Rev Bras Fisiol Exerc 2021;20(1):73-82
doi: 10.33233/rbfex.v20i1.4277
REVIEW
Quality analysis of current research on
temporomandibular disorders in professional athletes
Análise
da qualidade da pesquisa atual sobre desordens temporomandibulares em atletas
profissionais
Cornelis
Robert Springer1, Tatiana Lima Boletini1, Bárbara Capitanio de Souza2, André Luiz Lopes2,
Cristina Carvalho de Melo1, Franco Noce1
1Universidade Federal de Minas Gerais,
Belo Horizonte/MG, Brasil
2Universidade Federal do Rio Grande do
Sul, Porto Alegre/RS, Brasil
Received: July 17, 2020; accepted: December 7, 2020.
Correspondence: Cornelis Robert Araujo Springer,
Avenida Raja Gabaglia, 3950, 30350-540 Belo
Horizonte, MG, Brasil
Cornelis Robert
Springer: cornelisspringer@gmail.com
Tatiana Lima Boletini:
tatianaboletini@yahoo.com.br
Bárbara Capitanio de Souza:
barbara.capitanio@gmail.com
André Luiz Lopes: andregym23@hotmail.com
Cristina Carvalho de Melo: carvalho.cristina@gmail.com
Franco Noce: fnoce@hotmail.com
Abstract
Objective: To carry out a systematic review
to verify the latest scientific findings related to temporomandibular disorders
in professional athletes. Methods: For the studies' selection, PubMed, SPORTDiscus, Lilacs, ScienceDirect Journals (Elsevier), Web
of Science, and Scopus databases were used. The full texts of the qualified
publications were read and selected for the final decision, meeting the
inclusion criteria, after discussion between two reviewers. Newcastle-Ottawa
Quality Assessment Scale was used for qualitative analysis of the studies. The
risk of bias was also assessed in seven categories: selection bias, study
design, confounding factors, blinding, data collection methods, integrity, and
intervention analysis. Data analysis was performed by two examiners
independently. Results: The review included 6 independent studies. Most
of the articles suffer from uncertainties regarding the selection of the sample
and blinding of the evaluations and analyzes. Only two of the studies carried
out an outline to control possible confounding factors. Conclusion:
Studies on temporomandibular disorders help in the identification and
clarification of risk factors that may be prevalent for these subjects, as well
as contributing to the development of control and treatment strategies in the
case of the presence of these diseases. However, research in this area,
especially considering the patient athlete, is incipient, indicating the need
for further investigation on the subject.
Keywords: oral health;
temporomandibular joint dysfunction syndrome;
temporomandibular joint; sports medicine; dentistry.
Resumo
Objetivo: Realizar uma revisão sistemática para
verificar os últimos achados científicos relacionados à desordem
temporomandibular em atletas profissionais. Métodos: Para a seleção de
estudos, foram utilizados os bancos de dados PubMed, SPORTDiscus, Lilacs, ScienceDirect Journals
(Elsevier), Web of Science e Scopus. Os textos
completos das publicações qualificadas foram lidos e selecionados para decisão
final, atendendo aos critérios de inclusão, após discussão entre dois
revisores. Foi utilizada a Newcastle Ottawa Quality
Assessment Scale para análise qualitativa dos
estudos. O risco de viés também foi avaliado em sete categorias: viés de
seleção, desenho do estudo, fatores de confusão, cegamento, métodos de coleta
de dados, integridade e análise da intervenção. A análise dos dados foi
realizada por dois examinadores de forma independente. Resultados: A
revisão incluiu 6 estudos independentes. A maior parte dos artigos sofre de
incertezas quanto a seleção da amostra e cegamento das avaliações e das análises.
Apenas dois dos estudos realizam um delineamento com o objetivo de controlar
possíveis fatores de confusão. Conclusão: Os estudos sobre a desordem
temporomandibular auxiliam na identificação e no esclarecimento dos fatores de
risco que podem ser preponderantes para estes sujeitos, assim como contribuem
para a elaboração de estratégias de controle e tratamento no caso da presença
destas doenças. Entretanto, as pesquisas nesta área, especialmente considerando
o paciente atleta, são incipientes, indicando a necessidade de uma investigação
mais aprofundada sobre o tema.
