Rev Bras Fisiol Exerc 2021;20(1):38-51
doi: 10.33233/rbfex.v20i1.4426
ORIGINAL ARTICLE
Evaluation of the Pilates method in the treatment of
individuals with chronic non-specific low back pain: randomized clinical trial
Avaliação do método Pilates
no tratamento de indivíduos com dor lombar crônica inespecífica: ensaio clínico
randomizado
Bruna
Angela Antonelli1,2, Geovani Alves dos
Santos3, Luana Marcela Nascimento da Silva2,4, Maria
Danielly Alves de Vasconcelos2, Rita di
Cássia de Oliveira Angelo2, Paulo Adriano Schwingel1,2
1Universidade de Pernambuco, Recife, PE,
Brasil
2Universidade de Pernambuco, Petrolina,
PE, Brasil
3Faculdade UniNassau
Petrolina, Petrolina, PE, Brasil
4Faculdade São Francisco de Juazeiro,
Juazeiro, BA, Brasil
Received:
October 24, 2020; accepted:
December 21, 2020.
Correspondence: Bruna Angela Antonelli, Rua Arnóbio Marques, 310 Santo Amaro 50100-130 Recife PE, Brazil
Bruna Angela Antonelli:
brunautfpr@gmail.com
Geovani Alves dos Santos: tccgeovani@gmail.com
Luana Marcela Nascimento da Silva: luanahmarcela@gmail.com
Maria Danielly Alves de Vasconcelos:
daniellyavasc@gmail.com
Rita di Cássia de Oliveira Angelo: rita.angelo@upe.br
Paulo Adriano Schwingel:
paschwingel@gmail.com
Abstract
Introduction: Chronic
nonspecific low-back pain (CNLBP) is a common painful symptom in the lower
spine for more than twelve weeks and may be accompanied by neurological
symptoms in the lower limbs. CNLBP has a high worldwide prevalence, can lead to
function limitations and the treatment emphasizes active therapies, such as
Pilates exercises. Objective: To evaluate the effect of Pilates
exercises on painful perception, quality of life, functional disability and kinesiophobia of individuals with CNLBP, classified as
having low and medium risk of poor prognosis according to the Brazilian version
of the Start Back Screening Tool (SBST-Brazil). Methods: Randomized
controlled clinical trial with 59 patients clinically diagnosed with CNLBP,
divided into two groups: Control (CG) and Pilates (PG). For 12 weeks the CG
received drug intervention while the PG was submitted to a Pilates method
exercise protocol twice a week. Results: Pilates training reduced pain
and kinesiophobia in both subgroups with SBST-Brazil
Low and Medium. Contrary to participants with medium risk of poor prognosis in
the CG, the PG with medium risk showed a significant improvement (P < 0.05)
in functional capacity. The pharmacological intervention proved to be efficient
(P < 0.05) in reducing pain catastrophization and kinesiophobia in the CG classified as having a medium risk
of poor prognosis. Conclusion: Stratification in low and medium risks
for poor prognosis of disability has positive responses to treatment based on
Pilates exercises, considering the reduction of painful intensity and
functional limitation.
Keywords: low back pain; chronic pain;
disability evaluation; physical therapy; exercise therapy.
Resumo
Introdução: A dor lombar crônica inespecífica
(DLCI) é uma sintomatologia dolorosa comum na região inferior da coluna por
período superior a doze semanas, podendo ser acompanhada de sintomas
neurológicos em membros inferiores. A DLCI apresenta alta prevalência mundial,
pode conduzir a limitações de função e o tratamento enfatiza terapias ativas,
tais como exercícios de Pilates. Objetivo: Avaliar o efeito de
exercícios de Pilates na percepção dolorosa, qualidade de vida, incapacidade
funcional e cinesiofobia de indivíduos com DLCI,
classificados com baixo e médio riscos de mau prognóstico conforme a versão
brasileira do Start Back Screening Tool
(SBST-Brasil). Métodos: Ensaio clínico randomizado controlado com 59
pacientes diagnosticados clinicamente com DLCI, divididos em dois grupos:
Controle (GC) e Pilates (GP). Durante 12 semanas, o GC recebeu intervenção
medicamentosa enquanto o GP foi submetido a um protocolo de exercícios do
método Pilates duas vezes na semana. Resultados: O treinamento com
Pilates reduziu dor e cinesiofobia em ambos os
subgrupos com SBST-Brasil Baixo e Médio. Contrariamente aos participantes de
médio risco de mau prognóstico do GC, o GP com médio risco apresentou melhora
significativa (P < 0,05) da capacidade funcional. A intervenção farmacológica
se mostrou eficiente (P < 0,05) na redução da catastrofização
da dor e cinesiofobia no GC classificados com médio
risco de mau prognóstico. Conclusão: A estratificação em baixo e médio
riscos para mau prognóstico de incapacidade têm respostas positivas ao
tratamento baseado em exercícios do método Pilates, considerando a redução da
intensidade dolorosa e da limitação funcional.
Palavras-chave: dor lombar; dor crônica; avaliação da
deficiência; fisioterapia; terapia por exercício.
