Rev Bras Fisiol Exerc 2021;20(3):335-45
doi: 10.33233/rbfex.v20i3.4461
ORIGINAL ARTICLE
Influence of environmental temperature on aerobic
performance: physiological and perceptual responses in young adults
Influência
da temperatura ambiente no desempenho aeróbio: respostas fisiológicas e
perceptuais em adultos jovens
Flavio
de Souza Araujo1, Hiago Andrei de Lima
Pereira1, Geovani Alves dos Santos1, Gabriel Lucas Leite
da Silva Santos1, José Fernando Vila Nova de Moraes1
1Universidade Federal do Vale do São
Francisco - UNIVASF, Petrolina, PE, Brasil
Received:
November 20, 2020; Accepted:
March 30, 2021.
Correspondence: Flavio de Souza Araujo, UNIVASF
– CEFIS, Campus Petrolina, Av. José de Sá Maniçoba, S/N, Centro, 56304-917
Petrolina PE, Brazil
Flavio de Souza Araujo,
flavio.araujo@univasf.edu.br
Hiago Andrei de Lima Pereira,
hiagoandrei@hotmail.com
Geovani Alves dos Santos, geovani.ufrb@gmail.com
Gabriel Lucas Leite da Silva Santos, nuotogl@gmail.com
José Fernando Vila Nova de Moraes,
josefernando.moraes@univasf.edu.br
Abstract
Aim: The present study aimed to
analyze the influence of environmental temperature on physiological and
perceptual responses on aerobic performance in young adults. Methods:
Twelve male subjects (23.1 ± 3.3 years; 24.5 ± 3.0 kg/m²), underwent two
randomized sessions of incremental cycle ergometer tests in Heat condition
(32.7 ± 1.6ºC) and Thermoneutral (22.8 ± 0.6°C) 48-72 hours apart. Peripheral
temperature (PT), heart rate (HR), rate of perceived exertion (RPE), Thermal
sensation (TS), Feeling Scale (FS), maximum aerobic power (MAP) and exhaustion
time (ET) were measured. Results: During the Thermoneutral session, ET
and MAP were significantly higher when compared to Heat session (20.9 ± 4.1 min
vs. 19.5 ± 3.5 min; 212.9 ± 43.4 W vs. 198.3 ± 45.6 W; p < 0.05). PT and TS
were significantly higher in Heat session (p < 0.01). However, HR, RPE and
FS did not differ between sessions (p > 0.05). Conclusion: It is
concluded that, in young people, aerobic performance is lower in heat, mainly
influenced by the increase of PT and TS.
Keywords: exercise test; heat exhaustion;
physiology.
Resumo
Objetivo: O objetivo do presente estudo foi
analisar a influência da temperatura ambiente sobre as respostas fisiológicas e
perceptuais do desempenho aeróbio em adultos jovens. Métodos: Doze indivíduos
do sexo masculino (23,1 ± 3,3 anos; 24,5 ± 3,0 kg/m²) realizaram duas sessões
randomizadas de testes incrementais em cicloergômetro,
na condição Calor (32,7 ± 1,6ºC) e Termoneutro (22,8
± 0,6°C) com intervalo de 48-72 horas. Foram mensuradas temperatura periférica
(TP), frequência cardíaca (FC) percepção subjetiva de esforço (PSE), sensação
térmica (ST), valência afetiva (VA), potência aeróbia máxima (Pmax) e tempo de exaustão (TE). Resultados: Durante
a sessão Termoneutra, o TE e Pmax
foram significativamente maiores quando comparados a sessão Calor (20,9 ± 4,1
min vs. 19,5 ± 3,5 min; 212,9 ± 43,4 W vs. 198,3 ± 45,6 W; p < 0,05). A TP e
ST foram significativamente maiores na sessão Calor (p < 0,01). Porém, a FC,
PSE e VA não diferiram entre as sessões (p > 0,05). Conclusão:
Conclui-se que o desempenho aeróbio de jovens é menor no calor, influenciado
principalmente pelo aumento da TP e ST.
Palavras-chave: teste de esforço; exaustão por calor;
fisiologia.
