Rev Bras Fisiol Exerc 2021;20(1):101-24
doi: 10.33233/rbfex.v20i1.4254
REVIEW
Recommendations for physical activity during COVID-19:
an integrative review
Recomendações
para a prática de exercício físico em face do COVID-19: uma revisão integrativa
Carlos
José Nogueira1,2, Antônio Carlos Leal Cortez1,3,5,
Silvânia Matheus de Oliveira Leal1,6, Estélio
Henrique Martin Dantas1,4,5
1Universidade Federal do Estado do Rio de
Janeiro, Rio de Janeiro, RJ, Brazil
2Escola Preparatória de Cadetes do Ar -
EPCAR / Força Aérea Brasileira (FAB), Barbacena, MG, Brazil
3Centro Universitário Santo Agostinho,
Teresina, PI, Brazil
4Universidade Tiradentes, Aracajú, SE, Brazil
5Academia Paralímpica Brasileira, São
Paulo, SP, Brazil
6Instituto Brasiliense de Fisioterapia,
Brasília, DF, Brazil
Received on: June 6, 2020;
Accepted on: October 12, 2020.
Correspondence: Carlos José Nogueira, Universidade Federal do Estado do
Rio de Janeiro - UNIRIO / Laboratório de Biociências da Motricidade Humana
(LABIMH), Rua Dr Xavier Sigaud,
290/301, 22290-180 Rio de Janeiro RJ
Carlos José Nogueira: carlosjn29@yahoo.com.br
Antônio Carlos Leal Cortez:
antoniocarloscortez@hotmail.com
Silvânia Matheus de Oliveira Leal:
silvaniamatheus123@hotmail.com
Estélio Henrique Martin Dantas:
estelio@pesquisador.cnpq.br
Abstract
Objective: To evaluate and synthesize the
scientific evidence in relation to the recommendations on the practice of
physical activity during and after the pandemic period. Methods: A
search was carried out with the Medline/Pubmed,
Cochrane, Web of Science and Scopus databases, and manual searches in journals,
in the references of the selected studies, in addition to the use of pre-print
studies. The initial search totaled 1026 records and after applying the
filters, 321 publications were selected. After the exclusion by title, summary,
duplicates, and full reading, 13 publications remained, in addition to another
10 studies selected manually, totaling 23 publications. Results: After
analyzing the results, the evidence was categorized according to: the effects
of physical exercise on viral respiratory infections, the impact of COVID-19 in
relation to physical inactivity, physical and mental health and recommendations
on regular physical activity during the COVID-19 pandemic and recommendations
on post-pandemic physical activity. Conclusion: Most evidence recommends
regular moderate physical activity during and after the pandemic. However, more
specific recommendations on intensity, type of exercise, sets and duration of
training need further investigation.
Keywords: exercise; coronavirus; coronavirus infections; exercise therapy.
Resumo
Objetivo:
Avaliar e sintetizar as evidências
científicas com relação as
recomendações sobre a prática de atividade
física durante
e após o período da pandemia. Métodos: Realizou-se uma busca junto às
bases Medline/Pubmed, Cochrane, Web of Science e Scopus, e buscas manuais em periódicos, nas
referências dos estudos selecionados, além da utilização de estudos pré-print. A busca inicial totalizou 1026 registros e após
a aplicação dos filtros, 321 publicações foram selecionadas. Após a exclusão
por título, resumo, duplicatas e leitura na íntegra restaram 13 publicações,
além de mais 10 estudos selecionados manualmente, totalizando 23 publicações. Resultados:
Após análise dos resultados, as evidências foram
categorizadas de acordo com:
os efeitos do exercício físico sobre
infecções respiratórias virais, o impacto
da COVID-19 em relação à inatividade
física, saúde física e mental e
recomendações
sobre a atividade física regular durante a pandemia da COVID-19
e recomendações
sobre atividade física pós pandemia. Conclusão: A maioria das evidências
recomendam a realização de atividade física moderada regular durante e após a
pandemia. No entanto, recomendações mais específicas sobre a intensidade, o
tipo de exercício, séries e duração do treino precisam de maiores
investigações.
Palavras-chave: exercício físico; coronavírus;
infecções por coronavírus; terapia por exercício.
Introduction
Coronavirus
(COVID-19) emerged in late December 2019, in the city of Wuhan in China, as the
leading cause of viral pneumonia [1,2,3] and spread rapidly across the country
and all continents in the world [2,4,5,6]. In March 2020, the World Health
Organization (WHO) declared the SARS-Cov-2 virus to be a global pandemic [3,7].
The current
COVID-19 pandemic presents an unexpected public health challenge. Ambitious
measures are being implemented worldwide by governments, non-governmental organizations,
and individuals to delay the spread of the virus and prevent overloading the
health system [8]. However, much remains to be done to "flatten the
curve" and mitigate the impact of the coronavirus [9].
The transmission
of SARS-Cov-2 occurs mainly from the respiratory spread from person to person
(people in close contact or through respiratory droplets produced when an
infected person coughs or sneezes) and, to a lesser extent, from contact with
infected people, surfaces or objects [1,10]
Clinical
conditions such as hypertension, respiratory, cardiovascular, and metabolic
diseases are important risk factors for severity in COVID-19 [11,12]. Current
studies point to potential risk groups: the elderly [11,13,14], young adults,
obese individuals with the comorbidities described above, chronic diseases with
hemodynamic and immunological repercussions [6,15].
According to Carda et al. [16], COVID-19 has different clinical
manifestations and the most observed are: 1) mild: no dyspnea, no low blood
oxygen saturation (SatO2), with or without fever spikes, loss of
smell and taste; 2) moderate: dyspnea during light or strenuous activities,
SatO2 94% to 98%, and radiological signs of pneumonia; 3) severe:
dyspnea, SatO2 ≤ 93%, respiratory rate (RR) > 30/min,
radiological progression of the lesions, need for O2
supplementation, possibly with non-invasive ventilation; and 4) critical:
patients need mechanical ventilation.
Physical
activity helps to improve immunity in the prevention and complementary
treatment for chronic diseases and viral infections such as the new coronavirus
[1,6,11,17,18,19,20,21,22]. The protective effect of exercise on the immune system is
crucial to adequately respond to the threat of COVID-19 [15,21,23].