Palavras-chave: saúde bucal; síndrome da disfunção da
articulação temporomandibular; articulação temporomandibular; medicina
esportiva; odontologia.
Introduction
Amateur and
professional athletes seek to improve their competitive results routinely by
recruiting physiological stimuli. Many of these mechanisms, at some point, can
cause non-functional disorders. The American Academy of Orofacial Pain (AAOP)
defines temporomandibular disorders (TMD) as changes that involve different
problems associated with the muscles of the masticatory system, the
temporomandibular joint (TMJ) and other adjacent structures, in the presence of
painful symptoms, joint noise, and restriction of movements [1,2]. The etiology
of TMD is multifactorial and covers different factors among individuals, being
responsible for the appearance of signs and symptoms related to the
stomatognathic system, compromising the functions related to the structures
involved [3,4].
According to the
range of functions of the structures that may be compromised during the
existence of TMD, we can observe the presence of clinical problems, including
muscle pain, joint pain, and TMJ degeneration, displacement of the articular
disk, difficulty in chewing, swallowing and in speech, reduced range of motion
and mandibular deviation during TMJ function [3,4]. Besides, TMDs can
negatively influence the individual's mental health, affecting school
performance, work, and social activities, plus contributing to the appearance
of affective and cognitive problems [5,6].
TMDs, as they
eventually present very important symptomology, can limit the willingness of
individuals to perform sports, which, in a way, can increase their
consequences, as regular physical activity helps to control pain and other
symptoms, and may even reduce treatment costs for chronic conditions [7]. The
practice of regular physical activity or physical exercise is a relatively
accessible, safe, and low-cost activity, which can bring numerous important
improvements to the lives of practitioners, improving general muscle
conditioning, body composition and positively affecting the health of the
subjects [8,9].
Studies that
evaluate the athlete's routine or the performance of their activities in
competitions and the conditions that involve oral health are increasingly in
evidence. The research seeks to understand how these conditions can be related
and what impacts the athlete's development. Oral diseases such as TMD can have
consequences that modify some aspects of individuals' physical and mental
well-being and can, therefore, be a potentially significant factor when we
think about developing sports performance [5]. Besides, the limitation of
functional activities ends up potentiating forms of psychological suffering
such as anxiety, stress, and depression, causing social impairment, reduced
work capacity, physical disability, and increased social costs [10,11].
Understanding
the health conditions and oral and orofacial diseases is very important for
professionals who work with athletes since the disorders that affect this
region can harm people's lives, as well as limit the practice of sport and the
encouragement to perform physical activities, which can be even more crucial
when we think about the professional athlete. Thus, considering the importance
of high-performance sports, the objective of the study was to conduct a
systematic review of the literature, to verify the quality of the studies that
investigate TMDs in professional athletes.
Methods
This systematic
review was registered in PROSPERO under the code CRD42020164929 and was
conducted according to the guidelines described in Preferred Reporting Items
for Systematic Reviews and Meta-analyzes - PRISMA statement (Figure 1) [12].
Search strategy
For the studies'
selection, the databases PubMed, SPORTDiscus, Lilacs,
ScienceDirect Journals (Elsevier), Web of Science, and Scopus were used. As the
surveys were carried out during May 2019, the works published up to the search
time were included. The selection of studies was performed using the following
combination of descriptors: ("Temporomandibular Joint Syndrome" OR
"Temporomandibular Dysfunction*" OR "Temporomandibular
syndrome*" OR "TMJ Syndrome" OR "TMJ Dysfunction*" OR
"TMJ Disorder*" OR "temporomandibular disorder") AND
("athlete*" OR "sport*"). All research was limited to
studies in humans.
Eligibility and data extraction
All selected
references were managed in the EndNote X7 bibliographic software. Subsequently,
all duplicate references were deleted. The inclusion criteria were as follows:
1) observational studies, 2) studies that analyzed TMD in professional
athletes, using any evaluation method, and 3) complete studies published in
English. Two independent reviewers (CRS and TLB) selected the references
retrieved through the titles and abstracts of the publications, to test them
according to the eligibility criteria for inclusion in the review. The full
texts of the qualified publications were read and selected for a final
decision, meeting the inclusion criteria, after discussion between the two
reviewers. The resulting references were managed in an Excel file (Excel® -
Microsoft Corporation, Redmond, Washington), listing their year of publication,
the author's first name, title, journal, and reason for exclusion. There was no
restriction on the year of publication. The search started identified 212
articles. After removing duplicate papers, the titles, and abstracts of the
resulting 130 studies were evaluated. 26 eligible papers were read in full and
assessed for selection criteria. 20 articles were excluded because they did not
address the proposed theme of this review. After selection for review, the
following data were extracted from each article; author, sample
characteristics, sport practiced, objectives, type of study, main results, and
value of the Newcastle-Ottawa Quality Assessment Scale (NOS).
