Rev Bras Fisiol Exerc 2021;20(1):52-63
doi: 10.33233/rbfex.v20i1.4011
ORIGINAL ARTICLE
Effects of dual-task exercise on postural instability
and respiratory parameters in patients with Parkinson's disease
Efeitos
do exercício físico de dupla tarefa sobre a instabilidade postural e parâmetros
respiratórios em pacientes com doença de Parkinson
Hérica
Salvaro Fernandes1, Talita Tuon2,
Miguel Rosado1, Paulo Roberto Lino1, Ricardo A. Pinho3
1Universidade do Extremo Sul Catarinense,
Criciúma, SC, Brazil
2Universidade Federal de Santa Catarina,
Florianópolis, SC, Brasil
3Pontifícia Universidade Católica do
Paraná, Curitiba, PR, Brasil
Received:
April 9, 2020; accepted:
July 20, 2020.
Correspondence: Talita Tuon, Programa de
Pós-graduação em Ciências do Movimento Humano, Universidade Federal de Santa
Catarina, Campus Araranguá,
Unidade
Mato Alto, Rua Pedro João Pereira, 150 Mato Alto 88905-120 Araranguá SC
Hérica Salvaro
Fernandes: hericasalvaro@hotmail.com
Talita Tuon: talitatuon@gmail.com
Miguel Rosado: miguelrosara@outlook.com
Paulo Roberto Lino: paulolin0@hotmail.com
Ricardo A. Pinho: rapinho12@gmail.com
Abstract
Introduction: Parkinson’s
disease presents physiological changes that compromise the patient’s daily
physical behavior, altering postural instability as well as injuries on the
respiratory system. Objectives: The aim of the present study was to
verify the quality of life and the effects of dual-task exercise on postural
instability and respiratory parameters in patients with Parkinson’s disease. Methods:
Fourteen patients underwent dual-task exercises (vestibular and respiratory), 3
times a week and lasting 45 minutes for a period of 60 days. Quality of life,
disease staging, respiratory indicators, physical fitness, and vestibular
parameters were evaluated before and 48 hours after the intervention period. Results:
The quality of life indicators, such as mobility, activity of daily living,
emotional well-being, stigma, cognition, communication, and body discomfort,
showed a statistically significant difference when compared to baseline data.
Lung function, physical fitness and vestibular system data showed improvement
after the intervention program. Conclusion: The results obtained suggest
that the effects of dual-task physical exercise in PD patients with Parkinson´s
disease have positive effects on behavioral and functional aspects involved in
the quality of life, contributing to the regulation of the vestibular system.
Keywords: Parkinson's disease; physical
exercise; muscle strength; balance; breath.
Resumo
Introdução: A doença de Parkinson (DP) apresenta
alterações fisiológicas que comprometem o comportamento físico diário do
paciente alterando a instabilidade postural bem como agravos sobre o sistema
respiratório. Objetivos: o objetivo do presente estudo foi verificar a
qualidade de vida e os efeitos do exercício físico de dupla tarefa sobre a
instabilidade postural e parâmetros respiratórios em pacientes com doença de
Parkinson. Métodos: Quatorze pacientes com DP foram submetidos a
exercícios de dupla-tarefa (vestibulares e respiratórios), 3 vezes por semana e
duração de 45 minutos por um período de 60 dias. Indicadores de qualidade de
vida, estadiamento da doença, respiratórios, aptidão física e parâmetros
vestibulares foram avaliados antes e quarenta e oito horas após o período de
intervenção. Resultados: Os indicadores de qualidade vida de pacientes
com DP como mobilidade, atividade de vida diária, bem-estar emocional, estigma,
cognição, comunicação e desconforto corporal apresentaram diferença
estaticamente significativa quando comparadas aos dados basais. Dados de função
pulmonar, de aptidão de física e do sistema vestibular, apresentaram melhora
após o programa de intervenção. Conclusão: Os resultados obtidos sugerem
que os efeitos do exercício físico de dupla tarefa em pacientes com DP exercem
efeitos positivos sobre aspectos comportamentais e funcionais implicados na
qualidade de vida de pacientes com DP, contribuem para a regulação do sistema
vestibular.
Palavras-chave: doença de Parkinson; exercício físico;
força muscular; equilíbrio; respiração.