Introduction
During the
practice of aerobic exercise, in a hot environment, physiological changes occur
such as dehydration and metabolic overload that can affect cardiovascular
function, causing an increase in sympathetic activity and heart rate, modifying
the neuromuscular response which could anticipate the fatigue process and
impair the performance [1,2]. Thus, the human body uses thermoregulatory
pathways of heat exchange with the environment to maintain body temperature in
stable physiological parameters [1]. Moreover, changes on exercise intensity
and volume can also interfere on cardiovascular load, increasing metabolism and
heat production in the human body [2].
The
cardiovascular system is one of the main limiters of performance in aerobic
exercise under heat stress. The increase of blood flow with cutaneous
vasodilation and a higher sweating rate provides serious challenges to the
regulation of cardiac output and increase of sympathetic activity [3,4]. Such
cardiovascular adjustments follow the increase of skin temperature, leading to
the increase of central temperature and resulting in a thermic discomfort and
decrease in the voluntary ability to perform exercise [5,6].
Excessive heat
production during exercise is one of the main determinants for a good aerobic
performance [7]. Thermic stimuli, provoked by the increase of metabolism, body
temperature and changes in attention, play a significant role in the modulation
of the perception of thermic stress and feelings of pleasure related to
exercise [8,9]. These increases in thermic stress can lead to a higher rate of
perceived exertion (RPE), which involves several integrated sensations, thus,
appearing as another limiter of performance [2,10].
Generally,
perceptual responses, beyond physiological responses, can interfere in
tolerance to exercise and in adhesion to exercise in heat [11]. Exercising in
hot environments can put the body under higher thermic, perceptual, and physiological
tension than exercising in thermoneutral environments, resulting in a premature
onset of fatigue and decreasing the time of tolerance
to exhaustion [6,7,8,12].
In this scenario, maximal incremental test
models have been proposed to estimate, evaluate, and prescribe aerobic exercise
capacity in different individuals. However, little is known about up to which
point the temperature of the environment can interfere in the results of these
evaluations [13]. Thus, the aim of the present study was to analyze the
influence of the temperature of the environment on physiological and perceptual
responses to aerobic performance in young adults.
Methods
Study design and ethical aspects
The present
study is characterized as a randomized crossed trial [14]. The study was
approved by the Research and Ethics Committee of the Federal University of Vale
of São Francisco (n° 2.462.622, CAAE: 80612717.3.0000.5196). All participants
were informed of the procedures of the research and signed a free informed
consent form, as required by the Resolution 466/12 of the Brazilian National
Health Council.
Sample’s characteristics
Based on the
calculation using GPower v. 3.0, considering α =
0.05, power = 0.80 and two experimental sessions with a minimum of two
measurements in each session, the sample size required for the study was 12
participants, considering the effect size of 0.45 proposed by Cuttell et al. [15] for time to exhaustion (TE) and
skin temperature.
Thus, the sample
was composed by 12 physically active males, aged between 18 to 30 years (23.1 ±
3.3 years; 24.5 ± 3.0 kg/m²) (Figure 1). The exclusion criteria were any
cardiometabolic disease or dysfunctions; having any bone, joint or muscle
impairments that could compromise the physical integrity and the participation
in the study; using any drugs related to blood pressure control or diabetes
mellitus; and not showing up to the experimental sessions.
General procedures
The participants
were invited to attend the laboratory for three visits in a period of two weeks
(Figure 2). In the first week/visit the participants answered the Physical
Activity Readiness Questionnaire (PAR-Q) [16], the short version of the
International Physical Activity Questionnaire (IPAQ) [17], underwent
anthropometric measurements and performed a familiarization session of the
incremental test (IT) on the cyclergometer. In the
second week/visits a cross-randomization (Microsoft Excel) was carried out, in
which, initially, half of the participants were assigned to the Heat session
(32.7 ± 1.6ºC) and the other half to the Termoneutro
session (22.8 ± 0.6°C), later the reverse procedure was applied, with a
difference of 48-72 hours between sessions (Figure 2). All sessions were
performed during the morning. The ambient temperature and the relative humidity
of the air were monitored by a thermohygrometer (Impac, IP-780). The sessions were standardized in the same
room, and the room temperature was reached using an air conditioning unit
(RHEEM - 9000 BTUs) and a heater (CONSUL - 1500W) adjusting to the desired
temperature.
