Rev Bras Fisiol Exerc 2021;20(1):27-37
doi: 10.33233/rbfex.v20i1.4340
ORIGINAL ARTICLE
Relationship of obstructive sleep apnea with oxygen
consumption, physical activity, and diet
Relação
da apneia obstrutiva do sono com consumo de oxigênio, atividade física e
alimentação
Einstein
Zeus Alves de Brito1,2,3, Manoel Pereira Guimarães3,4,
Danilo Sobral da Silva Fernandes1,2,3, Victor Ribeiro Neves3,
Bruno Bavaresco Gambassi3,6, Paulo Adriano
Schwingel3,6, Fabrício Olinda de Souza Mesquita1,3,4,6,7
1Faculdade São Francisco de Juazeiro,
Juazeiro, BA, Brasil.
2Instituto Valler
Medicina Integrada, Juazeiro, BA, Brasil
3Universidade de Pernambuco, Petrolina,
PE, Brasil
4Universidade Federal do Vale do São
Francisco, Petrolina, PE, Brasil
5Universidade Ceuma,
São Luís, MA, Brasil
6Universidade de Pernambuco, Recife, PE,
Brasil
7Empresa Brasileira de Serviços
Hospitalares (EBSERH), Petrolina, PE, Brasil
Received:
2020, August 13; accepted 2020, November
30.
Correspondence: Fabrício Olinda de Souza Mesquita, Hospital Universitário
da Universidade Federal do Vale do São Francisco (HU-UNIVASF), Av. José de Sá
Maniçoba, s/n Centro 56304-205 Petrolina, PE, Brasil
Einstein Zeus Alves de Brito: einsteinzeus@outlook.com
Manoel Pereira Guimarães: manoelpeguimaraes@gmail.com
Danilo Sobral da Silva Fernandes:
danilosobra@gmail.com
Victor Ribeiro Neves: victor.neves@upe.br
Bruno Bavaresco Gambassi:
professorbrunobavaresco@gmail.com
Paulo Adriano Schwingel: paulo.schwingel@upe.br
Fabrício Olinda de Souza Mesquita:
fabricioolinda@hotmail.com
Abstract
Objective: To evaluate the maximum oxygen
consumption (VO2max), physical activity level, food consumption and
quality of life in patients with obstructive sleep apnea (OSA). Methods:
Descriptive qualitative and quantitative study with cross-sectional analysis
based on the application of structured questionnaires, carried out in a private
clinic at Petrolina/PE, Brazil. Quality of life was
assessed by the WHOQOL-bref, food consumption using
the form of food consumption markers contained in the SISVAN Protocol, and the
level of physical activity by the IPAQ short version. Results: Of the 16
included patients, 6 had no OSA, 4 had mild OSA, 2 had moderate OSA, and 4 had
severe OSA. Sedentary lifestyle was prevalent in 20% of the patients with mild
OSA, in 50% of those with moderate OSA and in 75% of those with severe OSA.
Healthy food consumption prevailed in all groups, with a higher consumption of
unhealthy foods in the severe OSA group. A predominance of regular quality of
life was identified in all groups, especially needing to improve the physical
domain of all of them. Both VO2max and the anaerobic threshold
showed reduced values as the severity of the disease increased, with lower
values in patients with the most severe form of the disease. Conclusion:
An inverse relationship was found between more severe OSA with VO2max
and the levels of physical activity of the patients analyzed. There is a
greater consumption of unhealthy foods with poor diet and sedentary behavior
that are important risk factors for the development and worsening of the
disease.
Keywords: food intake; exercise; quality of
life; sleep obstructive apnea; sedentary behavior.