Introduction
Low back pain
(LBP) is a symptom experienced by people of all age groups, being defined as
pain in the dorsal region, located between the lower margin of the twelfth pair
of ribs and the lower gluteal folds, which may or may not be accompanied by
pain or other neurological symptoms in one or both lower limbs [1].
In Brazil, it is
estimated that the annual prevalence of LBP in adult individuals is > 50% [2,3,4]. The literature science shows that 80% of
the population will present at least one episode of LBP during his life, and up
to 40% of these cases may become chronic [3,4].
LBP is
characterized by a serie of biophysical,
psychological, and social aspects that impair function, participation in
society and personal financial prosperity [5]. Its economic impact is
multisectoral, as it increases the costs of medical and social assistance
systems and the rate of absenteeism, being currently considered the number one
cause of years lost due to disability, and its burden is growing along with the
increase and aging of the population [1,6]. It is classified as acute,
subacute, and chronic, when the duration of the painful episode, respectively,
is less than six weeks, lasts between six to twelve weeks or is greater than
twelve weeks [6,7].
However, only a
low percentage of cases of LBP have a specific cause, with the nonspecific cause
of this painful sensation being more prevalent (in 85% of patients), which is
called nonspecific LBP due to the inability to determine its causal factor,
such as, for example, reduced space in the intervertebral discs, bone or joint
injuries and compression of nerve roots [5]. In addition, it is also observed
among patients emotional and behavioral impacts that favor the development of
chronic conditions [1,6], and the evidence shows that psychosocial factors such
as the patient's perception about the difficulty of coping with the disease,
the pain catastrophizing and other depressive symptoms are predictors of
dysfunction and directly interfere with the prognosis [8,9]. Therefore, the
application of a questionnaire that evaluates the interaction of LBP with
psychosocial factors, and classify patients according to their condition, can
help in decision making during treatment.
Several studies
have tested the effectiveness of the STarT Back
Screening Tool (SBST) questionnaire [8,10,11] and found that patients
classified and treated according to the SBST obtained satisfactory results due
to improved quality of life, decreased use health services and reduced days of
absenteeism from work compared to those not classified in the same way. It is
noteworthy that identifying patients with psychosocial factors can influence
the prognosis and assist in choosing the most specific treatment, in addition
to enabling the patient to better understand the signs and symptoms of LBP
[11,12]. Current recommendations for managing LBP emphasize self-management of
pain, psychosocial and exercise therapies, as well as some forms of
complementary medicine such as spinal manipulation, Tai Chi, massage,
acupuncture and yoga, with less emphasis on pharmacological and surgical treatments
[6,13]. In this context, the method Pilates is often used to treat LBP,
considering that consists of a collection of exercises that focus on static
control and dinamic the muscles of the trunk,
improving the stability and mobility of the spine, coordination breathing,
overall flexibility, muscular strength and the position [14]. However, due to
the insufficient number of quality clinical trials [15], as well as notable
heterogeneity in relation to the populations studied, the proposed interventions
and outcome measures, there is no consensus in relation to its effectiveness in
treating this condition.
Therefore,
considering that LBP is the painful syndrome that causes more functional
disability than any other health condition, causing a great socioeconomic
impact, interfering in the quality of life of this population [16,17,18], the aim
of the present study is to evaluate the effect of exercises based on the
Pilates method in reducing pain perception, quality of life, functional
capacity and kinesiophobia of adults with chronic
nonspecific low back pain (CNLBP), ranked at low and medium risks of poor
prognosis in the primary treatment as the Brazilian version of SBST
(SBST-Brazil).
Methods
Experimental design
To address the
question, a clinical trial, randomized-controlled, open, parallel, with two
arms was performed. 59 subjects with clinical diagnosis for CNLBP participated
in the study, divided into the Control (CG) and Pilates (PG) groups.
In both groups,
the participants were stratified into low and medium groups (SBST-Brazil)
ranked by the risks of poor prognosis in primary treatment. Prior and after the
intervention period, participants answered four questionnaires to assess
quality of life, kinesiophobia, functional disability
and pain catastrophizing. During a 12-week period, the CG received drug
intervention while the PG was submitted to a training protocol in the Pilates
method with floor exercises.
The study was
performed in accordance with the Regulatory Guidelines and Norms for Research
involving human beings (Resolution 466/2012 of the Brazilian National Health
Council) and ethical determinations of the Declaration of Helsinki (2000) and
was approved by the Research Ethics Committee of the Universidade
de Pernambuco (CEP-UPE), under the number 3,259,512. In addition, the
research also was registered in the Brazilian Registry of Clinical Trials
(BRCT) under number RBR 9s3fbm and in the World Health Organization (WHO) under
Universal Trial Number (UTN) number A00824830946. All participants signed an
informed consent form.
Recruitment and selection of participants
The recruitment
of participants was carried out by means of broadcasting on radio and
television, as well as through digital media on social networks and blogs and
poster display in public places in the Integrated Region of Economic
Development (IRED) of the Polo Petrolina/PE and
Juazeiro/BA.
Inclusion
criteria were clinical diagnosis of CNLBP; both sexes; age group between 18 and
59 years; literate; self-declared sedentary or irregularly active according to
the International Classification of Physical Activity Level Assessment
(IPAQ-short version) [19]; classified as having low or medium risk of poor
prognosis in primary treatment according to the SBST-Brazil questionnaire [12].
