Rev Bras Fisiol Exerc 2021;20(3):304-14
doi: 10.33233/rbfex.v20i3.4821
ORIGINAL ARTICLE
Patients with metabolic syndrome present decreased
cardiorespiratory fitness when subjected to maximum progressive exercise
Pacientes
com síndrome metabólica apresentam diminuição da aptidão cardiorrespiratória
frente ao exercício progressivo máximo
Caroline
Simões Teixeira1,2, Mariana Antonio Corrêa1,
Débora Dias Ferraretto Moura Rocco1,4, Giulliano Gardenghi3, Jefferson Cabral de
Carvalho1, Alessandra Medeiros2, Alexandre Galvão da
Silva1,4
1Faculdade de Educação Física e Esporte
(FEFESP), Universidade Santa Cecília (UNISANTA), Santos, SP, Brasil
2Universidade Federal de São Paulo
(UNIFESP), Campus Baixada Santista, Santos, SP, Brasil
3Hospital ENCORE, Aparecida de Goiânia,
GO, Brasil
4Clínica de Reabilitação PROCárdio, São Paulo, SP, Brasil
Received:
April 9, 2021; Accepted: May 28, 2021
Correspondence: Alexandre Galvão da Silva, Rua Oswaldo Cruz, 277,
11045-907 Santos SP
Caroline Simões Teixeira: carolteixeira@unisanta.br
Mariana Antônio Corrêa: mwhite.s@hotmail.com
Débora Dias Ferraretto Moura
Rocco: drocco@unisanta.br
Giulliano Gardenghi:
coordenacao.cientifica@ceafi.edu.br
Jefferson Cabral de
Carvalho : Jefferson.jcc@homail.com
Alessandra Medeiros: ale.med@icloud.com
Alexandre Galvão da Silva: agalvao@unisanta.br
Abstract
Background: Metabolic
Syndrome represents a set of predisposing factors for the development of
cardiovascular diseases and other pathophysiological repercussions such as
decreased aerobic capacity, an important marker of mortality. Due to
limitations in the measurement of VO2max, studies on the behavior of
ventilatory parameters in submaximal phases of exercise are necessary so that
it can be reproduced the patient’s general performance during maximum physical
effort. Objective: To compare cardiorespiratory fitness between women
with metabolic syndrome and sedentary eutrophic women. Methods: 277 female
individuals (42,1 ± 5.5 years) were evaluated, divided into two groups, Group 1
– Metabolic Syndrome (MetS = 210) and Group 2 –
Control Heath (HC = 67), all patients underwent the ergospirometric
test, which consists of performing a graduated exercise with direct analysis of
respiratory gases. The data were expressed as mean and standard deviation and
the inferential analysis performed with the Test T student. For multivariate
correlations, we used the linear regression model stepwise. For all tests, the
level of significance adopted was 5%. Results: MetS
Group showed loss when compared to the HC Group in weight, body mass index and
risk factors for MetS p < 0.05). In the
Cardiopulmonary Exercise Test, had lower values of VO2peak (21.2 ± 4.6; and
27.5 ± 9.3 ml/kg/min, respectively, Interaction; p < 0.05) and a lower value
for VO2 at the anaerobic threshold (14.3 ± 7.1; and 12.1 ± 4.0;
Interaction; p < 0.05). Correlating directly with the BMI (R = -0.48; p <
0.05) and CA (R = -0.47; P = 0.05). Conclusion: Patients with metabolic
syndrome have decreased cardiorespiratory efficiency compared to maximum
progressive exercise.
