Rev Bras Fisiol Exerc 2020;19(4):255-57
EDITORIAL
Idiosyncrasy
in science: an idea forgotten or not understood?
Jefferson Petto1,2,3,4,
Thiago Bouças Duarte3,5,6, Taissa Argolo
Jesus3
1ACTUS-CORDIOS
Reabilitação Cardiovascular, Respiratória e Metabólica, Salvador, BA, Brasil
2Centro Universitário
Social da Bahia, Salvador, BA, Brasil
3Faculdade do Centro Oeste
Paulista, Bauru, SP, Brasil
4Escola Bahiana de Medicina e Saúde Pública, Salvador, BA, Brasil
5Hospital Português da Bahia, Salvador, BA, Brasil
6Universidade Salvador –
Unifacs, Salvador, BA, Brasil
Received
on: August 5, 2020; Accepted on: August 21, 2020.
Corresponding author: Jefferson Petto, Av.
Anita Garibaldi, 1815, CME, Sala 13 Ondina 40170-130 Salvador BA
Jefferson
Petto: gfpec@outlook.com
Thiago
Bouças Duarte thiago_fisio@yahoo.com.br
Taissa Argolo
Jesus: taissa_argolo@hotmail.com
The idea of idiosyncrasy (idiosugkrasía)
emerged in Greek civilization and referred to the individual's peculiar
behavioral condition [1]. In current medicine, the term refers to "the
particular predisposition of the organism that causes an individual to react
personally to the influence of external agents, such as food and drugs"
[1].
Although most people intuitively think that for each action imposed the
reaction can be different, in the plurality of times, the prevailing thought is
that of generalization. This does not seem to be different in science and
clinical practice. The understanding that external and internal factors will be
determining the response to a treatment should be the basis, both in research
and in health practice, however it is not. Certainly, there are several reasons
for this behavior and one of them is the misinterpretation of the scientific
text.
We know that the most widely read section of a scientific article is the
summary, and the most widely read summary is its conclusion. The conclusion
points out “the authors' position or solution based on the arguments presented;
sometimes it suggests unfolding” [2]. Therefore, it answers in a conceptual and
generic way the question that generated the objective of the work. Not
intentionally, but the idiosyncrasy in this text is omitted, because it is
inherent in scientific writing.
For example, we recently published an article entitled “Plasma Renin in
Women Using and Not Using Combined Oral Contraceptive”, in which we tested the
hypothesis that women using combined oral contraceptive (COC) have plasma renin
values different from their counterparts that do not use this drug [3]. In
parallel, we also evaluated Reactive Protein C (RPC). It was an observational
cross-sectional study. Figure 1 shows the results of this study in relation to
plasma renin. As you can see, we see that the group using COC has plasma renin
values statistically higher than the group without COC. What is our conclusion?
I report: “Women using COC have higher serum levels of plasma renin and
C-Reactive Protein than women who do not use this drug. This points to the
possibility that this population has a higher risk of developing systemic
arterial hypertension in the long term, which associated with subclinical
inflammation can increase the risk of cardiovascular diseases” [3].
However, it is also possible to observe in figure 1, that not all women
using COC had higher renin values than the group without COC and that the
opposite is also likely, especially in a non-parametric distribution like this.
That is, although the conclusion is based on a well-performed statistical
analysis, it is necessary to understand that the fact that we found a
statistical difference between the groups does not mean that all the volunteers
in the sample behaved in the same way.
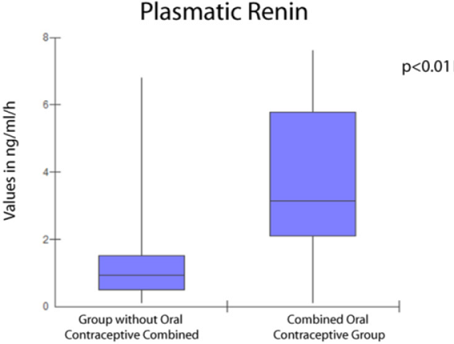
Figure
1 - Median and quartile intervals of the groups with
and without combined oral contraceptives
If a study shows that high-intensity exercise was beneficial for
patients with Ischemic Heart Failure with Intermediate Ejection Fraction, it
does not mean that everyone with this clinical condition will benefit. Physical
exercise is a therapy that, like any other, can have a neutral, positive or
negative effect. That is why understanding health idiosyncrasy is so important.
Knowing that our patient can respond differently to a treatment, even if the
evidence indicates that it is safe and effective, keeps our reasoning open to
changes that are necessary during the follow-up.
Therefore, it is imperative for quality praxis that the professional
uses the knowledge of science with good wisdom, interpreting it properly and
using the knowledge available considering the clinical, social and biological
condition of each patient or client. Scientific evidence provides us with a
basis for a better-founded therapeutic direction, but it does not tell us
exactly how we should conduct our intervention in an airtight manner.
Understanding and applying the idea of idiosyncrasy frees us from a general
protocol, from the evaluation, the preparation of the prognosis, the initial
prescription to the evolution of the treatment. No treatment is 100% foolproof
or 100% effective.
Corroborating this thought, there is in biostatistics what we call NNT
(number needed to treat), number of individuals treated so that the benefit of
a given intervention occurs in an individual. For example, for individuals
after myocardial infarction, it is necessary to treat 842 patients with
beta-blockers in order to avoid death (NNT 842). Considering Cardiac
Rehabilitation, the NNT for individuals after myocardial infarction is 66 [4].
So, will all post-myocardial infarction patients who enter a Cardiac
Rehabilitation program have the benefit of increased survival? The answer is
no. Because despite the studies pointing out that Cardiac Rehabilitation
increases survival, as we can see, we need to treat at least 66 patients to
obtain this response with 1 patient.
In short, correctly interpreting the relationship between idiosyncrasy
and the completion of scientific work, the basis of evidence-based medicine,
will allow us to achieve a better quality of treatment and consequently impact
the health of the community more effectively.
References
- Dicionário Eletrônico
Houaiss da Língua Portuguesa. Consultado em 30 de julho de 2020. Disponível em:
https://houaiss.uol.com.br/corporativo/apps/uol_www/v5-4/html/index.php#1
- Pereira MG. Artigos
científicos: como redigir, publicar e avaliar. Rio de Janeiro: Guanabara Koogan; 2012. p. 212.
- Oliveira SS, Petto J,
Diogo DP, Santos ACN, Sacramento MS, Ladeia AM. Plasma
renin in women using and not using combined oral contraceptive. Int J Cardiovasc
Sci 2020;33(3):208-14.
https://doi.org/10.36660/ijcs.20180021
- Carvalho T. Diretriz de
reabilitação cardiopulmonar e metabólica: aspectos práticos e
responsabilidades. Arq Bras
Cardiol 2006;86(1):74-82.
https://doi.org/10.1590/S0066-782X2006000100011