Rev Bras Fisiol Exerc 2022;21(3):184-94
doi: 10.33233/rbfex.v21i3.4734
REVIEW
Effects of pre-operative inspiratory muscular training in patients
subject to cardiac surgery: a systematic review
Efeitos do treinamento
muscular inspiratório pré-operatório em pacientes submetidos à cirurgia
cardíaca: uma revisão sistemática
Ana Cristina da Costa
Oliveira1, Aísa de Santana Lima1,
Vinicius Afonso Gomes2, Séres Costa de
Souza Nascimento1, Cássio Magalhães da Silva e Silva1
1Universidade Social da Bahia, Salvador,
BA, Brazil
2Escola Bahiana
de Medicina, Salvador, BA, Brazil
Received: April 15, 2021; Accepted:
September 15, 2022.
Correspondência: Ana Cristina da Costa Oliveira,
Programa de Pós-Graduação em Fisioterapia Hospitalar, Universidade Social da
Bahia, Av. Oceânica, 2717, 40170-010 Salvador BA
Ana Cristina
da Costa Oliveira: fisiocris.16@gmail.com
Aísa de Santana Lima:
aisafisio18@gmail.com
Vinicius
Afonso Gomes: vinifisioterapia@yahoo.com.br
Séres Costa de Souza
Nascimento: seres.souza@gmail.com
Cássio
Magalhães da Silva e Silva: cassiofisio2@yahoo.com.br
Abstract
Introduction: The diseases that affect the cardiovascular system
often lead the patient to undergo cardiac surgery in
search of better survival. This surgical procedure is associated with a high
incidence of postoperative complications related to respiratory function.
Preoperative inspiratory muscle training (IMT) can benefit patients who will
undergo cardiac surgery. Objective: Systematic review of randomized
clinical trials, informing the effects of preoperative inspiratory muscle
training in patients undergoing cardiac surgery. Methods: The search for
randomized clinical trials was carried out by two authors, including the
Medline, PubMed, PEDro and Scielo
databases. The methodological quality of the articles was assessed using the PEDro scale and the risk of bias was scored using the
Review Manager version 5.4 software from the Cochrane Collaboration. Results:
Initially, a total of 85 articles were identified in the databases. Five
articles were included for data extraction. The main outcomes of this
systematic review are: maximum inspiratory pressure (PImax);
forced expiratory volume in the first second (FEV1); forced vital capacity;
pneumonia, duration of postoperative hospitalization and postoperative
pulmonary complication. Conclusion: The IMT performed in the
preoperative period adds benefits that include prevention of postoperative
pulmonary complications, increasing the PImax
and FEV1, reducing the occurrence of pneumonia and reducing the length of
postoperative hospital stay.
Keywords: respiratory training; chest surgery; cardiac
surgery.
Resumo
Introdução: As doenças que acometem o sistema
cardiovascular levam frequentemente o paciente a realizar cirurgias cardíacas
em busca de uma melhor sobrevida. Esse procedimento cirúrgico está associado a
uma grande ocorrência de complicações pós-operatórias relacionadas com a função
respiratória. A realização do treinamento muscular inspiratório (TMI)
pré-operatório pode beneficiar pacientes que serão submetidos a cirurgias
cardíacas. Objetivo: Revisão sistemática de ensaios clínicos
randomizados, informando os efeitos do TMI pré-operatório em pacientes
submetidos a cirurgia cardíaca. Métodos: A busca dos ensaios clínicos
randomizados foi feita por dois autores, incluindo as bases de dados Medline, PubMed, Pedro e Scielo. A
qualidade metodológica dos artigos foi avaliada utilizando a escala PEDro e o risco de viés foi pontuado pelo software Review
Manager version 5.4 da Cochrane Collaboration.
Resultados: Inicialmente foi identificado um total de 85 artigos nas
bases de dados. Cinco artigos foram incluídos para extração de dados. Os
desfechos principais desta revisão sistemática são: Pressão inspiratória máxima
(PImáx); Volume expiratório forçado no primeiro
segundo (VEF1); Capacidade vital forçada CVF; Pneumonia, duração da internação
pós-operatória e complicação pulmonar pós-operatória. Conclusão: O TMI
realizado no período pré-operatório para pacientes submetidos a cirurgia
cardíaca agrega benefícios que incluem prevenção das complicações pulmonares
pós-operatórias, aumentando a PImax e o
VEF1, reduzindo a ocorrência de pneumonia e diminuindo o tempo de internação
pós-operatória.