Keywords: metabolic syndrome;
cardiorespiratory efficiency; sedentary women
Resumo
Introdução: A síndrome metabólica representa um
conjunto de fatores predisponentes para desenvolvimento de doenças
cardiovasculares e outras repercussões fisiopatológicas como diminuição da
capacidade aeróbia, importante marcador de mortalidade. Devido às limitações na
mensuração do VO2max, estudos sobre o comportamento dos parâmetros ventilatórios
em fases submáximas do exercício se fazem necessários para que possa reproduzir
o desempenho geral do paciente durante esforço físico máximo. Objetivo:
Comparar a capacidade cardiorrespiratória entre mulheres com síndrome
metabólica e mulheres eutróficas sedentárias. Métodos:
Foram avaliados 277 indivíduos (42,1 ± 5,5 anos) do sexo feminino, divididos em
dois grupos, Grupo 1 – Síndrome Metabólica (SMet =
210) e Grupo 2 – Controle saudável (CS = 67), todos os pacientes realizaram o
teste ergoespirométrico, que consiste na execução de exercício graduado com
análise direta dos gases respiratórios. Os dados foram expressos em média e
desvio-padrão e a análise inferencial realizada com o Teste T student. Para as correlações multivariadas, foi utilizado o
modelo de regressão linear de stepwise. Para todos os
testes, o nível de significância adotado foi de 5%. Resultados: O Grupo
com SMet apresentou prejuízo quando comparado ao CS
no peso, índice de massa corpórea e nos fatores de risco da SMet,
p < 0,05). No Teste de Exercício Cardiopulmonar, apresentou menores valores
de consumo de oxigênio pico (VO2pico, 21,2 ± 4,6; e 27,5 ± 9,3 ml/kg/min,
respectivamente, Interação; P < 0,05) comparados com CS e menor valor para o
limiar anaeróbio VO2LA (14,3 ± 7,1; e 12,1 ± 4,0; Interação; P <
0,05), correlacionando-se diretamente com as IMC (R = -0,48; P < 0,05) e CA
(R =-0,47; P = 0,05). Conclusão: Pacientes com SMet
apresentam diminuição da eficiência cardiorrespiratória frente ao exercício
progressivo máximo.
Palavras-chave: síndrome metabólica; eficiência
cardiorrespiratória; mulheres sedentárias.
Introduction
The Metabolic
Syndrome (MetS) is considered as a complex metabolic
disorder for the development of cardiovascular diseases [1,2]. Regardless of the
entity or group that defines MetS, the
components/risk factors are always the same, associated with the development of
cormobidities with pathophysiological repercussions
[1].
Studies show
that in addition to metabolic changes, MetS also had
a negative impact on cardiorespiratory adjustments, such as, for example,
decreased aerobic capacity, an important marker of mortality [3].
The maximum
oxygen consumption (VO2max) is directly related to cardiac output,
arterial oxygen content and alveolar-capillary gas exchange, a gold standard
technique for assessing the relationship of cardiorespiratory and
musculoskeletal systems [4,5].
Patients with MetS, according to the data in the literature, present a
decrease in aerobic competence, being one of the justifications for such
alteration, the decrease in the mandatory adequate muscle strength [6,7,8].
According to the
study by Yokota et al. [9], it was characterized that there is a
relationship between decreased aerobic capacity and abnormalities in skeletal
muscle metabolism. The decrease in VO2 in relation to exercise is
very present in .com MetS, however, the literature
must also include this decrease, which can be proven by the influence of
patient and professional motivation [10,11,12].
Due to these
limitations in the measurement of VO2, ventilatory parameters are
being used by researchers in submaximal phases of the exercise so that they can
reproduce the patient's general performance [13,14,15].
To date, there
are few investigations and studies on the behavior of cardiorespiratory
parameters in relation to submaximal effort in patients with MetS, not scientifically evidencing whether this set of
risk factors that classify MetS, impairs the
cardiorespiratory efficiency of individuals during the performance physical
exercise.
The aim of the
present study was to compare cardiorespiratory fitness between women with MetS and sedentary eutrophic women during progressive
physical exercise and their relationship with the risk factors involved.
Methods
277 female
individuals were evaluated, considering the high frequency of this gender in
the search for our rehabilitation service (42.1 ± 5.5 years), separated into MetS Group (MetS) (n = 210) and
Healthy Control Group (HC) (n = 67), followed by the PROCárdio
LTDA Rehabilitation Clinic and the UNIFESP Physical and Experimental Training
Laboratory. Initially, they were screened and received information about the
project so that they could be invited to participate in the study. Then, they
underwent clinical and laboratory evaluation to determine their health
condition. Those who did not present the factors that characterize the MetS were invited to participate in the study as a healthy
control group with the objective of comparing parameters.
This study was
sent to the Research Ethics Committee of the Federal University of São Paulo
(UNIFESP), Santos, SP and approved under number 3,036,417.