Regular physical
activities of moderate to vigorous intensity, according to the guidelines of
the American College of Sports Medicine (ACSM), will improve the immune
responses to infections; decrease chronic low-grade inflammation, and improve
immunological and inflammatory markers in various disease states, including
cancer, HIV, cardiovascular disease, diabetes, cognitive impairment, and
obesity [21,23].
To fight
sedentary lifestyle and improve physical and mental health, ACSM [24] recently
released a guide suggesting that moderate-intensity physical activity (PA)
should be maintained in the COVID-19 quarantine, emphasizing the importance of
every physically active minute for health. The guidelines, in the current
situation, suggest 150 to 300 minutes per week of aerobic physical activity of
moderate intensity and two sessions per week of muscle strength training
[11,24].
This
recommendation is also for people in social distance who are not infected with
COVID-19 and people who are infected but remain asymptomatic. If symptoms
persist, exercise should be stopped, and the individual should seek medical
advice [25].
Although
containing the virus as quickly as possible is an urgent public health
priority, there are few guidelines for the public on what people can or should
do in terms of maintaining their daily exercise or physical activity routines
[26].
Given the
concerns about the increasing spread of COVID-19, it is imperative that
infection control and safety precautions, as well as appropriate recommendations
for physical exercise, be followed [26].
In view of the
world pandemic of COVID-19 and the inevitable need of the population to remain
active mainly through physical activity, the present study aims to evaluate and
summarize the scientific evidence on the recommendations for engaging in
physical activity and exercise during and after the pandemic COVID-19.
Methods
The stages of
this review were conducted based on methodology that provides synthesis of
knowledge and applicability of results of significant publications to practice
[27].
The review
followed the following stages: formulation of the guiding question; selection
of studies based on the year of publication and title; selection of studies by
their abstracts and selection by the full text; and afterwards, extraction of
data from the studies included; evaluation and interpretation of results, and,
finally, presentation of the review of the knowledge produced [28].
Selection of studies
The literature
survey was carried out in the Medical Literature Analysis and Retrieval System
Online (MEDLINE) databases through the National Library of Medicine (PUBMED),
Cochrane Central Register of Controlled Trials, Web of Science, and Scopus.
Other sources were also searched: journal hand-searching, references described
in the selected studies, and use of unpublished material (pre-print).
The initial
search identified 1026 records and after applying the filters, 321 publications
were selected. After removing duplicates, manual screening was performed and
those that were not relevant were excluded. Selected publications were assessed
in full text for eligibility. Those that did not meet the inclusion criteria
were excluded. Ten (10) publications were included by journal handsearching and
references in the selected and pre-print studies. The selection of publications
is described in the flowchart (Figure 1).
Search strategy
The search was
carried out by trained researchers with experience in the topic of the
articles. The searches were carried out in April 2020. The descriptors selected
in the Health Sciences Descriptors (DeCS) and Medical
Subjetc Headings (MeSH) were: exercise, coronavirus, covid-19, and coronavirus
infections, as described and presented together with the search strategy in
Chart 1. From this search, publications for complete reading that met the
inclusion criteria for this review were selected. Regarding the scientific
analysis of publications, according to Qualis CAPES
and SCImago Journal Rank (SJR), it was observed that
52.2% were classified as belonging to extract A by Qualis
CAPES and 34% of publications were classified as belonging to quartile 1 (Q1)
according to SJR.
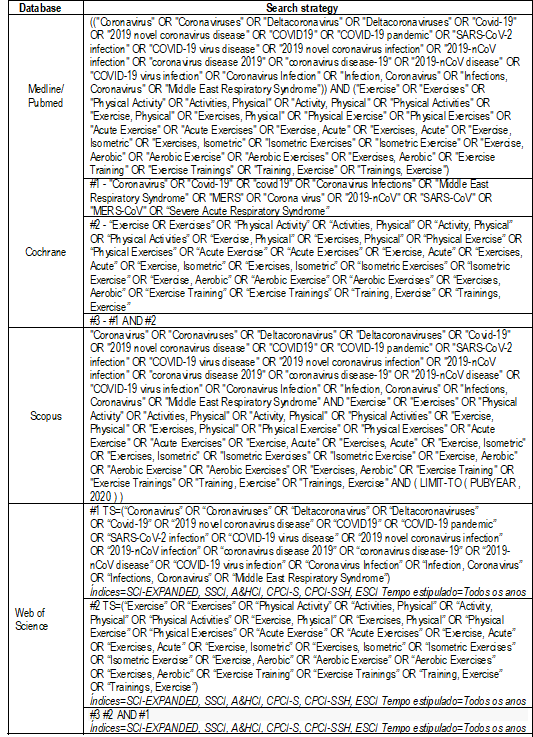
Source:
Author 2020
Chart I - Controlled descriptors used
to build the search strategy in the Medline/Pubmed,
Cochrane, Web of Science, and Scopus databases
Eligibility criteria
Full articles in
English, Spanish, or Portuguese related to the effects of exercise and
recommendations on PA during and after the COVID-19 pandemic were included. The
evidence included original articles and consensus, reviews, editorials,
interviews, in addition to studies in the pre-publication phase (pre-print).
Data extraction
The summary
included the extraction of the following data: authors and year of publication,
type of study, objective, and evidence. Finally, the results relevant to
current knowledge on the study topic were evaluated for producing evidence.
Results
The search
identified 1026 records and after applying the filters, 321 publications were
selected. Two-hundred ninety-seven (297) studies were excluded by title,
abstract, duplicates, and after reading full-text articles. At the end, 13 publications
made up the sample and were analyzed, in addition to another 10
pre-print studies hand selected. Figure 1 (Prisma Flow) describes the
path taken to select the studies, according to the consulted basis.
According to the
descriptors used in the research, 118 publications were identified in Medline/Pubmed, 12 in Cochrane, 43 in Web of Science and 853 in
Scopus. Figure 1 shows the search strategy after applying the filters in the
Prisma Flow diagram.
