Rev Bras Fisiol Exerc 2021;20(4):422-32
doi: 10.33233/rbfex.v20i4.4541
ORIGINAL ARTICLE
Is it possible that a cardiac rehabilitation program
can reduce the cardiovascular risk in individuals with metabolic syndrome?
É
possível que um programa de reabilitação cardíaca reduza o risco cardiovascular
em indivíduos com síndrome metabólica?
Ana
Denise Brandão1, Keila Larissa Pereira Reis1, Nathalia
Moraes Ribeiro1, Patricia Figueiredo1,
Daniela Martins de Fausto2, Antônio Adolfo Mattos de Castro2,
Elias Ferreira Porto1
1Universidade Adventista de São Paulo
(UNASP), São Paulo, SP, Brasil
2Universidade Federal do Pampa
(UNIPAMPA), Uruguaiana, RS, Brasil
Received:
December 28, 2020; Accepted:
June 14, 2021.
Correspondence: Elias Ferreira Porto, Estrada de Itapecerica da Serra
5859, 5858001 São Paulo SP. eliasfporto@gmail.com
Ana Denise Brandão: anadeniseb@hotmail.com
Keila Larissa Pereira Reis: keylalarissapr@hotmail.com
Nathalia Moraes Ribeiro Patricia
Figueiredo: nathaliamr@gmail.com
Daniela Martins de Fausto: dmfausto@gmail.com
Antônio Adolfo Mattos de Castro:
antonioamcastro@yahoo.com.br
Elias Ferreira Porto: eliasfporto@gmail.com
Abstract
Background: Metabolic
syndrome is a complex disorder represented by a set of cardiovascular risk
factors usually related to central fat deposition, insulin resistance,
hypertension, and dyslipidemia. It is associated with accelerated
atherosclerosis in response to chronic inflammation and vascular endothelial
dysfunction, increasing overall mortality. Objective: We aimed to
evaluate the effect of a cardiac rehabilitation program on cardiovascular risk
factors in patients with metabolic syndrome. Methods: This is
prospective interventional study. All patients underwent a 20-session cardiac
rehabilitation program with aerobic and resisted exercises as well as an educational
program for lifestyle changes. Results: Forty-seven patients
participated in the present study. After the cardiac rehabilitation program
(CRP), a significant reduction (p = 0,0092) for cardiovascular risk and fatigue
(p > 0.001) was observed; 78% of the patients had positive effects on
physical capacity, 72% of the patients presented HbA1c reduction, 51% increased
HDL-cholesterol, 70% reduced total cholesterol, 63% reduced triglycerides, 61%
reduced systolic blood pressure and 53% reduced diastolic blood pressure. Conclusion:
Cardiac rehabilitation program with aerobic and resisted exercises associated
with educational program for lifestyle changes is an effective approach in the
treatment of patients with metabolic syndrome mainly seen by a reduced
cardiovascular risk factors and reducing fatigue, improved physical capacity
and reduced components of metabolic syndrome.
Keywords: metabolic syndrome; diabetes; cardiac rehabilitation; lifestyle.
Resumo
Introdução: A síndrome metabólica é uma desordem
complexa representada por um conjunto de fatores de risco cardiovascular
geralmente relacionados à deposição central de gordura, resistência à insulina,
hipertensão e dislipidemia. Está associada à aterosclerose acelerada em
resposta à inflamação crônica e disfunção endotelial vascular, aumentando a
mortalidade geral. Objetivo: O objetivo foi avaliar o efeito de um
programa de reabilitação cardíaca sobre os fatores de risco cardiovascular em
pacientes com síndrome metabólica. Métodos: Este é um estudo prospectivo
de intervenção. Todos os pacientes foram submetidos a um programa de
reabilitação cardíaca de 20 sessões com exercícios aeróbicos e resistidos, além
de um programa educacional para mudanças no estilo de vida. Resultados:
Quarenta e sete pacientes participaram do presente estudo. Após o programa de
reabilitação cardíaca, observou-se redução significativa (p = 0,0092) para
risco cardiovascular e fadiga (p > 0,001); 78% dos pacientes tiveram efeitos
positivos na capacidade física, 72% dos pacientes apresentaram redução do
HbA1c, 51% aumentaram o colesterol HDL, 70% reduziram o colesterol total, 63%
reduziram os triglicerídeos, 61% reduziram a pressão arterial sistólica e 53%
reduziram a pressão arterial diastólica. Conclusão: Programa de
reabilitação cardíaca com exercícios aeróbicos e resistidos associado a um
programa educacional para mudanças no estilo de vida é uma abordagem eficaz no
tratamento de pacientes com síndrome metabólica por redução dos fatores de
risco cardiovascular e redução da fadiga, melhora da capacidade física e
redução dos componentes da síndrome metabólica.