All volunteers
signed the Free and Informed Consent Form, authorizing their participation in
the study.
We included
sedentary women with Metabolic Syndrome according to the diagnostic criteria of
the National Cholesterol Education Program, Adult Treatment Panel III (NCEP
III) and sedentary women, between 18 and 50 years old, without metabolic
syndrome, for the control group. We excluded women enrolled in physical
activity or training programs, or dietary treatment, smokers, with a history of
alcohol consumption, cardiovascular disease or any other pathology or physical
limitation that made it impossible to perform the cardiopulmonary stress test
(TECP) and women who did not participate in any of the stages of this project.
Procedures
Individuals who
agreed to participate in the study underwent medical evaluation and underwent
all initial examinations. Three blood pressure measurements were taken before
the cardiopulmonary test.
The body
composition was evaluated, and height (m) and body weight (kg) were measured on
a Filizola scale. The body mass index (BMI) was determined
by calculating the weight divided by the height squared [BMI = weight
(kg)/height² (m)].
The evaluation
of abdominal circumference was measured at the midpoint between the last rib
and the iliac crest because many obese patients had their navel directed
downwards due to the excessive curvature of the abdominal wall. Three
consecutive measurements were taken, always by the same appraiser, and the
value that most repeated was recorded.
Laboratory tests
were performed in the morning, with the individual fasting for 12 hours. An
antecubital vein was catheterized to collect venous blood for laboratory
evaluations: complete blood count (it was performed by automated electronic
counting and a morphological study in smears stained with panoptic dyes), blood
glucose (it was carried out by the enzymatic, automated method - Roche), total
cholesterol and fractions , triglycerides and HDL-cholesterol (made by the
colorimetric enzymatic method) and the calculation of LDL-cholesterol (Low
Density Lipoproteins or low density Lipoproteins) according to the Lipid
Research Clinics Program. Following the guidance of the IV Brazilian Guidelines
on Dyslipidemias of the Brazilian Society of Cardiology (2007), direct
measurement of LDL-cholesterol was made (and not calculated by the equation)
whenever the results of triglycerides are greater than or equal to 400 mg/dL.
The
cardiopulmonary stress test was performed on the Cortex equipment of Meta
Analysis 3s. The values were collected with each breath and converted into an
average of 30 seconds. The parameters analyzed were:
oxygen consumption (VO2 L min-1 or mL kg-1 min-1
STPD); carbon dioxide production (VCO2 mL/min-1 STPD);
pulmonary ventilation (VE L/min BTPS); tidal volume (VCL/min BTPS); respiratory
rate (RR rpm); estimated functional dead space (VD/VT); respiratory exchange
ratio (RER); ventilatory equivalents of oxygen (VE/VO2) and carbon
dioxide (VE/VCO2) and final expiratory pressures of oxygen and
carbon dioxide (PetO2 and PetCO2 mmHg). Before each
assessment, the metabolic analyzer was calibrated using gases with carbon
dioxide and oxygen balanced with nitrogen, and the flow meter was calibrated
with a 3-liter syringe. The test was performed on a treadmill (Micromed), using the ramp protocol with constant increase
in speed and/or inclination every minute until exhaustion, with load increments
calculated by the maximum load predicted until exhaustion.
For the analysis
of the heart rate behavior during the exam, an electrocardiogram with twelve
standard leads was used (D1, D2, D3, aVR, aVL, aVF, V1, V2, V3, V4, V5, V6
- ECG Marquette Medical Systems, InC.CardioSoft,
Wisconsin, USA) and to evaluate blood pressure the auscultatory method was
used. The test was considered maximum when the patient reached respiratory
exchange ratio values ≥ 1.10 associated with the exhaustion reported by
the patient himself. Physical capacity was determined by peak oxygen
consumption (VO2peak) at the end of the exam. At rest, during and
after the cardiorespiratory functional assessment, electrocardiographic
recording was performed, in addition to periodic blood pressure measurements by
an auxiliary. Periodically, the patient was asked about his symptoms on
exertion, such as tiredness, heaviness in the legs and dizziness.
The ventilatory
anaerobic threshold (LAV) was measured by the V-slope method (Beaver et al.
1986), which consists of the loss of linearity between the production of VCO2
and the consumption of VO2.
