimed to determine the effects of PE on hemodynamic and
respiratory parameters in critically ill patients receiving vasopressor or
inotropic support at a low dose. The medical records of 120 patients were
evaluated and were retrospectively grouped into two groups in which
thirty-eight patients did not receive vasopressor / inotropic support (group 1)
and 82 patients received low-dose vasopressor / inotropic support (group 2).
Central venous pressure, heart rate, mean arterial pressure, and oxygen
saturation were recorded before and immediately after PE. No statistically
significant difference was observed in the rate of change in hemodynamic or
respiratory parameters between the two groups after PE. This retrospective
study confirmed that PE results in similar hemodynamic and respiratory changes
in critically ill patients who received low doses of vasopressor / inotropic
support compared to those who did not.
In a recent study by Gardenghi et al.
[24], 26 patients underwent cardiac surgery for myocardial revascularization or
valve replacement, performed with median sternotomy, and half were using
dobutamine and norepinephrine with doses at medical discretion. They were
submitted to active exercises on the 1st PO day using a cycle ergometer for
upper limbs for 5 minutes with intensity assessed by effort and dyspnea (4 and
5 on the Borg scale), and by the parameters of HR, SpO2 and MAP. Gardenghi et al. were able to demonstrate that EM in this
group was safe, as there were no related adverse events, and mainly, there were
no abnormal hemodynamic changes even in patients using VADs.
Liu et al. [15] showed that EM is safe, even when performed by
professionals who are not specialized in EM, in a hospital without a culture of
mobilization, performing basic training for only one month. They determined the
safety of mobilization by assessing the incidence rate of adverse events in
rehabilitation sessions. During 587 sessions there were 13 adverse events that
included seven episodes of patient intolerance and six of orthostatic
hypotension, and activity was stopped. There were no serious adverse events
that required additional treatment such as increasing the dose of VAD. In
addition, it was observed that patients who received therapy for about 20
minutes, the real time being determined according to the case of each patient,
took an average time of 1.2 days to get out of bed.
Garzon-Serrano et al. [7] evaluated the level of mobilization
performed by physiotherapists and nurses in patients admitted to the ICU, on a
scale of 0 to 4, where 4 was the highest level of mobilization. Activities were
carried out at the bedside, transfers from bed to chair and gait training, so
mobilization was considered a process of improving mobility in the ICU. The use
of VADs was not a predictor of exclusion for mobilization, and they were used
to maintain stable hemodynamic parameters, and their use did not promote
adverse effects on patients. The level of patient mobilization achieved by
physical therapists was higher than that achieved by nurses. Among the
professionals, different mobilization barriers were identified, such as hemodynamic
instability and renal replacement therapy, which were barriers more considered
by nurses, while neurological impairment was classified as a higher barrier by
physical therapists. Due to a direct relationship between the level of
mobilization and the beneficial effects of it, initiatives to standardize this
intervention among intensivists become important.
In the prospective multicenter cohort study carried out by Hodgson et
al. [12], developed in 12 ICUs in Australia and New Zealand, with 192
patients, the practice of EM, strength at discharge from the ICU and functional
recovery of patients on mechanical ventilation were investigated. As barriers
to EM, sedation and intubation were identified. Activities were performed in
bed, bedside and out of bed, with sedation, orthostasis, ambulation and active
movements for upper limbs and lower limbs in flexion and extension, after an
average of 5 days of hospitalization. Ambulation was performed after day 7 of
hospitalization. 209 mobilizations were recorded, and there were no serious
adverse events, except for 6 records where interruption due to cardiovascular
or respiratory instability occurred, without the need for medical intervention.
The use of VAD was present in 66% of the patients and was not an impediment to
treatment. Thus, the MRC-SS score was higher in patients who were mobilized on
MV (50.0 ± 11.2 versus 42.0 ± 10.8, P = 0.003). And yet, more than 50% of
patients discharged from the ICU developed weakness acquired in the ICU
associated with death after discharge.
In the study by Wolfe et al. [20], which consists of a secondary
analysis of patients who were selected to receive early mobilization within 72
hours of MV, patients were subjected to tests of muscle strength by the bed by
a blind therapist, to assess whether had developed muscle weakness acquired in
the ICU (ICU-AW). Of the 172 patients analyzed, 80 demonstrated ICU-AW at
hospital discharge. The authors reported that the use of VADs was associated
with a three-fold increase in the chances of developing ICU-AW, regardless of
other established risk factors. They mention that this effect is directly
associated with the duration of vasoactive medication and the cumulative dose
of norepinephrine, which is not seen in vasopressin and phenylephrine. They
also observed that only the β-adrenergic groups of VADs (noradrenaline,
epinephrine, dopamine and dobutamine) were significantly linked to the
development of ICU-AW [20].
In 2016 Hodgson [27] followed an EM protocol, where patients performed
activities at the highest level they could, aiming to maximize the safety of
the mobilization. Patients were not excluded because they were using VAD, they
were only excluded from early mobilization if they had a norepinephrine
dose> 0.2µg / kg / min or a 25% increase in the dose of any VAD in the last
6 hours. It resulted in an increase in mobility minutes performed by patients
in the ICU, reaching a higher level of activity after discharge. On the other
hand, four adverse events were reported, namely agitation and transient
hypotension and only one was necessary to interrupt the therapy, none of which
required complementary drug therapy.