Palavras-chave: síndrome metabólica; diabetes;
reabilitação cardíaca; estilo de vida.
Introduction
Metabolic
Syndrome (MS) is a complex disorder represented by a set of cardiovascular risk
factors usually related to central fat deposition, insulin resistance, hypertension,
and dyslipidemia. It is associated with cardiovascular disease increasing
overall and cardiovascular mortality up to two and threefold, respectively.
Studies have shown that the prevalence of MS is high and varies with age [1].
Its prevalence accounts for up to 21.8% and 23.7% of subjects with unadjusted
and adjusted age matched peers, respectively [2]. Prevalence increases from
6.7% among subjects aged 20-29 years to 43.5% and 42.0% for subjects aged 60-69
and at over 70 years, respectively [3].
Health-related
lifestyle can be a very effective strategy that is being used mainly in the
prevention of chronic degenerative diseases [4]. Some studies have already
shown positive associations between health-related lifestyle and components of MS
improvement: systemic arterial blood, hypertriglyceridemia, high blood glucose
and HDL-c reductions. In addition, cardiac rehabilitation programs are
considered adequate strategies for overall survival; it includes physical
training, eating habits reeducation, smoke cessation and stress management [5].
Adopting a
healthy lifestyle associated to a cardiopulmonary rehabilitation program may be
an effective low-cost alternative treatment to reduce cardiovascular diseases
risks, fatigue and loss of functional capacity associated to MS [6,7,8,9,10]. The aim
of this study was to evaluate the effectiveness of a cardiac rehabilitation
program and a therapeutic healthy lifestyle approach on the cardiovascular risk
factors, fatigue, and functional capacity of MS in adult volunteers.
Methods
This is a
prospective study. The Research Ethics Committee of UNASP approved this
research under the number 2.170.175, in agreement with Resolution No. 466/2012
of the National Health Council and Declaration of Helsinki (WMA, 2013) [11].
The sample of
this study consisted of 47 patients with MS invited to participate in our
facility Cardiac Rehabilitation Program (CRP). Both genders participated in the
study who presented minimally 3 of the 5 criteria for MS; also subject aged
between 40 and 60 years old. Patients with MS receiving chemotherapy, with
hemodynamic instability and uncontrolled arrhythmias were excluded.
To evaluate
cardiovascular risk, the Framingham Questionnaire was used; to assess
individual's lifestyle we used the Individual Lifestyle Profile (PEVI) [12]
questionnaire, and to evaluate global fatigue, the Chalder's Fatigue Scale
[13]. Every questionnaire was performed pre and post rehabilitation.
For
cardiovascular risk assessment, all patients underwent measurements of total
and fractioned cholesterol, triglycerides, fasting blood glucose, blood
pressure, weight, body mass index (BMI) and abdominal circumference. Also,
patients performed an incremental lower limb test (BRUCE treadmill protocol)
[14] and a six-minute walk test. All patients accomplished a comprehensive
cardiac rehabilitation program.
Framingham
cardiovascular risk has a score of 0 to 25 points, and the higher the score,
the higher the cardiovascular risk.
The global
fatigue was assessed using the Chalder scale, which has six questions. All
individuals should have answered the first two questions, and only individuals
who responded positively to the first two questions should have answered the
last four questions. The last four questions were ought to quantify the
individual's overall fatigue, and the higher the score, the greater the
fatigue.