Resumo
Objetivo: Avaliar o consumo máximo de oxigênio
(VO2máx), nível de atividade física, consumo alimentar e qualidade
de vida em pacientes com apneia obstrutiva do sono (AOS). Métodos:
Estudo descritivo quali-quantitativo com análise
transversal a partir de aplicação de questionários estruturados, realizado em
uma clínica privada de Petrolina, PE. A qualidade de vida foi avaliada pelo
WHOQOL-bref, o consumo alimentar pelo formulário de
marcadores do consumo alimentar que consta no Protocolo do SISVAN e o nível de
atividade física pela versão curta do IPAQ. Resultados: Dos 16 pacientes
incluídos, 6 não tinham AOS, 4 apresentaram AOS leve, 2 AOS moderada e 4 AOS grave. Sedentarismo foi prevalente em 20% dos pacientes
com AOS leve, em 50% dos com AOS moderada e em 75% dos com AOS
grave. Consumo alimentar saudável prevaleceu em todos os grupos, com
maior consumo de alimentos não saudáveis por pacientes com AOS
grave. Foi identificado predomínio de qualidade de vida regular em todos
os grupos, necessitando melhorar especialmente o domínio físico de todos eles.
Tanto VO2máx quanto o limiar anaeróbico apresentaram valores
reduzidos à medida que a gravidade da doença aumentava, sendo menores os
valores nos pacientes com a forma mais grave da doença. Conclusão: Foi
constatada relação inversa entre AOS mais grave com o VO2máx e os níveis de
atividade física dos pacientes analisados. Há um maior consumo de alimentos não
saudáveis com má alimentação e comportamento sedentário que constituem
importantes fatores de risco para o desenvolvimento e agravamento da doença.
Palavras-chave: consumo de alimentos; exercício
físico; qualidade de vida; apneia obstrutiva do sono; comportamento sedentário.
Introduction
Obstructive
sleep apnea (OSA) is characterized by repeated upper airway obstructions [1,2].
This disorder is highly prevalent and has a considerable influence on the
morbidity and mortality of the Brazilian population [2,3]. OSA may be
associated with the development of type II diabetes mellitus [2]. It is also a
risk factor for systemic arterial hypertension, stroke, depression, insomnia,
anxiety, and cardiovascular diseases [1,3]. Besides, it is known that the
drowsiness characteristic of this disorder is the cause of many traffic and
work accidents [1].
Advancing age is
the principal risk factor associated with OSA [4]. Also, sleep disorders are
correlated with decreased fiber intake, increased carbohydrate intake, and
increased fat consumption [5]. Obese patients are more likely to have a
positive OSA diagnosis, mainly due to the increased fat deposition in the neck
region. This increases the circumference of the cervical region and makes the
upper airways narrower, which leads to collapse during sleep [6].
The diagnosis
and severity of OSA are assessed using the apnea-hypopnea index (AHI) using
polysomnography. AHI is calculated by dividing the total number of apneas and
hypopneas by the number of hours of sleep. AHI is considered normal when less
than 5 events per hour occur, mild OSA between 5 and 14 events/hour, moderate
OSA between 15 and 29 events/hour, and severe OSA ≥ 30 events/hour [7,8].
As a result of
insomnia (morning headache, increased drowsiness, and fatigue) caused by
recurrent sleepless nights, patients with OSA tend to have multifactorial
changes in functional capacity, maximum oxygen consumption (VO2max),
and in their activities of daily living (ADLs) [9]. This favors an increased
risk for the onset of diseases and chronic conditions such as diabetes,
obesity, cardiovascular disease, and depression [10].
This work is
justified by the gaps concerning the study of OSA, mainly about data from
populations in the interior of the Brazilian Northeast. Thus, this study aims
to describe VO2max, level of physical activity, food consumption,
and quality of life in patients with OSA in the Vale do São Francisco region.
Methods
Study design
It is a
qualitative and quantitative analytical study using mixed methods of
investigation through the retrospective description of secondary data, obtained
through the medical records of the patients included in the study and
cross-sectional analysis using structured questionnaires. The research was
approved by the Research Ethics Committee of the Federal University of Vale do
São Francisco (UNIVASF), with a certificate of presentation for ethical
appreciation (CAAE) number 65947617.2.0000.5196.
Scenario
The study was
carried out between July 2015 and November 2017 in a private clinic at Petrolina/PE. Participants were invited to the place where
the study was carried out, where the informed consent form (ICF) was read in
conjunction with the researchers, and the questionnaires were properly applied.