Introduction
Parkinson's
disease (PD) is a progressive, slow, and irreversible neurodegenerative
disease, with an estimated prevalence of 1 to 3% in the world population aged
over 55 years, with its main neuropathological characteristic being the loss of
dopaminergic neurons [1,2]. The reduction in dopaminergic neurons may be
associated with different mechanisms, including oxidative stress, excitoxicity, homeostatic calcium disturbance,
inflammation, genetic factors, apoptosis, environmental factors and protein
aggregation [1,3,4] which compromise daily physical behavior altering postural
instability [5], as well as causing damage to the respiratory system [6].
Postural
instability has been identified as one of the main complaints by PD patients
[7] in which disturbances in sensory information, impaired sensory motor
processing and impaired motor coordination affect the patient's postural
control [8]. In addition, PD promotes dysfunctions of the respiratory system,
such as dyspnea, hypoventilation, atelectasis, retention of pulmonary
secretions, abnormalities associated, mainly with a greater predisposition to
respiratory infections, decreased chest mobility and peak expiratory flow [8].
These dysfunctions are associated with muscle stiffness and this induces a loss
of flexibility in the respiratory muscles. Postural changes that, as a hyperkyphotic
pattern, influence the lower chest expansion resulting in less lung volumes and
restrictive ventilation deficit, changes in muscle activation and coordination
and involvement of the upper airways at the level of glottic and supraglottic
structures [9].
In this
scenario, the regular practice of physical exercises contributes to the control
of neurodegenerative disorders related to PD [10]. In addition to improving
motor functions [11], exercises help to improve ventilatory capacity and
cardiorespiratory rate in individuals with PD [12]. Physical exercise can cause
cortical activation patterns like those achieved with the use of
pharmacological resources in these patients, which suggests that it is
extremely important for the symptomatic relief of motor impairments of the
disease [13]. Although the evidence points to the importance of physical
exercise in controlling PD, the findings that reveal the role of dual-task
exercises on vestibular and respiratory changes are still inconclusive. In this
context, the aim of the present study was to verify the quality of life and the
effects of dual-task physical exercise on postural instability and respiratory
parameters, in patients with PD.
Methods
Participants and ethical procedures
The recruitment
of participants was conducted through dissemination by local media. Those
eligible were those who had a clinical diagnosis of PD confirmed by a medical
report for at least 1 year, residing in the city of Criciúma
/ SC and region and registered in the UNESC's Pharmacy School program. All
subjects met the following inclusion criteria: Preserved level of
consciousness, be between stages 1 and 4 on the Hoenh
and Yahr scale and use the same class of drugs for
the treatment of Parkinson's disease. Exclusion criteria were subjects who
underwent some type of supplementation, who had physical limitations that
compromised the performance of activities and / or other associated
degenerative diseases and violated the inclusion criteria. The present proposal
was inserted in the Platform Brazil and approved by the institution's ethics
committee (CEP) under protocol No. 1,425,772. A total of 22 male subjects were
interested in participating in the study, but only 15 met the inclusion
criteria and 14 completed the intervention period, as shown in the flowchart
below (Figure 1).
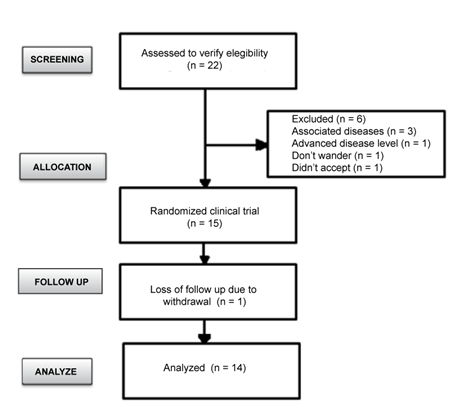
Figure 1 - Flowchart referring to the
recruitment and selection of the sample
Initial data
were obtained through prior assessment of patients during a home visit
previously carried out before the intervention protocol. These sample
characterization data are described in table I.
Table I - Characterization of the sample
(n = 14)
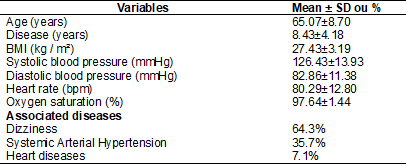
Data
presented as mean and standard deviation or percentage. Body mass index (BMI)
mm of mercury (mmHg), beats per minute (bpm), percentage (%)
Intervention
The study was
conducted for a period of 60 days, in the months of October, November and
December, with training frequency of 3 times a week and duration of 45 minutes
as recommended by the European Physiotherapy Guideline for Parkinson's disease.