Palavras-chave: treinamento respiratório; cirurgia
torácica; cirurgia cardíaca.
Introduction
The conditions that affect the cardiovascular system,
more precisely in the valvular region of the heart and in the coronary
arteries, can lead the individual to need cardiac surgery [1]. Worldwide, more
than 23 million people are affected by this complex syndrome [2]. In 2015,
Brazil recorded 91,738 deaths from cardiac complications, an average of 7,645
deaths per month [3].
The cardiac surgical procedure, when combined with
factors such as obesity, sedentary lifestyle, smoking, diabetes and pre-existing
lung diseases, predisposes to the occurrence of postoperative complications
[4]. Thus, in addition to a threat to patient survival, there is a risk of
increased length of stay and hospital costs [5]. According to data from the
Brazilian Society of Cardiovascular Surgery, Brazil is the second country in
the world in number of heart surgeries performed annually, totaling about
102,000 surgeries/year [6].
In this scenario, the performance of the inspiratory
muscles is commonly compromised (approximately 50%), reducing lung volumes and
capacities, compromising lung compliance, impairing gas exchange and coughing
effectiveness [4]. Such changes can also trigger pneumonia and atelectasis [7].
Inspiratory muscle training (IMT) appears, then, as a
type of physical exercise for these patients, including indication already in
the preoperative period [8]. By conditioning the inspiratory muscles
preventively, the consequences of the postoperative period tend to be
mitigated, with an expectation of improvement in lung function and consequent
optimization of clinical outcomes [7].
Given the relevance of the subject, the objective of
this study was to perform a systematic review of randomized clinical trials on
the effects of preoperative IMT in patients undergoing cardiac surgery.
Methods
This is a systematic review of the literature, which
included and analyzed original studies, such as a randomized clinical trial, on
the effects of preoperative respiratory muscle training in cardiac surgeries.
The systematic review was planned and conducted in accordance with the
recommendations of the Cochrane Collaboration and reported in accordance with
the guidelines of the Preferred Reporting Items for Systematic Reviews e
Meta-Analyses (PRISMA) [9].
Sources of information and research strategies
The studies were identified by the researchers,
searching the following databases: Public Medline (PubMed), National Library of
Medicine (Medline), Physiotherapy Evidence Database (PEDro)
and Scientific Eletronic Library Online (SciELO) from July 2019 to February 2020 publications in
Portuguese or English. For the research, the following combinations were used
“AND” and “OR” of the following descriptors and their respective counterparts
in English: Inspiratory training, Thoracic surgery associated with Cardiac
surgery and Clinical Trial. Registration number PROSPERO: CRD42020205437. Chart
1 presents the manual search strategies.
Chart 1 - Search strategy in the PubMed database
("inhalation"[MeSH Terms] OR
"inhalation"[All Fields] OR "inspiratory"[All Fields]) AND
("muscles"[MeSH Terms] OR
"muscles"[All Fields] OR "muscle"[All Fields]) AND
("education"[Subheading] OR "education"[All Fields] OR
"training"[All Fields] OR "education"[MeSH
Terms] OR "training"[All Fields]) AND ("thoracic surgical
procedures"[MeSH Terms] OR
("thoracic"[All Fields] AND "surgical"[All Fields] AND
"procedures"[All Fields]) OR "thoracic surgical
procedures"[All Fields] OR ("thoracic"[All Fields] AND
"surgery"[All Fields]) OR "thoracic surgery"[All Fields] OR
"thoracic surgery"[MeSH Terms] OR
("thoracic"[All Fields] AND "surgery"[All Fields])).