To assess total,
fractionated cholesterol (HDL-C, LDL-C) triglycerides, fasting glucose and
Hb1Ac all participants underwent venous blood collection. Total cholesterol
below 200 mg/dl was considered normal. Reference values for LDL cholesterol
were < 130 mg/dl, for HDL in men was > 40 mg/dl and in women was > 50 mg/dl. Triglycerides were normal when the value
found was below 150 mg/dl on an empty stomach. For glycosylated hemoglobin
(Hb1Ac) a normal value was considered between 4.0 and 5.6%
Body composition
BMI was
classified according to criteria proposed by the World Health Organization (BMI
< 18.5 kg/m² was considered as low weight, BMI between 18.5 and 24.9 kg/m²
as eutrophic; BMI between 25 and 29.9 kg/m² as overweight; BMI between 30 and
34.9 kg/m² as grade I obesity; BMI between 35 and 39.9 kg/m² as grade II obesity
and BMI > 40 kg/m² as grade III obesity. For the elderly population aged 60
or over in this study, the classification recommended by the WHO was adopted in
which BMI up to 18.49 kg/m2 is classified as low weight, between
18.5 to 24.99 kg/m2 as eutrophic, between 25 and 29.9 kg/m2
as overweight and >
30kg/m2 as obesity.
MS was defined
using the International Diabetes Federation (IDF) diagnosis criteria. It
includes five components: waist circumference, blood pressure, high-density lipoprotein
(HDL) cholesterol, triglycerides, and fasting glucose. 3 abnormal results
assume the MS diagnosis.
Cardiac rehabilitation program
Patients with
metabolic syndrome performed a comprehensive rehabilitation program with 20
sessions, each lasting 60 minutes, 4 times per week. All patients were assessed
by our team doctors and then referred to rehabilitation. Each session had 30
minutes of aerobic training for lower limbs on a treadmill. This training
started with 3 minutes of warm-up, with 2.6 km/h of speed, twenty-two minutes
at a fixed speed and treadmill inclination ranging from 60 to 80% intensity of
the maximum value reached during the Bruce protocol; finally, the last five
minutes had 2.7km/h speed decreased for cool down purposes.
Upper limbs and
lower limbs strengthening exercises comprised of 15 minutes each; 2 sets of 10
reps for each exercise (with dumbbells and ankle weights ranging from 1 to 3
kg, theraband and Swiss ball). Specific loads were given for each individual
and an interval of 60 seconds between each exercise was provided.
The participants
were encouraged to practice health-promoting practices, through classes three
times per week by our physiotherapists, athletic trainers, and nutritionists.
Adoption of a diet rich in fruits and vegetables was oriented to meet metabolic
targets [15] (mostly 3 to 5 times a day of fruit intake - the diet provided was
comprehensive and, generally, oriented to all). No individual diet consult was
provided; we oriented physical activity practice for at least 30 minutes three
times a week, breathing fresh air and frequent water intake, smoking cessation
and avoidance of alcoholic beverages and soft drinks, 7-8 h/day of sleeping
period, adequate exposure to sunlight [16].
Statistical analysis
The Shapiro-Wilk
normality test was used to evaluate the distribution of data in relation to
normality. The data are presented in mean and standard deviation, the paired
test was used to compare the differences between the anthropometric variables
and the functional capacity before and after intervention within groups.
Proportions were analyzed using the chi square test. Univariate logistic
regression analysis was used to identify which baseline variables were
significantly associated with being a non-responder treatment patient. Due to
the small number of non-responder patients, a multivariate logistic regression
model was performed including the four baseline variables that showed the
strongest association for being a non-responder in the univariate analyses. p
< 0.05 was considered as statistically significant.