The training protocol consisted of warm-up exercises, strength exercises and proprioceptives. Vestibular rehabilitation exercises were
based on the protocols of Cawthorne & Cooksey, by
Herdman (2007). Breathing exercises [12] were
performed in association with the other exercises.
Functional assessments
The evaluations
were performed before and 48 hours after the physical training program.
Parkinson's disease stage and severity were evaluated using the modified Hoehn
and Yahr Staging Scale, patients' quality of life
through the Parkinson's Disease Questionnaire-39 (PDQ-39), the elderly's
functional fitness by battery of Senior Fitness Test tests proposed by Rikli and Jones [14], evaluation of static balance through
the sensitized Romberg test with open eyes and proprioceptive loss through the
Fukuda steps test [8] and lung function by spirometry from a forced breathing
maneuver using the spiro USB spirometer (Carefusion,
USA).
Statistical analysis
Initially the
data were analyzed by GraphPad, considering an alpha = 0.05. Subsequently, the
Kolmogorov-Smirnov test was used to verify the normality of the data obtained.
The data were analyzed by the Wilcoxon test considering a statistical
difference when the p was < 0.05. All data were expressed as mean ± standard
deviation and percentage.
Results
Quality of life
As seen in Table
II, quality of life indicators such as daily life activity, emotional
well-being, stigma, cognition, communication, and body discomfort showed a
statistically significant difference when compared to data prior to the
intervention program.
Table II - Quality of life indicators of
patients with Parkinson's disease submitted to a dual task physical exercise
program
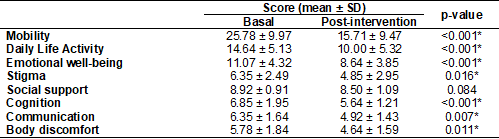
The
data are presented as mean and standard deviation considering the maximum score
obtained in the questions of the Parkinson’s Disease Questionnaire; *Values
obtained after application of Student's t tests for paired samples and
Wilcoxon's T tests (n = 14)
Staging of
PD: There were no statistical differences in the stages of development of PD,
however, it is worth mentioning that some individuals showed changes after the
intervention program that can have positive effects on PD control, as shown in
Figure 2.
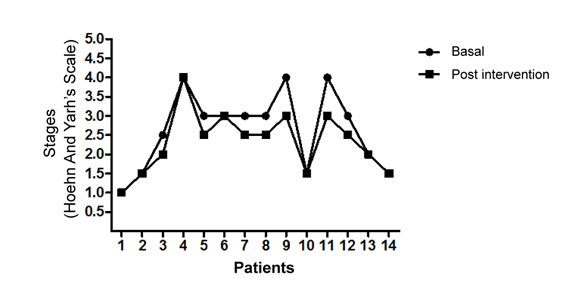
Baseline
values compared to post-intervention values
Figure 2 - Developmental stages of PD
according to the Hoehn and Yahr Staging Scale
Respiratory parameters
Table III shows,
in average terms, that patients showed changes in functional breathing
indicators after the intervention program. Although these values are not
statistically different, they may represent an important change in the
patients' breathing pattern.
Table III - Pulmonary function data of
patients with Parkinson's disease submitted to a dual task physical training
program
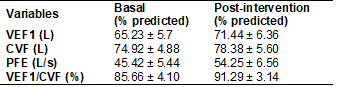
Values
are expressed as mean and standard deviation based on the predicted value of
each patient (n = 10); The values of Forced expiratory volume in the first
second (FEV1), Forced vital capacity (FVC), Peak expiratory flow (PEF) and the
FEV1 / FVC ratio
Physical aptitude
As noted in
table IV, patients showed important differences after the intervention program.
Only the test of sitting and reaching the feet did not show a statistically significant
result. The other variables such as sitting and getting up from the chair,
forearm flexion, walking 2.44 meters, reaching the back, and walking 6 minutes
showed significant changes before and after the exercise program.