(("inhalation"[MeSH Terms] OR
"inhalation"[All Fields] OR "inspiratory"[All Fields]) AND
("muscles"[MeSH Terms] OR
"muscles"[All Fields] OR "muscle"[All Fields]) AND
("education"[Subheading] OR "education"[All Fields] OR
"training"[All Fields] OR "education"[MeSH
Terms] OR "training"[All Fields]) AND ("thoracic surgical
procedures"[MeSH Terms] OR
("thoracic"[All Fields] AND "surgical"[All Fields] AND
"procedures"[All Fields]) OR "thoracic surgical
procedures"[All Fields] OR ("thoracic"[All Fields] AND
"surgery"[All Fields]) OR "thoracic surgery"[All Fields] OR
"thoracic surgery"[MeSH Terms] OR
("thoracic"[All Fields] AND "surgery"[All Fields]))) AND
Clinical Trial[ptyp](("breathing
exercises"[MeSH Terms] OR
("breathing"[All Fields] AND "exercises"[All Fields]) OR
"breathing exercises"[All Fields] OR ("respiratory"[All
Fields] AND "muscle"[All Fields] AND "training"[All
Fields]) OR "respiratory muscle training"[All Fields]) AND
("thoracic surgical procedures"[MeSH Terms]
OR ("thoracic"[All Fields] AND "surgical"[All Fields] AND
"procedures"[All Fields]) OR "thoracic surgical
procedures"[All Fields] OR ("thoracic"[All Fields] AND "surgery"[All
Fields]) OR "thoracic surgery"[All Fields] OR "thoracic
surgery"[MeSH Terms] OR
("thoracic"[All Fields] AND "surgery"[All Fields])))
((("breathing exercises"[MeSH Terms] OR
("breathing"[All Fields] AND "exercises"[All Fields]) OR
"breathing exercises"[All Fields] OR ("respiratory"[All
Fields] AND "muscle"[All Fields] AND "training"[All
Fields]) OR "respiratory muscle training"[All Fields]) AND
("thoracic surgical procedures"[MeSH Terms]
OR ("thoracic"[All Fields] AND "surgical"[All Fields] AND
"procedures"[All Fields]) OR "thoracic surgical
procedures"[All Fields] OR ("thoracic"[All Fields] AND
"surgery"[All Fields]) OR "thoracic surgery"[All Fields] OR
"thoracic surgery"[MeSH Terms] OR
("thoracic"[All Fields] AND "surgery"[All Fields]))) AND
Clinical Trial[ptyp]
Study selection
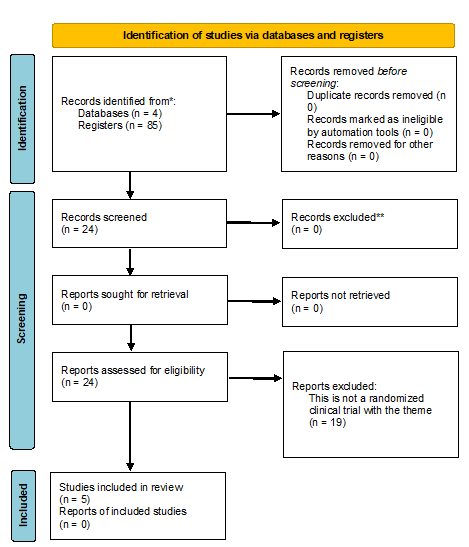
Figure 1 - Search and selection of studies for inclusion in
the systematic review according to the PRISMA methodology - 2020
Study eligibility assessment
The titles and abstracts of each data source were
evaluated by the researchers, and the studies eligible for the systematic
review were defined. If at least one of the researchers considered an eligible
reference, the full text was obtained for full reading. The full texts of the
selected articles were independently evaluated by the researchers to identify
those that met the inclusion or exclusion criteria. The references of each
selected article were analyzed to identify other potentially qualified studies.
After reading and inclusion, the works were evaluated for the construction of
the systematic review.
Methodological quality
The quality of the included articles was assessed
using the PEDro scale. This evaluates the tests
through 11 pre-established items PEDro [10]. The PEDro score was not used as an inclusion or exclusion
criterion for the articles, but as an indicator of scientific evidence of the
studies [8,11].
Risk of bias in primary studies
The risk of bias in the studies included in this
systematic review was scored using the Review Manager version 5.4 software
(REVMAN - Cochrane Collaboration), which is domain-based, with critical
assessment done separately for different aspects of the risk of bias of the
study type in question [12].