At another time, data was collected from the medical records of patients who
adhered to the study.
Inclusion and exclusion criteria
The study
included patients who underwent polysomnography exams with ApneaLink
(Resmed, Sydney, Australia) and ergospirometry,
using Ergostik (Geratherm,
Bad Kissingen, Germany), during the period analyzed at the clinic. Patients
with medical records who presented incomplete data and those who did not have a
polysomnography report were excluded.
Data collection
Data collection
took place through the sample of patients at risk for OSA who underwent
polysomnography. This population was divided into groups according to the AHI:
Normal (≤ 5 events/hour), Mild (5-14 events/hour), Moderate (15-29
events/hour), and Severe (≥ 30 events/hour), which will serve as a basis
for correlations with secondary data [7,8].
Thus, the
application of questionnaires to analyze the quality of life (QoL), physical
activity level (PAL), and food consumption was performed with patients who
underwent the cardiopulmonary stress test (CPET) within the diagnosed
population. The parameters analyzed in CPET were VO2max and the
anaerobic threshold (AT).
The sample that
composed this study was obtained for convenience.
Quality of life assessment
QoL was assessed
using the World Health Organization Quality of Life Instrument Bref questionnaire (WHOQOL-bref)
translated and validated by the World Health Organization (WHO) in Brazil,
being considered an instrument that is easy to apply and understand for the
adult population. The WHOQOL-bref is the short
version of the WHOQOL 100 and consists of 26 questions. Two questions are about
the general quality of life, and 24 represent each of the 24 facets that make
up the original instrument. This instrument consists of four domains of quality
of life. Each of them aims to analyze, respectively, physical capacity,
psychological well-being, social relationships, and the environment where the
individual is inserted and is also composed of a domain that investigates the
global quality of life. Each field is composed of questions, whose response
scores vary between 1 and 5. The final scores for each domain are calculated
using a syntax, which considers the answers for each question that makes up the
domain, resulting in final scores on a scale of 1 to 5. Depending on the score,
the QoL of the population can be classified into four categories: needs
improvement (1 to 2.9), regular (3 to 3.9), good (4 to 4.9), or very good (5)
[11].
Physical activity level assessment
The PAL
evaluation was performed using the International Physical Activity
Questionnaire (IPAQ) in its short version, translated and validated for Brazil
[12]. Its questions are related to the time spent by the subject performing
physical activities in the last week, including the activities he did at his
workplace, to go from one place to another, for leisure and sports. The
analysis of the results is performed following the criteria of frequency,
duration, and intensity, classifying the individual as active, insufficiently
active, or sedentary. An individual is considered active if they reach the
following criteria: a) vigorous physical activity with a frequency equal to or
greater than three days per week with a duration equal to or greater than 20
minutes per session; b) moderate physical activity or walking with a frequency
equal to or greater than five days/week and duration equal to or greater than
30 minutes/session; c) any physical activity whose added frequency is equal to
or greater than five days/week and with a duration equal to or greater than 150
minutes/week. The subjects who did not reach the criteria were classified as
insufficiently active or sedentary according to the IPAQ standardization [12].
Food intake assessment
For the
assessment of food intake, the form of food consumption markers for individuals
older than five years of age was used, which appears in the Protocol of the
Food and Nutrition Surveillance System (SISVAN). This instrument seeks to
portray the usual food intake, which is a type of retrospective record of the
frequency of consumption of some foods and drinks in the last seven days of the
evaluation. The instrument is related both to a healthy diet (for example,
daily consumption of beans, fruits, and vegetables) and to practices that are
not recommended (frequent consumption of fried foods and sweets, for instance)
[13]. This form aims to identify the dietary pattern of the individual broadly,
not intending to quantify the diet in terms of calories and nutrients, but
rather to indicate the quality of the food in its positive and negative
characteristics [14].