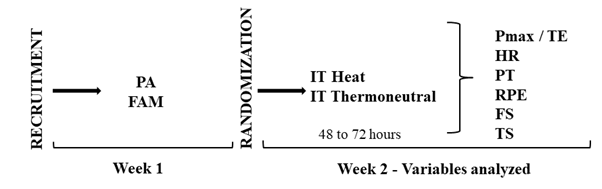
PA = physical
evaluation; FAM = familiarization; IT = incremental test; Pmax = maximal
aerobic power; TE = time to exhaustion: HR = heart rate; PT = peripheral
temperature; RPE = rate of perceived exertion; FS = feeling scale; TS = thermal
sensation
Figure 1 - Experimental
design of the study
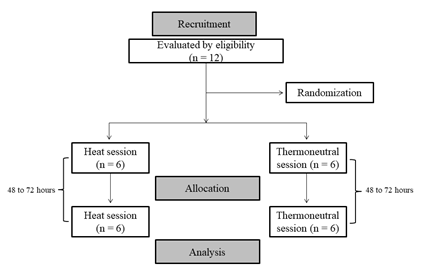
Figure 2 - Flowchart
of the study
Tests and aerobic sessions
In the second
week of the study the participants performed two randomized IT sessions in a
heated (32.7 ± 1.6 ºC) and thermoneutral (22.8 ± 0.6 ºC) environment with an
interval of 48-72 hours. The IT protocol was performed on a cyclergometer
(Cefis, Biotec 2100,
Brazil). The test began with 35 watts (W) of power and a speed of 70 rotations
per min (rpm), with increments of 35W every 3 min (stages) until maximal
voluntary exhaustion or not being able to maintain the pre-determined speed at
70 rpm [13]. At the end of each session, time to exhaustion (TE) and maximal
aerobic power (Pmax) were registered. In both IT sessions the following
physiological and perceptual variables were analyzed: coloration and specific
gravity of urine (SGU), peripheral temperature (PT), heart rate (HR), thermal
sensation (TS), rate of perceived exertion (RPE) and feeling scale (FS).
The participants
were advised to refrain from tobacco, caffeine and alcohol use or intake, as
well as not to perform physical activity in the 24 hours preceding the
sessions. To standardize the participants’ diets before IT, the subjects were
instructed, by a qualified nutritionist, to report their food consumption in
the 24 hours preceding the first session in order to
replicate the same diet 24 hours before the second session.
Heart rate and peripheral temperature
Heart rate (HR)
was measured using a heart rate monitor (RS800CX Polar®, ElectroOy,
Finland) [18] during 10 min at rest and at the last minute of each 3 min stage
of IT, in both conditions. Peripheral temperature (PT) was also measured during
10 min at rest and at the last minute of the 3 min stages. The analysis of
temperature was obtained from four different parts of the body (chest, arm, thigh,
and leg) through skin thermistors, attached to the participants using a
transparent waterproof adhesive, connected to a teletermometer
[15] (model THERM 37904, Viamed Ltd, West Yorkshire,
United Kingdom), as proposed by Ramanathan [19].
Scale of coloration and specific gravity of urine
When arriving in
the laboratory, the participants were asked to drink 0.5L of water, 60 min
before sessions. Thus, the participants provided a sample of urine to measure
the specific gravity of urine (SGU), using a portable refractometer (Biobrix, Model 301), which was previously calibrated
adjusting the scale with deionized water. The analysis of the scale of
coloration of the urine was also performed, in which values higher that 1.020
g·ml-1 (SGU) and coloration higher than 5 indicated levels of dehydration
[1,20]. These variables were measured before each IT session to evaluate the
hydration level of each participant.