Table IV - Physical fitness data of
patients with Parkinson's disease submitted to a dual task physical training
program
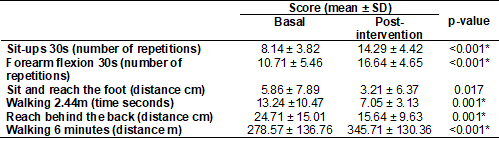
Data
are presented as mean and standard deviation considering the maximum score
obtained in the questions of the Senior Fitness Test; *Values obtained after
application of Student's t tests for paired samples and Wilcoxon's T tests (n =
14)
Vestibular system
The variables
for assessing the vestibular system were described in Table V. The presence of
nystagmus was observed in 71.4% of the sample population. The Romberg test
which assesses body balance with eyes open, showed a statistically significant
difference, showing that in the initial evaluation only 35.7% were able to
perform the test and in the final evaluation, after the intervention, 78.6%
were able to perform it. The Fukuda test also showed significant results both
in the angle and in the displaced meters before, and after the intervention.
Table V - Vestibular system parameters
data of patients with Parkinson's disease submitted to a dual task physical
training program
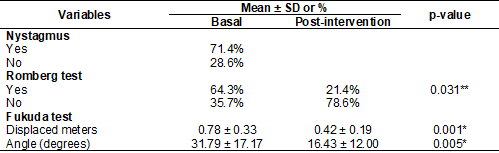
Data
are presented as mean and standard deviation or percentage considering the
maximum score obtained in the different tests; *Values obtained after
application of Student's t tests for paired samples and Wilcoxon test (n = 14)
Discussion
Behavioral
changes, such as the adoption of a more active lifestyle or participation in
physical training programs for specific purposes, have been pointed out in
several studies as a fundamental condition for maintaining health or reducing
the risks associated with several chronic-degenerative diseases. In this sense,
PD consists
of a neurological, chronic, and progressive disease affects body movements and
is highly susceptible to the effects of exercise. Experimental studies in
animal models of our group [3,4] or studies in humans [10,15] have revealed
that regular physical exercise promotes quantitative and qualitative benefits
to neurological functions. Despite these advances and scientific reports, the
data obtained are still inconclusive since physical exercise is constituted by
different forms and characteristics in its execution such as specificity,
frequency, intensity, duration and type or model.
Dual-function or
dual-task exercises involve performing a main activity, which is the focus of
attention, and a secondary activity performed at the same time [16]. In this context,
the motor and cognitive systems work with each other to guarantee more
pronounced effects resulting from exercise. This exercise model, respecting
specificity, intensity, frequency, and duration criteria, can be a relevant
strategy that contributes to improving the behavioral, functional, and
biochemical parameters of patients with PD. Thus, our study aimed to verify the
potential effect of a dual-task physical exercise program on postural
instability and respiratory parameters in patients with PD.
The quality of
life of patients with PD consists of at least three major domains: physical,
mental, and social [17]. Several instruments have been proposed to identify the
role of a given intervention on a patient's quality of life. In this scenario, the
Parkinson’s Disease Questionnaire - 39 (PDQ-39) has been indicated as the most
appropriate instrument for assessing the quality of life of patients with PD
[18]. Our results revealed that mobility and activity of daily living were the
two domains that showed higher levels of commitment by patients, especially
about tasks of motor origin, involving situations such as walking, performing
leisure activities, bathing. This result is consistent with previous studies
emphasizing that disorders related to the development of motor activities are
detected as factors that negatively alter the perception of quality of life
[17,19,20].
After the
intervention period with physical exercise, a significant improvement was
observed in almost all the domains investigated, except for social support.
This is in agreement with Deane et al. [21], in which they demonstrate
the practice of physical exercises in the rehabilitation of individuals with
PD, reducing the debilitating effects of sensorimotor impairment in order to improve
participation in social activities and consequent improvement in quality of
life.
The etiology of
PD is complex and, therefore, the disease progression stages depend on
psychosocial and biological factors that can contain or delay the harmful and
degenerative effects during life. The results of the Hoehn and Yahr Staging Scale (modified) show that the patients had
scores from 1 to 4 on that scale, however the descriptive analysis reveals that
some patients improved the disease stage after the intervention program.
Studies show that there is an association between the severity of the disease
and the upper and lower body strength. These effects are possibly associated
with the improvement in the indicators of functional capacity or physical fitness
promoted by the training program. In this sense, Wade and Tarsy
et al. [22,23] suggest that several types of physical training are
probably effective in improving the functional outcome for patients with PD,
showing the effectiveness of the intervention given the functionality and stage
of the disease of the investigated patients.