At the end, the
group with MetS was compared with the healthy control
group to analyze the results.
Diagnosis of MetS
The MetS was diagnosed according to the National Cholesterol
Education Program - Adult Treatment Panel III (NCEP ATPIII) where the
individual is characterized as having the syndrome in the presence of three of
the five cardiovascular risk factors, as it follows:
- Abdominal circumference ≥ 102 cm for men and ≥
88 cm for women;
- Triglycerides ≥ 150 mg/dL;
- HDL-cholesterol < 40 mg/dL for men and < 50
mg/dL for women;
- Systolic blood pressure ≥ 130 mmHg or diastolic
blood pressure ≥ 85 mmHg;
- Fasting blood glucose ≥ 110 mg/dL.
Statistical analysis
The sample size
was calculated using the OpenEpi99 statistical program. A power of 80% was
proposed, with a 95% confidence interval (two-tailed) to admit the probability
of type 1 error in only 5%. Thus, it was found that at least 23 patients per
group should be recruited.
The variables
analyzed in this study were subjected to the Kolmogorov-Smirnov test to verify
whether they had a normal distribution. The variables that did not show this
distribution were analyzed after logarithmic transformation.
The data on the
anthropometric, metabolic and baseline cardiorespiratory characteristics of
both groups were submitted to Student's t-test statistical analysis for
non-repeated measures.
For multivariate
correlations, the stepwise linear regression model was used. For all tests, the
level of significance adopted was 5%.
Results
Baseline evaluation and characteristics according to MetS
In Tables I, II
and III we observed baseline data regarding anthropometric, metabolic, and
cardiorespiratory characteristics of the studied groups (MetS
Group and HC Group).
Significant
differences were observed between the groups studied in anthropometric,
metabolic, and cardiorespiratory parameters.
Anthropometric parameters
The evaluation
of the anthropometric parameters, according to the comparison of the groups,
gave the patients significant differences regarding the BMI, the body
composition (abdominal waist, lean mass, fat mass) as expected for the group
with Met (Table I).
We did not
observe differences in relation to age and height in the groups studied (Table
I).
Table I - Clinical
characteristics of the 277 individuals studied according to the separation of
the metabolic syndrome (MetS) and healthy control
groups (HC)
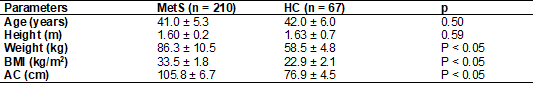
Values are expressed as
mean ± SD; No statistical significance p > 0.05. Statistical significance p
< 0.05; AC = Abdominal circumference; HC = Healthy Control; BMI = Body Mass
Index; Met = Metabolic Syndrome
Metabolic parameters
Following the
same pattern of organization and comparison of the groups, the influence of MetS on metabolic parameters was evaluated. In Table II,
the MetS group conferred significant differences on
the metabolic variables to the patients.
Table II - Laboratory
characteristics of the 277 individuals studied according to the separation of
the metabolic syndrome (MetS) and healthy control
groups (HC)
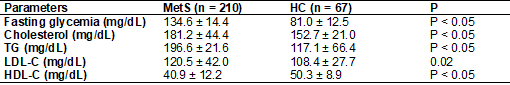
Values are expressed as
mean ± SD, Statistical Significance p < 0.05. HC =Healthy Control; HDL-c =
High Density Lipoprotein Cholesterol; LDL-c = Low Density Lipoprotein
Cholesterol; TG = triglycerides; Met = Metabolic Syndrome
Hemodynamic and cardiorespiratory parameters
About baseline
cardiorespiratory data, significant differences were observed in systolic blood
pressure (SBP) and in maximum functional capacity (VO2peak) between the MetS groups and the healthy control group (Table III).