Perceptual variables
Before the IT
sessions a verbal or memory anchorage of the RPE [21], FS [22] and TS [23,24]
scales was performed. The perceptions were analyzed during 10 min at rest and
at the last 20 seconds of each 3 min stage of the IT sessions.
ST was measured
using a seven-point scale in which the participant stated their sensation
according to the values -3 (very cold), -2 (cold), -1 (slightly cold), 0
(neutral = comfort), +1 (slightly hot), +2 (hot) and +3 (very hot), with the
possibility of choosing intermediary values [23,24,25].
The FS in
quantified from +5 to -5, corresponding, respectively, to two opposite
descriptors of the feeling during exercise (+5 = very good and -5 = very bad).
In addition to those, the scale also presents intermediary descriptors: +3 =
good; +1 = reasonably good; 0 = neutral; -1 = reasonably bad; -3 = bad [22,26].
Lastly, RPE was
measured using a perceived exertion scale (from 6 to 20 points), in which 7
corresponds to the lowest exercise intensity and 19 to the highest [21].
Statistical analysis
Data was
analyzed using descriptive statistics (mean and standard deviation). Shapiro
Wilk’s test was performed to verify data normality. Since data normality was
confirmed, inferential statistics were performed using two-way repeated
measures ANOVA with Bonferroni post hoc to compare between and within values of
both sessions (heat and thermoneutral). The level of significance adopted was p
< 0.05 and the effect size was reported using eta squared values (h²) (SPSS, version 22.0).
Results
Table I presents
the control variables (temperature of environment, relative air humidity,
specific gravity of urine and urine coloration) in both sessions. Results
showed that temperature of environment was significantly higher in the heat
session when compared to thermoneutral (p < 0.01). Relative air humidity,
SGU and urine coloration scale were similar in both sessions. Lastly, TE and
Pmax were higher in the thermoneutral session when compared to heat (p <
0.05).
Table I - Comparison
of control and performance variables during the maximum incremental aerobic
test with different environment temperatures
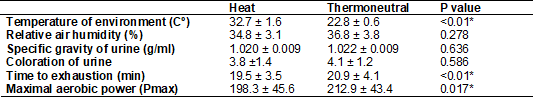
*p < 0.05
When comparing
HR and PT temperature in both sessions (Figure 3), statistically significant
differences were found for HR when comparing different stages of the same
session with values at rest (p < 0.01; h² = 0.961). However, no differences were found when
comparing stages between sessions (p = 0.83; h² = 0.021). PT, on the other hand, presented
significant differences to rest in stages of the same session (p < 0.01; h² = 0.891) as well as between stages of both sessions
(p < 0.01; h² =
0.398).
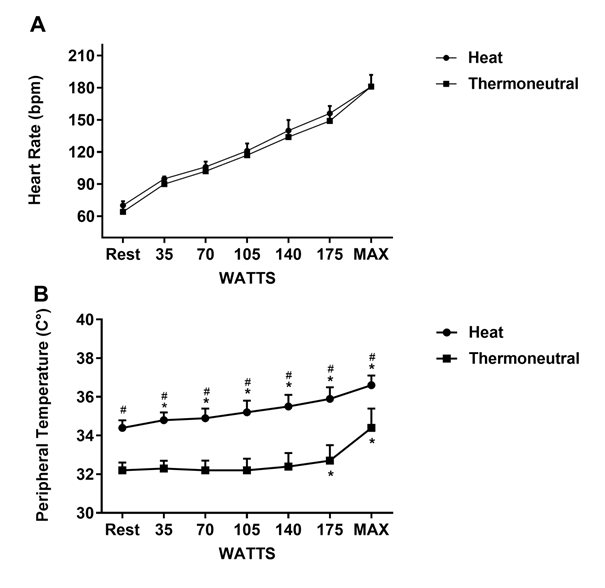
MAX = maximum watts; *p
< 0.05 when compared to rest in the same session; #p < 0.05 when compared
to the same stage in the thermoneutral session
Figure 3 - Heart
rate responses and peripheral temperature during maximum aerobic incremental
test in different environment temperatures
Statistically
significant differences were also found regarding the perceptual variables
(RPE, FS and TS) during the sessions (Figure 4). RPE showed differences when
comparing different stages of the same session to values at rest (p < 0.01; h² = 0.944), however, no differences were found when
comparing stages between sessions (p = 0.40; h² = 0.045). Likewise, FS presented statistical
differences when comparing stages to rest in the same session (p < 0.01; h² = 0.398), while no differences were found when
comparing stages between sessions (p = 0.850; h² = 0.020). Lastly, the analysis of TS showed
differences when comparing stages to rest in the same session (p < 0.01; h² = 0.810) and between sessions (p < 0.01; h² = 0.199).