Results
Description of selected studies
Initially, a total of 85 articles were identified in
the selected databases (PubMed), (Medline), (PEDro) e
(SciELO), reducing to 24 articles, when the “clinical
trial” filter was applied, which analyzed the full text. Six articles met the
eligibility criteria and were included for data extraction, 1 of which was
excluded due to difficult access. The other 17 clinical trials were excluded
due to inadequacy, after reading the titles and abstracts.
Methodological quality of studies
Table I - Methodological quality of studies by the Scale PEDro [10]
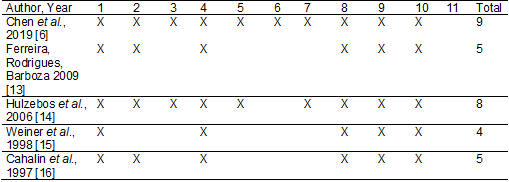
1) specification of inclusion criteria (item not
scored); 2) random allocation; 3) allocation secrecy; 4) similarity of groups
in the initial or baseline phase; 5) masking of subjects; 6) therapist masking;
7) evaluator masking; 8) measurement of at least one primary outcome in 85% of
allocated subjects; 9) intention-to-treat analysis; 10) comparison between
groups of at least one primary outcome and 11) reporting of measures of
variability and estimation of parameters of at least one primary variable
Table II - General characteristics of the included studies
in the Systematic Review
Detailing the risk of bias
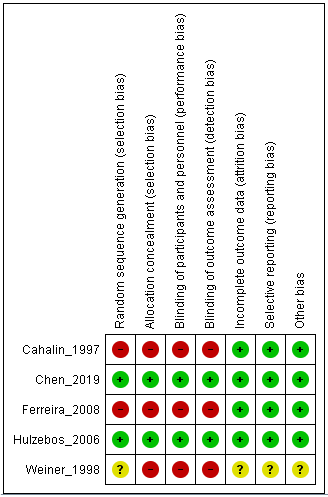
Figure 2 - Summary of the risk of bias established by the
Cochrane Collaboration
The articles included were published between 1997 and
2019. Their sample size ranged from 14 to 279 adult subjects, randomized to the
IMT group or the control group. The prescribing charge of MIP ranged from 15 to
60%. Five studies used 30% of the MIP in the IMT group, Chen et al. [6];
Ferreira et al. [13]; 2 published articles by Hulzebos
[14,17]; one study ranged from 15 to 60% [15] and another used with 20% [16].
Regarding the control group, one study used 9% of the minimum device load [6].
A physical therapist guided deep breathing exercises without special equipment
and daily walks to the limit [13], another study used instructions on deep
breathing, coughing and nasal mobilization maneuvers [14]. In the following
study, measurements were performed without the use of resistance [15], one of
the studies had no control group [16].
The intervention period varied between 2 daily series,
for 20 minutes; 3 daily sets of 10 minutes; 1 daily series of 20 minutes, 15
minutes, three times a day and 1 series of 30 minutes daily. The training
protocols were daily and lasted between 5 days and 8 weeks. Table I presents
the characterization of the sample, methodology, main variables, results and
score on the PEDro scale [10].
Based on the results found in the studies, they were
divided into 5 large groups of outcomes: MIP; FEV1; FVC; Pneumonia, duration of
postoperative hospital stay and postoperative
pulmonary complication.
Discussion
The aim of the present study was to analyze the
effects of preoperative IMT in patients undergoing cardiac surgery. It was
possible to observe an increase in MIP, VEF1 and FVC [13,16], reduction in
length of stay, in addition to a decrease in the incidence of pneumonia and
other postoperative pulmonary complications in the evaluated studies [6,14,15].
Of all the variables, MIP seems to be a central
pillar, which also affects the others. Far from being an isolated marker of
strength, it has shown considerable relevance, as seen in the study by Bessa et al. [4], where an inverse association
between inspiratory muscle strength and mortality was demonstrated. It is
necessary to understand how this factor can be so important, not only in the
survival of patients, but also in the ability to perform activities of daily
living [18], as inspiratory muscle fatigue may partially explain exercise
intolerance [4].