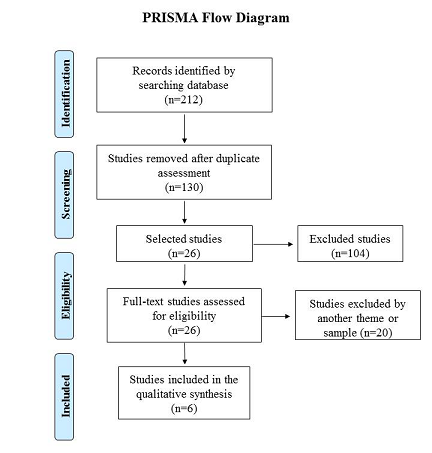
Figure 1 - Flow diagram of research and
selection of literature, according to the PRISMA statement
Quality assessment and risk of bias
The reviewers independently assessed the risk of bias in the included studies, using the Newcastle-Ottawa Quality Assessment Scale (NOS). The NOS assigned a score ranging from zero to nine stars for each article, in which a larger number of stars indicates a higher quality study. Moreover, the risk of bias was also assessed in seven categories: selection bias, study design, confounding factors, blinding, data collection methods, integrity, and intervention analysis. Each section was judged on low risk, moderate risk, or high risk, based on the study's description. The NOS scale and its usage guidelines are available in full at http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
Data analysis
CRS and TLB
independently evaluated each study, considering seven items of risk of bias
(selection bias, study design, confounding factors, blinding, data collection
methods, integrity, and analysis of the intervention). Disputes were resolved
through a third reviewer (BCS). The critical analysis also considered the
approach adequacy, using criteria with the sample selection method, blinding,
control of variables, target population, the analysis performed, according to
the type of study and the NOS scale.
Results
Description of selected studies
The search in
the databases initially identified 212 articles, of which 82 were excluded
because they were duplicates and 104 were excluded after reviewing the title
and abstract (figure 1). Of the 26 resulting studies, 20 studies were excluded
in the last stage of the selection evaluations because they did not correspond
to the proposed theme or use another type of sample. Thus, the systematic
review included 6 independent studies. The characteristics of the included
studies are summarized in Table I. Among these studies, three were carried out
in Brazil, one in Spain, one in Turkey, and one in Australia. According to the
study design, three were cross-sectional observational studies, a case-control
study, a case report, and the other was a series of cases. Among the sports
evaluated, we find cycling, basketball, boxing, handball, karate, and Mixed
Martial Arts (MMA). Regarding the quality of the study, the NOS score ranged
from 1 to 9.
Table I - Basic characteristics of the
included studies (see PDF annexed)
Quality of the studies
Most of the
articles suffer from uncertainties that could be the cause of the bias, as
follows: four articles did not mention how the sample size was calculated, to
guarantee the power of the study, or indicate only that the sample was for
convenience [13,14,15,16]. Only two articles register that the sample calculation was
performed, considering the established variables [17,18]. Also, we can observe
the lack of procedures that guarantee the blindness of the evaluators [13-16].
Two of the studies carried out a methodological design to control possible
confounding factors that could potentially interfere with the results [17,18].
Taking this into account, the methodological quality of the six articles
evaluated presented a risk of high bias in one study [13], moderate in three
studies [14,15,16] and low in two [17,18] (Figure 2).