Table III - Cardiorespiratory
characteristics of the 277 individuals studied according to the separation of
the metabolic syndrome (MetS) and healthy control
(HC) groups)
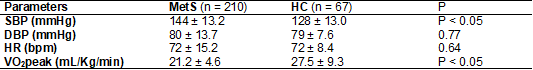
Values are expressed as
mean ± SD; without statistical significance p > 0.05; Statistical
significance p < 0.05; HR = Heart Rate; SBP = Systolic Blood Pressure; DBP =
Diastolic Blood Pressure
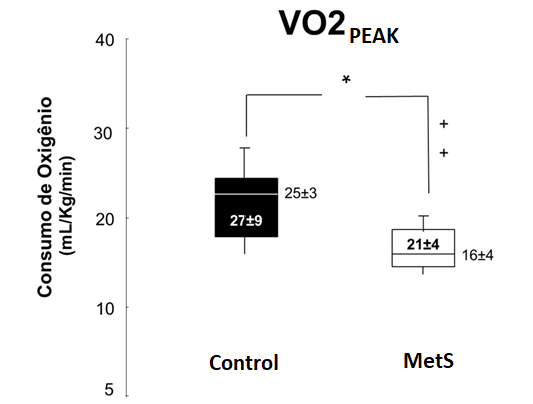
Figure 1 –
Comparison of VO2peak values between the metabolic syndrome (MetS) and control groups. Values are expressed as mean ±
standard deviation; *p < 0.05 mL/kg/min vs GC
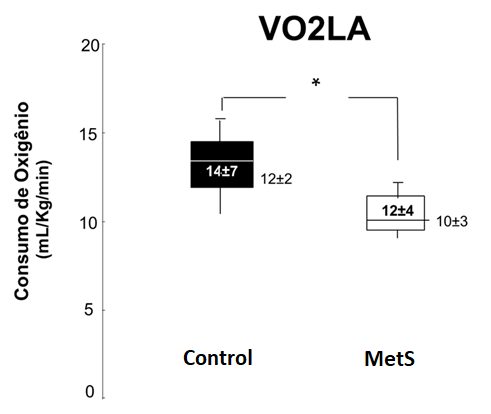
Figure 2 - Comparison
of VO2LA values between the metabolic syndrome (MetS)
and control groups. Values are expressed as mean ± standard deviation, *p <
0.05 mL/kg/min vs control group
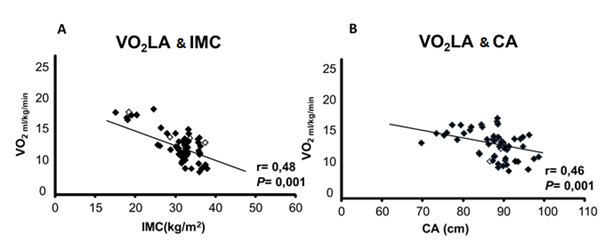
Figure 3 – In
the analysis of VO2LA multivariate correlation between risk factors
for MetS, as expected there was an inverse and
significant correlation of Body Mass Index (BMI) (Figure 3A) and the Abdominal
Circumference (AC) (Figure 3B)
Discussion
The present
study expanded the current knowledge about the factors that influence the
harmful effects of MetS on the behavior of the
cardiorespiratory system in the face of a situation of physical stress in women
with MetS during progressive physical exercise. The
hypothesis suggested was that the cluster of abnormalities and pathologies that
make up patients with MetS, could negatively modulate
cardiorespiratory adjustments during a situation of physical stress. It was
found in this investigation that the relative oxygen consumption at peak effort
(VO2peak) and aerobic efficiency (VO2LA) were reduced in
patients with MetS when compared with eutrophic
individuals and the direct influence of the accumulation of adipose tissue on
the physical capacity of this population.
Corroborating, Miyatake N et al. [8] studying the influence of MS
in the Japanese population noticed that this population showed a decrease in VO2peak
and VO2LA, when compared to eutrophic individuals [8]. The authors
evidenced the influence of the increase in fat mass and decrease in the
percentage of lean mass, reflecting in the lower physical capacity of
individuals with MetS [8].
Yokota et al.
[9] observed that the metabolic changes present in patients with MetS, mainly to insulin resistance, are strongly associated
with changes in skeletal muscle metabolism, the study demonstrated a decrease
in mitochondrial metabolism for oxidative phosphorylation and ATP production
impairing the aerobic capacity of individuals with MetS.
In this sense,
researchers have described that mortality increases in the period of 14 years
as there is a decrease in VO2peak, both in healthy individuals and
in cardiac patients [3]. However, the literature has shown that the measurement
of VO2peak may have a bias as it is highly influenced by the
motivation of the patient and the investigator [17,18]. Due to these
limitations in the measurement of VO2peak, several researchers have
used submaximal exercise parameters to reproduce the individual's overall
performance [19,20,21].