Exclusion
criteria were: previous participation in a Pilates exercise program or other
therapeutic exercises in the last six months; schedule or history of spinal
surgery; unexplained weight or appetite loss in the past 6 months; history of
cancer or malignancy; lesion of the horse tail; loss of bladder or bowel
control; saddle paresthesia; pregnancy; spine fractures; rheumatological
diseases; inflammatory and/or infectious diseases of the spine; presence of
comorbidities that prevented the practice of physical exercises.
Aiming at the
eligibility criteria and aiming to classify the risk of poor prognosis in
primary treatment and in individuals with CNLBP according to the presence of
physical and psychosocial factors, the volunteers answered the SBST-Brazil. The
stratification of subgroups was held in accordance with the results of the
questionnaire [12]: a) individuals with low risk of poor prognosis (between 0
and 3 points of the total score): presence of minimal physical and psychosocial
factors; b) individuals with medium risk of poor prognosis (values > 3 on the total score and subscale ≤ 3 points):
presence of physical and psychosocial factors, but at lower levels than
individuals classified as high risk).
Meeting the
eligibility criteria, volunteers classified as having low or medium risks for
poor prognosis in primary treatment according to the SBST-Brazil, were sent to
an interview, conducted by a physiotherapist, containing sociodemographic
information, factors associated with behavior and lifestyle habits, personal
history, and clinical-orthopedic data.
Then the
participants were referred for evaluation with orthopedic doctor to confirm or
not the diagnosis of CNLBP and to evaluate the clinical conditions for possible
performance of interventions through exercises with Pilates method or drug
intake.
After all these
procedures, the groups were allocated by a researcher who was not involved in
the evaluation and intervention of the participants, based on the generation of
random numbers in Excel® (Microsoft Corporation, Redmond, WA, United States,
Release 12.0.6662, 2012). The data for each patient were protected in
individual, numbered, and sealed opaque envelopes [17]. According to the
SBST-Brazil classification (low and medium) the participants were allocated
according to the type of intervention resulting in the groups CG SBST Low, CG
SBST Medium, PG SBST Low and PG SBST Medium.
Procedures
Psychometric
assessments were applied individually in a private room, where each volunteer
responded to the following instruments: 1) Medical Outcomes Study 36 - item
Short- Form Health Survey - SF36 [20]; 2) Roland Morris questionaire
disability [21]; 3) Tampa Scale for Kinesiophobia
[22]; 4) Scale of Catastrophic Thoughts on Pain [23] duly validated for the
Brazilian population. The evaluations (PRE and POST moments) took place at the Universidade de Pernambuco (UPE) Campus Petrolina in the period between March and December 2019.
Both the CG SBST
Low as CG SBST Medium received drug intervention with 550 mg of naproxen sodium
at no cost for the participant, being prescribed by an orthopedist. The
medication was administered continuously for 12 weeks twice a day, respecting
the contraindications. These two subgroups were properly monitored by the same
doctor orthopedist until the end of the protocol. The use of medication in the
CG was chosen considering the evidence in the scientific literature [24,25,26,27],
which, in view of pain complaints, the failure to use an effective treatment
violates the ethical principles that guide research with human beings.
PG SBST Low and
Medium received exercises based on Pilates method, guided
and supervised by a qualified physiotherapist twice a week also for 12 weeks.
The exercises are part of a protocol developed by the researchers themselves,
which includes the use of exercises on the ground and on the equipment
(Springboard, Cadillac, Reformer, Ladder Barrel and Chair). The prescription of
the protocol with three levels of four weeks each was composed of: I. Basic
Level (integration of upper and lower supine position, stabilization of the
spine and stimulus to mobilize low amplitude motion); II. Intermediate Level
(lowering of weight on lower limbs; control of the stabilizing muscles of the
pelvis and trunk; stimulation of vertebral mobilization); III. Advanced Level
(integration of upper and lower limbs; control of trunk stabilizing muscles in
sedation and in orthostasis; dynamic spine stabilization in multiple planes;
orthostatic load support).
The training/treatment
sessions lasted 60 minutes, 10 minutes of warm-up, 40 minutes of exercises on
the floor and on the equipment and 10 minutes of cooling down. As a protective
and monitoring measure, before and after each care session, painful perception was
assessed using the Visual Analogue Scale (VAS). Blood pressure and heart rate
were also collected using the HEM-7130 automatic arm blood pressure monitor
(Omron Healthcare, Inc., Lake Forest, IL, USA). To verify the subjective
perception of effort, the Borg scale (version 6 to 20 points) [28] was used
after each session as a guiding instrument for maintaining and removing some
exercise.
Participants
were instructed not to participate in another therapeutic intervention during
the same period. After the end of the twelve weeks of intervention, the
individuals, from both groups, underwent a reassessment (post-intervention
moment), containing the same procedures performed in the initial evaluation.
The
physiotherapists who applied the protocol were not masked for randomization due
to active supervision of the exercise intervention. However, the professionals
were not informed about the stratification of the SBST in Medium or Low. It is
noteworthy that the professionals who carried out the pre- and post-intervention
evaluations did not participate in the interventions.