Statistical analysis
Statistical
analysis was performed using the SPSS statistical package (SPSS Inc., Chicago,
IL, USA, Release 16.0.2, 2008). The normality and homoscedasticity of the data
were verified using a histogram following Bartlett's criteria. Continuous
variables are presented as mean ± standard deviation, while categorical
variables are presented using absolute and relative frequencies. One-way
analysis of variance (ANOVA) was used to compare the results obtained between
the groups studied. All analyzes performed were two-tailed, with the exact
values of P calculated at a significance level of 5%.
Results
Of the 446
individuals who underwent polysomnography from July 2015 to November 2017, 58
underwent CPET. Of these, 42 were excluded after applying the exclusion
criteria. The total sample of this study consisted of 16 individuals, of which 25%
(n = 4) of the patients had severe OSA, 12.5% (n = 2) moderate OSA, 25% (n = 4)
mild OSA and 37.5% (n = 6) normal results (without OSA). Table I presents the
general characterization of the sample.
Table I - Sample characterization
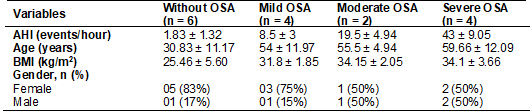
AHI =
apnea-hypopnea index; BMI = body mass index
Table II shows
the average values of VO2max and AT, relative to the total body mass
of everyone, stratified according to the severity of the disease. The analysis
of the ergospirometric data showed that the average
VO2max of the group without OSA was 19.9 ml/kg/min, this average
being reduced as the disease severity increased. The same happened with the AT,
which presented an average value of 12.2 ml/kg/min in the group without OSA and
was lower in patients who had the most severe forms of the disease.
Table II - Mean value of VO2max
and AT
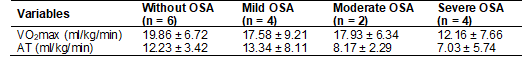
VO2max
= maximum oxygen consumption; AT = anaerobic threshold
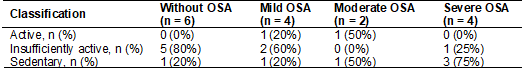
The data related
to PAL are shown in table III, showing sedentary behavior that is more
prevalent in groups with moderate and severe OSA.
Table III - Classification of physical
activity level
The analysis of
the QoL domains is described in table IV, in which in general is observed a
worsening of QoL as the severity of OSA increases.
Table IV - Classification of the level
of quality of life
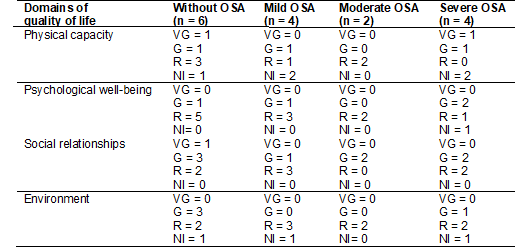
VG =
Very good; G = Good; R = Regular; NI = Needs improvement.
The results regarding
the analysis of the consumption of foods considered healthy or not are shown in
Graph 1. The group without OSA showed higher consumption of healthy foods when
compared to the other groups.
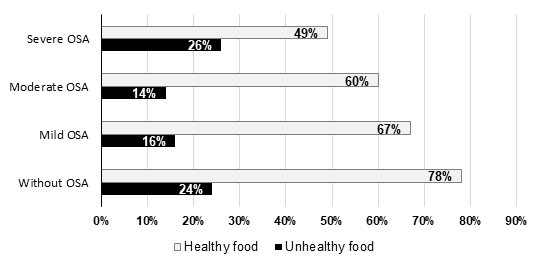
Graph 1 - Frequency of eating healthy
and unhealthy foods
Discussion
It was observed
in the present study that patients with a higher level of OSA severity have
lower VO2max when compared to the reference group (without OSA), in
the same way that these patients also present a higher frequency of sedentary
behavior and lower values of individual AT.
The results
found can be explained for several reasons. Initially, the lower VO2max in
the groups with OSA is possibly due to the decline in lung volume, which can
decrease tracheal traction forces [15]. Besides, the low PAL of patients with
OSA can also contribute to the reduced values of VO2max [16]. Low
PAL is associated with a higher degree of obesity that provides the
accumulation of fat in the cervical region and narrows the upper airways, worsening
OSA [15]. Therefore, the reduced values of the AT in the groups with OSA are
explained both by the reduced PAL itself and by the cardiovascular
comorbidities of these patients, mainly heart failure [17]. The low PAL
observed in groups with OSA is mainly due to obesity and the low quality of
sleep that causes daytime sleepiness [1,15].
