Rev Bras Fisiol Exerc 2022;21(2):101-12
doi: 10.33233/rbfex.v21i2.5102ORIGINAL ARTICLE
High and low volume core stabilization training in
chronic low back pain: randomized crossover study
Alto
e baixo volume do treino de estabilização do core na dor lombar crônica: ensaio
randomizado cruzado
Poliana
de Jesus Santos1, Marta Silva Santos1, Alan Bruno Silva
Vasconcelos2, Marzo Edir Da Silva
Grigoletto2
1Universidade Federal de Sergipe,
Aracajú, SE, Brazil
2Departamento de Educação Física, Centro
Universitário Ages, Paripiranga, BA, Brazil
Received: February 17,2022; Accepted: March 18, 2022.
Correspondence: Poliana de Jesus Santos, Department of physiology, Cidade Univ. Prof.
José Aloísio de Campos Av. Marechal Rondon, s/n, Jd. Rosa Elze,
São Cristóvão SE, Brazil
Poliana
de Jesus Santos: polianasantos.28@hotmail.com
Marta
Silva Santos: martasilvaedf@gmail.com
Alan
Bruno Silva Vasconcelos: abs.vasconcelos@gmail.com
Marzo Edir Da Silva Grigoletto:
marzogrigoletto@gmail.com
Resumo
Introdução: O treino de estabilização do core é
indicado na literatura como opção eficaz na dor lombar crônica (DLC), no
entanto, o volume adequado desse treinamento para induzir analgesia nessa
população permanece desconhecido. Objetivo: Avaliar o efeito de uma
sessão do treino de estabilização do core de alto e baixo volume na modulação
endógena da dor em mulheres com DLC. Metodologia: Trata-se de um ensaio
clínico, randomizado, cruzado e cego em relação ao avaliador. Dezoito
voluntárias realizaram duas sessões do treinamento de estabilização do core:
alto e baixo volume. Foi avaliado o limiar de dor por pressão (LDP), somação
temporal (ST) e modulação condicionada da dor (MCD) antes a após a realização
do treinamento. A ANOVA de medidas repetidas 2x2 foi realizada para comparar
treino e tempo, o teste post hoc de Bonferroni para
comparação em pares das interações (tempo e treinamento). Os dados foram
expressos em média e desvio padrão e o nível de significância estabelecido em
5%. Resultados: O treino de estabilização do core de baixo volume
apresentou aumento significativo do LDP em L5 (p < 0,05) e tibial anterior
(p < 0,01). Já o treino de alto volume não apresentou aumento significativo
no LDP. No entanto, nenhum dos protocolos investigados alteraram a ST e MCD em
mulheres com DLC. Conclusão: O treino de estabilização do core de baixo
volume produz analgesia local e hipoalgesia remota,
no entanto, nenhum dos protocolos investigados foram capazes de reduzir a
sensibilização central avaliada por meio da CPM e ST.
Palavras-chave: dor crônica; lombalgia; exercício
físico; analgesia; mulheres.
Abstract
Introduction: Core
stabilization training is pointed as an effective option for pain relief
chronic non-specific low back pain (CNLBP), however, the adequate training
volume to induce analgesia is still unknown. Objective: To evaluate the effect
of one session of high and low volume core stabilization training protocols on
endogenous pain modulation in women with CNLBP. Methods: This is an
evaluator-blinded randomized crossover trial. Eighteen volunteers participated
of the study, whom performed two core stabilization training sessions: high and
low training volume. The variables evaluated were the pressure pain thresholds
(PPT) and temporal summation (TS) by digital pressure algometer, in addition to
the conditioned pain modulation (CPM) using a pressure algometer and ischemic
compression with sphygmomanometer as conditioned stimulus. A 2x2 repeated
measures ANOVA was performed to compare training and time, Bonferroni's post
hoc test for pairwise comparison from interactions (time and training). Data
were expressed as mean ± standard deviation and the significance level
established in 5%. Results: When comparing pre and post intragroup, low
volume core stabilization training showed significant increase at the PPT in L5
(p < 0.05) and tibialis anterior (p < 0.01). High volume training not
showed a significant increase in none of the PPT measures. However, none of the
investigated protocols changed TS and CPM in women with CNLBP. Conclusion:
Low volume core stabilization training produces local analgesia and remote
hypoalgesia, demonstrated by increased PPT in L5 and tibialis anterior.
However, none of the investigated protocols were effective to reduce the
central sensitization assessed by CPM and TS.
Keywords: Low back pain; physical exercise;
analgesia; women.