Statistics
The sample size
to satisfy a statistical power of 80 % with 95% confidence was estimated by the
computer program Bioestat (Civil Society Mamirauá, Tefé, AM, Brazil, Release
5.3, 2008) using data published by Silva et al. [29] who evaluated the effect
of 12 sessions of the Pilates method in individuals with chronic low back pain.
The minimum number of subjects per group, Control or Pilates, was of 12
individuals according to averages and deviations previously published
standards.
The data were
analyzed with the help of the Statistical Package for Social Sciences (SPSS
Inc., Chicago, IL, USA, Release 16.0.2, 2008) after insertion through double
typing with automatic amplitude and consistency check. Initially,
homoscedasticity (Bartlett's criterion) and normality (Kolmogorov-Smirnov) of
continuous data were verified. Two-way analysis of variance (ANOVA) with
Bonferroni's post-hoc test was used to compare the results obtained between
groups overtime. Categorical variables were summarized using absolute and
relative frequencies with associations verified by Fisher's exact test.
Correlations were calculated by the Pearson correlation coefficient and the
effect size was established using Cohen's d. All statistical methods were
two-tailed, P values were exact calculated and significance level was set as P ≤
0.05.
Results
In total, during
the recruitment period, 408 questionnaires were answered from March to July 2019
by the interested people who answered the disclosure. It was identified that 78
(19.1%) of these individuals showed SBST Low, 153 (37.5%) SBST Medium and 177
(43.4%) SBST High. They contacted the 231 stakeholders with SBST Low and SBST
Medium, and then subjected to evaluation pre-intervention the 120 individuals
who did not have exclusion criteria at the time of initial contact. During the
driving medical evaluation, 27 individuals did not meet the eligibility
criteria, a fact that resulted in 93 patients eligible for research. These
participants were randomized into the CG and PG groups (Figure 1). The
evaluator was blinded to the allocation of treatment.
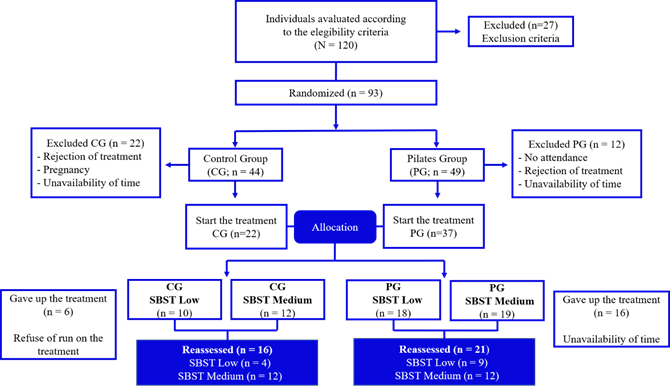
Figure 1 - Flowchart of randomization
and allocation of individuals among the study groups
CG finished with
16 participants classified SBST Low (n = 4) and SBST Medium (n = 12) aged
average (± Standard Deviation) 25.3 (± 5.4) years and 41.8 (± 9.7) years,
respectively. Eight of them (50.0%) were single, seven (43.8%) were married and
just one was (6.2%) divorced. As to education, seven (43.8%) participants had
college graduates, seven (43.8%) had completed high school and two (12.4%)
completed elementary school.
PG had nine
(42.9%) volunteers classified with SBST Low and twelve (57.1%) with SBST
Medium. Twelve (57.1%) were single, seven (33.3%) were married, one (4.8%)
divorced and one (4.8%) widowed. The education of the group was characterized
by seven (33.3%) participants with college education, 11 (52.4%) had completed
high school and three (14.3%) with incomplete elementary education.
Regarding the
work activities of the CG volunteers, 12 (75.0%) were formal professionals,
with paid services, being three (18.8%) teachers, three (18.7%) general service
workers and six (37.5%) exercising other professions related to their higher or
technological education, one (6.2%) participant was an independent work and
three (18.8%) were students. In the PG, 12 (57.1%) performed paid activities,
being three (14.3%) teachers, four (19.0%) trade workers and five (23.9%)
worked in other professions related to their higher education, five (23.8%)
were independent professionals and four (19.0%) were students.
The table I
presents the characteristics of participants in CG and PG stratified into
subgroups Medium and Low according to the prognosis in primary treatment
evaluated by the SBST-Brazil. Age, total body mass, height and BMI were similar
between groups (P > 0.05).
Table I - Description of the sample (n
= 37)
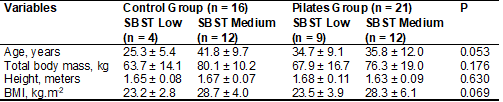
Data
in mean and standard deviation; SBST = Brazilian version of the STarT Back Screening Tool
It was
identified that there was no interaction effect with respect to pain sensation
(F[3,33] = 1.506; P = 0.231) as the groups CG and PG, as well as any effect
compared to group has been reported (F[3,33] = 1.787; P = 0.169). However, an
effect on time (F[1.33] = 22.610; P <0.001) was
observed. Additional comparisons showed that both subgroup SBST Low (4.8 ± 1.6
vs. 1.6 ± 1.8; P = 0.002 and d = 1.35) and the SBST Medium (6.1 ± 2.2 vs. 3.0 ±
2.0; P < 0.001 and d = 0.98) of the PG obtained a reduction in painful
sensation. In other hand, no significant decrease was observed in CG (Table
II). As the analysis of kinesiophobia was identified
statistically significant effect only for the time (F[1,33]
= 19.38; P = 0.001). In addition, there was a reduction in participants with
low and medium SBST in the PG, however, in the CG only participants with average
SBST showed a reduction in kinesiophobia levels.