It has also been
described, in the literature, that individuals with reduced VO2max tend
to have less physical and functional capacity [1,3,17]. This will directly
impact the ADLs of these individuals, as VO2max is an indicator of
cardiorespiratory resistance capacity and an important predictive parameter of
morbidities associated with OSA, such as heart failure, stroke, among others
that have been reported in similar studies [18]. Lin et al. [18] analyzed, in a
case-control study using CPET, 20 overweight patients who had OSA and found
that VO2max and performance during the test were significantly lower
(P < 0.05) in individuals who had OSA (21.6 ml/kg/min) compared to the
control group (30.2 ml/kg/min).
However, the
evidence in the literature has shown conflicting results. More recent studies
have not shown a significant difference in VO2max in patients with
and without OSA. Fernandez et al. [19] in a randomized clinical trial
that included 46 obese patients, 31 with OSA (mean AHI of 43.6 events/hour) and
15 who did not have the disease, found no difference in VO2peak of
the groups with OSA (25.0 ml/kg/min) and without OSA (25.3 ml/kg/min), as well
as there was no difference in AT (56.5 l/min vs. 56.1 l/min, respectively). In
short, it is not clear whether obesity or OSA can decrease individuals' maximum
oxygen consumption. Current findings suggest that OSA does not impair
individuals' functional capacity in terms of VO2max values.
Regarding the
level of physical activity analyzed using the IPAQ, it was seen that only 12.5%
of patients in the entire sample were considered active and 75% of patients
with severe OSA were considered sedentary, which corroborates the findings
regarding the VO2max of this study, since individuals in the severe
OSA group, in addition to having a low PAL, also obtained reduced values of VO2max.
In this sense, PAL demonstrates its importance as a VO2max
prediction parameter. The less active the individual is, the lower their VO2max
values tend to be [16,20]. These results are in line with other studies that
claim that sedentary and obese individuals have a greater propensity for a
positive diagnosis of the disease, with physical inactivity constituting one of
the main risk factors for its development, with physical exercise being a
fundamental integral in the treatment of OSA. Physical exercise has a range of
varieties and can be practiced even by diabetic individuals [21].
Aiello et al.
[22], in a meta-analysis, found that physical exercise was effective both in
improving OSA and in reducing the severity of the disease. However, the
mechanisms that lead to physical exercise to reduce the disease symptoms are
still not well understood. However, it is known that physical activity
modulates the secretion of a series of fundamental cytokines for body
homeostasis [23]. Iftikhar et al. [24] demonstrated that the effects of
physical exercise on sleep apnea are independent of a reduction in BMI and body
weight.
When analyzing
the domains of the QoL questionnaire of patients who presented OSA, a greater
predominance of regular QoL is found. Improvements are needed, especially in
the physical domain, which includes questions related to pain and discomfort,
energy and fatigue, sleep and rest, mobility, activities of daily living,
dependence on medication or medical treatment, and work capacity. In the
present study, patients with OSA had lower scores when compared to patients without
OSA in this domain. This fact has as aggravating factor a low PAL in this
population, a situation that possibly impacted on the functional capacity of
these individuals, as well as may have been responsible for the reduction in
performance during the performance of ADLs and that certainly contributed to
the decrease in the QoL of this group. Yosunkaya et
al. [25] analyzed the QoL of 200 patients with suspected OSA and found that
overall health, life satisfaction, energy, and vitality in those diagnosed with
OSA were worse than those whose diagnosis was negative. According to the
authors, these factors are related to a reduction in the quantity and quality
of sleep during the night, mainly in the period of a deep sleep, due to the
frequent interruptions caused by OSA.