Introduction
Chronic low back pain (CLBP) can be
classified as specific or non-specific, according to its origin. Chronic
nonspecific low back pain (CNLBP) is not associated with a disease or
attributable cause and represents the majority of cases, about 90% [1]. A
comparative study shows that patients with CLBP have greater pain sensitization
when compared with healthy controls [2]. Despite not having a justifiable
cause, studies show that central sensitization (CS) can contribute to the
development and maintenance of CNLBP [3]. In the current scientific literature,
the CS is commonly evaluated by means of the temporal summation (TS) [4].
Physical exercise is recommended as
a treatment to CNLBP [5], since exercise activates endogenous analgesia
pathways [6] of healthy people or patients with CNLBP [7]. Regarding healthy
people, pain-free individuals, an acute exercise session results in a period of
hypoalgesia known as exercise induced hypoalgesia (EIH) [8]. EIH is usually
assessed by pressure pain thresholds (PPT) measured before and after an
exercise session [9]. There is an increase in these thresholds during EIH
period, which may last for up to 30 minutes after exercise [10]. In individuals
with chronic pain, different results were found after an acute exercise session
on pain sensitivity [11,12] which can be explained in part by the increase
central excitability and decrease in the conditioned pain modulation (CPM)
[13]. CPM is the traditional method to assess the activation of the endogenous
descending inhibitory pathways and brain facilitators [14,15].
In this context, studies showed
that physical exercises focused on improvement of the strength, motor control
and endurance of the trunk muscles are more effective in reducing signs and
symptoms and improving functional capacity of individuals with CNLBP when
compared the cardiorespiratory exercises, global exercise and pilates [15,16]. Thus, evidence suggests that stabilization
exercises have better results in reducing pain intensity and disability when
compared with controls or other types of exercise [17,18].
A recent systematic review [19]
showed that, in general, this training is performed with three sets, however,
it is not clear if this training volume is the most adequate. In addition, is
necessary estimate the minimum training dose for patients with CNLBP. Physical
exercise can excite and inhibits the CNS, resulting in hyperalgesia or
hypoalgesia, respectively [13], and the training volume is related to these
effects. Thus, it is important to determine the necessary training volume to induce
analgesia in women with CNLBP.
In this sense, this study is
justified by the importance of evaluating the effects of core stability
training volume in women with CNLBP, since the ideal training dose cannot be
determined by the current published data [20,21]. Therefore, the objective of
this study was to evaluate the effect of a high and low volume of a core
stabilization training session on endogenous pain modulation of women with
CNLBP. We hypothesized that low volume core stabilization training generates
activation of endogenous analgesic pathways, resulting in increased PPT,
activation of CPM and decreased TS in these patients. We believe that low
volume training do not cause increased central
sensitization, but the activation of endogenous descending inhibitory pathways.
Methods
This is an evaluator-blinded
randomized clinical crossover trial carried in the Department of Physical
Education of the Federal University of Sergipe. The study was registered in the
Brazilian Registry of Clinical Trials-ReBEC No:
RBR-6wy5y4t (https://ensaiosclinicos.gov.br/rg/RBR-6wy5y4t).
Participants
We included 18 post-menopausal
women with a clinical diagnosis of chronic nonspecific low back pain; aged
between 45 and 59 years; with pain level greater than three on the numerical
pain rating scale; body mass index (BMI < 30); not having undergone spinal
surgery; not exercising regularly; not perform physical therapy or other pain
treatment; do not use analgesic, anti-inflammatory, opioid or immunosuppressive
medication. The exclusion criteria were missing one of the test days; having
some motor, psychiatric or cognitive impairment, hearing, visual or
communication disorder that make impossible to perform the protocol. The
patients were recruited from waiting list for attendance in the rehabilitation
center of the University Hospital.
The trial protocol was approved by
the Research Ethics Committee of the Federal University of Sergipe, Brazil
under No. 4.884.045 (CAAE 28060319.3.0000.5546) and followed the principles of
the 1964 Declaration of Helsinki and its later amendments. Informed consent was
obtained from all participants.
Sample size
The sample calculation was
performed using the G-Power program, version 3.1.9.4, based on the results of Paungmali [22]. For a power of 95% and an alpha of 0.05,
considering two conditions and two times, the total sample suggested was 16
volunteers. Five more participants were added, resulting in a total of 21
participants.
Outcomes
An evaluator blinded to the
interventions received the participants and evaluated them before and after the
training protocols.