Finally, pain catastrophizing reduced only in participants with SBST Medium in
the CG (4.8 ± 1.6 vs. 1.6 ± 1.8; P < 0.002 and d = 0.78). Furthermore, no
interaction effect (F[3,33] = 0.280; P = 0.840) for
the groups (F[3,33] = 0.769; P = 0.520) was found.
Table II - Intragroup and intergroup
comparison of Control and Pilates treatments (n = 37
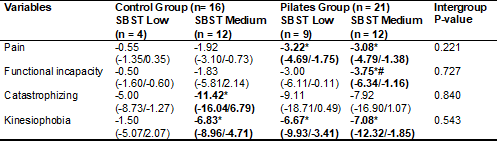
Data
reported in mean differences between pre- and post-intervention with the 95%
confidence interval. SBST = Brazilian version of the STarT
Back Screening Tool; *P < 0.05 in relation to preintervention; #P
< 0.05 in relation to post-intervention of SBST Medium from Control Group
Analyzing a
possible relationship between the soreness and the different domains of pain
catastrophizing in the preintervention, a positive correlation between pain and
pain amplification was found (r = 0.52; P = 0.038), but at the end of the
intervention the same association was not confirmed (r = 0.10; P = 0.716) in
participants with SBST in the CG, suggesting a possible positive effect of the
drug intervention.
Comparing the
effects of the intervention on the functional capacity in relation to the CG
and PG, was checked that no interaction effect happened (F[3,33]
= 4.349; P = 0.7 27). However, were identified effects in relation to the
groups (F[3,33] = 3.205; P = 0.036) and time (F[1,33]
= 4.900; P = 0.03). Comparisons over time demonstrated that the intervention
was effective in improving the functional capability of participants with SBST
Medium in the PG (7.1 ± 4.5 vs. 3.3 ± 3.5; P < 0.05 and d = 0.78). In
addition, when comparing the moments post-intervention between subgroups SBST
Medium of CG and PG, also it was identified difference (P < 0.05) between
them (Figure 2).
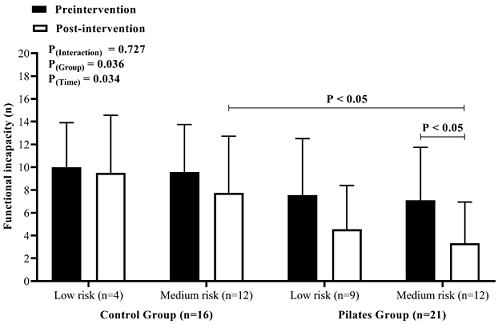
Figure 2 - Comparison of functional
incapacity by SBST subgroup in the two evaluation moments (pre- and
post-intervention) from both groups (n = 37)
Discussion
The main
findings indicate that training with the Pilates method reduced pain and kinesiophobia for both subgroups with low and medium risks
of disability and that the PG SBST Medium achieved an improvement in functional
capacity unlike the medium risk participants who received drug treatment. In
addition, pharmacological intervention proved to be effective in reducing pain
catastrophizing and kinesiophobia for the subgroup
SBST Medium. The results point to the need for a risk classification for
disability and pain catastrophizing prior to intervention as tools to aid
therapeutic planning in individuals with CNLBP.
It was observed
that strategies of classification of SBST and evaluation of pain
catastrophizing were important tools for conducting interventions. It is
observed that the CG had a positive association between the level of pain and
the pain magnification (magnification of displeasure) pre-intervention, in
other words, a possible influence negative of aspects not only related to
functionality. However, after the 12 weeks of pharmacological intervention, no
association was observed. Therefore, the reduction of pain catastrophizing in
CG SBST Medium may be related to the mechanism of action of the administered
drug [26,27], this means that SBST Medium represents the presence of physical
and psychosocial factors for the poor prognosis in the primary treatment for
LBP [12].
Given this
context, it is understood that the naproxen sodium has an analgesic action
reducing the feeling of persistent pain, which makes it able to its direct
interference in the reduction of pain magnification or exaggeration in valuing
the threat it represents, even in the face of a non-significant clinical
reduction in self-reported pain.
On the other
hand, the lack of correlation between some of the domains of pain
catastrophizing and pain perception in the participants of PG suggests that
limitations functional can be involved in the pain mechanism besides the
biopsychosocial aspects, especially for adults with CNLBP ranked as SBST Medium
[12]. The results found for improving functional capacity and reducing pain for
these participants support the rational presupposition of our study.
Taking into
account that the painful perception and the presence of disabling conditions
faced by individuals with CNLBP, such as fear-avoidance of pain [14], in
addition to muscle weakness, especially in the deep abdomen muscles, and less
articular flexibility in the spine and in the lower limbs [29,30], a possible
interpretation to reduce pain and physical capacity limitations in the PG
ranked as SBST Medium, is due to the fact that physical exercise is able to
induce hypoalgesia, by activation of endogenous pain inhibitory systems [31].