In addition to
the use of VO2peak as an important predictor of mortality,
assessments of oxygen consumption in submaximal loads have already been
described as a marker of poor prognosis, such as VO2 at the
anaerobic threshold (VO2LA) [19] and the oxygen consumption ratio
and workload (DVO2/DW) [8], which indicate the individual's metabolic
efficiency. Studies have observed that patients who reach VO2LA ≤
11 ml/kg/min are at higher cardiovascular risk [22].
Likewise, we
demonstrated that the aerobic capacity (VO2peak), and the submaximal
index (VO2LA) were reduced in patients with MetS.
Thus, we show that, in fact, the changes in the MetS
are the main factors for the decrease in the TECP indexes.
Finally, this
investigation showed a strong correlation to the direct influence of BMI and AC
on the oxygen consumption evaluated in submaximal loads (VO2LA) with
VO2peak. The data from this investigation demonstrate an inverse
relationship between weight gain and cardiopulmonary capacity efficiency during
the ergospirometric test. Therefore, the increase in
body weight interfered negatively in the response of oxygen consumption to
submaximal exercise in individuals with MetS.
Excessive
concentration of body fat has a profound influence on aerobic fitness, showing
that adiposity reduces maximum aerobic power in relation to weight (VO2max/kg)
[23,24] and that functional fitness during exercise is negatively related to
the degree of obesity [24,25].
There is a
negative relationship between the increase in abdominal waist and VO2LA
during submaximal physical exercise. These data are consistent with previous
findings that demonstrated that changes in ventilatory function were attributed
to extrinsic mechanical compression of adiposity, which can cause a reduction
in chest wall compliance and, consequently, increase in respiratory work, thus,
determining factors for the decrease in aerobic capacity [26,27,28]. There was no
direct relationship between the other risk factors for MetS
and the ventilatory responses during the examination of ergospirometry.
Results of previous studies [8] support the notion that VO2 at peak
effort, as well as hemodynamic responses to exercise, is directly influenced by
obesity during cardiopulmonary assessment [8]. Thus, it can be observed that
obesity has a direct interference with the cardiorespiratory efficiency of the
patient with MetS, leading to a greater risk of
cardiovascular complications in the future.
It is worth
mentioning that a new health perspective arises due to the current situation, a
pandemic caused by Sars-CoV-2 where the population most vulnerable to gravity
and mortality is precisely the one studied in this investigation. The knowledge
provided by this research can help to better understand the relationship
between the risk factors for cardiovascular diseases and the main system
affected by Sars-CoV-2, the respiratory system.
In the same
context, individuals with MetS, due to changes in
cardiorespiratory efficiency mainly due to pulmonary limitations, such as
abnormalities in the ventilation-perfusion ratio, become more predisposed to
depend on mechanical ventilation and other intensive care if they contract
Covid-19 [29].
Conclusion
Based on the
results, we can conclude that patients with MetS
presented a decrease in Maximum Oxygen Consumption compared to the maximum
progressive exercise and that among the various risk factors for MetS, BMI and AC have a direct relationship in physical
capacity in this population group.
Conflict of interest
No potential conflict
of interest.
Academic affiliation
This article represents
the master's dissertation performed by student Caroline Simões
Teixeira, supervised by Professor Dr. Alessandra Medeiros and co-supervised by
Professor Doctor Alexandre Galvão da Silva at the
Federal University of São Paulo (UNIFESP) – Baixada Santista
Campus, Santos, SP, Brazil.
Authors’ contribution
Conception and design
of the research: Teixeira HC, Rocco DDFM, Silva AG. Data gathering: Teixeira
HC, Corrêa MA, Carvalho JC, Rocco DDFM, Silva AG.
Analysis and interpretation of data: Medeiros A, Rocco DDFM, Silva AG.
Statistical analysis: Silva, AG. Fund Raising: not applicable. Writing of the
manuscript: Teixeira HC, Medeiros A, Rocco DDFM, Silva AG. Critical review of
the manuscript for important intellectual content: Gardenghi
G.