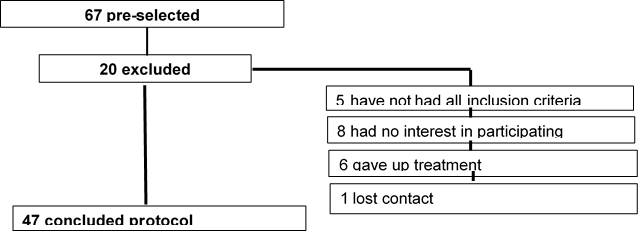
Figure 1 – Selection of the
participants.
Results
The sample
consisted of 47 patients with metabolic syndrome; out of these, 70.2% were
female (n = 33). Sample’s age ranged from 53 to 69 years. BMI was classified
according to criteria proposed by the World Health Organization [17].
29.5% patients
with grade I obesity, 27.7% with grade II obesity and 23.4% with grade III
obesity. Initially, only 8% of patients had their blood arterial hypertension
controlled, 55% of patients had total cholesterol over 200 mg/dl, 64.2% had low
HDL, 31.9% had high LDL and 76.5% had high triglycerides.
None of the
women presented belly obesity; on the other hand, 28% of men presented
abdominal circumference < 102 cm. After the cardiac rehabilitation program
there was an increase in patients’ proportion who had controlled blood pressure
and total cholesterol lower than 200 mg/dl (Table I).
Table I - Demographic
characteristics at baseline and after cardiac rehabilitation
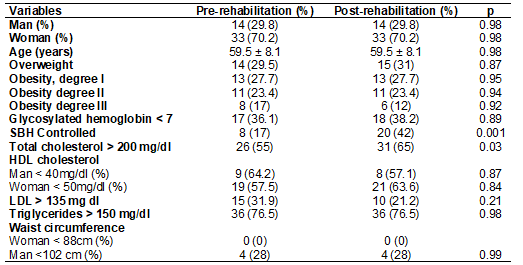
HDL = high density
lipoprotein, LDL = low density lipoprotein
After the
cardiac rehabilitation program, we observed that 55.3% of patients reduced BMI
and 59.6% reduced belly obesity. Overall fatigue reduced significantly (p >
0.001). It was also observed an increased six minutes walking distance at the
SMWT (p > 0.001) and a Bruce protocol duration test (p = 0.0008) (Table II).
Table II - Comparison
of anthropometric results and physical capacity before and after intervention
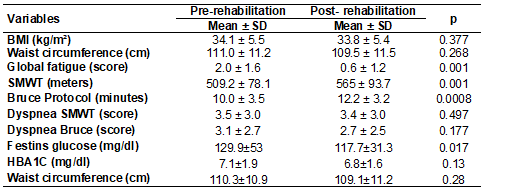
BMI = Body Mass Index;
SMWT = six minutes walking test; HBbA1c = glycosylated hemoglobin; SD =
standard deviation
Figure 1
compares the Framingham scores before and after the cardiac rehabilitation
program. At the end of the program, the cardiovascular risk reduction was
statistically significant in our patients with metabolic syndrome (p = 0.0092,
Figure 1).
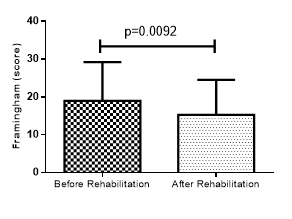
Figure 2 – Comparison of
the Framinghan score for cardiovascular risk before and after rehabilitation
Table III - Univariate
baseline predictors of being a non-responder to cardiac rehabilitation and
lifestyle programs in patients with metabolic syndrome
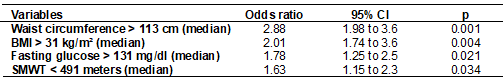
BMI = Body Mass Index;
SMWT = six minutes walking test; HbA1c = glycosylated hemoglobin
We created a
multivariate logistic regression model containing the four baseline variables
most closely associated with being a non-responder patient considering the
univariate analyses (Table IV). High waist circumference, BMI and fasting
glucose, low physical capacity in the six-minute walk test were variables that
remained significant predictors of maintaining the diagnosis of MS (table IV).