The primary outcome was the pain,
measured through the pressure pain threshold (PPT), assessed using a digital
pressure algometer with an area of 1 cm2 (Sistema®, EMG, São José
dos Campos, SP, Brazil). The measurement was performed in two different body
sites, in the paravertebral and anterior tibial muscles. In the lumbar region
the PPT was evaluated bilaterally 5 cm lateral to the spinous processes of L3
and L5 [23,24] and in the tibialis anterior the measurement occurred in the
right leg at 5 cm from tibial tuberosity [24,25,26]. With the algometer positioned
perpendicular to the patient's tissue, increasing pressure was applied and the
patient was instructed to report when the pressure was clearly painful. Three
measurements were done and the mean was recorded. The PPT was evaluated by a
physical therapist with clinical experience in the treatment of patients with
chronic low back pain and master in physiological sciences.
The secondary outcome was central
sensitization (CS) assessed through conditioned pain modulation (CPM) and
temporal summation (ST). To assess CPM, first, PPT was measured on the right
forearm, 7.5 cm from wrist line. Then the conditioned stimulus was applied, to
this an ischemic compression of 270 mmHg was performed on the contralateral arm
with a sphygmomanometer (Mikatos®, Embu, SP, Brazil)
positioned 3 cm close the cubital fossa. Pain intensity was verbally requested
using the numerical classification pain scale and when equal or greater than 4,
the PPT was measured in the right forearm, 7.5 cm from wrist line, during
ischemic compression. Five minutes after this procedure, the PPT was measured
again, now without compression [27].
TS was assessed with the algometer
positioned 7.5 cm above the wrist line, exerting a constant pressure of 4
kg/cm2. The volunteer was asked to verbally inform the pain intensity through
the 11-point numerical pain classification scale that ranges from 0 to 10, with
0 indicating no pain and 10 worst pain imaginable [28], during the 1º, 10º, 20º
and 30º seconds of stimulation [27].
Factors as medication use, sleep, kinesiophobia, and depression can influence perception and
sensory testing. To control these factors, the participants were instructed not
to use medication 24 hours before the tests performed and questionnaires were
applied to assess the quality of sleep, kinesiophobia
and the level of depression of the volunteers.
Randomization
Randomization was performed using a
Latin square design, the treatments were distributed so that each one appeared
only once in each line [29]. In the first session, the volunteer performed the
corresponding training protocol and 48 hours after finish the first protocol,
the volunteer returned to the laboratory to the second training, completing the
crossover.
Intervention
All participants performed the
interventions in a temperature-controlled environment (23 ± 0.5°C), always
during the morning, with 48 hours between sessions to minimize any possible
transmission effects between workouts [20,22]. The training protocols were
conducted by a physical education professional with master's degree in physical
education and years of experience in the realization training protocol. All
protocols were performed by the same evaluator.
Before starting training, the
volunteers were instructed on the breath they have maintain during the
protocols, for this, performed five hollowing maneuvers, three sets of five
bracing breaths, then, to prepare the muscles for the exercises, thoracic,
lumbar and hip mobility was performed, five sets each.
The training protocols consisted of
two moments: in the first, exercises were performed to maximum muscle strength
and motor control, for this, were performed the hunting dog exercises, lateral
plank with support on both feet, bilateral pelvic lifting, lateral plank with
support of one foot, superman static and front plank. In the second moment, the
exercises had as objective to train the resistance of this musculature, through
the abdominal curl up, abdominal oblique and hip flexion (in dorsal decubitus
and knee flexion), carried out in this order. The density of the exercises was
1:2 for both training, with 20 seconds of exercise and 40 seconds of rest. The
number of sets was 3 for high and 1 for low, considering the same exercises.
Moreover, there was no rest between exercises and all were performed in
isometric.
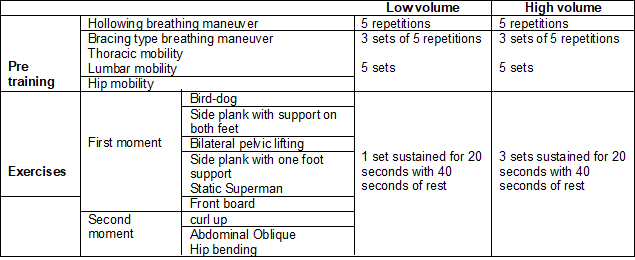
The sequence of the high and low
volume core stability training exercises can be viewed in board 1.
Board 1 - Description of core stability
training
Statistical analysis
The data were statistically
analyzed using the Social Sciences Statistical Package (SPSS), version 23.0.