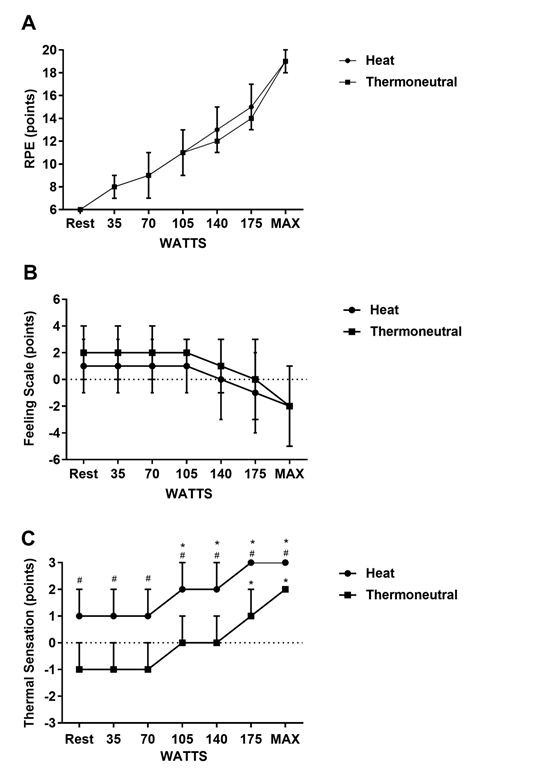
RPE = rate of perceived
exertion; MAX = maximum watts; *p < 0.05 when compared to rest in the same
session; #p < 0.05 when compared to the same stage in the thermoneutral
session
Figure 4 - Rate
of perceives exertion, affective valence, and thermal sensation responses
during maximum aerobic incremental test in different environment temperatures
Discussion
The present
study aimed to analyze the influence of environment temperature on the
physiological and perceptual responses to aerobic performance in young adults. To
do so, the temperature of the environment and levels of hydration of the
participants were controlled (Table I). The main findings showed lower aerobic
performance in a heated environment when compared to a thermoneutral one, with
lower TE and Pmax after IT (Table I). Moreover, when analyzing the
physiological responses, it was possible to observe that the participants’ PT
was higher in the heated session when compared to thermoneutral. However, HR
did not differ between sessions (Figure 3). Lastly, perceptual responses also
indicated a higher TS in the heated session when compared to thermoneutral,
which did not occur to RPE and FS when comparing sessions (Figure 4).
Studies show a
decrease in aerobic performance when exercise is performed in high temperatures
[4,6,27]. Possible mechanisms associated to this are related to alterations
caused by the stress induced to the central nervous system and skeletal muscle
functions, which could lead to a higher relative exercise intensity, increase
of cortisol levels, and decrease in maximal oxygen uptake [4,10]. Agreeing with
literature, the present study showed that during a maximum aerobic IT in heat,
TE and Pmax were lower than when compared to a thermoneutral session. However,
the exercise protocol used differs from previous studies, since the IT is
performed with incremental loads, causing an increase in intensity and a short
execution time. Thus, cooling strategies have been proposed to minimize the
effects of heat related to exercise, such as controlling hydration and wearing
cooling vests [1,15].