One of the
factors apparently secondary to PD are changes in respiratory function, which
potentiates the degenerative effects of the disease and worsens the patient's
health status. This disorder probably remains unnoticed while the disease
develops, because physical disability in PD generally leads the patient to lead
a sedentary life, consequently limiting him from activities where breathing
problems can become evident [24]. The results observed in the present study
reveal that patients have spirometric characteristics
compatible with restrictive ventilatory disorder. An increase of 9.52% in the
values of forced expiratory volume in the first second (FEV1) and 19.44% in the
peak expiratory flow (PEF) were observed. Although there is no statistical
difference on these data, this difference can represent an important clinical
improvement for these patients. The increase in such parameters in patients
with restrictive functional characteristics may impact the increase in chest
expansion and reduce the deficit in lung volume, compatible with the
restriction pattern [24]. In this sense, although the respiratory function does
not undergo significant changes, it does not exclude the importance of
dual-task exercise for the clinical condition of patients with PD.
The assessment
of functional capacity in PD has been increasingly reported in the literature,
highlighting a sensitive measure that could be used as a possible predictor for
the evolution of the disease. In this context, Gustafsson et al. [25]
demonstrate the importance of motor assessment through batteries of tests in
normal individuals. The authors observed, from a prospective study involving
1,317,713 men, deficits in isometric strength of the upper limbs, three decades
before the first symptoms of PD manifestations. In the present study, we used
the Senior Fitness Test battery, which, according to Rikli
and Jones [14], measures the physical fitness of the elderly to perform
activities of daily living in old age and is composed of six motor tests that
assess the strength of the upper limbs and lower limbs, flexibility of upper
and lower limbs, agility / dynamic balance and aerobic endurance. The results
observed in the present study show important differences after the intervention
program. In particular, the variables of sitting and getting up from the chair,
forearm flexion, walking 2.44 meters, reaching the back, and walking 6 minutes,
showed significant changes after the exercise program. These results are in
line with previous studies in which they demonstrated that an intervention
through exercises can improve strength, measures of static postural stability
and motor symptoms in people with PD [11,26,27].
According to Christofoletti [28], among the several benefits promoted by
physical training, the increase in tone and strength of the muscles involved in
walking and balance promote improvements in the mobility of patients with PD.
The data from the present study corroborate these findings. In addition to
observing the significant improvement in the strength of the lower and upper
limbs, the training program promoted the biomechanical alignment of the
posture, the reduction of the time of execution of the motor tasks and the
improvement of the gait speed [22,25].
According to Colnat-Coulbois et al. [29], parkinsonian patients
have an inadequate interaction of the systems responsible for body balance,
vestibular, visual and proprioceptive systems due to changes in low dopamine
levels that, when leading to inefficient movement control, affect the
processing of vestibular, visual and proprioceptives
responsible for maintaining body balance [22,26]. The results of this study
show that 71.4% of the patients had nystagmus and were completely reversed
after the exercise program. In addition to these findings, the patients' body
balance was also significantly improved with regular physical exercise. The
possible effects of exercise on these postural parameters are possibly
associated with the dual task used in the exercise protocol. According to Azadian et al. [15], when the training has dual task
exercises, positive effects are observed in space-time parameters, such as
walking speed, stride size, oscillatory dynamic balance, and symmetry of the
lower limbs. Zeigelboim et al. [30]
demonstrate that vestibular rehabilitation can induce or even cancel the signs
and symptoms triggered by PD.
Conclusion
The results
observed in the present study reveal that patients with Parkinson's disease
have spirometric characteristics compatible with
restrictive ventilatory disturbance but have shown changes in functional
breathing indicators after the intervention program. Although there is no
statistical difference on these data, this difference can represent an
important clinical improvement for these patients. Taken together, the results
obtained suggest that the effects of dual-task physical exercise have positive
effects on behavioral and functional aspects involved in the quality of life of
patients with Parkinson's disease, as well as contributing to the regulation of
the vestibular system.
Acknowledgements
We are grateful to all patients with Parkinson's
disease who participated in this study. We would also like to thank the
Physiotherapy Course of the Universidade do Extremo Sul Catarinense for
assigning the physical space to carry out the activities.
Potencial
conflict of interest
No conflicts of interest with potential for this
article have been reported.
Financing
This study was partially supported by the National
Council for Scientific and Technological Development (CNPQ).
Academic link
This study is linked to the Graduate program in Health
Sciences – PPGCS, from the Universidade do Extremo Sul Catarinense.