This article has limitations that should be noted. As it is a literature
review, it is not possible through it to specify that all literature on the
subject has been included, no matter how much the authors have tried to do so.
It also includes different populations, which can interfere with the
conclusion.
Conclusion
In the search to reduce the distance between scientific research and
clinical practice, this literature review showed that early mobilization for
ICU patients using vasoactive drugs proved to be effective and safe without
promoting relevant hemodynamic and cardiorespiratory changes, which would
determine their absolute contraindication. Thus, in view of the beneficial
responses, early mobilization can and should be used as a resource in intensive
care, as long as there is a monitoring of risks by the
multidisciplinary team.
Conflict
of interest statement
The authors report no financial relationships or conflicts of interest
in relation to the content of this document.
Authors'
participation
Conception and design of the study: GG and JAAS. Data acquisition: AMM,
DNP, DGC and VBAFS. Analysis and interpretation of data: GG and JAAS. Writing
of the manuscript: AMM, DNP, DGC and VBAFS. Critical review: GG and JAAS.
References
- Hodgson
C, Needham D, Haines K, Bailey M, Ward A, Harrold M, Young P, Zanni J et al. Feasibility and inter-rater reliability of
the ICU Mobility. Scale Heart & Lung: The Journal of Agute
and Critical Care 2014;43(1):19–24. https://doi.org/10.1016/j.hrtlng.2013.11.003
- Camargo JBG, Cavenaghi
OM, Mello JRC, Brito MVC, Ferreira LL. Mobilidade funcional de pacientes
críticos em terapia intensiva: um estudo piloto. Revista de Atenção à Saúde
2020;18(63):14-20.
- Aquim EE, Bernardo WM, Buzzini RF, Azeredo NAG, Cunha LS, Damasceno MCP et al.
Diretrizes Brasileiras para Mobilização Precoce em Unidade de Terapia
Intensiva. Rev Bras Ter
Intensiva 2019;31(4):434-43. https://doi.org/10.5935/0103-507x.20190084
- Timenetsky KT, Neto AS, Assunção
MSC, Taniguchi L, Eid RAC, Corrêa TD. Mobilization
practices in the ICU: A nationwide 1-day point- prevalence study in Brazil. PLoS ONE 2020;15(4):e0230971.
https://doi.org/10.1371/journal.pone.0230971
- Hashem
MD, Nelliot A, Needham DM. Early mobilization and
rehabilitation in the ICU: moving back to the future. Respiratory Care
2016;61(7):971-9. https://doi.org/10.4187/respcare.04741
- Tipping
CJ, Harrold M, Holland A, Romero L, Nisbet T, Hodgson CL. The effects of active
mobilization and rehabilitation in ICU on mortality and function: a systematic
review. Intensive Care Med 2017;43:171-83.
https://doi.org/10.1007/s00134-016-4612-0
- Garzon-Serrano
J, Ryan C, Waak K, Hirschberg R, Tully S, Bittner EA,
Chipman DW, et al. Early mobilization in critically ill patients: patients'
mobilization level depends on health care provider's profession. PM&R
2011;3(4):307-13. https://doi.org/10.1016/j.pmrj.2010.12.022
- Morris
PE, Griffin L, Berry M, Thompson C, Hite RD, Winkelman C, Hopkins RO et al.
Receiving early mobility during an intensive care unit admission is a predictor
of improved outcomes in acute respiratory failure. Am J Med Sci
2011;341(5):373-7. https://doi.org/10.1097/MAJ.0b013e31820ab4f6
- Fontela PC, Lisboa TC, Forgiarini-Júnior LA,
Friedman G. Early mobilization practices of mechanically ventilated patients: a
1-day point-prevalence study in southern Brazil. Clinics 2018;73:e241. https://doi.org/10.6061/clinics/2018/e241
- Feliciano
VA, Albuquerque CG, Andrade FMD, Dantas CM, Lopez A,
Ramos FF et al. A
influência da mobilização precoce no tempo de internamento na Unidade de
Terapia Intensiva. ASSOBRAFIR Ciência
2012;3(2):31-42
- Pires-Neto RC, Lima NP, Cardim GM, Park
M, Denehy L. Early mobilization practice in a single Brazilian Intensive Care
Unit. J Crit Care 2015;30(5):896-900.
https://doi.org/10.1016/j.jcrc.2015.05.004
- Hodgson
C, Bellomo R, Berney S,
Bailey M, Buhr H, Denehy L, Harrold M et al. Early mobilization and recovery in
mechanically ventilated patients in the ICU: a bi-national, multi-centre, prospective cohort study. Crit
Care 2015;19(1):81. https://doi.org/10.1186/s13054-015-0765-4
- McWilliams
D, Jones C, Atkins G, Hodson J, Whitehouse T, Veenith
T, Reeves E et al. Earlier and enhanced rehabilitation of mechanically
ventilated patients in critical care: a feasibility randomised
controlled trial. J Crit Care 2018;44:407-12.
https://doi.org/10.1016/j.jcrc.2018.01.001
- Jolley
SE, Moss M, Needham DM, Caldwell E, Morris PE, Miller RR, Ringwood N, et al.