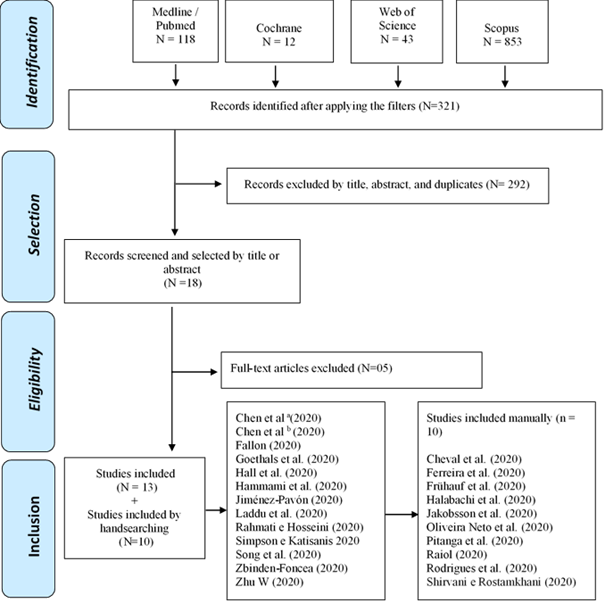
Source:
Author, 2020 adaptation by Moher et al. (2008) [29]
Figure 1 - Flow diagram of article
selection (Prisma Flow)
A narrative
synthesis of the selected publications was carried out, presenting the
scientific evidence on physical exercise and COVID-19 and the main
recommendations for physical activity during and after the pandemic. Data
extraction was performed with a specific instrument, containing information
about authors; year of publication; journal, database, Qualis,
SJR, as well as the identification of the scientific evidence of the selected
studies. The included reports were organized in tables according to the
identified variables.
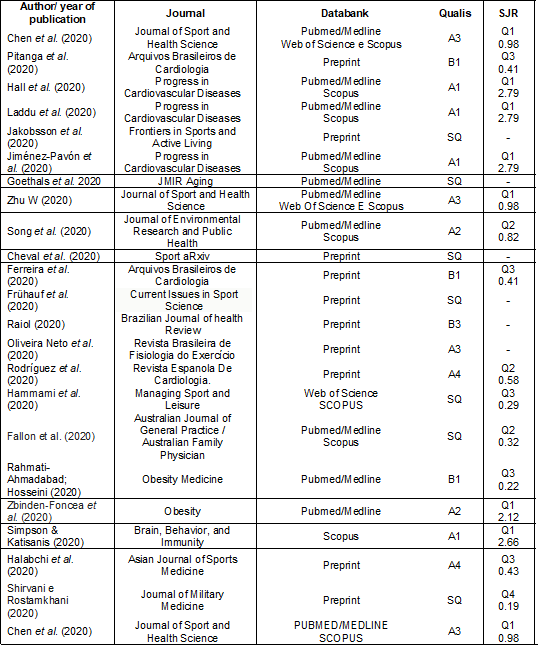
**Preprint = study hand selected (Preprint means pre-publication: a scientific study that has not yet been published). SQ: Without QUALIS; Source: Author, 2020
Chart II - Synthesis of the reports
included in the integrative review, according to author/year of publication,
journal, database, Qualis and SJR
Table II shows
that the journals that published articles on the topic are dispersed. Two
journals (Progress in Cardiovascular Diseases and Journal of Sport and Health
Science) published 03 articles each, making 26.6% of the total articles
selected. Of these journals, 47.83% are indexed in Pubmed/Medline
and 43% in Scopus and, it is noteworthy that some journals are indexed in more
than one database.
Taking into
account Qualis Capes (Brazilian journal evaluation
system) and SJR (a measure of the scientific influence of academic journals
that accounts for the number of citations received by a journal and the
importance or prestige of the cited journals), we found that 52.2% were
classified as Qualis A and, 8 journals, 34.8%, were
classified and qualified as Q1 by SJR.
After analyzing
the results, four thematic categories emerged, which were characterized below
and presented according to their scientific evidence on physical activity and
COVID-19 in Table III:
a) Effects of physical exercise on viral respiratory infections;
b) Impact of COVID-19 related to physical inactivity,
physical and mental health;
c) Recommendations on regular physical activity during
the COVID-19 pandemic;
d) Recommendations on post-COVID-19 physical activity.
Chart III - Systematization of the main
evidence on physical activity related to COVID-19 (see PDF annexed)
Discussion
Effects of physical activity on viral respiratory
infections
The main
question in sports and exercise medicine is whether physical activity is
appropriate during the viral respiratory tract epidemic or not [1]. Studies
have indicated that exercise performed at moderate intensity has positive
effects on the immune system's responses to viral respiratory infections
[17,19,23,30,41,42,43] and is associated with several anti-influenza benefits,
including reduced risk influenza and the increase in vaccine efficacy rates
[21,23,30,31].
After moderate
intensity physical activity, an increase in the count of neutrophil and natural
killer cells (NK) is detected, and an increase in the salivary concentrations
of IgA [42,43]. Moderate physical activity increases stress hormones and, thus,
reduce excessive inflammation [43] and lead to increased immunity against viral
infections by altering the responses of Th1/Th2 cells [42].
To study this
situation more deeply, Song et al. [14] summarized the current literature on
the effects of exercise on influenza or pneumonia in the elderly to determine
the appropriate exercise that contributes to beneficial clinical outcomes for
this population. The results confirmed that aerobic exercise with moderate
intensity can help to reduce the risk of influenza-related infection, improve
immune responses to influenza and pneumonia vaccine in the elderly. Even
traditional Asian martial arts can also contribute to some related benefits.
Impact of COVID-19 on physical inactivity and physical
and mental health
The COVID-19
pandemic appears to have a major impact on physical activity behaviors
worldwide, forcing people to remain self-isolated in their homes for a period.
These acts will negatively affect people's physical activity behaviors
[25,32,33].
Currently,
the world lives with two concomitant pandemics. Although of a different nature,
the physical inactivity pandemic has been present in society for some years and
becomes even more worrying, given that COVID-19 is making people move less than
before, bringing the risk of worsening the situation with resuming to
normality. The interaction between the current risks of health complications
and the mortality rates associated with COVID-19 and the current state of
physical inactivity and physical inactivity cannot be ignored. Therefore,
global society needs to establish great effort to encourage people to engage in
physical activity after COVID-19, or at the very least to maintain at the level
they had before the pandemic. In this way, they will avoid a possible vicious
cycle in which current and high standards of physical inactivity and sedentary
behaviors worsen the impact of future pandemics [34].