Authors’ contribution
Conception and design of the research: Hérica S. Fernandes, Talita Tuon
Ricardo A. Pinho; Data collection: Hérica S. Fernandes, Talita Tuon,
Miguel Rosado, Paulo Roberto Lino; Analysis and interpretation of data: Hérica S. Fernandes, Talita Tuon,
Ricardo A. Pinho; Writing of the manuscript: Hérica S. Fernandes, Talita Tuon,
Ricardo A. Pinho; Critical review of the
manuscript for important intellectual content: Talita Tuon.
References
- Emborg ME.
Evaluation of animal models of Parkinson's disease for neuroprotective
strategies. J Neurosci Methods
2004;139(2):121-43. doi: 10.1016/j.jneumeth.2004.08.004 [Crossref]
- Protter D, Lang C, Cooper AA. Α-Synuclein and mitochondrial dysfunction: a pathogenic partnership in Parkinson’s disease? Parkinson's Disease 2012;1-12. doi: 10.1155/2012/829207 [Crossref]
- Tuon T, Souza OS, Santos MF, Pereira FT, Pedroso GS, Luciano TF et al. Physical training regulates mitochondrial parameters and neuroinflammatory mechanisms in an experimental model of Parkinson’s disease. Oxidative Medicine and Cellular Longevity 2015;1-10. doi: 10.1155/2015/261809 [Crossref]
- Tuon T, Valvassori SS, Lopes-Borges J, Luciano T, Trom CB, Silva LA et al. Physical training exerts neuroprotective effects in the regulation of neurochemical factors in an animal model of Parkinson’s disease. Neuroscience 2012;227:305-12. doi: 10.1016/j.neuroscience.2012.09.063 [Crossref]
- Ni M, Signorile JF, Mooney K, Balachandran A, Potiaumpai M. Comparative effect of power training and high-speed yoga on motor function in older patients with Parkinson disease. Arch Phys Med Rehabil 2016;97(3):345-54. doi: 10.1016/j.apmr.2015.10.095 [Crossref]
- Ramos
ML, Neves DR, Lima VP, Orsini M, Machado D, Bastos
VH, Santos AP. Análise de parâmetros pneumofuncionais
em pacientes com doença de Parkinson: estudo piloto. Rev Bras Neurol
2014;50(2):38-43
- Suarez H, Dario G, Ferreira ED, Nogueira S, Arocena S, San Roman C, Suarez A. Balance in Parkinson's disease patients changing the visual input. Braz J Otorhinolaryngol 2011;77(5):651-5. doi: 10.1590/S1808-86942011000500019 [Crossref]
- Sallem AF,
Sapienza CM, Okun MS. Respiratory muscle strength training: treatment and
response duration in a patient with early idiopathic Parkinson´s disease. Neuro Rehabilitation
2005;20:323-33
- Ferreira FV, Cielo CA, Trevisan ME. Aspectos respiratórios, posturais e vocais da doença de Parkinson: considerações teóricas. Rev CEFAC 2011;13(3):534-40. doi: 10.1590/S1516-18462010005000135 [Crossref]
- Zigmond M, Cameron JL, Hoffer BJ, Smeyne RJ. Neurorestoration by physical exercise: moving forward. Parkinsonism Relat Disord 2012;18(Suppl1):147-50. doi: 10.1016/S1353-8020(11)70046-3 [Crossref]
- Kurtais Y, Kutlay S, Tur BS, Gok H, Akbostanci C. Does treadmill training improve lower-extremity tasks in Parkinson disease? A randomized controlled trial. Clin J Sport Med 2018;18(3):289-91. doi: 10.1097/JSM.0b013e318170626d [Crossref]
- Pelosin E, Faelli E, Lofrano F, Avanzino L, Marinelli L, Bove M, Ruggeri P, Abbruzzese G. Effects of treadmill training on walking economy in Parkinson's disease: a pilot study. Neurol Sci 2009;30(6):499-504. doi: 10.1007/s10072-009-0141-8 [Crossref]
- Alberts JL, Phillips M, Lowe MJ, Frankemolle A, Thota A, Beall EB et al. Cortical and motor responses to acute forced exercise in Parkinson's disease. Parkinsonism Relat Disord 2016;24:56-62. doi: 10.1016/j.parkreldis.2016.01.015 [Crossref]
- Rikli Re, Jones CJ. Functional fitness normative scores for community-residing older adults, ages 60-94. J Aging Phys Act 1999;7:162-81. doi: 10.1123/japa.7.2.162 [Crossref]
- Azadian E, Torbati HR, Kakhki AR, Farahpour N, Azadian E. The effect of dual task and executive training on pattern of gait in older adults with balance impairment: A Randomized controlled trial. Arch Gerontol Geriatr 2016;62:83-9. doi: 10.1016/j.archger.2015.10.001 [Crossref]
- Christofoletti G, Andrade LP, Beinotti F, Borges G. Cognition and dual-task performance in older adults with Parkinson's and Alzheimer's disease. Int J Gen Med 2014;7:383-8. doi: 10.2147/IJGM.S65803 [Crossref]
- Assumpção FB, Kuczynski E, Sporovieri MH, Aranha EMG. Escalas de avaliação de qualidade de vida. Arq Neuropsiquiatr 2000;58:119-27. doi: 10.1590/S0004-282X2000000100018 [Crossref]
- Marinus J, Ramaker C, Van Hilten JJ, Stiggelbout AM. Health related quality of life in Parkinson's disease: a systematic review of disease specific instruments. J Neurol Neurosurg Psychiatry 2002;72(2):241-8. doi: 10.1136/jnnp.72.2.241 [Crossref]
- Hoehn MM, Yahr MD.