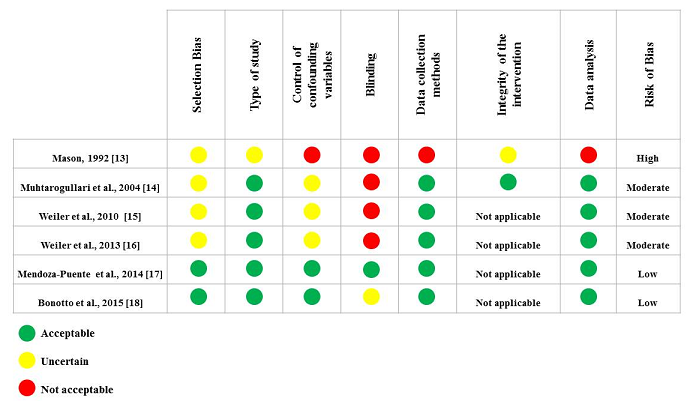
Figure 2 - Assessment of the studies’
methodological quality
Discussion
It was possible
to verify that a small number of studies were selected to compose this review,
possibly due to the lack of work on this topic, for this population in
particular, and because sports dentistry is a relatively new specialty in most
countries, compared to other dentistry specialties. No studies were identified
addressing the possible causes of TMD in athletes, nor about the relationship
of this disorder with other variables in the sports field, such as stress,
mood, anxiety, motivation, resilience, burnout, among others. Only one study
showed results on the consequences of TMD in sportspeople [17], the others
investigated the prevalence of this dysfunction [15,16,18] or reported cases
with clinical interventions [13,14]. This research suggests that we know little
about TMD in athletes and that the moderate prevalence of this disorder in this
population group should be considered to guide further studies in the area.
Considering the
criteria of the qualitative analysis, it was possible to observe that the
studies, in general, have significant methodological problems such as the lack
of sample calculation and blinding methods during the evaluations. These
criteria confer representativeness, power, and reliability of the data.
Likewise, the control of confounding variables is essential when analyzing
complex conditions such as TMD. The athlete patient has specific risk factors
related to the modalities of the sport practiced, such as, for example, the
occurrence of orofacial trauma and periods of tension and stress, which can
favor the onset of this disease or crucial symptoms in the TMJ region [19,23].
Studies with a
low bias risk present interesting results regarding their findings. Fight
sports athletes have increased excitability in the trigeminal nerve's sensory
branches and the masseter muscle, a higher report of orofacial and head pain,
as well as a greater risk of TMD when compared to other sports [17,18]. Disc
displacement was the most common TMD subtype among professional athletes
practicing martial arts [18]. The results of the studies suggest that the
pathology investigated may have a higher prevalence in these athletes, as well
as having risk factors conditioned to the sport.
TMDs correspond
to a group of musculoskeletal disorders that affect the masticatory muscles
and/or the temporomandibular joint and have a relevant prevalence in the
population, being reported that it is possible to find some pathological
symptom in almost 60% of individuals [19]. The etiology of these conditions is
widely studied, but still little known, considering the magnitude of its influence
on the development of TMD, and reports of different influencing factors can be
found, such as occlusion, parafunction, emotional stress, hormonal changes,
physical trauma, microtrauma in teeth, joint hypermobility, and some dental
treatments [20,21]. As it presents a significant potential for comorbidity,
influencing people's habits and quality of life, the study of TMDs is relevant,
since their better understanding contributes to a more accurate clinical
practice [22].
There is a
growing increase in studies that correlate the quality of life or the
performance of individuals' routine activities and the conditions that involve
oral health. These surveys seek to clarify how these conditions are related and
what importance they represent in people's lives. Situations related to oral
health and the stomatognathic system, such as TMD, can have consequences that
modify some aspects of individuals' physical and mental well-being and, by
extension, we can also suggest that these conditions may have an impact on
sports activity [5]. The pains and symptoms reported are commonly located in
the masticatory muscles and the preauricular region, which can be easily
exacerbated by chewing and by the jaw movement activity, resulting from the
body's natural physiological functions. These factors are expressive when
considering a professional athlete who needs a constant physical and mental
effort to carry out all their training and competitions routine [11].
As TMD can also
involve other conditioning factors such as psychological conditions, anxiety,
tension, pain, and even disorders related to changes in the spine, [24] it is
necessary to understand its causes and consequences in sports, as well as its
interference in the physical and emotional activities of the athletes, who are
subject to numerous situations during sports activities, involving training and
competitions. The results of this review showed us that little is known about
the mechanisms of TMD development in athletes and much can be studied and discussed
to understand the role of this pathology on the sports patient.