The impact of a
sedentary lifestyle may be less for children and young adults, but much more
decisive for at-risk populations, which include older people (± 60 years),
presenting obesity, diabetes, hypertension, cardiovascular disease, history of
smoking, and chronic obstructive pulmonary disease (COPD) [6].
Because of the
higher risk of COVID-19 infection, older people need to stay at home, making
physical activities during quarantine crucial to avoid sedentary lifestyle [35].
How will the elderly maintain their independence and mental wellbeing after
ending the quarantine if they have no appropriate promotion of physical
activity at home?
In this sense,
Goethals et al. [35] conducted a qualitative study to assess the impact
of quarantine on the program of the French Federation of Physical Education and
Voluntary Gymnastics and on the physical and mental wellbeing of older adults.
They also looked at the alternatives that could be offered to this population
to avoid a sedentary lifestyle. The research was carried out using
semi-structured interviews with managers of the PA programs for the elderly and
sports coaches who supervise these programs. The results of the study suggested
that COVID-19 affected the number of PA programs in the elderly groups even
before the quarantine measures were implemented. It was found that the elderly
expressed the need to exercise at home during quarantine despite the decline in
participation in physical activities before isolation measures due to fear of
contact with infected people. Therefore, the authors recommend assistance to
help the elderly to engage in simple and safe ways to remain physically active
during the pandemic and a national policy to support this population to
exercise at home [35].
For this
population, Jiménez-Pavón et al. [13] propose a
more precise prescription and recommendation to ensure an appropriate exercise
program, which is designed to maintain or improve the main components of
health-related physical fitness during COVID-19 through regular participation
in moderate-intensity aerobic exercise, muscle strengthening, balance,
coordination, and stretching activities.
Another risk
group, vulnerable to respiratory infection and adverse effects of COVID-19 are
obese, overweight, and insulin-resistant people with diabetes. These
individuals usually have low-grade chronic inflammation characterized by
elevated levels of various pro-inflammatory cytokines. Considering that the
COVID-19 progression depends largely on the individual's initial health status
and the immune response triggered by the infection, it is suggested that
previous physical training and high levels of cardiorespiratory fitness by
moderate intensity aerobic training are probably immunoprotective
in patients infected with SARS-CoV-2, especially those with these chronic
comorbidities [6]. Thus, as exercise of moderate intensity can increase the
immune response and reduce the patterns of pro-inflammatory cytokines, it is
recommended for this population to carry out moderate regular physical activity
in a safe environment combined with an adequate diet to promote beneficial
effects on immune function and health maintenance avoiding the complications of
COVID-19 [36].
Recommendations on regular physical activity during
the COVID-19 pandemic
Due to the
global increase in the pandemic, it is essential to follow the measures of
infection control and safety. Thus, staying at home is a fundamental safety
principle that can limit the spread of infections [26]. However, staying at
home for a long time can intensify behaviors that lead to a sedentary lifestyle
and contribute to anxiety and depression, which can result in a series of
chronic health conditions [26,33]. For this reason, it is important that the
population be informed about the need to reduce sedentary behavior during the
period of social isolation [37].
In this regard,
maintaining regular physical activity and exercising routinely in a safe home
environment is an important strategy for a healthy life during the coronavirus
pandemic [26]. The same authors, following the guidelines of the US Department
of Health and Human Services, recommend at least 30 minutes of moderate
physical activity every day and/or at least 20 min of vigorous physical
activity every other day, in addition to regular strengthening exercise [26].
It is suggested that children, the elderly, and people who have already had
symptoms of coronavirus infection or are susceptible to chronic cardiovascular
or pulmonary disease should seek guidance from specialized health professionals
on the safety of physical activity [26,31].
Cheval et al.
[38] found that changes in physical activity and sedentary behaviors during
lockdown are associated with changes in physical and mental health. The authors
assessed differences in physical activity and sedentary behaviors before and
during the lockdown in a total of 267 (1st wave of COVID-19) and 110
participants (2nd wave of COVID-19) who live in France or Switzerland. Based on
the results, the authors reinforce that ensuring sufficient levels of physical
activity and reducing sedentary time during the lockdown can benefit health of
individuals.
It is
important to underline the reasons why regular exercise should not be
interrupted during the COVID-19 pandemic. For this purpose, Raiol
et al. [25] studied the beneficial effects of exercise for people in
social distance, addressing aspects of immunity, disease control, functional
capacity, and mental health. After analyzing the literature, the authors
suggested that, during social distance, physical exercises should be performed
at home or in open-air places without crowds. The frequency should be 5-7 days
a week for aerobic exercises and, at least, 2-3 days a week for muscle
strengthening exercises, both with moderate intensity, in
order to maximize the positive effects on the immune system.
Based on proven
evidence, Laddu et al. [19] extend the benefits of regular physical
activity to improving immune function and reducing the risk, duration, or
severity of viral infections. Therefore, they recommend the usual practice (~
150 min per week) of moderate intensity physical exercises to obtain ideal
immune support. However, evidence strengthens that even acute PA sessions can
protect people from viral infections [45], agreeing with the view that moving
daily in a structured manner can optimize immune system functions and prevent
or mitigate the severity of infection, especially among vulnerable and
immunocompromised populations.
Consistent with
available evidence and the similarity of some of the signs and/or symptoms of
COVID-19 with the H1N1 virus, moderate exercise may be recommended during the
outbreak for healthy or asymptomatic individuals. People with mild symptoms of
the upper respiratory tract (eg, runny nose, nasal
congestion, mild sore throat) may exercise lightly with precautions [30]. It is
worth mentioning that prolonged exercise programs or high intensity training
without adequate recovery can cause immunodepression and increase
susceptibility to pathogens and infectious diseases [19,23,30,31,41,42,45,46].
Oliveira Neto et
al. [39] proposed an exercise prescription during the COVID-19 pandemic,
integrating the physiological and psychobiological aspects, considering the
barriers confronted by the population in the face of social isolation
worldwide. They recommend a prescription that encourages at least 150 minutes
of aerobic exercise with moderate intensity complemented with strength
exercises for the main muscle groups. The authors emphasize the importance of
behavioral and motivational aspects alongside physiological variables as one of
the major challenges, given the need to train with little or no face-to-face
supervision, which can increase behavioral difficulties (for example, habit) to
exercise.