A systematic review with meta-analysis in patients
with heart failure performed by Sadek et al.
[19] used some of the exercise principles and categorized the IMT in 4 ways:
high intensity and moderate duration (60% MIP charge lasting 10 weeks and
frequency of 3 times a week); high intensity and high duration (60% MIP load
lasting 12 weeks and frequency of 6 times a week); low intensity and low
duration (30-40% MIP load lasting 6-8 weeks and frequency of 7 times a week)
and low intensity and high duration (30% MIP load lasting 12 weeks and
frequency of 7 times a week) [19].
Still on the study of Sadek et
al. [19], it was possible to verify that the high intensity and high
duration training were the most effective in increasing the MIP. By way of
comparison, none of the studies in our review used a load > 50% of MIP for
prescription, showing that there would still be a possibility for even better
results in relation to MIP. It is necessary to point out that the simple
maintenance of the MIP is already considered beneficial in the postoperative
period of cardiac surgery (where it is usual to fall), which in a way justifies
the use of lower workloads and the achievement of positive results even without
increasing inspiratory muscle strength.
In addition to MIP, other factors can be optimized by
IMT and among them we can highlight the improvement in lung function [20]. In
the study by Ferreira et al. [13], IMT proved to be safe, in addition to
improving FVC and maximum voluntary ventilation of patients undergoing the
surgical procedure. The improvement of these parameters occurs by optimizing
variables such as endurance, strength, power and even increasing the strength
of the expiratory muscles [7].
But how would it be possible to increase the strength
of expiratory muscles through inspiratory resistance therapy? A study done in
patients with bronchiectasis showed that IMT increased MEP, through a principle
called “last force extension”. Inspiration against resistance in IMT can
increase the activation of the expiratory system, muscles responsible for the
last force extension, which can result in a significant increase in MEP [21].
In our review, the study by Cahalin et al.
[16] was also able to increase MEP, showing that in this population it is also
possible to extrapolate the benefits of IMT to the expiratory muscles.
Although none of the studies directly assessed
coughing ability, the importance of IP and MEP for some of its phases is known.
In addition, cough malfunction compromises the elimination of pathogens,
inducing pulmonary infections, atelectasis and increased costs and length of
hospital stay [22]. According to this line of reasoning, the works by Hulzebos et al. [14] and Weiner et al. [15]
found a reduction in complications and consequently in the length of hospital
stay in patients who underwent IMT.
Some factors should be highlighted, and one of them is
that although pulmonary function has increased, interestingly, the study by
Ferreira et al. [13] did not change MIP. Studies need to be more
specific regarding the principles of physical exercise, repetitions, intensity,
load progression [23,24].
Certain goals can be achieved with prescription
adjustments varying within a range. Strength training is typically used with a
higher load and fewer repetitions, with endurance goals done in reverse
[25,26]. The outcomes evaluated in this study can benefit from both types of training,
remembering the importance of individualized prescription and even that a mixed
training can be used. It was not clear in the studies evaluated whether
reassessments were carried out between sessions and whether the training load
could be increased. The time of use of the technique was also very
heterogeneous, varying between 5 days, as in the study by Chen et al.
[6] and 8 weeks in the study by Cahalin et al.
[16].
Thus, IMT has beneficial effects on lung function and
length of hospital stay, although its prescription still needs to be
individualized. It is necessary to define more clearly the principles of
physical exercise and endurance, as well as the benefits resulting from them.
Conclusion
The results of this systematic review indicate that
IMT is beneficial in the prevention of pulmonary complications such as
pneumonia, increase in MIP, FEV1 and VC, in addition to reducing the length of
hospital stay, when performed in the preoperative period of cardiac surgery.
Despite the findings mentioned here, further research needs to be carried out,
detailing the principles of physical exercise, endurance and training
periodization.
Potential conflict of interest
No conflict of interest.
Funding source
There is no funding.