Limitations and recommendations for further studies
Among the
detected limitations, the selection and dimensioning of the samples, the
criteria for blinding the evaluators, and the control of confounding variables
are highlighted. Most studies have a small and convenient sample, composed of
selected volunteers, which reduces the representativeness of the information
obtained. The sample size calculation must be performed to improve the
quantitative analyzes of the studies. Furthermore, researches could be carried
out with athletes from different sports to check if there is any difference
between the risk factors for the development of TMD and relevant data on the
prevalence of this situation, according to the sport practiced. Another
possible evaluation method could consider the training experience, comparing
the occurrence of changes in the TMJ of amateur and professional athletes. As
it is a condition that can comprise different risk factors, a multivariate
analysis could be considered to identify a cut-off point on the number of
exposure factors necessary to cause significant damage to the development of
routine activities of a patient athlete.
Conclusion
Research on the
proposed topic is still very incipient, indicating the need for more accurate
research on the subject. The athlete's evolution within the sport modality, as
to his performance, depends on the physical preparation and the harmony of physical,
psychological, and biological factors. Thus, studies on TMD in athletes can
help to identify and clarify risk factors for sports performance.
Potential conflict of interest
No conflicts of interest with potential for this
article have been reported.
Financing source
Non-applicable.
Academic linkage
This study is linked to The Postgraduate Program in
Sport Science - PPGCE, from the Federal University of Minas Gerais.
Authors' contribution
Conception and design of the research: CRS, TLB, FN.
Data collection: CRS, TLB. Analysis and interpretation of data: CRS, BCS.
Writing of the manuscript: CRS, BCS. Critical review of the manuscript for
important intellectual content: ALL, CCM, FN.
References
- Adèrn B, Stenvinkel C, Sahlqvist L, Tegelberg ÅK. Prevalence of temporomandibular dysfunction
and pain in adult general practice patients. Acta Odontol Scand
2014;72:585-90. doi: 10.3109/00016357.2013.878390 [Crossref]
- Mello VV, Barbosa AC, Morais MP, Gomes SG, Vasconcelos MM, Caldas Júnior AF. Temporomandibular disorders in a sample population of the Brazilian Northeast. Braz Dent J 2014;25:442-6. doi: 10.1590/0103-6440201302250 [Crossref]
- Marklund S, Wänman A. Risk factors associated with incidence and persistence of signs and symptoms of temporomandibular disorders. Acta Odontol Scand 2010;68:289-99. doi: 10.3109/00016357.2010.494621 [Crossref]
- Trize DM, Calabria MP, Franzolin S, Cunha CO, Marta SN. Is quality of life affected by temporomandibular disorders? Einstein 2018;16:eAO4339. doi: 10.31744/einstein_journal/2018AO4339 [Crossref]
- Dahlström L, Carlsson GE. Temporomandibular disorders and oral health-related quality of life. A systematic review. Acta Odontol Scand 2010;68:80-5. doi: 10.3109/00016350903431118 [Crossref]
- Resende CM, Alves AC, Coelho LT, Alchieri JC, Roncalli AG, Barbosa GA. Quality of life and general health in patients with temporomandibular disorders. Braz Oral Res 2013;27:116-21. doi: 10.1590/s1806-83242013005000006 [Crossref]
- Geneen LJ, Moore RA, Clarke C, Martin D, Colvin LA, Smith BH. Physical activity and exercise for chronic pain in adults: an overview of Cochrane Reviews. Cochrane Database Syst Rev 2017;1:CD011279. doi: 10.1002/14651858.CD011279 [Crossref]
- Speck RM, Courneya KS, Mâsse LC, Duval S, Schmitz KH. An update of controlled physical activity trials in cancer survivors: a systematic review and meta-analysis. J Cancer Surviv 2010;4:87-100. doi: 10.1007/s11764-009-0110-5 [Crossref]