The normality of the data was tested through the Kolmogorov Smirnov test. A 2x2
repeated measures ANOVA was performed to compare training and time, and
comparison in pairs the interactions between factors time and training through
the Bonferroni post hoc. The data were expressed as mean and standard deviation
and the level of significance established in 5%.
Results
This trial was carried between
October 2019 and February 2020. 75 potential participants were selected and/or
evaluated, of which 21 were selected to be part of the study. 18 participants
(52.72 ± 3.40 years) were included in the study, all volunteers performed two
types of protocols, low volume core stabilization training and high volume core stabilization training. The flow diagram of
the enrollment, randomization, training, and data analysis process can be
visualized in figure 1. The personal characteristics of the sample can be
visualized in table I.
Table I - Personal characteristics of
the sample
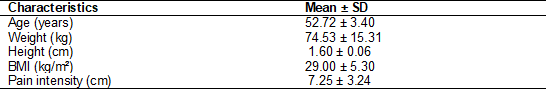
BMI = Body Mass Index
When compared the pre and post intragroups, the low volume core stabilization training
significantly increased the PPT in L5 (3.21 ± 1.42 pre; 3.58 ± 1.61 post;
p < 0.05) and tibialis anterior (4.49 ± 1.67 pre; 4.97 ± 1.45 post;
p<0.01). High-volume training did not increase none of the PPT measures. No
differences were noted when compared the PPT between low and high
volume groups. These results of low and high volume
core training in the PPTs can be seen in Figure 2.
The intragroup comparison showed
not significant difference in the TS in high volume training, however,
low-volume training showed a significant difference for the 30ºs measure (7,83
± 1,94 pre; 7,05 ± 2,53 post; p < 0,05). In the CPM analysis, the intragroup
comparison showed not significant difference from pre to post in none of the
protocols investigated. When comparing the effect of low volume with high
volume training not significant difference for none intervention in the CPM and
TS. The results of the low and high volume core
stabilization training in the TS and CPM can be seen in Figure 3.
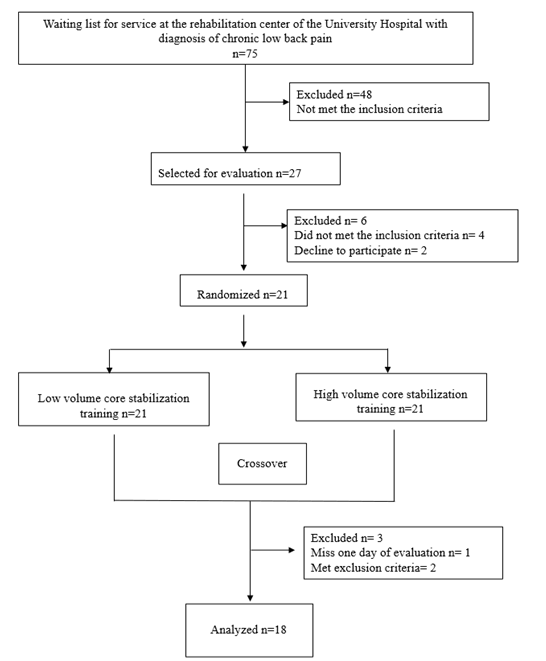
Figure 1 - Flow diagram of the
randomized crossover trial
Patients were recruited from the
waiting list of a rehabilitation center, which contained only: name, sex, age,
health problem that made him seek the physical therapy service and contact
number. Thus, only a few criteria could be evaluated at this first moment.