In conformity
with the WHO recommendations, Jakobsson et al. [33] highlight the
benefits of PA during the COVID-19 pandemic in the respect that “doing
something is better than doing nothing”. They also establish the following
recommendations: avoid prolonged sitting time; reduce sedentary lifestyle with
brief active breaks during the day; accumulate at least 150 minutes of moderate
intensity PA or 75 minutes of vigorous intensity per week; use training
applications to monitor PA and/or follow online exercise classes to motivate
exercise; include cardiovascular and muscle strengthening exercises; always be
cautious and aware of your own limitations, and do not exercise with infection
symptoms.
Hammami et
al. [32] present useful information for daily home PA for sedentary people
during the pandemic, extending the recommendations to children and adolescents.
Children and young people (5 to 17 years old) should perform 60 min/week of
daily PA with aerobic exercises of moderate to vigorous intensity in addition
to muscle and bone strengthening three times a week. For adults and the elderly
(>17 years), they recommend 75 min/week of daily PA with aerobic exercises
of vigorous intensity or 150 min/week of moderate aerobic intensity, with
muscle and bone strengthening twice a week. They also recommend that people
remain active by exercising at home. In this respect, different types of
activities can be scheduled, including aerobic exercises using stationary bikes
or rowing ergometers, strength training with body weight, exercises based on
dance, and active games.
Fallon et al.
[18] increase the types of exercises to be performed at home during the
COVID-19 pandemic. A simple search on the Internet or YouTube will reveal many
home programs for dance, aerobics, yoga, Pilates, strength, and stretching
exercises. Aerobic exercise can be facilitated using stairs and inclines;
running on the spot; home bikes, treadmills; or laps around the backyard pool.
The strengthening activity can be performed through bodyweight exercises such
as squats, push-ups, abdominal work, and stair or inclination calf raises are
also useful. Simple household items such as full water bottles and cans or food
packages can be used as overload. However, Simpson and Katisanis
[23] maintain that it is probably unnecessary to use specialized technology and
equipment to remain physically active during the coronavirus outbreak, since
exercising at home or outdoors through fast walks, climbing stairs, working in
the yard/house and/or playing active games can be equally effective using
online exercise platforms in this period.
To better cope
with the social isolation, Ferreira et al. [11] proposes to the
population some behaviors and attitudes that will help in maintaining an active
life and improving physical and mental health: performing pleasurable physical
activities, exploring the best available spaces and materials; perform routine
activities such as cleaning, maintenance and organization of domestic spaces;
playing and exercising with children, adolescents, and pets (so that energy
expenditure is higher than in the resting condition); avoid sedentary behavior,
alternating sitting or lying down with periods of PA, reducing the time spent
using electronic devices [37], and allowing a few minutes for stretching,
relaxation, and meditation activities [11].
Due to the
increased need for exercise during the quarantine, Jiménez-Pavón
et al. [13] made a critical analysis of the most appropriate
recommendations for exercising, especially for the elderly population and
adjusted and increased the international recommendations on PA for the current
situation. The authors suggest an increase to 200 to 400 minutes per week,
spread over 5 to 7 days to compensate for the decrease in normal daily levels
of PA. In addition, a minimum of 2-3 days a week of resistance training may be
recommended, in addition to daily stretching routines and balance and
coordination exercises at least twice a week, which are distributed among the
different training days. Pitanga et al. [37]
recommend the duration of approximately 30 to 60 minutes a day for each
exercise session. The control of exercise intensity is crucial to avoid harmful
effects and promote the improvement of the immune system. For this purpose,
during quarantine times, moderate intensity (40 to 60% of heart rate reserve or
65 to 75% of maximum heart rate) should be the best option, especially for the
elderly [13].
Rodrígues et
al. [15] analyzed the recommendations for performing PA in health
institutions during the pandemic period, inside and outside Spain. In general,
all entities provide the same general recommendations: stay active at home,
take short breaks, and avoid a sedentary lifestyle. They also reinforce that,
to remain active during lockdown, the population must carry out multifunctional
programs for the whole body, which include aerobic exercises, muscle
strengthening, balance and stretching, in addition to cognitive tasks that are
strongly recommended for the elderly. However, none of the institutions makes
specific recommendations about series and repetitions, intensity, or frequency,
and most recommend the use of online classes or mobile applications [15].
Considering PA
outside the home environment, publications based on scientifically sound
findings and observing the current rules of social distance recommend the
permission of moderate outdoor sports activities (such as running, walking, and
cycling) and park trails, hiking trails, and forest roads on easy terrain [8,48].
The results of a recent study on the aerodynamic effects of movement carried
out through a computer simulation of fluid dynamics, in the absence of head
wind, tail wind, and cross wind, point to the need for additional precautions
of social distance for outdoors activities and sports. Distances of 05 meters
must be kept when walking fast at 4 km/h and 10 meters when running at 14.4
km/h. In addition, people should avoid walking or running directly behind the
main person and keep a distance of 1.5 m in an
alternating or side-by-side arrangement [49].
Some indirect
evidence shows that moderate PA can be recommended as a non-pharmacological,
inexpensive, and feasible way of facing COVID-19 infection. However,
high-intensity exercise can be harmful and exacerbate the infection, especially
in patients at risk. This is probably due to the oxidant production and the
suppression of the immune system. Thus, the recommendation of these exercises
needs further investigation [40,47]. The results of a recent systematic review
have shown that long, intense exercise can lead to higher levels of
inflammatory mediators, which can lead to an increased risk of injury and
chronic inflammation. However, moderate or vigorous
exercise with appropriate rest periods can be significantly beneficial for
improving immune function [47].
According to Zhu
[31], it is safe to exercise during the coronavirus outbreak. However, there
may be some additional precautions to reduce the risk of transmission. For
social exercisers, it is opportune to limit exposure to symptomatic exercise
partners and in some cases, it may be appropriate to use a mask during exercise
to avoid exposure.
Azizi et al.
[50] present some recommendations to athletes and non-athletes during the COVID-19
pandemic to maintain good health conditions for a future return to activities:
regular physical activity of moderate intensity avoiding extreme physical
efforts; aerobic or resistance activities in safe environments, respecting the
recommended social distance; disinfection of the training equipment; no
physical activity in case of fever or other suggestive symptoms; choose to
perform physical activity at home through safe, simple physical exercises that
are easy to perform and adapt; avoid drinking alcohol, and maintain quality
sleep.