Table IV - Multivariate
predictors of being a non-responder to cardiac rehabilitation and exercise
training programs in the entire metabolic syndrome cohort
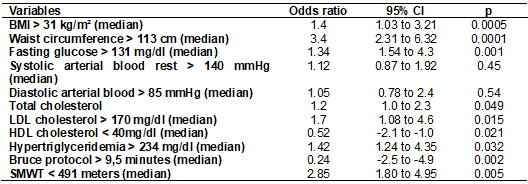
BMI = Body Mass Index;
SMWT = six minutes walking test
Discussão
The objective of
this study was to evaluate the effect of a cardiac rehabilitation program on
cardiovascular risk factors of patients with metabolic syndrome. Among the main
results of this study, we can highlight that, after the cardiac rehabilitation
program, there was reduction for cardiovascular risk (Framingham score). 78% of
our patients had a positive effect on physical ability, 72% had hemoglobin
glycosylated reduction, 51% increased HDL cholesterol, 70% reduced total
cholesterol, 63% reduced triglycerides, 61% reduced SBP, 53% reduced DBP and 5%
reduced overall fatigue.
Pontes et al.
[18], while evaluating the effects of physical exercises in metabolic syndrome
patients, also noticed significant reductions in cardiovascular risk assessed
by the Framingham Score. Other authors showed that physical inactivity is one
of the leading modifiable risk factors for global mortality in these patients -
an estimated 20% to 30% increased risk of death compared with those who are
physically active [19]. Physically active people of all age groups have higher
levels of cardiorespiratory fitness, health, wellness, and a lower risk for
developing several chronic medical illnesses, including cardiovascular disease
- compared with those who are physically inactive [20,21]. Another study [22],
also obtained significant values for reduction of cardiovascular risk with
exercise and lifestyle changes in a sample of obese, hypertensive and
dyslipidemic women.
The positive
effects to reduced cardiovascular risk caused by the aerobic training are
associated with the speed and load imposed on the treadmill. Pontes et al. [18]
confirm that disease burden imposes a positive impact on the cardiorespiratory
performance. In this study, training speed was based on maximal heart rate and
a load of 60 to 80% of maximum HR was applied. When performing exercise in this
modality, some effects are known such as the increase of the shear stress
mediated by the flow in the arteries walls that improves endothelial function.
This mechanism increases the synthesis and release of nitric oxide that leads
to endothelium vasodilation and inhibits multiple processes involving
atherogenesis and thrombosis [23].
One of the ways
to reduce cardiovascular risk is to reduce blood pressure. The mechanism for
blood pressure reduction is already well described both at short and long term;
the short term it is due to the release of pro-vasodilation factors by the
vascular endothelium after moderate to high intensity load exercise. In the
long term, it occurs by vascular neo-formation in the muscles during
anaerobiosis [24]. Reductions of only 2 mmHg in diastolic blood pressure can
substantially reduce the risk of diseases and deaths associated with
hypertension [25].
Aerobic training
may reduce the risk of death from cardiac events due to reduced ventricular
tachyarrhythmias by reducing sympathetic activity and increasing
parasympathetic (vagal) activity, as evidenced by increased heart rate
variability and increased baroreceptor sensitivity [23].
When assessing
fatigue by Chalder's scale, patients in our study reported a significant
decrease in fatigue after CRP. Fatigue symptoms may be due in part to the
inability of the muscle to use oxygen reducing heart overload [26,27,28]. Physical
exercise can reverse this situation through adaptations of skeletal muscle,
such as improvement of mitochondrial capacity, decrease of insulin resistance
[3] and reduction of systemic oxidative stress and improvement in well-being
[29].
A systematic
review with a meta-analysis [30] that evaluated cardiovascular risk factors
during exercise testing in metabolic syndrome patients observed significant
mean reductions in waist circumference, blood pressure, HDL cholesterol,
glucose, and triglycerides.
Aerobic and
resistive physical exercises have positive effects on insulin sensitivity [27].
One study showed that exercises have effects on insulin sensitivity between 12
and 48 hours after exercise, but these changes returned to pre-activity levels
3 to 5 days after the last exercise session. Exercise improves the dyslipidemic
profile by increasing the ability of muscle tissue to consume fatty acids and
increases the activity of the lipoprotein lipase enzyme in the muscle, causing
an improvement in dyslipidemia in individuals with MS [31].