- Cormie P, Zopf EM, Zhang X, Schmitz KH. The impact of exercise on cancer mortality, recurrence, and treatment-related adverse effects. Epidemiol Vern 2017;39:71-92. doi: 10.1093/epirev/mxx007 [Crossref]
- Castro AR, Siqueira SRDT, Perissinotti DMN, Siqueira JTT. Psychological evaluation and cope with trigeminal neuralgia and temporomandibular disorder. Arq Neuropsiquiatr 2018;66:716-9. doi: 10.1590/s0004-282x2008000500021 [Crossref]
- Cioffi I, Perrotta S, Ammendola L, Cimino R, Vollaro S, Paduano S et al. Social impairment of individuals suffering from different types of chronic orofacial pain. Prog Orthod 2014;15:27. doi: 10.1186/s40510-014-0027-z [Crossref]
- Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA Statement. PLoS Med 2009;6:e1000097. doi: 10.1371/journal.pmed1000097 [Crossref]
- Mason R. Sport TMJ dysfunction. Case report. Aust Dent J 1992;37:472. doi: 10.1111/j.1834-7819.1992.tb05904.x [Crossref]
- Muhtaroğullari M, Demiralp B, Ertan A. Non-surgical treatment of sports-related temporomandibular joint disorders in basketball players. Dent Traumatol 2004;20:338-43 doi: 10.1111/j.1600-9657.2004.00267.x [Crossref]
- Weiler RM, Vitalle MS, Mori M, Kulik MA, Ide L, Pardini SR et al. Prevalence of signs and symptoms of temporomandibular dysfunction in male adolescent athletes and non-athletes. Int J Pediatr Otorhinolaryngol 2010;74:896-900. doi: 10.1016/j.ijporl.2010.05.007 [Crossref]
- Weiler RM, Santos FM, Kulic MA, De Souza Lima MP, Pardini SR, Mori M et al. Prevalence of signs and symptoms of temporomandibular dysfunction in female adolescent athletes and non-athletes. Int J Pediatr Otorhinolaryngol 2013;77:519-24. doi: 10.1016/j.ijporl.2012.12.024 [Crossref]
- Mendoza-Puente M, Oliva-Pascual-Vaca Á, Rodriguez-Blanco C, Heredia-Rizo AM, Torres-Lagares D, Ordoñez FJ. Risk of headache, temporomandibular dysfunction, and local sensitization in male professional boxers: a case-control study. Arch Phys Med Rehabil 2014;95:1977-83. doi: 10.1016/j.apmr.2014.06.011 [Crossref]
- Bonotto D, Namba EL, Veiga DM, Wandembruck F, Mussi F, Cunali PA et al. Professional karate-do and mixed martial arts fighters present with a high prevalence of temporomandibular disorders. Dent Traumatol 2016;32:281-5. doi: 10.1111/edt.12238 [Crossref]
- Ebrahimi M, Dashti H, Mehrabkhani M, Arghavani M, Daneshvar-Mozafari A. Temporomandibular disorders and related factors in a group of Iranian adolescents: a cross-sectional survey. J Dent Res Dent Clin Dent Prospects 2011;5:123-7. doi: 10.5681/joddd.2011.028 [Crossref]
- Sari S, Sonmez H. Investigation of the relationship between oral parafunctions and temporomandibular joint dysfunction in Turkish children with mixed and permanent dentition. J Oral Rehabil 2002;29:108-12. doi: 10.1046/j.1365-2842.2002.00781.x [Crossref]
- Winocur E, Littner D, Adams I, Gavish A. Oral habits and their association with signs and symptoms of temporomandibular disorders in adolescents: a gender comparison. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006;102:482-7. doi: 10.1016/j.tripleo.2005.11.007 [Crossref]
- Saha FJ, Pulla A, Ostermann T, Miller T, Dobos G, Cramer H. Effects of occlusal splint therapy in patients with migraine or tension-type headache and comorbid temporomandibular disorder: A randomized controlled trial. Medicine Baltimore 2019;98:16805. doi: 10.1097/MD.0000000000016805 [Crossref]
- Maydana AV, Tesch RS, Denardin OVP, Ursi WJS, Dworkin SF. Possíveis fatores etiológicos para desordens temporomandibulares de origem articular com implicações para diagnóstico e tratamento. Dental Press J Orthod 2010;15:78-86. doi: 10.1590/S2176-94512010000300010 [Crossref]
- Sambataro S, Cervino G, Bocchieri S, La Bruna R, Cicciù M. TMJ dysfunctions systemic implications and postural assessments: a review of recent literature. Journal of Functional Morphology and Kinesiology 2019;4:58. doi: 10.3390/jfmk4030058 [Crossref]