Changes in
exercise intensity and climate conditions can interfere in the cardiovascular load
since they modify the dissipation of heat and promote an increase in HR [2]. Natera et al. [28] verified the influence of environment in
HR responses during an incremental test in rugby athletes and found higher HR
values in an outdoor environment (34 ºC, 64.1% air humidity) than indoors (22
ºC, 50% air humidity). These results do not agree with the found in the present
study, since HR was similar in both IT sessions. However, it is important to
highlight that those cardiovascular adaptations can suffer interferences of
several factors beyond environmental conditions, such as exercise intensity and
duration [3]. Thus, it is suggested that the short duration of the IT sessions
performed in the present study, as well as the progressive increase of
intensity, may have masked differences in HR between sessions.
The results of
the present study also showed that during the maximum aerobic IT in heat
session, PT was higher in all stages than when compared to thermoneutral
(Figure 3). According to literature, performing exercise in hot environments
leads to an increase in body temperature. Therefore, thermoreceptors located
throughout the body detect changes in temperature and transmit this information
through afferent channels to the brain, altering the control of sensation and
thermic comfort and influencing the decrease of aerobic performance in heat
[6]. Changes in TS are results of dynamic increases and decreases in skin
temperature during exercise [7]. This corroborates with the present study’s
findings, in which throughout the whole maximum aerobic IT in heat, TS remained
higher than when compared to thermoneutral (Figure 4). The increase in PT and
TS demonstrates greater sensitivity to being influenced both by the intensity
of the exercise (increased load) and by the ambient temperature (Heat and
Thermoneutral), which did not occur with HR, RPE and FS, and which did not
differ between sessions.
The activation
of peripheral thermo sensors can also result in a conscious change of the
subjective thermal perception, which can include affective components related
to pleasure [7]. However, in the present study, FS did not differ between
sessions (Figure 4). In this scenario, Cheung et al. [8] verified that
exercise in heat under a constant workload resulted in higher cardiovascular
tension, promoting a higher thermic discomfort and changes in effort
perception. These results differ from the ones of the present study, since no
differences were found in RPE between sessions, as the tests were performed
with progressive intensities (Figure 4). Cleary et al. [29] demonstrated
that cooling strategies can modify thermal perception without altering RPE,
such a tool is widely used as a control variable for exercise intensity [30].
Thus, these two variables, FS and RPE, can also singly respond to aspects
related to exercise temperature and intensity, and intensity/load factor can overlap
and directly influence your responses.
Given the
exposed, it is recommended that the evaluation and prescription of aerobic
training, through maximum aerobic IT, reflect the environment in which exercise
is performed. So those professionals be alert that possible
changes in evaluations are derived from the temperature of the
environment, compromising the results of the prescription. Such information can
enhance the concept of exercise prescription related to health and performance
and improve the work of physical education and sports professionals [31].
Conclusion
Young adult physically active males presented
lower performance during maximum aerobic IT in heat when compared to a
thermoneutral condition. Such performance was influenced by an increase in PT
and TS in heat. However, HR, RPE and FS responses were not different between
conditions. In this scenario, the importance of controlling environment
temperature is highlighted when it comes to a good aerobic exercise
prescription and evaluation.
Conflict of interest
No conflicts of
interest have been reported for this article.
Financing source
There were no external
sources of funding for this study.
Authors’ contributions
Conception and design
of the research: Araujo FS, Pereira HAL, Moraes JFVN.
Data collection: Pereira HAL, Santos GA, Santos GLLS. Statistical analysis and
data interpretation: Araujo FS, Moraes JFVN. Writing
of the manuscript: Araujo FS, Pereira HAL. Critical review of the manuscript:
Santos GA, Santos GLLS. Final revision of the manuscript: Araujo FS, Moraes JFVN.