In the sample of
this study, it was also observed that the impairment of QoL was not
proportional to the severity of OSA, since patients with mild OSA reported the
same or greater impairment in some domains of the WHOQOL-bref
than those who had the most severe form of the disease. This corroborates some
studies described in the literature, such as that of D’Ambrosio
et al. [26], in which the QoL of 29 patients with OSA was assessed and
identified that the disease had an impact on the QoL of individuals in several
ways. However, some of these patients with mild OSA reported the same degree of
impairment in the QoL domains, as those with severe OSA, with no association,
as in this study, between the decrease in QoL scores and the severity of the
disease.
When dealing
with the eating habits of the population studied, there was a higher prevalence
in all groups of consumption of foods considered healthy when compared to
unhealthy ones. However, the group that presented the most severe form of the
disease consumed less healthy foods (49%) when compared to the group without
OSA (78%), a factor that directly contributes to the pathophysiology of OSA.
Since the increase in the consumption of processed foods, which contains a high
caloric density, associated with physical inactivity are predisposing factors
for the development of obesity, hypertension, and, consequently, OSA due to the
increased distribution of fat in the body and increased deposition of fat in
the neck area. Trakada et al. [27], in a
recent study, through the evaluation of 19 patients with OSA, demonstrated that
apneas increased significantly on the second night after eating a high-fat
diet. Besides, recent studies such as Smith et al. [28] demonstrated
that sleep restriction and interruption can increase ghrelin levels and reduce
leptin, hormones responsible for regulating appetite and satiety. Thus,
individuals with OSA have an increased appetite and a greater propensity to
consume food with high-fat content. These aspects are associated with the fact
that individuals with OSA stay more awake provide more time for eating at
night. This will possibly contribute to the increase in obesity and,
consequently, the severity of the disease. It is necessary to adopt a healthy
lifestyle with a diet rich in nutrients in this population so that together
with the association of physical activities, disease control is carried out, a
fact that has a direct impact on the health and well-being of these individuals
[28].
In this study,
we consider the small sample size as the main limitation, mainly due to the
small number of patients who underwent CPET. Therefore, the sample size did not
allow the identification of statistically significant differences between the
groups. Still, the results suggest that OSA leads to changes in VO2max,
PAL, QoL, and food consumption of these individuals. Given this, the present
study will continue following to adapt to this limitation and, possibly,
improve comparisons and results of the work.
Conclusion
According to the
results found, we suggest the existence of an inverse relationship between the
most severe levels of obstructive sleep apnea (moderate and severe) with the
maximum oxygen consumption and with the levels of physical activity. Higher
consumption of unhealthy foods, showing poor diet, and sedentary behavior are
important risk factors for the development and worsening of obstructive sleep
apnea.
Acknowledgments
We
thank Clínica Todo Ser, Dr. André Luis
de Sousa Bezerra Brandão and Dr. Samira Mariella Gonçalves Pereira Aires Ramos Rocha for logistical support during the study.
Conflict of interest
No conflicts of interest have been reported for this
article.
Financing source
No funding.
Authors´s
contributions
Conception and design of the research:
Brito EZA, Fernandes DSS, Schwingel PA, Mesquita FOS.
Data collection: Brito EZA, Guimarães MP, Fernandes
DSS, Neves VR, Gambassi BB, Schwingel
PA, Mesquita FOS. Analysis and interpretation of data: Brito EZA, Guimarães MP, Fernandes DSS, Neves
VR, Gambassi BB, Schwingel
PA, Mesquita FOS. Statistical analysis: Schwingel PA. Writing
of the manuscript: Brito EZA, Guimarães MP,
Fernandes DSS, Neves VR, Gambassi BB, Schwingel PA, Mesquita FOS. Critical revision of the
manuscript for important intellectual content: Neves VR, Gambassi BB, Schwingel PA,
Mesquita FOS.