Specifically
related to strength and power training, with equipment and load variety, in
order to limit access to training sites due to the COVID19 pandemic, Guimarães-Ferreira and Bocalini
[51] present practical recommendations for strength training in the home
environment during the pandemic to maintain physical fitness and reduce the
deleterious effects of detraining. These authors recommend performing exercises
using your own body weight, household items and, when accessible, dumbbells,
and elastic bands. For low loads (30-50% of 1 maximum repetition), the series
should be performed to concentric failure to optimize gains in strength and
muscle mass. Exercises should be performed on most days of the week (>5 days/week),
in combination with domestic and leisure activities that involve the movement
of the whole body. To maintain and/or develop muscle power, ballistic movements
should be included with or without external loads.
Recommendations on physical activity after COVID-19
An important
situation to be discussed is the maintenance or return to PA during or after an
upper respiratory tract infection. Halabchi et al.
[1] are based on evidence about the neck check rule. If symptoms of upper
respiratory tract infection are limited to the neck, including coughing,
sneezing, and sore throat, the individual is asked to run for 10 minutes. If
the general condition and signs are deteriorated, physical activity should be
prohibited until full recovery. If the conditions do not change after 10
minutes of running, the person may return to physical activity of low to
moderate intensity (below 80% of VO2max). However, due to the new
COVID-19 characteristics and its negative effect on the immune system and rare
cardiac complications, including myocarditis, more caution is required
regarding the continuation of exercise in symptomatic patients [1].
Therefore,
people who have already been infected with influenza, severe acute respiratory
syndrome (SARS), or the current COVID-19 can exercise moderately as long as
they have mild symptoms of the upper respiratory tract (for example, runny
nose, nasal congestion, mild sore throat). However, physical exercise is not
recommended for people with symptoms of severe sore throat, body aches,
shortness of breath, general fatigue, chest cough or fever [30]. It is
recommended to seek medical attention if you experience these symptoms [31]. In
general, recovery from respiratory viral infections takes 2 to 3 weeks, which
corresponds to the time for the immune system to generate cytotoxic T cells
needed to clear the virus from infected cells. After this period, when the
symptoms disappear, it is safe to start exercising regularly in a progressive
manner [31].
With regard to
school-age children and adolescents returning to PA after COVID-19, Chen et
al. [41] point out that with the resumption of school activities, public
health need to ensure that all children and youth effectively overcome the
imposed restrictions that limited exercise. Children should participate in the
recommended levels of PA during the school day, including the time they spend
in physical education classes. This return to PA can help students recover from
the stress and anxiety they experienced while in quarantine. Thus, restoration
of daily physical and sports activities must be progressive, starting with
short periods of activities more attractive to children and young people and
gradually increasing the number of days and the amount of time for
participation, so that eventually it will be enough to meet the guidelines,
minimizing the risk of injury after lockdown [41].
There are two
limitations in this research. First, the absence of randomized clinical trials
and the scarcity of studies with experimental design, with little
methodological rigor on the current topic, making it impossible to determine
the validity of methods and results. Second, it refers to publications about
different populations due to the emergence of the topic under study.
Conclusion
Regarding the
effects of exercise on viral respiratory infections, the evidence points to the
positive effects of exercising in an appropriate manner with moderate intensity
in the responses of the immune system, which may contribute to the reduction of
inflammation and the risk of infection.
With respect to
the impact of COVID-19 related to physical inactivity, physical health and
mental wellbeing, the results show a negative impact of physical inactivity and
sedentary lifestyle during and after the pandemic, with a greater effect on populations
at risk, especially the elderly.
In relation to
the recommendations on regular PA during COVID-19, it is evident that moving
daily in a structured way, by exercising, can optimize the functions of the
immune system and prevent or mitigate the severity of the infection, especially
in the most vulnerable populations. In this sense, most recommendations are for
PA of moderate intensity during the period of social isolation. Aerobic
exercises 5-7 days a week are suggested, muscle strengthening exercises at
least 2-3 days a week, and coordination, balance, and mobility exercises.
Prolonged exercise programs or high intensity training without adequate
recovery to avoid immunosuppression and greater susceptibility to infections
are contraindicated. Physical outdoor activities are recommended if additional
precautions for social distance are taken.
The analysis of
the evidence in the present study shows a lack of publications that focus on
determining the intensity of exercises during the pandemic, as well as specific
recommendations on series and repetitions. Caution is required regarding the
return, maintenance, and continuity of PA after COVID-19, mainly due to the
negative effect on the immune system and cardiac complications caused by the virus.
Conflict of interest
No conflicts of interest have been reported for this
article.
Financing source
This
study was financed in part by the Coordenação de
Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) - Finance Code 001.
Authors´s
contributions
Conception and design of the research:
Nogueira CJ, Cortez AL. Data collection: Nogueira CJ, Cortez AL, Leal SMO. Analysis
and interpretation of data: Nogueira CJ, Cortez AL. Obtaining financing: Dantas EHM. Writing of the manuscript: Nogueira CJ,
Cortez AL, Leal SMO, Dantas EHM. Critical revision
of the manuscript for important intellectual content: Nogueira CJ, Cortez
AL, Leal SMO, Dantas EHM.
References
- Halabchi F,
Ahmadinejad Z, Selk-Ghaffari M. COVID-19 Epidemic:
exercise or not to exercise; that is the question! Asian J Sports Med
2020;11(1). doi: 10.5812/asjsm.102630 [Crossref]
- Silva CMS, Andrade ADN, Nepomuceno B, Xavier DS, Lima E, Gonzalez I et al. Evidence-based physiotherapy and functionality in adult and pediatric patients with COVID-19. J Hum Growth Dev 2020;30(1):148-55. doi: 10.7322/jhgd.v30.10086 [Crossref]
- World Health Organization. World Health Organization.