References
- Melo-Marins
D, Sousa-Silva AA, Silami-Garcia E, Laitano O. Termorregulação e equilibro hídrico no exercício
físico: aspectos atuais e recomendações. Rev Bras Ciênc Mov
2017;25(3):170-81. doi: 10.18511/rbcm.v25i3.6570 [Crossref]
- Pompermayer MG, Rodrigues R, Baroni BM, Lupion RDO, Meyer F, Vaz MA. Rehydration during exercise in the heat reduces the physiological strain index in healthy adults. Rev Bras Cineantropom Desempenho Hum 2014;16(6):629-37. doi: 10.5007/1980-0037.2014v16n6p629 [Crossref]
- Périard JD, Travers GJ, Racinais S, Sawka MN. Cardiovascular adaptations supporting human exercise-heat acclimation. Auton Neurosci 2016;196:52-62. doi: 10.1016/j.autneu.2016.02.002 [Crossref]
- Silva RPM, Barros CLM, Mendes TT, Garcia ES, Valenti VE, De Abreu LC, et al. The influence of a hot environment on physiological stress responses in exercise until exhaustion. PloS One 2019;14(2): e0209510. doi: 10.1371/journal.pone.0209510 [Crossref]
- Schlader ZJ, Simmons SE, Stannard SR, Mündel T. The independent roles of temperature and thermal perception in the control of human thermoregulatory behavior. Physiol Behav 2011;103(2):217-24. doi: 10.1016/j.physbeh.2011.02.002 [Crossref]
- Hartley GL, Flouris AD, Plyley MJ, Cheung SS. The effect of a covert manipulation of ambient temperature on heat storage and voluntary exercise intensity. Physiol Behav 2012;105(5):1194-1201. doi: 10.1016/j.physbeh.2011.12.017 [Crossref]
- Flouris AD, Schlader ZJ. Human behavioral thermoregulation during exercise in the heat. Scand J Med Sci Sports 2015; Suppl 1:52-64. doi: 10.1111/sms.12349 [Crossref]
- Cheung SS. Interconnections between thermal perception and exercise capacity in the heat. Scand J Med Sci Sports 2010;(Suppl3):53-9. doi: 10.1111/j.1600-0838.2010.01209.x [Crossref]
- Silva WQA, Fontes EB, Forti RM, Lima ZL, Machado DGDS, Deslandes AC, et al. Affect during incremental exercise: The role of inhibitory cognition, autonomic cardiac function, and cerebral oxygenation. PloS One 2017;12(11):e0186926. doi: 10.1371/journal.pone.0186926 [Crossref]
- Cheuvront SN, Kenefick RW, Montain SJ, Sawka MN. Mechanisms of aerobic performance impairment with heat stress and dehydration. J Appl Physiol 2010;109(6):1989-95. doi: 10.1152/japplphysiol.00367.2010 [Crossref]
- Rodrigues CA, Leites GT, Meyer F. Thermoregulatory and perceptual responses of lean and obese fit and unfit girls exercising in the heat. J Pediatr 2019;S0021-7557(18):30949-5. doi: 10.1016/j.jped.2018.12.011 [Crossref]
- Tyler CJ, Reeve T, Hodges GJ, Cheung SS. The effects of heat adaptation on physiology, perception and exercise performance in the heat: a meta-analysis. Sports Med 2016;46(11):1699-1724. doi: /10.1007/s40279-016-0538-5 [Crossref]
- Caputo F, Denadai BS. The highest intensity and the shortest duration permitting attainment of maximal oxygen uptake during cycling: effects of different methods and aerobic fitness level. Eur J Appl Physiol 2008;103(1):47-57. doi: 10.1007/s00421-008-0670-5 [Crossref]
- Nedel WL, Silveira F. Os diferentes delineamentos de pesquisa e suas particularidades na terapia intensiva. Rev Bras Ter Intensiva 2016;28(3):256-60. doi: 10.5935/0103-507X.20160050 [Crossref]
- Cuttell SA, Kiri V, Tyler CA. Comparison of 2 practical cooling methods on cycling capacity in the heat. J Athl Train 2016;51(7):525-32. doi: 10.4085/1062-6050-51.8.07 [Crossref]
- Andreazz IM, Takenaka VS, Da Silva PSB, Araújo MP. Exame pré-participação esportiva e o PAR-Q, em praticantes de academias. Rev Bras Med Esporte 2016;22(4):272-6. doi: 10.1590/1517-869220162204158121 [Crossref]
- Matsudo S, Araujo T, Matsudo V, Andrade D, Andrade E, Oliveira LC, et al. Questionário internacional de atividade física (I PAQ): Estudo de validade e reprodutibilidade no Brasil. Rev Bras Ativ Fís Saúde 2001;6(2):6-18. doi: 10.12820/rbafs.v.6n2p5-18 [Crossref]
- Williams DP, Jarczok MN, Ellis RJ, Hillecke TK, Thayer JF, Koenig J. Two-week test–retest reliability of the Polar® RS800CXTM to record heart rate variability. Clin Physiol Funct Imaging 2017;37(6):776–81. doi: 10.1111/cpf.12321 [Crossref]
- Ramanathan NL. A new weighting system for mean surface temperature of the human body. J Appl Physiol 1964;19:531-33. doi: 10.1152/jappl.1964.19.3.531 [Crossref]
- Armstrong LE, Maresh CM, Castellani JW, Bergeron MF, Kenefick RW, Lagasse KE, et al. Urinary indices of hydration status. Int J Sport Nutr 1994;4(3):265-79. doi: 10.1123/ijsn.4.3.265 [Crossref]
- Kaercher PLK,
Glänzel MH, Rocha GG, Schmidt LM, Nepomuceno P, Stroschöen L, et al. Escala
de percepção subjetiva de esforço de Borg como ferramenta
de monitorização da intensidade de esforço físico. RBPFEX 2018;12(80):1180-85.