Acknowledgements
We would like to thank
the senior management of the institution represented by Dr. Silvia Teixeira,
Dr. Lucia Teixeira and Dr. Marcelo Teixeira from the
Santa Cecilia University for their support as well as our Laboratory of
Exercise Physiology and Health (LAFES).
Referências
- Pesaro
AEP, Serrano CV, Nicolau JC. Infarto agudo do miocárdio – síndrome coronariana
aguda com supradesnível do segmento ST. Rev Assoc Med Bras
2004;50(2):214-20. doi: 10.1590/S0104-42302004000200041 [Crossref]
- Colombo
RCR, Aguillar OM. Estilo de vida e fatores de risco de pacientes com primeiro
episódio de infarto agudo do miocárdio. Rev Latinoam Enferm 1997;5(2):69-82. doi: 10.1590/S0104-11691997000200009 [Crossref]
- Ishitani LH, Franco GC, Perpétuo IHO, França E. Desigualdade social e mortalidade precoce por doenças cardiovasculares no Brasil. Rev Saúde Pública 2006;40(4):684-91. doi: 10.1590/S0034-89102006000500019 [Crossref]
- Palange P, Ward SA, Carlsen KH, Casaburi R, Gallagher CG, Gosselink R, et al. Recommendations on the use of exercise testing in clinical practice. Eur Respir J 2007;29(1):185-209. doi: 10.1183/09031936.00046906 [Crossref]
- Myers J, Prakash M, Froelicher V, Do D, Partington S, Atwood JE. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med 2002;346(11):793-801. doi: 10.1056/NEJMoa011858 [Crossref]
- Jurca R, Lamonte MJ, Barlow CE, Kampert JB, Church TS, Blair SN. Association of muscular strength with incidence of metabolic syndrome in men. Med Sci Sports Exerc 2005;37(11):1849-55. doi: 10.1249/01.mss.0000175865.17614.74 [Crossref]
- Kosola J, Vaara JP, Ahotupa M, Kyrolainen H, Santtila M, Oksala N. Elevated concentration of oxidized LDL together with poor cardiorespiratory and abdominal muscle fitness predicts metabolic syndrome in young men. Metabolism 2013;62(7):992-9. doi: 10.1016/j.metabol.2013.01.013 [Crossref]
- Miyatake N, Saito T, Wada J, Nishikawa H, Matsumoto S, Miyachi M. Linkage between oxygen uptake at ventilatory threshold and muscle strength in subjects with and without metabolic syndrome. Acta Med 2007;61(5):255-9. doi: 10.18926/AMO/32895 [Crossref]
- Yokota T, Knugawa S, Okita K, Hirabayashi K, Suga T, Hatorri M, et al. Lower aerobic capacity was associated with abnormal intramuscular energetic in patients with metabolic syndrome. Hypertens Res 2011;34(9):1029-34. doi: 10.1038/hr.2011.78 [Crossref]
- Lakka TA, Laaksonem DE, Laaka HM, Männikö N, Niskanen LK, Raumramaa R, et al. Sedentary life style, poor cardiorespiratory fitness, and the metabolic syndrome. Med Sci Sports Exerc 2003;35(8):1279-86. doi: 10.1249/01.MSS.0000079076.74931.9A [Crossref]
- Clark Al, Poole-Wilson PA, Coats AJ. Effects of motivation of the patient on indices of exercise capacity in chronic heart failure. Br Heart J 1994;71(2) 162-5. doi: 10.1136/hrt.71.2.162 [Crossref]
- Yazbeck
Junior P, Carvalho RT, Sabbag LMS, Battistella LR. Ergoespirometria. Teste de esforço cardiopulmonar,
metodologia e interpretação. Arq Bras
Cardiol 1998;71(5):719-24. doi: 10.1590/S0066-782X1998001100014 [Crossref]
- Weber KT, Kinasewitz GT, Janicki JS, Fishman AP. Oxygen utilization and ventilation during exercise in patients with chronic cardiac failure. Circulation 1982;65(6):1213-23. doi: 10.1161/01.cir.65.6.1213 [Crossref]
- Andreacci J, Le Mura LM, Cohen SL, Urbansky EA, Chelland SA, Duvillard V. The effects of frequency of encouragement on performance during maximal exercise testing. J Sports Sci. 2002;20(4):345-52. doi: 10.1080/026404102753576125 [Crossref]
- Beaver WL, Wasserman K, Whipp
BJ. A new method for detecting anaerobic threshold by gas exchange. J Appl Physiol 1986;60(6):2020-7. doi: 10.1152/jappl.1986.60.6.2020 [Crossref]
- Neto
AS. Fatores de risco para aterosclerose relacionado ao nível de aptidão
cardiorrespiratória em adolescentes [Dissertação]. Curitiba: Ciências
Biológicas da Universidade Federal do Paraná, Curitiba; 2007.