References
- Perceval
AH, Meucci RD. Prevalência de alto risco para a
síndrome da apneia obstrutiva do sono na população idosa residente na área
rural de Rio Grande/RS. Cad Saúde Coletiva
2020;28(2):241-50. doi: 10.1590/1414-462x202028020189 [Crossref]
- Sun S, Zhai H, Zhu M, Wen P, He X, Wang H. Insulin resistance is associated with Sfrp5 in obstructive sleep apnea. Braz J Otorhinolaryngol 2019;85(6):739-45. doi: 10.1016/j.bjorl.2018.07.002 [Crossref]
- Leite AR, Martinez DM, Garcia-Rosa ML, Macedo EA, Lagoeiro AJ, Martins W de A et al. Risk of obstructive sleep apnea and echocardiographic parameters. Arq Bras Cardiol 2019;113(6):1084-89 doi: 10.5935/abc.20190181 [Crossref]
- Liu D, Myles H, Foley DL, Watts GF, Morgan VA, Castle D et al. Risk factors for obstructive sleep apnea are prevalent in people with psychosis and correlate with impaired social functioning and poor physical health. Front Psychiatry 2016;7:139. doi: 10.3389/fpsyt.2016.00139 [Crossref]
- Carvalho JB, Andrade GKP, Nascimento LA, Rodrigues ALCC, Suiter E, Solognesi J et al. Risco para síndrome da apneia obstrutiva do sono e sua relação com consumo alimentar. Rev Neurociencias 2015;23(4):567-74. doi: 10.34024/rnc.2015.v23.7980 [Crossref]
- Daltro CHC, Fontes FHO, Santos-Jesus R, Gregorio PB, Araújo LMB. Síndrome da apnéia e hipopnéia obstrutiva do sono: associação com obesidade, gênero e idade. Arq Bras Endocrinol Metabol 2006;50(1):74-81. doi: 10.1007/BF01432432 [Crossref]
- Garg RK, Afifi AM, Sanchez R, King TW. Obstructive sleep apnea in adults: the role of upper airway and facial skeletal surgery. Plast Reconstr Surg 2016;138(4):889-98. doi: 10.1097/PRS.0000000000002481 [Crossref]
- Dal-Fabbro C, Chaves Junior CM, Bittencourt LRA, Tufik S. Avaliação clínica e polissonográfica do aparelho BRD no tratamento da síndrome da apneia obstrutiva do sono. Dental Press J Orthod 2010;15(1):107-17. doi: 10.1590/S2176-94512010000100013 [Crossref]
- Herdy AH, Uhlendorf D. Valores de referência para o teste cardiopulmonar para homens e mulheres sedentários e ativos. Arq Bras Cardiol 2010;96(1):54-9. doi: 10.1590/S0066-782X2010005000155 [Crossref]
- Piccin CF, Tassinari CR, Beck MC, Scapini F, Oliveira LCA, Signori LU et al. Capacidade funcional e qualidade de vida entre sujeitos saudáveis e pacientes com apneia obstrutiva do sono. Sleep Sci 2015;8(4):186. doi: 10.11606/issn.2176-7262.v49i2p152-159 [Crossref]
- Fogaça MC, Carvalho WB, Nogueira-Martins LA. Preliminary study about quality of life of physicians and nurses working in pediatric and neonatal intensive care units. Rev Esc Enferm 2010;44(3):708-12. doi: 10.1590/S0080-62342010000300022 [Crossref]
- Pinto Guedes D, Correa Lopes C, Pinto Guedes JER. Reproducibility and validity of the International Physical Activity Questionnaire in adolescents. Rev Bras Med do Esporte 2005;11(2):151-8. doi: 10.1590/S1517-86922005000200011 [Crossref]
- Brasil.
Ministério da Saúde. Protocolos do Sistema de Vigilância Alimentar e
Nutricional - SISVAN na assistência à saúde. Secretaria de atenção à saúde.
Brasília: Ministério da Saúde; 2008.