As previously shown
[32,33], therapeutic lifestyle changes and cardiac rehabilitation programs can
be extremely beneficial for MS patients. Other studies have seen clinical
improvement in MS patients such as ours [34,35]. For instance, Met Fit program
showed significant reductions in waist circumference, body fat, systolic and
diastolic blood pressures in those patients accomplishing a comprehensive
12-week sessions of 45 minutes of exercise and 45 minutes of education. The
target 150 to 200 minutes weekly exercise and 5% loss in body weight were
achieved by all patients [34]. Another study showed a significant improvement
at 6 weeks and at 6 months period in waist circumference, body weight,
diastolic blood pressure, and total cholesterol occurred in 240 patients with MS
after a cardiometabolic program [35].
This study
brings important clinical applications mainly related to the fact that cardiac
rehabilitation program and small lifestyle changes may improve cardiovascular
risk in patients with MS. The limitations of this study are related to the fact
that we only measured the behavior of these variables after the cardiac
rehabilitation program, not being able to measure the effects over a long
period, as well as to follow other end points such as hospitalization and
mortality. However, this cannot invalidate our results.
Conclusion
After evaluating
the effect of the cardiac rehabilitation program on the cardiovascular risk
factors, physical capacity, and metabolic changes in patients with metabolic
syndrome, our study can conclude that this is an effective result in the
treatment of these patients by reducing cardiovascular risk factors, fatigue,
blood pressure, triglycerides, total cholesterol and LDL cholesterol and
fasting glucose and improving physical ability and HDL cholesterol.
Conflict of interest
No conflict of interest
with relevant potential.
Financing source
Own financing
Authors' contributions
Data acquisition and
analysis: Brandão AD, Reis KLP, Ribeiro NM, Figueiredo P; Data interpretation: Figueiredo
P, Castro AAM; Work draft and substantially revised; Castro AAM, Fausto DM,
Porto EF; Substantial contributions to the conception, design of the work,
approved the submitted version: Porto EF
References
- Kuschnir MCC,
Bloch KV, Szklo M, Klein CH, Barufaldi
LA, Abreu GDA, Moraes AJ PD. ERICA: prevalence of
metabolic syndrome in Brazilian adolescents. Rev Saúde
Pública 2016;50(11):256-68. doi: 10.1590/S01518-8787.2016050006701 [Crossref]
- Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults findings from the third National Health and Nutrition Examination Survey. JAMA 2002;287(3):356-9. doi: 10.1001/jama.287.3.356 [Crossref]
- Tjønna AE, Lee SJ, Rognmo Ø, Stølen TO, Bye A, Haram PM, et al. Aerobic interval training versus continuous moderate exercise as a treatment for the metabolic syndrome. Circulation 2008;118(4):346-54. doi: 10.1161/CIRCULATIONAHA.108.772822 [Crossref]
- Porto EF, Souza AC. Health promotion and lifestyle: limitations and perspectives. Lifesytle Journal 2016;4(2):7-9. doi: 10.19141/2237-3756.lifestyle.v3.n2.p7-10 [Crossref]
- Takahara M, Shimomura I. Metabolic syndrome and lifestyle modification. Rev Endocr Metab Dis 2014;15(4):317-27. doi: 10.1007/s11154-014-9294-8 [Crossref]
- Lavie CJ, Milani RV. Cardiac rehabilitation and exercise training programs in metabolic syndrome and diabetes. J Cardiopulm Rehabil 2005;25(2):59-66. doi: 10.1097/00008483-200503000-00001 [Crossref]
- Savage PD, Banzer JA, Balady GJ, Ades PA. Prevalence of metabolic syndrome in cardiac rehabilitation/secondary prevention programs. American Heart Journal 2005;149(4):627-31. doi: 10.1016/j.ahj.2004.07.037 [Crossref]
- Lavie CJ, Morshedi, Meibodi A, Milani RV.