http://www.educadores.diaadia.pr.gov.br/arquivos/File/2010/artigos_teses/EDUCACAO_FISICA/
dissertacao/STABELINI,NETO.pdf
- Sociedade Brasileira de Cardiologia. I Diretriz brasileira de diagnóstico e tratamento da síndrome metabólica. Arq Bras Cardiol 2005;84(supl1):1-28. doi: 10.1590/S0066-782X2005000700001 [Crossref]
- Rennie KL, McCarthy N, Yazdgerdi
S, Marmot M, Brunner E. Association of metabolic syndrome with both vigorous
and moderate physical activity. Int J Epidemiol 2003;32(4):600-6. doi: 10.1093/ije/dyg179 [Crossref]
- Gustat J, Srinivasan SR, Elkasabany A, Berenson GS. Relation of self-rated measures of physical activity to multiple risk factors of insulin resistance syndrome in young adults: the Bogalusa Heart study. J Clin Epidemiol 2002;55(10):997-1006. doi: 10.1016/s0895-4356(02)00427-4 [Crossref]
- Wareham NJ, Hennings SJ, Byrne CD, Hales CN, Prentice AM, Day NE. A quantitative analysis of the relationship between habitual energy expenditure, fitness and the metabolic cardiovascular syndrome. Br J Nutr 1998;80(3):235-41. doi: 10.1017/s0007114598001287 [Crossref]
- Ciolac
EG, Guimarães GV. Exercício físico e síndrome metabólica. Rev
Bras Med Esporte 2004;10(4):319-24.
- Myers J, Arena R, Oliveira RB, Bensimhon D, Hsu L, Chase P, et al. The lowest VE/VCO2 ratio during exercise as a predictor of outcomes in patients with heart failure. J Cardiac Fail 2009;15(9):756-62. doi: 10.1016/j.cardfail.2009.05.012 [Crossref]
- Marinov B , Kostianev S, Turnovska T. Ventilatory efficiency and rate of perceived exertion in obese and non-obese children performing standardized exercise. Clin Physiol Funct Imaging 2002;22(4):254-60. doi: 10.1046/j.1475-097x.2002.00427.x [Crossref]
- Rowland TW. Effects of obesity on aerobic fitness in
adolescent females. Am J Dis Child 2001;145(7):764-8.
- Arena R, Cahalin LP. Evaluation of cardiorespiratory fitness and respiratory muscle function in the obese population. Prog Cardiovasc Dis 2014;56(4):457-64. doi: 10.1016/j.pcad.2013.08.001 [Crossref]
- Welch BE, Riendeau RP, Crisp CE, Isenstein RS. Relationship of maximal oxygen consumption to various components of body composition. J Appl Physiol 1958;12(3):395-8. doi: 10.1152/jappl.1958.12.3.395 [Crossref]
- Whipp BJ, Davis JA. The ventilatory stress of exercise in obesity. Am Rev Respir Dis 1984;129 (2 Pt 2):S90- 2. doi: 10.1164/arrd.1984.129.2P2.S90 [Crossref]
- Delorey DS, Wyrick BL, Babb TG. Mild-to-moderate obesity: implications for respiratory mechanics at rest and during exercise in young men. Int J Obes 2005;29(9):1039-47. doi: 10.1038/sj.ijo.0803003 [Crossref]
- Sales-Peres SHC, Azevedo-Silva LJ, Bonato RCS, Sales-Peres MC, Pinto ACS, Junior JFS. Coronavirus (SARS-CoV-2) and the risk of obesity for critically illness and ICU admitted: Meta-analysis of the epidemiological evidence. Obes Res Clin Pract 2020;14(5):389-97. doi: 10.1016/j.orcp.2020.07.007 [Crossref]