In addition, the hypoalgesia exercise-induced improve general well-being, based
on action on some psychological factors through multiple cellular and molecular
events produced at different levels of the nervous system following physical
exercise.
Regarding
exercises based on Pilates method, they can act with functional reeducation
improving the overall posture and breathing pattern of these individuals, as
well as strengthening the deep trunk muscles and the static and dynamic
stability of the muscles related to the lumbar segment, favoring an improvement
in health-related quality of life and a better performance in activities of
daily and professional life [29,31]. Treatment with Pilates method still has
variability in the length of service and sessions, but it is noteworthy that
there is evidence [31] showing that the frequency of twice a week seems to be
better than once a week and have similar effects to training three times a
week. Thus, in this research were prioritized two weekly 60-minute duration
over 12 weeks, totaling 24 sessions [31,32,33].
The association
between decreased functional capacity of muscles of core and the CNLBP may be
one of the main defense arguments to use the Pilates method as a therapeutic
intervention [32,34,35]. There is also evidence that people with CNLBP may
demonstrate a prevalence of low pelvic loin control [36]. Current literature [37]
recommends that patients in the low-risk group receive information about LBP
and have advice to remain as physically active as possible and to continue
daily activities; medium-risk patients should have interventions based on the
management of symptoms and physical function, in addition to information and
advice, while high-risk patients, due to their greater limitations on recovery,
should receive therapy based on a cognitive-behavioral approach, focusing on
the psychosocial obstacles faced by them.
In view of the
exposed, it is confirmed that the guidelines for non-pharmacological treatment
of CNLBP emphasize the importance of participating in Pilates training programs
[6,32,38,39]. Although it is expected, the intervention guidelines and
literature reviews do not yet mention the comparison of the efficiency of the
protocols in the face of minimal interventions and different classifications to
the risk of poor prognosis [9,38,39]. It is emphasized that not only for
ethical criteria, but also by comparison of the efficiency of Pilates method in
reducing pain, provide improved functional capacity and daily activities, more
therapeutic interventions compared to minimal intervention (pharmacological)
are required.
As limitations
of this study, it is noteworthy the low rate of adhesion to treatment with
exercises, however, consistent with what is observed in current literature
[40]. In addition, the highest dropout rate in the study was among patients
with low SBST for both groups. One of the reasons reported for the withdrawals
of the participants in the Pilates group was the unavailability of time, as
well as the difficulty of traveling to the place where the appointments took
place. It is speculated also that individuals with low SBST have low adherence
to treatment due to an overestimation related to clinically acceptable minimum
change. Future studies are required to evaluate this possible relationship.
Conclusion
The
stratification in low and medium risks of poor prognosis in the primary
treatment, according to SBST-Brazil tool, has positive responses to treatment
based on Pilates exercises, considering the reduction in pain intensity and
functional incapacity.
Acknowledgments
We thank Instituto Valler Petrolina and Dr. Neydson André Solposto Marques de Souza, Orthopedic Surgeon and Sports
Medicine physician, for regular clinical monitoring during the research.
Conflict of interest
No conflicts of interest have been reported for this
article.
Financing source
The study was funded by National Council for
Scientific and Technological Development (CNPq)
through the Universal Call 01/2016 - Funding Code APQ 402444 / 2016-7 - and was
carried out with support from the Coordination for the Improvement of Higher
Education Personnel - Brazil (CAPES) - Code Funding 001.
Authors´s
contributions
Conception and design of the research:
Antonelli BA, Angelo RCO, Schwingel PA. Data collection:
Antoneli, BA, Nascimento LMS, Vasconcelos MDA. Analysis and interpretation of data:
Antonelli BA, Santos GA, Nascimento LMS, Vasconcelos MDA Statistical
analysis: Antonelli BA, Santos GA, Schwingel PA. Obtaining financing: Schwingel PA. Writing of the manuscript: Antonelli
BA, Santos GA, Schwingel PA. Critical revision of
the manuscript for important intellectual content: Angelo RCO.