- Alves ED, Panissa VLG, Barros BJ, Franchini E, Takito MY. Translation, adaptation, and reproducibility of the Physical Activity Enjoyment Scale (PACES) and Feeling Scale to Brazilian Portuguese. Sport Sci Health 2019;15(2):329-36. doi: 10.1007/s11332-018-0516-4 [Crossref]
- Faria VC, Lima LM, Pereira JC, Marins JCB. Variáveis psicofisiológicas durante exercício físico frente a diferentes condutas de alimentação e hidratação. Rev Bras Ciênc Esporte 2016;38(4):334-341. doi: 10.1016/j.rbce.2014.09.001 [Crossref]
- Straub KW, Leão EFTB, Kuchen E, Leão M. Determinação da temperatura de neutralidade em salas de aula do ensino superior para as zonas bioclimáticas do estado de Mato Grosso. Ambiente Construído 2017;17(1):97-109. doi: 10.1590/s1678-86212017000100126 [Crossref]
- Cunningham D, Stolwijk J, Wenger
C. Comparative thermoregulatory responses of resting men and women. J Appl Physiol
Respir Environ Exerc Physiol 1978;45(6):908-15. doi: 10.1152/jappl.1978.45.6.908 [Crossref]
- Frazão DT, Farias Junior LF, Dantas TCB, Krinski K, Elsangedy HM, Prestes J, et al. Feeling of pleasure to high-intensity interval exercise is dependent of the number of work bouts and physical activity status. PLoS One 2016;11(3):e0152752. doi: 10.1371/journal.pone.0152752 [Crossref]
- Nybo L, Rasmussen P, Sawka MN. Performance in the heat-physiological factors of importance for hyperthermia-induced fatigue. Compr Physiol 2014;4(2):657-89. doi: 10.1002/cphy.c130012 [Crossref]
- Natera AOW,
Jennings J, Oakley AJ, Jones TW. Influence of environmental conditions on performance
and heart rate responses to the 30-15 incremental fitness test in rugby union athletes.
J Strength Cond Res 2019;33(2):486-91. doi: 10.1519/JSC.0000000000001865 [Crossref]
- Cleary MA, Toy MG, Lopez RM. Thermoregulatory, cardiovascular, and perceptual responses to intermittent cooling during exercise in a hot, humid outdoor environment. J Strength Cond Res 2014;28(3):792-806. doi: 10.1519/JSC.0b013e3182a20f57 [Crossref]
- Arcenio LL. O uso de escalas de percepção subjetiva de esforço em periódicos nacionais. Rev Bras Fisiol Exerc 2019;18(1):23-31. doi: 10.33233/rbfe.v18i1.2799 [Crossref]
- Cortez ACL. Atividade física: da saúde a performance. Rev Bras Fisiol Exerc 2018;17(3):138-40. doi: 10.33233/rbfe.v17i3.2577 [Crossref]