After this survey, an evaluation was scheduled with everyone who met the
inclusion criteria. After this evaluation, 4 people were excluded from the
sample because they had a BMI > 30, had undergone spinal surgery and were
undergoing physical therapy
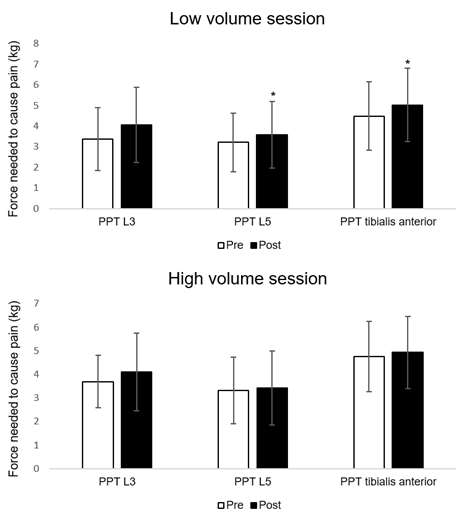
*Significant intragroup difference
(p < 0.05); PPT = pressure pain threshold; L3 = third lumbar vertebra; L5 =
fifth lumbar vertebra
Figure 2 - Difference between the means
of pre and post training results in the PPT
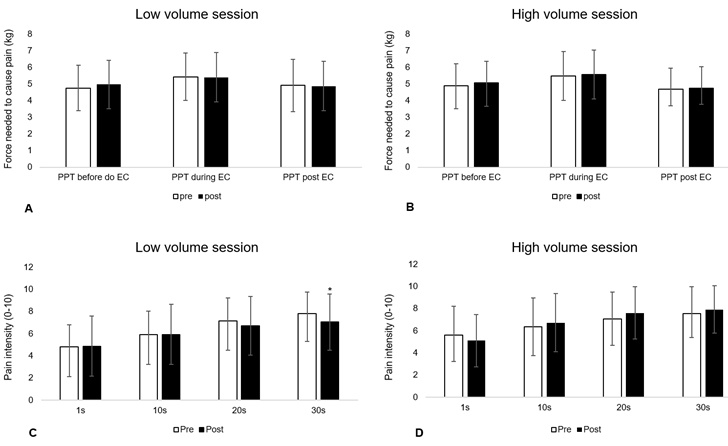
A and B) Conditioned pain modulation;
C and D) Temporal summation of pain; *Significant intragroup difference (p <
0.05). PPT: pressure pain threshold; EC = conditioned stimulus; S = seconds
Figure 3 - Difference between the means
of pre and post training results in the CPM and ST.
Discussion
Our study showed that low-volume
core stabilization training decreased PPT in L5 and tibialis anterior muscle.
Thus, the proposed training protocol caused an EIH in the injury site and
remote hypoalgesia. However, the training protocol was not able to decrease CS
and activate descending inhibitory pathways of women with CNLBP.
The mechanisms responsible for EIH
are not fully understood. Human research shows controversial results [8], while
animal studies showed that opioid hypothesis is more consistent. However, EIH
can also occur through activation of the endocannabinoid, serotoninergic,
immune, autonomic nervous system, and conditioned pain modulation systems [8,10,13,30]. In populations with chronic pain, this phenomenon may be impaired in
some people, and may remain unchanged or even have hyperalgesia in response to
exercise. The mechanisms that can explain this fact are unknown [10].
Depending on the dose applied,
physical exercise can either excite or inhibit the CNS, resulting in
hyperalgesia or hypoalgesia [13]. The study by Dailey et al. [31] showed
that patients with fibromyalgia report greater increases in pain and perceived
fatigue after performing a physically strenuous task when compared to healthy
individuals. Furthermore, a recent systematic review showed that a training
duration of 20 to 30 minutes had a greater impact on effect sizes on pain and
disability [19]. As evidenced in the studies above, patients with chronic pain
benefit from a protocol of less fatiguing training for pain reduction, perhaps,
that's why low volume training showed better results compared to high volume.
Studies have also shown increased
excitability in the central nervous system in people with CKD and in other
chronic pain conditions [26,32] these patients when undergoing an acute
exercise session do not show EIH and in some cases even show hyperalgesia in
response to training [33]. As observed in the present study, high volume showed
no difference in reducing pain after performing training. This may be explained
in part by the fact that this training generates a very large stimulus and
excites the CNS even more.
Pain reduction post core stability
training could be due the improved motor control, since when have good local
motor control, it is possible to control the peripheral nociceptive impulse in
progress and, eventually, central sensitization can be avoided [22]. However,
as showed here, a single session of this training was not able to reduce
central sensitization assessed through TS and CPM. Similar results were already
found [34] and, in some cases, showing increased neuronal excitability after
exercise [35].
One of the factors that probably
influenced our results was the age and gender of the patients evaluated. The
current literature shows that CPM is reduced with age and is more impaired in
women with chronic pain conditions [36]. In human research, women have shown
greater central excitability in measures as temporal summation, secondary
hyperalgesia, referred pain, and decreased CPM [33,37,38]. These gender
differences may, in part, explain impaired EIH in the chronic pain population.
However, studies do not provide evidence that EIH is less effective in women
[10].