Authors' contribution
Research conception and design: Lima AS, Oliveira ACC, Silva CMS; Obtaining data: Lima AS,
Oliveira ACC; Data analysis and interpretation: Silva CMC, Souza SC,
Gomes VA; Writing of the manuscript: Lima AS, Oliveira AC; Critical
review of the manuscript for important intellectual content: Silva CMS,
Souza SC, Gomes VA
Referências
- Cordeiro ALL, Melo TA, Neves
D, Luna J, Esquivel MS, Guimarães ARF, et al. IMT and
functional capacity after cardiac surgery. Braz J
Cardiovasc Surg 2016;31(2):140-4. doi: 10.5935/1678-9741.20160035 [Crossref]
- Rohde LE, Montera MW, Bocchi EA, Clausell N, Albuquerque DC, Rassi S, et
al. Brazilian guidelines on chronic and acute heart failure. Arch Bras Cardiol [Internet]. 2018 [cited 2022 May
26];111(3):436-539. Available from:
https://observatorio.fm.usp.br/handle/OPI/29870
- Dordetto PR, Pinto GC, Rosa TCSC. Pacientes
submetidos à cirurgia cardíaca: caracterização sociodemográfica, perfil
clínico-epidemiológico e complicações. Rev Fac Ciênc Méd Sorocaba [Internet].
2016 [cited 2020 Nov 4];18(3):144-9. Available from:
https://revistas.pucsp.br/index.php/RFCMS/article/view/25868
- Bessa EJC, Lopes AJ, Rufino R. The
importance of measurement of respiratory muscle strength in pulmonology
practice. Pulmão RJ [Internet]. 2015 [cited 2022 May
26];24(1):37-41. Available from:
http://www.sopterj.com.br/wp-content/themes/_sopterj_redesign_2017/_revista/2015/n_01/10.pdf
- Laizo A, Delgado FE, Rocha GM. Complicações que aumentar o tempo de internação em UTI dos pacientes submetidos à cirurgia cardíaca. Rev Bras Cir Cardiovasc 2010;25(2):166-71. doi: 10.1590/S0102-76382010000200007 [Crossref]
- Chen X, Hou L, Zhang Y, Liu X, Shao B, Yuan B, et al. The effects of five days of intensive preoperative inspiratory muscle training on postoperative complications and outcome in patients having cardiac surgery: a randomized controlled trial. Clin Rehabil 2019;33(5):913-22. doi: 10.1177/0269215519828212 [Crossref]
- Matheus GB, Dragosavac D, Trevisan
P, Costa CE da, Lopes MM, Ribeiro GC de A. Postoperative muscle training improves
tidal volume and vital capacity in the postoperative period of CABG surgery.
Rev Bras Cir Cardiovasc [Internet]. 2012 [cited 2020 Nov 4]; 27(3):362-9.
Available from: https://pubmed.ncbi.nlm.nih.gov/23288176/
- Verhagen AP, Vet HCW, Bie RA, Kessels AGH, Boers M, Bouter LM, et al. TheDelphi list: A criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. J Clin Epidemiol 1998;51(12):1235-41. doi: 10.1016/s0895-4356(98)00131-0 [Crossref]
- Moher D, Liberati A, Tetzlaff J, Altman DG, Altman D, Antes G, et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement (Chinese edition). J Chinese Integr Med 2009;7(9):889-96. doi: 10.1371/journal.pmed.1000097 [Crossref]
- Moseley AM, Elkins MR, van der Wees PJ, Pinheiro MB. Using research to guide practice: The Physiotherapy Evidence Database (PEDro). Braz J Phys Ther 2020;24(5):384-91. doi: 10.1016/j.bjpt.2019.11.002 [Crossref]
- Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability
of the PEDro scale for rating quality of randomized
controlled trials. Phys Ther [Internet]. 2003 [cited
2022 May 22];83(8):713-21. Available from:
https://pubmed.ncbi.nlm.nih.gov/12882612/
- Carvalho APV, Silva VGA.
Avaliação do risco de viés de ensaios clínicos randomizados pela ferramenta da
colaboração Cochrane. Diagn Tratamento [Internet].