References
- Hartvigsen J,
Hancock MJ, Kongsted A, Louw
Q, Ferreira ML, Genevay S et al. What low back pain
is and why we need to pay attention. The Lancet 2018;391(10137):2356-67. doi: 10.1016/s0140-6736(18)30480-x [Crossref]
- Nascimento PRCD, Costa LOP. Prevalência da dor lombar no Brasil: uma revisão sistemática. Cad Saúde Pública 2015;31(6):1141-56. doi: 10.1590/0102-311x00046114 [Crossref]
- Carvalho RC, Maglioni CB, Machado GB, Araújo JE, Silva JR, Silva ML. Prevalence and characteristics of chronic pain in Brazil: a national internet-based survey study. Br J Pain 2018;1(4):331-8. doi: 10.5935/2595-0118.20180063 [Crossref]
- Vos T, Abajobir AA, Abate KH, Abbafati C, Abbas KM, Abd-Allah F et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017;390(10100):1211-59. doi: 10.3410/f.731220250.793569875 [Crossref]
- Chenot JF, Greitemann B, Kladny B, Petzke F, Pfingsten M, Schorr SG. Non-specific low back pain. Dtsch Arztebl Int 2017;114(51-52):883-90. doi: 10.3238/arztebl.2017.0883 [Crossref]
- Foster NE, Anema JR, Cherkin D, Chou R, Cohen SP, Gross DP et al. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet 2018;391(10137):2368-83. doi: 10.1016/s0140-6736(18)30489-6 [Crossref]
- Stochkendahl MJ, Kjaer P, Hartvigsen J, Kongsted A, Aaboe J, Andersen M et al. National Clinical Guidelines for non-surgical treatment of patients with recent onset low back pain or lumbar radiculopathy. Eur Spine J 2018;27(1):60-75. doi: 10.1007/s00586-017-5099-2 [Crossref]
- Beneciuk JM, Bishop MD, Fritz JM, Robinson ME, Asal NR, Nisenzon NA et al. The STarT back screening tool and individual psychological measures: evaluation of prognostic capabilities for low back pain clinical outcomes in outpatient physical therapy settings. Phys Ther 2013;93(3):321-33. doi: 10.2522/ptj.20120207 [Crossref]
- Buchbinder R, van Tulder M, Öberg B, Costa LM, Woolf A, Schoene M et al. Low back pain: a call for action. Lancet 2018;391(10137):2384-88. doi: 10.1016/S0140-6736(18)30488-4 [Crossref]
- Bier JD, Sandee-Geurts JJ, Ostelo RW, Koes BW, Verhagen AP. Can primary care for back and/or neck pain in the Netherlands benefit from stratification for risk groups according to the STarT back tool classification? Arch Phys Med Rehabil 2018;99(1):65-71. doi: 10.1016/j.apmr.2017.06.011 [Crossref]
- Pauli, J, Starkweather A, Robins JL. Screening tools to predict the development of chronic low back pain: an integrative review of the literature. Pain Med 2019;20(9):1651-77. doi: 10.1093/pm/pny178 [Crossref]
- Pilz B, Vasconcelos RA, Marcondes FB, Lodovichi SS, Mello W, Grossi DB. The Brazilian version of STarT Back Screening Tool-translation, cross-cultural adaptation and reliability. Braz J Phys Ther 2014;18(5):453-461. doi: 10.1590/bjpt-rbf.2014.0028 [Crossref]
- Kamper SJ, Apeldoorn AT, Chiarotto A, Smeets RJEM, Ostelo RWJG, Guzman J et al. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain: Cochrane systematic review and meta-analysis. Cochrane Database Syst Rev 2014;(9):CD000963. doi: 10.1002/14651858.cd000963.pub3 [Crossref]
- Baillie L, Bacon CJ, Hewitt CM, Moran RW. Predictors of functional improvement in people with chronic low back pain following a graded Pilates-based exercise programme. J Bodyw Mov Ther 2019;23(1):211-8. doi: 10.1016/j.jbmt.2018.06.007 [Crossref]
- Yamato TP, Maher CG, Saragiotto
BT, Hancock MJ, Ostelo RW, Cabral CM et al. Pilates
for low back pain. Cochrane Database Syst Rev 2015;(7):CD010265. doi: 10.1002/14651858.cd010265.pub2 [Crossref]
- Amaral DDV, Miyamoto GC, Franco KFM, Santos FYR, Bastos NTO, Hancock MJ et al. Examination of a subgroup of patients with chronic low back pain likely to benefit more from Pilates-based exercises compared to an educational booklet. J Orthop Sports Phys Ther 2020;50(4):189-97. doi: 10.2519/jospt.2019.8839 [Crossref]
- Santos FYR, Liebano RE, Moura KF, Oliveira NTB, Miyamoto GC, Santos MO et al. Efficacy of the addition of interferential current to Pilates method in patients with low back pain: a protocol of a randomized controlled trial. BMC Musculoskelet Disord 2014;15:420. doi: 10.1186/1471-2474-15-420 [Crossref]
- Ford J, Story I, O'Sullivan P, McMeeken J. Classification systems for low back pain: a review of the methodology for development and validation. Phys Ther Rev 2007;12(1):33-42. doi: 10.1179/108331907x174961 [Crossref]
- Matsudo S, Araújo T, Marsudo V, Andrade D, Andrade E, Oliveira LC et al. Questionário internacional de atividade física (IPAQ): estudo de validade e reprodutibilidade no Brasil. Rev Bras Ativ Fis Saúde 2001;6(2):5-18. doi: 10.12820/rbafs.v.6n2p5-18 [Crossref]