Director-General’s remarks at the media briefing on 2019-nCoV on 11 February
2020 [Internet]. 2020 [cited
2020 Maio 8]. p. 1-5. Available from:
https://www.who.int/dg/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020
- Bogoch II, Watts A, Thomas-Bachli A, Huber C, Kraemer MUG, Khan K. Potential for global spread of a novel coronavirus from China. J Travel Med 2020;13;27(2):1-3. doi: 10.1093/jtm/taaa011 [Crossref]
- Lu R, Zhao X, Li J, Niu P, Yang B, Wu H et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet 2020;395(10224):565-74. doi: 10.1016/S0140-6736(20)30251-8 [Crossref]
- Zbinden-Foncea H, Francaux M, Deldicque L, Hawley JA. Does high cardiorespiratory fitness confer some protection against pro-inflammatory responses after infection by SARS-CoV-2? Obesity 2020;oby.22849. doi: 10.1002/oby.22849 [Crossref]
- Di Gennaro F, Pizzol D, Marotta C, Antunes M, Racalbuto V, Veronese N et al. Coronavirus diseases (COVID-19) current status and future perspectives: a narrative review. Int J Environ Res Public Health 2020;17(8):2690. doi: 10.3390/ijerph17082690 [Crossref]
- Frühauf A, Schnitzer M, Schobersberger W, Weiss G, Kopp M. Jogging, nordic walking and going for a walk - inter-disciplinary recommendations to keep people physically active in times of the covid-19 lockdown in Tyrol, Austria. Curr Issues Sport Sci 2020. doi: 10.15203/CISS_2020.100 [Crossref]
- Mann RH, Clift BC, Boykoff J, Bekker S. Athletes as community; athletes in community: covid-19, sporting mega-events and athlete health protection. Br J Sports Med 2020;54(18). doi: 10.1136/bjsports-2020-102433 [Crossref]
- Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395(10223):497-506. doi: 10.1016/S0140-6736(20)30183-5 [Crossref]
- Ferreira MJ, Irigoyen MC, Consolim-Colombo F, Saraiva JFK, De Angelis K. Vida Fisicamente ativa como medida de enfrentamento ao COVID-19. Arq Bras Cardiol 2020;114(4):601-02. doi: 10.36660/abc.20200235 [Crossref]
- Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis 2020;94:91-5. doi: 10.1016/j.ijid.2020.03.017 [Crossref]
- Jiménez-Pavón D, Carbonell-Baeza A, Lavie CJ. Physical exercise as therapy to fight against the mental and physical consequences of COVID-19 quarantine: Special focus in older people. Prog Cardiovasc Dis 2020;63(3);386-88. doi: 10.1016/j.pcad.2020.03.009 [Crossref]
- Song Y, Ren F, Sun D, Wang M, Baker JS, István B, et al. Benefits of exercise on influenza or pneumonia in older adults: a systematic review. Int J Environ Res Public Health 2020;17(8):2655. doi: 10.3390/ijerph17082655 [Crossref]
- Rodríguez MA, Crespo I, Olmedillas
H. Ejercitarse en tiempos del COVID-19: ¿qué recomiendan los expertos hacer entre cuatro paredes? Rev Española Cardiol
2020;73(7):527-29. doi: 10.1016/j.recesp.2020.04.002 [Crossref]
- Carda S, Invernizzi M, Bavikatte G, Bensmaïl [Crossref] D, Bianchi F, Deltombe T, et al. The role of physical and rehabilitation medicine in the COVID-19 pandemic: the clinician’s view. Ann Phys Rehabil Med 2020;63(6)554-56. doi: 10.1016/j.rehab.2020.04.001 [Crossref]
- Campbell JP, Turner JE. Debunking the myth of exercise-induced immune suppression: redefining the impact of exercise on immunological health across the lifespan. Front Immunol 2018;9(4):1-21. doi: 10.3389/fimmu.2018.00648 [Crossref]
- Fallon K. Exercise in the time of COVID-19. Aust J Gen Pract 2020;49. doi: 10.31128/AJGP-COVID-13 [Crossref]
- Laddu DR, Lavie CJ, Phillips SA, Arena R. Physical activity for immunity protection: Inoculating populations with healthy living medicine in preparation for the next pandemic. Prog Cardiovasc Dis 2020;40:4-6. doi: 10.1016/j.pcad.2020.04.006 [Crossref]
- Luan X, Tian X, Zhang H, Huang R, Li N, Chen P, et al.
Exercise as a prescription for patients with various diseases. J Sport Heal Sci
2019;8(5):422-41. doi: 10.1016/j.jshs.2019.04.002 [Crossref]
- Simpson RJ, Campbell JP, Gleeson M, Krüger K, Nieman DC, Pyne DB et al. Can exercise affect immune function to increase susceptibility to infection? Exerc Immunol Rev 2020;26:8-22.Available from: http://eir-isei.de/2020/eir-2020-008-article.pdf
- Wu Y, Ho W, Huang Y, Jin D-Y, Li S, Liu S-L et al. SARS-CoV-2 is an appropriate name for the new coronavirus. Lancet 2020;395(10228):949–50. doi: 10.1016/S0140-6736(20)30557-2 [Crossref]
- Simpson RJ, Katsanis E. The immunological case for staying active during the COVID-19 pandemic. Brain Behav Immun 2020:87:6-7. doi: 10.1016/j.bbi.2020.04.041 [Crossref]
- Medicine AAC of S. Staying physically active during
the COVID-19 Pandemic 2020 [cited 2020 May 8]. p.2.