Impact of cardiac rehabilitation on coronary risk factors, inflammation, and
the metabolic syndrome in obese coronary patients. J Cardiometab Syndr 2008;3(3):136-40. doi: 10.1111/j.1559-4572.2008.00002.x [Crossref]
- Galvão TF, Pereira MG. Systematic reviews of the literature: steps for preparation. Epidemiol Serv Saúde 2014;23(1):183-4. doi: 10.5123/S1679-49742014000100018 [Crossref]
- Santos CMDC, Pimenta, CADM, Nobre MRC. The PICO strategy for the research question construction and evidence search. Rev Latinoam Enferm 2007;15(3):508-511. doi: 10.1590/s0104-11692007000300023 [Crossref]
- World Medical Association (WMA). Declaration of
Helsinki. [Internet]. 2013
[cited 2021 Jun 12]. Available from:
http://www.wma.net/en/30publications/10policies/b3/
- Castro JBP, Souza Vale RG, Aguiar RS, Silva Mattos R. Perfil do estilo de vida de universitários de Educação Física da cidade do Rio de Janeiro. Revista Brasileira de Ciência e Movimento 2017;25(2):73-83. doi: 10.18511/rbcm.v25i2.6234 [Crossref]
- Chalder T, Berelowitz G, Pawlikowska T, Watts L, Wessely S, Wright S, Wallace EP. Development of a fatigue scale. Journal of Psychosomatic Research 1993;37(2):147-53. doi: 10.1016/0022-3999(93)90081-P [Crossref]
- Karvonen JJ, Kentala E, Mustalam O. The effects of training on heart rate: a “longitudinal” study. Ann Med Exp Biol Fenn 1957;35:307-15. doi: 10.1038/sj.jhh.1002173 [Crossref]
- Fung TT, Hu FB, Wu K, Chiuve SE, Fuchs CS, Giovannucci E. The Mediterranean and Dietary Approaches to Stop Hypertension (DASH) diets and colorectal cancer. Am J Clin Nutr 2010;92(6):1429-35. doi: 10.3945/ajcn.2010.29242 [Crossref]
- Meira
MDD, Abdala GA, Teixeira CA, Ninahuaman MFM, Moraes
MCL. Profile of adult lifestyle of São Paulo south zone. Life
Style Journal [Internet]. 2015 [cited 2021 Jun 12];2(2):29-45.
https://revistas.unasp.edu.br/LifestyleJournal/article/view/607
- World Health Organization (WHO). The top 10 causes of
death. 2016 [cited 2018 April 15]. Available from:
http://www.who.int/mediacentre/factsheets/fs310/en/index3.html
- Pontes HT, Araujo SP, CorrêA CD, Cerqueira PA, Oliveira NC, Portes LA. Supervised physical activity and metabolic syndrome components of women assisted in primary health care. J Metabolic Synd 2012;1(111):2167-0943. doi: 10.4172/2167-0943.1000111 [Crossref]
- Fletcher GF, Landolfo C, Niebauer J, Ozemek C, Arena R, Lavie CJ. Promoting physical activity and exercise: JACC health promotion series. J Am Coll Cardiol 2018;72(14):1622-39. doi: 10.1016/j.jacc.2018.08.2141 [Crossref]
- Ozemek C, Lavie CJ, & Rognmo Ø. Global physical activity levels-Need for intervention. Prog Cardiovasc Dis 2019;62(2):102-7. doi: 10.1016/j.pcad.2019.02.004 [Crossref]
- Lavie CJ, Ozemek C, Carbone S, Katzmarzyk PT, Blair SN. Sedentary behavior, exercise, and cardiovascular health. Circ Res 2019;124(5):799-815. doi: 10.1161/CIRCRESAHA.118.312669 [Crossref]
- Chagas EFB, Bonfim MR, Brondino NCM, Monteiro HL. Physical exercise and cardiovascular risk factors in obese women in the postmenopausal period. Rev Bras Med Esporte 2015;21(1):65-9. doi: 10.1590/1517-86922015210101834 [Crossref]
- Leon AS, Franklin BA, Costa F, Balady