To the best of our knowledge, this
was the first study to evaluate the effects of core stability training in the
endogenous pain modulation of women with CNLBP. The present research also
investigated the influence of training volume in this population. To avoid
hormonal interference, our study included postmenopausal women. In addition,
majority research that evaluated EIH was conducted with young or healthy
population, and those that evaluated PPT in individuals with chronic low back
pain not present the PPT values of each investigated point separately
[23,24,26]. The anatomical and biomechanical characteristics between the lumbar
vertebrae may interfere the final results of the PPT evaluated. Therefore,
values for each point should be presented separately. Furthermore, the studies
that investigated core stabilization training not provide information about the
training volume [19]. Future research should explore the effects of this
long-term training in the endogenous pain modulation in this population.
Nevertheless, the study proposal to
assess the volume of core stability training in women with CNLBP has important
theoretical and clinical implications. Thus, is suggested that professionals
that choose to use this method for treating patients with CNLBP, consider all
of the above points before implementing the study results in the clinical
practice. At the same time, our study indicated that the proposed training not
increase pain perception, unlike studies that investigated the effects of
physical exercise in other populations with chronic pain. Both training
protocols are safe to be tested longitudinally, since they do not increase the
pain threshold, however, the effects for pain reduction should be tested in the
long term, comparing with other types of treatment suggested for chronic low
back pain and a control group. Furthermore, this research can help professional
in the clinical practice and researchers understand the neurophysiological
process behind the training investigated in women with CNLBP.
Conclusion
Low volume core stabilization
training produces local analgesia and secondary hypoalgesia, demonstrated by
the increase in the PPTs of L5 and anterior tibialis. However, none of the
treatment protocols were able to activate endogenous descending inhibitory
pathways and decrease central sensitization. Further studies should investigate
the long-term effects of the volume of this training.
Conflict of interest
None
Financing source
Santos
PJ - Master's scholarship holder from Coordenação de
Aperfeiçoamento de Pessoal de Nível Superior-CAPES, Brazil
(Process number:
88882.443503/2019-01).
Authors’ contribution
Research conception and design: Santos PJ, Santos MS, Grigoletto
MES; Data collection: Santos PJ, Santos MS; Statistical analysis: Santos PJ,
Santos MS; Data analysis and
interpretation: Santos PJ, Santos MS; Statistical analysis: Santos PJ,
Santos MS; Writing of the document: Santos PJ, Santos
MS, Vasconcelos ABS; Critical review of the manuscript
for important intellectual content: Vasconcelos ABS, Grigoletto
MES.
References
- Balagué F,
Mannion AF, Pellisé F, Cedraschi
C. Non-specific low back pain. Lancet 2012;379(9814):482-91. doi: 10.1016/S0140-6736(11)60610-7 [Crossref]
- Giesbrecht RJ, Battié MC. A
comparison of pressure pain detection thresholds in people with chronic low
back pain and volunteers without pain. Phys Ther 2005
[Internet];85(10):1085-92. [cited 4 June 2022] Available from:
https://pubmed.ncbi.nlm.nih.gov/16180957/
- Curatolo M, Arendt-Nielsen L. Central hypersensitivity in chronic musculoskeletal pain. Phys Med Rehabil Clin N Am 2015;26(2):175-84. doi: 10.1016/j.pmr.2014.12.002 [Crossref]
- Arribas-Romano A, Fernández-Carnero J, Molina-Rueda F, Angulo-Diaz-Parreño S, Navarro-Santana MJ. Efficacy of physical therapy on nociceptive pain processing alterations in patients with chronic musculoskeletal pain: a systematic review and meta-analysis. Pain Med 2020;21(10):2502-17. doi: 10.1093/pm/pnz366 [Crossref]