Point prevalence study of mobilization practices for acute respiratory failure
patients in the United States. Crit Care Med
2017;45(2):205-15. https://doi.org/10.1097/CCM.0000000000002058
- Liu
K, Ogura T, Takahashi K, Nakamura M, Ohtake H, Fujiduka K, Abe E, Oosaki H, et
al. The safety of a novel early mobilization protocol conducted by ICU physicians:
a prospective observational study. J Int Care 2018;(6):10. https://doi.org/10.1186/s40560-018-0281-0
- Mendonça LBA, Madeiro
AC, Lima FET, Barbosa IV, Brito MEM, Cunha LGP. Uso de catecolaminas de infusão
contínua em pacientes de unidade de terapia intensiva. Rev
Enferm UFPE on line 2012;6(1):26-31.
- Fonseca JCL. Drogas
vasoativas – Uso racional. Rev Soc
Cardiol 2001;14:49-53.
- Ostini FM, Antoniazzi P, Filho AP, Bestetti
R, Cardoso MCM, Filho AB. O uso de drogas vasoativas em terapia intensiva.
Simpósio: Medicina Intensiva: I. Infecção e choque; 1998;31:400-11.
- Udesen NLJ, Helgestad
OKL, Banke ABS, Frederiksen PH, Josiassen
J, Jensen LO et al. Impact of concomitant vasoactive treatment and mechanical
left ventricular unloading in a porcine model of profound cardiogenic shock. Crit Care 2020;24(1):95. https://doi.org/10.1186/s13054-020-2816-8
- Wolfe
KS, Patel BK, MacKenzie EG, Giovanni SP, Pohlman AS, Churpek MM et al. Impact of vasoactive medications on
ICU-acquired weakness in mechanically ventilated patients. Chest
2018;154(4):781-7. https://doi.org/10.1016/j.chest.2018.07.016
- Jentzer JC, Coons JC, Link CB,
Schmidhofer M. Pharmacotherapy update on the use of
vasopressors and inotropes in the intensive care unit. J Cardiovasc Pharmacol Ther 2014;20(3),249-60.
https://doi.org/10.1177/1074248414559838
- Conceição TMA, Gonzáles AI, Figueiredo FCXS,
Vieira DSR, Bündchen DC. Critérios de segurança
para iniciar uma mobilização precoce em unidades de terapia intensiva. Revisão
sistemática. Rev Bras Ter
Intensiva 2017;29(4):509-19. https://doi.org/10.5935/0103-507x.20170076
- Fontanela PC, Jr Forgiarini LA, Friedman G. Atitudes clínicas e barreiras
percebidas para a mobilização precoce de pacientes graves em unidades de
terapia intensiva adulto. Rev Bras
Ter Intensiva 2018;30(2);187-194. https://doi.org/10.5935/0103-507x.20180037
- Gardenghi G, Kushida
CL, Dias AB, Cruz JB, Lima KR, Souza AH. Estudo piloto da viabilidade no uso de
cicloergômetro para membros superiores no primeiro
dia pós-operatório de cirurgia cardíaca. Rev
Pesqui Fisioter
2019;9(2):179-86. http://doi.org/10.17267/2238-2704rpf.v9i2.2303
- Boyd
J, Paratz J, Tronstad O,
Caruana L, McCormack P, Walsh J. When is it safe to exercise mechanically
ventilated patients in the intensive care unit? An evaluation of consensus
recommendations in a cardiothoracic setting. Heart Lung 2018;47(2):81-6.
https://doi.org/10.1016/j.hrtlng.2017.11.006
- Pires-Neto RC, Kawaguchi YMF, Hirota AS, Fu C,
Tanaka C, Caruso P et al. Very early passive
cycling exercise in mechanically ventilated critically ill patients:
physiological and safety aspects - A case series. PLoS
One 2013;8(9):e74182.
https://doi.org/10.1371/journal.pone.0074182
- Hodgson
CL, Bailey M, Bellomo R, Berney
S, Buhr H, Denehy L, Gabbe B et al. A binational
multicenter pilot feasibility randomized controlled trial of early goal-directed
mobilization in the ICU. Crit Care Med
2016;44(6):1145-52. https://doi.org/10.1097/CCM.0000000000001643
- Genc A, Koca
U, Ali G. What are the hemodynamic and respiratory effects of passive limb
exercise for mechanically ventilated patients receiving low-dose vasopressor /
inotropic support? Crit Care Nurs
Q 2014;37(2):152-8. https://doi.org/10.1097/CNQ.0000000000000013
- Hodgson
C, Stiller K, Needham D, Tipping C, Harrold M, Baldwin C, Bradley S et al.
Expert Consensus and recommendations on safety criteria for active mobilization
of mechanically ventilated critically ill adults. Crit Care
2014;18(6):658.