- Ministério
da Saúde (BR). Uso dos formulários e registro das informações no novo Sistema
Informatizado da Vigilância Alimentar e Nutricional. SISVAN 2008;
Available from: http://189.28.128.100/nutricao/docs/geral/informe_sisvan_web_040608.pdf608.pdf
- Carvalho MMB, Coutinho RQ, Barros IML, Costa LOBF, Medeiros AKL, Lustosa TC, et al. Prevalence of obstructive sleep apnea and obesity among middle-aged women: implications for exercise capacity. J Clin sleep Med JCSM Off Publ Am Acad Sleep Med 2018;14(9):1471–5. doi: 10.5664/jcsm.7316 [Crossref]
- Herdy AH, Uhlendorf D. Reference values for cardiopulmonary exercise testing for sedentary and active men and women. Arq Bras Cardiol 2011;96(1):54-9. doi: 10.1590/S0066-782X2010005000155 [Crossref]
- Fox H, Bitter T, Sauzet O, Rudolph V, Oldenburg O. Automatic positive airway pressure for obstructive sleep apnea in heart failure with reduced ejection fraction. Clin Res Cardiol 2020;(0123456789). doi: 10.1007/s00392-020-01701-1 [Crossref]
- Lin C-C, Hsieh W-Y, Chou C-S, Liaw S-F. Cardiopulmonary exercise testing in obstructive sleep apnea syndrome. Respir Physiol Neurobiol 2006;150(1):27-34. doi: 10.1016/j.resp.2005.01.008 [Crossref]
- Alonso-Fernández A, García-Río F, Arias MA, Mediano O, Pino JM, Martínez I et al. Obstructive sleep apnoea–hypoapnoea syndrome reversibly depresses cardiac response to exercise. Eur Heart J 2005;27(2):207-15. doi: 10.1093/eurheartj/ehi621 [Crossref]
- Denadai BS. Consumo máximo de oxigênio: fatores determinantes e limitantes. Rev Bras Ativ Fis Saúde 1995;1;1. doi: 10.12820/rbafs.v.1n1p85-94 [Crossref]
- Carvalho LPC, Souza SSN, Souza DC, Araujo FDS, Carvalho FO, Moraes JFVN et al. Analysis of glycemic safety of a moderate-intensity resistance exercise session in patients with diabetes type 1. Rev Bras Fisiol do Exerc 2020;19(1):16. doi: 10.33233/rbfe.v19i1.3905 [Crossref]
- Aiello KD, Caughey WG, Nelluri B, Sharma A, Mookadam F, Mookadam M. Effect of exercise training on sleep apnea: A systematic review and meta-analysis. Respir Med 2016;116:85-92. doi: 10.1016/j.rmed.2016.05.015 [Crossref]
- Carvalho LPC, Gomes MBC, Oliveira ICS, Santos PHS, Oliveira IIAC, Vitavar LMG et al. Responses of myokines concentrations from exercise stimulus: a systematic review. Rev Bras Fisiol do Exerc 2020;19(5):421. doi: 10.33233/rbfex.v19i5.4393 [Crossref]
- Iftikhar IH, Bittencourt L, Youngstedt SD, Ayas N, Cistulli P, Schwab R et al. Comparative efficacy of CPAP, MADs, exercise-training, and dietary weight loss for sleep apnea: a network meta-analysis. Sleep Med 2017;30:7-14. doi: 10.1016/j.sleep.2016.06.001 [Crossref]
- Yosunkaya S, Kutlu R, Cihan F. Evaluation of depression and quality of life in patients with obstructive sleep apnea syndrome. Niger J Clin Pract 2016;19(5):573-9. doi: 10.4103/1119-3077.18870 [Crossref]
- D’Ambrosio C, Bowman T, Mohsenin V. Quality of life in patients with obstructive sleep apnea: effect of nasal continuous positive airway pressure--a prospective study. Chest 1999;115(1):123-9. doi: 10.1378/chest.115.1.123 [Crossref]
- Trakada G, Steiropoulos P, Zarogoulidis P, Nena E, Papanas N, Maltezos E et al. A fatty meal aggravates apnea and increases sleep in patients with obstructive sleep apnea. Sleep Breath 2014;18(1):53–8. doi: 10.1007/s11325-013-0847-y [Crossref]
- Smith SS, Waight C, Doyle G, Rossa KR, Sullivan KA. Liking for high fat foods in patients with Obstructive Sleep Apnoea. Appetite 2014;78:185-92. doi: 10.1016/j.appet.2014.03.019 [Crossref]