GJ, Berra KA, Stewart KJ, Lauer MS. Cardiac rehabilitation
and secondary prevention of coronary heart disease. Circulation 2005;111:369-76. doi: 10.1161/01.CIR.0000151788.08740.5C [Crossref]
- Porto
EF, Kumpel C, Portes LA, Leite JRO. Comparative
study between two methods of supervised and semi-supervised cardiac
rehabilitation on maximal oxygen consumption and functional capacity. Rev Soc Cardiol Estado de São Paulo [Internet]. 2007 [cited 2021 Jun 12];17(2):18-24. Available
from: https://pesquisa.bvsalud.org/portal/resource/pt/lil-461835
- Ciolac EG, Guimarães GV. Ejercicio físico y síndrome metabólico. Rev Bras Med Esporte 2004;10(4)319-24. doi: 10.1590/S1517-86922004000400009 [Crossref]
- Pozehl B, Ducan K, Hertzog M. The effects of exercise training on fatigue and dyspnea in heart failure. Eur J Cardiovasc Nurs 2008;7(2):127-132. doi: 10.1016/j.ejcnurse.2007.08.002 [Crossref]
- Jackson L, Leclerc J, Erskine Y, Linden W. Getting the
most out of cardiac rehabilitation: a review of referral and adherence
predictors. Heart 2005;91(1):10-14. doi: 10.1136/hrt.2004.045559 [Crossref]
- Mann DL, Reid MB. Exercise training and skeletal muscle inflammation in chronic heart failure: feeling better about fatigue. J Am Coll Cardiol 2003;42(5):869-72. doi: 10.1016/S0735-1097(03)00847-7 [Crossref]
- Windthorst P, Mazurak N, Kuske M, Hipp A, Giel KE, Enck P, Nieb A, Zipfel S, Teufel M. Heart rate variability biofeedback therapy and graded exercise training in management of chronic fatigue syndrome: An exploratory pilot study. J Psychosom Res 2017;93:6-13. doi: 10.1016/j.jpsychores.2016.11.014 [Crossref]
- Pattyn N, Cornelissen VA, Eshghi SRT, Vanhees L. The effect of exercise on the cardiovascular risk factors constituting the metabolic syndrome. Sports Med 2013;43(2):121-33. doi: 10.1007/s40279-012-0003-z [Crossref]
- Chagas EFB, Bonfim MR, Brondino NCM, Monteiro HL. Physical exercise and cardiovascular risk factors in obese women in the postmenopausal period. Rev Bras Med Esporte 2015;21(1):65-9. doi: 10.1590/1517-86922015210101834 [Crossref]
- Milani RV, Lavie CJ. Prevalence and profile of metabolic syndrome in patients following acute coronary events and effects of therapeutic lifestyle change with cardiac rehabilitation. Am J Cardiol 2003;92(1):50-4. doi: 10.1016/s0002-9149(03)00464-8 [Crossref]
- Lavie CJ, Milani RV, O'Keefe JH. Dyslipidemia intervention in metabolic syndrome: emphasis on improving lipids and clinical event reduction. Am J Med Sci 2011;341(5):388-93. doi: 10.1097/MAJ.0b013e31821483fa [Crossref]
- Rubenfire M, Mollo L, Krishnan S, Finkel S, Weintraub M, Gracik T, Kohn D, Oral EA. The metabolic fitness program lifestyle modification for the metabolic syndrome using the resources of cardiac rehabilitation. J Cardiopulm Rehabil Prev 2011;31:282-9. doi: 10.1097/HCR.0b013e318220a7eb [Crossref]
- Rodriguez-Escudero JP, Somers VK, Heath AL, Thomas RJ, Squires RW, Sochor O, Lopez-Jimenez F. Effect of a lifestyle therapy program using cardiac rehabilitation resources on metabolic syndrome components. J Cardiopulm Rehabil 2013;33(6):360-70. doi: 10.1097/HCR.0b013e3182a52762 [Crossref]