Available from:
https://www.acsm.org/read-research/newsroom/news-releases/news-detail/2020/03/16/staying-physically-active-during-covid-19-pandemic
- Raiol RA. Praticar exercícios físicos é fundamental para a saúde física e mental durante a pandemia da COVID-19. Brazilian Journal of Health Review 2020;3:2804-13. doi: 10.34119/bjhrv3n2-124 [Crossref]
- Chen P, Mao L, Nassis GP, Harmer P, Ainsworth BE, Li F. Coronavirus disease (COVID-19): The need to maintain regular physical activity while taking precautions. J Sport Heal Sci 2020;9(2):103-4. doi: 10.1016/j.jshs.2020.02.001 [Crossref]
- Souza MT, Silva MD, Carvalho RD. Integrative review: what is it? How to do it? Einstein (São Paulo) 2010;8(1):102-6. http://doi.org/10.1590/s1679-45082010rw1134 [Crossref]
- Beyea SC. Writing an integrative review. AORN J 1998;67(4):877-80. doi: 10.1016/s0001-2092(06)62653-7 [Crossref]
- Moher D, Altman DG, Liberati A, Tetzlaff J. PRISMA Statement. Epidemiology 2011;22(1):128. doi: 10.1097/EDE.0b013e3181fe7825 [Crossref]
- Shirvani H, Rostamkhani F. Exercise considerations during coronavirus disease 2019 (COVID-19) Outbreak: A narrative review. J Mil Med 2020;22(2):161-8. doi: 10.30491/JMM.22.2.161 [Crossref]
- Zhu W. Should, and how can, exercise be done during a coronavirus outbreak? An interview with Dr. Jeffrey A. Woods J Sport Heal Sci 2020;9(2):105-7. doi: 10.1016/j.jshs.2020.01.005 [Crossref]
- Hammami A, Harrabi B, Mohr M, Krustrup P. Physical activity and coronavirus disease 2019 (COVID-19): specific recommendations for home-based physical training. Manag Sport Leis 2020;0(0):1-6. doi: 10.1080/23750472.2020.1757494 [Crossref]
- Jakobsson J, Malm C, Furberg M, Ekelund U, Svensson M. Physical activity during the coronavirus (COVID-19) pandemic: prevention of a decline in metabolic and immunological functions. Front Sport Act Living 30 abr 2020. doi: 10.3389/fspor.2020.00057 [Crossref]
- Hall G, Laddu DR, Phillips SA, Lavie CJ, Arena R. A tale of two pandemics: How will COVID-19 and global trends in physical inactivity and sedentary behavior affect one another? Prog Cardiovasc Dis 2020;40:4-6. doi: 10.1016/j.pcad.2020.04.005 [Crossref]
- Goethals L, Barth N, Guyot J, Hupin D, Celarier T. Need for a physical activity promotion strategy for older adults living at home during quarantine due to Table of Contents. JMIR Aging 2020;3(1):e19007. doi: 10.2196/19007 [Crossref]
- Azizi GG, Orsini M, Dortas Júnior SD, Cerbino SA. Obesidade e imunologia do exercício: implicações em tempos de pandemia de COVID-19. Rev Bras Fisiol Exerc 2020;19(2supl):S35-S39. doi: 10.33233/rbfe.v19i2.4023 [Crossref]
- Pitanga FJG, Beck CC, Pitanga CPS. Atividade física e redução do comportamento sedentário durante a pandemia do Coronavírus. Arq Bras Cardiol 2020;114(6):1058-60. doi: 10.36660/abc.20200238 [Crossref]
- Cheval B, Sivaramakrishnan H, Maltagliati S, Fessler L, Forestier C, Sarrazin P, et al. Relationships between changes in self-reported physical activity and sedentary behaviours and health during the coronavirus (COVID-19) pandemic in France and Switzerland. SportRxiv 25 apr 2020. doi: 10.1080/02640414.2020.1841396 [Crossref]
- Oliveira Neto L, Elsangedy HM, Tavares VDO, Teixeira CVLS, Behm DG DS-GM. #TreineEmCasa – Treinamento físico em casa durante a pandemia do COVID-19 (SARS-COV2): abordagem fisiológica e comportamental. Rev Bras Fisiol Exerc 2020;19(2):S9-S19. doi: 10.33233/rbfe.v19i2.4006 [Crossref]
- Rahmati-Ahmadabad S, Hosseini F. Exercise against SARS-CoV-2 (COVID-19): Does workout intensity matter? (A mini review of some indirect evidence related to obesity). Obes Med 2020;2:100245. doi: 10.1016/j.obmed.2020.100245 [Crossref]
- Chen P, Mao L, Nassis GP, Harmer P, Ainsworth BE, Li F. Returning Chinese school-aged children and adolescents to physical activity in the wake of COVID-19: Actions and precautions. J Sport Heal Sci 2020;9(4):322-24. doi: 10.1016/j.jshs.2020.04.003 [Crossref]
- Martin SA, Pence BD, Woods JA. Exercise and respiratory tract viral infections. Exerc Sport Sci Rev 2009;37(4):157-64. doi: 10.1097/JES.0b013e3181b7b57b [Crossref]
- Harris MD. Infectious disease in athletes. Curr Sports Med Rep 2011;10(2):84-9. doi: 10.1249/JSR.0b013e3182142381 [Crossref]
- Sallis J. A
call to action: physical activity and COVID-19. EIM Blog. American College of
Sports Medicine. [cited
2020 Apr 16]. Available from:
https://www.exerciseismedicine.org/support_page.php/stories/?b=896
- Dimitrov S, Hulteng E, Hong S. Inflammation and exercise: Inhibition of monocytic intracellular TNF production by acute exercise via b 2 -adrenergic activation. Brain Behav Immun 2017;61:60-8. doi: 10.1016/j.bbi.2016.12.017 [Crossref]
- Ahmadinejad Z, Alijani N, Mansori S, Ziaee V. Common sports-related infections: a review on clinical pictures, management and time to return to sports. Asian J Sports Med 2014;5(1):1-9. doi: 10.5812/asjsm.102630 [Crossref]
- Cerqueira E, Marinho DA, Neiva HP, Lourenço O. Inflammatory effects of high and moderate intensity exercise - a systematic review. Front Physiol 202;9(10):1-14. doi: 10.1016/j.obmed.2020.100245 [Crossref]
- Nyenhuis SM, Greiwe J, Zeiger JS, Nanda A, Cooke A. Exercise and Fitness in the age of social distancing during the COVID-19 Pandemic. J Allergy Clin Immunol Pract 2020;8(7):2152-55. doi: 10.1016/j.jaip.2020.04.039 [Crossref]
- Blocken B, Malizia F, van Druenen T, Marchal T. Towards aerodynamically equivalent COVID19 1.5 m
social distancing for walking and running [Internet]. Urban Physics 2020
[cited 2020 may 11]. Available from: http://www.urbanphysics.net/Social Distancing v20_White_Paper.pdf
- Azizi GG, Orsini M, Dortas Júnior SD, Vieira PC, Carvalho RS, Pires CSR et al. COVID-19 e atividade física: qual a relação entre a imunologia do exercício e a atual pandemia? Rev Bras Fisiol Exerc 2020;19(2supl):S20-S29. doi: 10.33233/rbfe.v19i2.4115 [Crossref]
- Guimarães-Ferreira L, Bocalini DS. Atenuação do destreinamento durante a pandemia de COVID-19: considerações práticas para o treinamento de força e potência em ambiente doméstico. Rev Bras Fisiol Exerc 2020;19(2supl):S47-S55. doi: 10.33233/rbfe.v19i2.4112 [Crossref]