- Hayden JA, Wilson MN, Stewarts S, Cartwright JL, Smith AO, Riley RD, et al. Exercise treatment effect modifiers in persistent low back pain: an individual participant data meta-analysis of 3514 participants from 27 randomised controlled trials. Br J Sports Med 2020;54(21):1277-78. doi: 10.1136/bjsports-2019-101205 [Crossref]
- Nijs J, Kosek E, Van Oosterwijck J, Meeus M. Dysfunctional endogenous analgesia during exercise
in patients with chronic pain: to exercise or not to exercise? Pain Physician
2012 [Internet] ;15(3 Suppl):Es205-13. [cited June 4,
2022]. Available from: https://pubmed.ncbi.nlm.nih.gov/22786458/
- van Middelkoop M, Rubinstein SM, Verhagen AP, Ostelo RW, Koes BW, van Tulder MW. Exercise therapy for chronic nonspecific low-back pain. Best Pract Res Clin Rheumatol 2010;24(2):193-204. doi: 10.1016/j.berh.2010.01.002 [Crossref]
- Koltyn KF. Analgesia following exercise: a review. Sports Med 2000;29(2):85-98. doi: 10.2165/00007256-200029020-00002 [Crossref]
- Grimby-Ekman A, Ahlstrand C, Gerdle B, Larsson B, Sandén H. Pain intensity and pressure pain thresholds after a light dynamic physical load in patients with chronic neck-shoulder pain. BMC Musculoskelet Disord 2020;21(1):266. doi: 10.1186/s12891-020-03298-y [Crossref]
- Rice D, Nijs J, Kosek E, Wideman T, Hasenbring MI, Koltyn K, et al. Exercise-induced hypoalgesia in pain-free and chronic pain populations: state of the art and future directions. J Pain 2019;20(11):1249-66. doi: 10.1016/j.jpain.2019.03.005 [Crossref]
- Burrows NJ, Booth J, Sturnieks DL, Barry BK. Acute resistance exercise and pressure pain sensitivity in knee osteoarthritis: a randomised crossover trial. Osteoarthritis Cartilage 2014;22(3):407-14. doi: 10.1016/j.joca.2013.12.023 [Crossref]
- Kuithan P, Heneghan NR, Rushton A, Sanderson A, Falla D. Lack of exercise-induced hypoalgesia to repetitive back movement in people with chronic low back pain. Pain Pract 2019;19(7):740-50. doi: 10.1111/papr.12804 [Crossref]
- Lima LV, Abner TSS, Sluka KA. Does exercise increase or decrease pain? Central mechanisms underlying these two phenomena. J Physiol 2017;595(13):4141-50. doi: 10.1113/JP273355 [Crossref]
- Navratilova E, Nation K, Remeniuk B, Neugebauer V, Bannister K, Dickenson AH, et al. Selective modulation of tonic aversive qualities of neuropathic pain by morphine in the central nucleus of the amygdala requires endogenous opioid signaling in the anterior cingulate cortex. Pain 2020;161(3):609-18. doi: 10.1097/j.pain.0000000000001748 [Crossref]
- Rhudy JL, Lannon EW, Kuhn BL, Palit S, Payne MF, Sturycz CA, et al. Assessing peripheral fibers, pain sensitivity, central sensitization, and descending inhibition in Native Americans: main findings from the Oklahoma Study of Native American Pain Risk. Pain 2020;161(2):388-404. doi: 10.1097/j.pain.0000000000001715 [Crossref]
- Searle A, Spink M, Ho A, Chuter V. Exercise interventions for the treatment of chronic low back pain: a systematic review and meta-analysis of randomised controlled trials. Clin Rehabil 2015;29(12):1155-67. doi: 10.1177/0269215515570379 [Crossref]
- Bhadauria EA, Gurudut P. Comparative effectiveness of lumbar stabilization, dynamic strengthening, and Pilates on chronic low back pain: randomized clinical trial. J Exerc Rehabil 2017;13(4):477-85. doi: 10.12965/jer.1734972.486 [Crossref]
- Niederer D, Mueller J. Sustainability effects of motor control stabilisation exercises on pain and function in chronic nonspecific low back pain patients: A systematic review with meta-analysis and meta-regression. PLoS One 2020;15(1):e0227423. doi: 10.1371/journal.pone.0227423 [Crossref]
- Mueller J, Niederer D. Dose-response-relationship of stabilisation exercises in patients with chronic non-specific low back pain: a systematic review with meta-regression. Sci Rep 2020;10(1):16921. doi: 10.1038/s41598-020-73954-9 [Crossref]
- Paungmali A, Joseph LH, Punturee K, Sitilertpisan P, Pirunsan U, Uthaikhup S. Immediate effects of core stabilization exercise on β-endorphin and cortisol levels among patients with chronic nonspecific low back pain: a randomized crossover design. J Manipulative Physiol Ther 2018;41(3):181-8. doi: 10.1016/j.jmpt.2018.01.002 [Crossref]