2013 [cited 2022 May 12];18(1):38-44. Available from:
http://files.bvs.br/upload/S/1413-9979/2013/v18n1/a3444.pdf
- Ferreira PEG, Rodrigues AJ, Evora PRB. Effects of an inspiratory muscle rehabilitation program in the postoperative period of cardiac surgery. Arq Bras Cardiol 2009;92(4):275-82. doi: 10.1590/s0066-782x2009000400005 [Crossref]
- Hulzebos EHJ, Helders PJM, Favié NJ, De Bie RA, Riviere AB, van Meeteren NLU. Preoperative intensive inspiratory muscle training to prevent postoperative pulmonary complications in high-risk patients undergoing CABG surgery: a randomized clinical trial. JAMA 2006;296(15):1851-7. doi: 10.1001/jama.296.15.1851 [Crossref]
- Weiner P, Zeidan F Zamir D, Pelled B, Waizman J, Beckerman M, et al. Prophylactic inspiratory muscle training in patients undergoing coronary artery bypass graft. World J Surg 1998;22(5):427-31. doi: 10.1007/s002689900410 [Crossref]
- Cahalin LP, Semigran MJ, Dec GW. Inspiratory muscle training in patients with chronic heart failure awaiting cardiac transplantation: results of a pilot clinical trial. Phys Ther 1997;77(8):830-8. doi: 10.1093/ptj/77.8.830 [Crossref]
- Hulzebos EHJ, van Meeteren NLU, van den Buijs BJWM, Bie RA, Riviere AB, Helders PJM. Feasibility of preoperative inspiratory muscle training in patients undergoing coronary artery bypass surgery with a high risk of postoperative pulmonary complications: a randomized controlled pilot study. Clin Rehabil 2006;20(11):949-59. doi: 10.1177/0269215506070691 [Crossref]
- Faghy MA, Brown PI. Functional training of the inspiratory muscles improves load carriage performance. Ergonomics 2019 Aug; 62(11):1439-49. doi: 10.1080/00140139.2019.1652352 [Crossref]
- Sadek Z , Salami A, Joumaa WH, Awada C, Ahmaidi S, Ramadan W. Best mode of inspiratory muscle training in heart failure patients: a systematic review and meta-analysis. Eur J Prev Cardiol [Internet]. 2018 [cited 2022 May 12];25(16):1691-701. doi: 10.1177/2047487318792315 [Crossref]
- Gomes Neto M, Martinez BP, Reis HF, Carvalho VO. Pre- and postoperative inspiratory muscle training in patients undergoing cardiac surgery: systematic review and meta-analysis. Clin Rehabil 2016;31(4):454-64. doi: 10.1177/0269215516648754 [Crossref]
- Ozalp O, InalInce D, Cakmak A, CalikKutukcu E, Saglam M, Savci S, et al. High-intensity inspiratory muscle training in bronchiectasis: a randomized controlled trial. Respirology 2018;24(3):246-53. doi: 10.1111/ resp.13397 [Crossref]
- Freitas FS, Parreira VF, Ibiapina CC. Aplicação clínica do pico de fluxo da tosse: uma revisão de literatura. Fisioter Mov 2010;23(3):495-502. doi: 10.1590/S0103-51502010000300016 [Crossref]
- Pescatello LS, Arena R,
Riebe D, Thompson PD. [Crossref] ACSM guidelines for testing effort and prescribing. 9.
ed. São Paulo: Grupo Nacional; 2014.
- van Peppen RP, Kwakkel G, Wood-Dauphinee S, Hendriks HJ, van der Wees PJ, Dekker J. The impact of physical therapy on functional outcomes after stroke: what’s the evidence? Clin Rehabil 2004;18(8):833-62. doi: 10.1191/0269215504cr843oa [Crossref]
- Silva E, Bianchi T, de
Freitas W, Sposito L, da Silva F, de Souza R, et al.
Artigo de revisão treinamento concorrente: endurance
x força concurrent training: endurance
vs. strength [Internet]. 2018 [cited 2020
Nov 4]. Available from:
https://portalrevistas.ucb.br/index.php/RBCM/article/view/7175
- Savci S, Degirmenci B, Saglam M, Arikan H, Inal-Ince D, Turan HN, et al. Short-term effects of inspiratory muscle training in coronary artery bypass graft surgery: a randomized controlled trial. Scandin Cardiovasc J 2011;45(5):286-93. doi: 10.3109/14017431.2011.595820 [Crossref]