Parkinsonism: onset, progression and mortality. Neurology 1967;17(5):427-42.
- Lana RC, Álvares LMRS, Nasciutti-Prudente C, Goulart FRP, Teixeira-Salmela LF, Cardoso FE. Percepção da qualidade de vida de indivíduos com doença de Parkinson através do PDQ-39. Rev Bras Fisioter 2007;11(5):397-402. doi: 10.1590/S1413-35552007000500011 [Crossref]
- Deane KH, Jones D, Playfor DED, Ben-Shlomo Y, Clarke CE. Physiotherapy for patients with Parkinson's Disease: a comparison of techniques. Cochrane Database Syst Rev 2001;3.CD002817. doi: 10.1002/14651858 [Crossref]
- Wade DT, Gage H, Owen C, Trend P, Grossmith C, Kaye J. Multidisciplinary rehabilitation for people with Parkinson's disease: a randomised controlled study. J Neurol Neurosurg Psychiatry 2003;74(2):158-62. doi: 10.1136/jnnp.74.2.158 [Crossref]
- Tarsy D, Hurtig HI, Dashe JF.
Nonpharmacologic management of Parkinson disease. Uptodate:
last literature review 2008;1-5.
- Torsney KM, Forsyth D. Respiratory dysfunction in Parkinson's disease. J R Coll Physicians Edinb 2017;47(1):35-39. doi: 10.4997/JRCPE.2017.108 [Crossref]
- Gustafsson H, Strahle JAS, Nordstrom A, Nordstrom P. Low muscle strength in late adolescence and Parkinson disease later in life. Neurology 2015;84(18):1862-9. doi: 10.1212/WNL.0000000000001534 [Crossref]
- Jöbges EM, Spittler-Schneiders H, Renner CI, Hummelsheim H. Clinical relevance of rehabilitation programs for patients with idiopathic Parkinson syndrome. II: Symptom-specific therapeutic approaches. Parkinsonism Relat Disord 2007;13(4):203-13. doi: 10.1016/j.parkreldis.2006.07.018 [Crossref]
- Goodwin VA, Richards SH, Taylor RS, Taylor AH, Campbell JL. The effectiveness of exercise interventions for people with Parkinson's disease: a systematic review and meta-analysis. Mov Disord 2008;23(5):631-40. doi: 10.1002/mds.21922 [Crossref]
- Christofoletti G, Freitas RT, Cândido ER, Cardoso CS. Eficácia de tratamento fisioterapêutico no equilíbrio estático e dinâmico de pacientes com doença de Parkinson. Fisioter Pesqui 2010;17(3):259-63. doi: 10.1590/S1809-29502010000300013Colnat [Crossref]
- Colnat-Coulbois S, Gauchard GC, Maillard L, Barroche G, Vespignani H, Auque J, Perrin PHP. Bilateral subthalamic nucleus stimulation improves balance control in Parkinson’s disease. J Neurol Neurosurg Psychiatry 2015;76:780-7. doi: 10.1136/jnnp.2004.047829 [Crossref]
- Zeigelboim BS, Klagenberg KF, Teive HA, Munhoz RP, Martins-Bassetto
J. Vestibular rehabilitation: clinical benefits to patients with
Parkinson's disease. Arq
Neuro-Psiquiatr 2009;67(2):219-23. doi: 10.1590/S0004-282X2009000200009 [Crossref]