- Ware Junior JE. SF-36 health survey update. Spine 2000;25(24):3130-9. doi: 10.1097/00007632-200012150-00008 [Crossref]
- Roland M, Morris R. A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine;8(2):141-4. doi: 10.1097/00007632-198303000-00004 [Crossref]
- Siqueira FB, Teixeira-Salmela LF, Magalhães LDC. Análise das propriedades psicométricas da versão brasileira da escala tampa de cinesiofobia. Acta Ortop Bras 2007;15(1):19-24. doi: 10.1590/s1413-78522007000100004 [Crossref]
- O'Sullivan P. It's time for change with the management of non-specific chronic low back pain. Br J Sports Med 2012;46(4):224-7. doi: 10.1136/bjsm.2010.081638 [Crossref]
- Balazcs E, Sieper J, Bickham K, Mehta A, Frontera N, Stryszak P et al. A randomized, clinical trial to assess the relative efficacy and tolerability of two doses of etoricoxib versus naproxen in patients with ankylosing spondylitis. BMC Musculoskelet Disord 2016;17(1):426. doi: 10.1186/s12891-016-1275-5 [Crossref]
- Nissen SE, Yeomans ND, Solomon DH, Lüscher TF, Libby P, Husni ME et al. Cardiovascular safety of celecoxib, naproxen, or ibuprofen for arthritis. N Engl J Med 2016;375(26):2519-29. doi: 10.1056/nejmc1702534 [Crossref]
- Angiolillo DJ, Weisman SM. Clinical pharmacology and cardiovascular safety of naproxen. Am J Cardiovasc Drugs 2017;17(2):97-107. doi: 10.1007/s40256-016-0200-5 [Crossref]
- Ho KY, Gwee KA, Cheng YK, Yoon KH, Hee HT, Omar AR. Nonsteroidal anti-inflammatory drugs in chronic pain: implications of new data for clinical practice. J Pain Res 2018;11:1937-48. doi: 10.2147/jpr.s168188 [Crossref]
- Cabral LL, Nakamura FY, Stefanello JM, Pessoa LC, Smirmaul BP, Pereira G. Initial validity and reliability of the Portuguese Borg rating of perceived exertion 6-20 scale. Meas Phys Educ Exerc Sci 2020;24(2):103-14. doi: 10.1080/1091367x.2019.1710709 [Crossref]
- Silva PHBD, Silva DFD, Oliveira JKDS, Oliveira FBD. Efeito do método Pilates no tratamento da lombalgia crônica: estudo clínico, controlado e randomizado. Br J Pain 2018;1(1):21-8. doi: 10.5935/2595-0118.20180006 [Crossref]
- Toscano JJDO, Egypto EPD. A influência do sedentarismo na prevalência de lombalgia. Rev Soc Bras Med 2001;7(4):132-7. doi: 10.1590/s1517-86922001000400004 [Crossref]
- Miyamoto GC, Franco KFM, van Dongen JM, Santos FYR, Oliveira NTB, Amaral DDV, et al. Different doses of Pilates-based exercise therapy for chronic low back pain: a randomised controlled trial with economic evaluation. Br J Sports Med 2018;52(13):859-68. doi: 10.1136/bjsports-2017-098825 [Crossref]
- Eliks M, Zgorzalewicz-Stachowiak M, Zeńczak-Praga K. Application of Pilates-based exercises in the treatment of chronic non-specific low back pain: state of the art. Postgrad Med J 2019;95(1119):41-5. doi: 10.1136/postgradmedj-2018-135920 [Crossref]
- Wells C, Kolt GS, Marshall P, Hill B, Bialocerkowski A. The effectiveness of Pilates exercise in people with chronic low back pain: a systematic review. Plos One 2014;9(7):e100402. doi: 10.1371/journal.pone.0100402 [Crossref]
- Fleming KM, Herring MP. The effects of Pilates on
mental health outcomes: a meta-analysis of controlled trials. Complement Ther Med 2018;37:80-95. doi: 10.1016/j.ctim.2018.02.003 [Crossref]
- Barbosa JES, Santos ALP, Oliveira MP, Sacramento MDS, Gomes VA, Petto J, Santos ACN. Influência do músculo diafragma no controle postural, na propriocepção e na dor lombar. Rev Bras Fisiol Exerc 2020;18(4):236-46. doi: 10.33233/rbfe.v18i4.3111 [Crossref]
- Jung SH, Hwang UJ, Ahn SH, Kim HA, Kim JH, Kwon OY. Lumbopelvic motor control function between patients with chronic low back pain and healthy controls: a useful distinguishing tool: the STROBE study. Medicine (Baltimore) 2020;99(15):e19621. doi: 10.1097/md.0000000000019621 [Crossref]
- Riis A, Rathleff MS, Jensen CE, Jensen MB. Predictive ability of the start back tool: an ancillary analysis of a low back pain trial from Danish general practice. BMC Musculoskelet Disord 2017;18(1):360. doi: 10.1186/s12891-017-1727-6 [Crossref]
- Qaseem A, Wilt TJ, McLean RM, Forciea MA. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med 2017;166(7):514-30. doi: 10.7326/m16-2367 [Crossref]
- Owen PJ, Miller CT, Mundell NL, Verswijveren SJJM, Tagliaferri SD, Brisby H et al. Which specific modes of exercise training are most effective for treating low back pain? Network meta-analysis. Br J Sports Med 2019;54:1279-87. doi: 10.1136/bjsports-2019-100886 [Crossref]
- Jack K, McLean SM, Moffett JK, Gardiner E. Barriers to
treatment adherence in physiotherapy outpatient clinics: a systematic review. Man Ther
2010;15(3):220-8. doi: 10.1016/j.math.2009.12.004 [Crossref]