- Waseem M, Karimi H, Gilani SA, Hassan D. Treatment of disability associated with chronic non-specific low back pain using core stabilization exercises in Pakistani population. J Back Musculoskelet Rehabil 2019;32(1):149-54. doi: 10.3233/BMR-171114 [Crossref]
- Paungmali A, Joseph LH, Sitilertpisan P, Pirunsan U, Uthaikhup S. Lumbopelvic core stabilization exercise and pain modulation among individuals with chronic nonspecific low back pain. Pain Pract 2017;17(8):1008-14. doi: 10.1111/papr.12552 [Crossref]
- Corrêa JB, Costa LO, de Oliveira NT, Sluka KA, Liebano RE. Effects of the carrier frequency of interferential current on pain modulation in patients with chronic nonspecific low back pain: a protocol of a randomised controlled trial. BMC Musculoskelet Disord 2013;14:195. doi: 10.1002/ejp.889 [Crossref]
- Corrêa JB, Costa LO, de Oliveira NT, Sluka KA, Liebano RE. Central sensitization and changes in conditioned pain modulation in people with chronic nonspecific low back pain: a case-control study. Exp Brain Res 2015;233(8):2391-9. doi: 10.1007/s00221-015-4309-6 [Crossref]
- Dailey DL, Rakel BA, Vance CG, Liebano RE, Amrit AS, Bush HM, et al. Transcutaneous electrical nerve stimulation reduces pain, fatigue and hyperalgesia while restoring central inhibition in primary fibromyalgia. Pain 2013;154(11):2554-62. doi: 10.1016/j.pain.2013.07.043 [Crossref]
- O'Neill S, Kjær P, Graven-Nielsen T, Manniche C, Arendt-Nielsen L. Low pressure pain thresholds are associated with, but does not predispose for, low back pain. Eur Spine J 2011;20(12):2120-5. doi: 10.1007/s00586-011-1796-4 [Crossref]
- Leite PMS, Mendonça ARC, Maciel LYS, Poderoso-Neto ML, Araujo CCA, Góis HCJ, et al. Does electroacupuncture treatment reduce pain and change quantitative sensory testing responses in patients with chronic nonspecific low back pain? a randomized controlled clinical trial. Evid Based Complement Alternat Med 2018:8586746. doi: 10.1155/2018/8586746 [Crossref]
- Karcioglu O, Topacoglu H, Dikme O. A systematic review of the pain scales in adults: Which to use? Am J Emerg Med 2018;36(4):707-14. doi: 10.1016/j.ajem.2018.01.008 [Crossref]
- Nogueira CSN, Corrente EC, Piedade SMS. Quadrados latinos obtidos por meio de técnicas de confundimento em ensaios fatoriais. Sci Agr 2020;57:421-4. doi: 10.1590/S0103-90162000000300008 [Crossref]
- Koltyn KF, Brellenthin AG, Cook DB, Sehgal N, Hillard C. Mechanisms of exercise-induced hypoalgesia. J Pain 2014;15(12):1294-304. doi: 10.1016/j.jpain.2014.09.006 [Crossref]
- Dailey DL, Keffala VJ, Sluka KA. Do cognitive and physical fatigue tasks enhance pain, cognitive fatigue, and physical fatigue in people with fibromyalgia? Arthritis Care Res (Hoboken) 2015;67(2):288-96. doi: 10.1002/acr.22417 [Crossref]
- Imamura M, Chen J, Matsubayashi SR, Targino RA, Alfieri FM, Bueno DK, et al. Changes in pressure pain threshold in patients with chronic nonspecific low back pain. Spine (Phila Pa 1976) 2013;38(24):2098-107. doi: 10.1097/01.brs.0000435027.50317.d7 [Crossref]
- Meeus M, Roussel NA, Truijen S, Nijs J. Reduced pressure pain thresholds in response to exercise in chronic fatigue syndrome but not in chronic low back pain: an experimental study. J Rehabil Med 2010;42(9):884-90. doi: 10.2340/16501977-0595 [Crossref]
- Ray CA, Carter JR. Central modulation of exercise-induced muscle pain in humans. J Physiol 2007;585(Pt 1):287-94. doi: 10.1113/jphysiol.2007.140509 [Crossref]
- Kapandji AI. Fisiologia articular. 5 ed. Rio de
Janeiro: Guanabara Koogan; 2000.
- Lannersten L, Kosek E. Dysfunction of endogenous pain inhibition during exercise with painful muscles in patients with shoulder myalgia and fibromyalgia. Pain 2010;151(1):77-86. doi: 10.1016/j.pain.2010.06.021 [Crossref]
- Lewis GN, Rice DA, McNair PJ. Conditioned pain modulation in populations with chronic pain: a systematic review and meta-analysis. J Pain 2012;13(10):936-44. doi: 10.1016/j.jpain.2012.07.005 [Crossref]
- Arendt-Nielsen L, Fernández-de-Las-Peñas C, Graven-Nielsen T. Basic aspects of musculoskeletal pain: from acute to chronic pain. J Man Manip Ther 2011;19(4):186-93. doi: 10.1179/106698111X13129729551903 [Crossref]
- Roussel NA, Nijs J, Meeus M, Mylius V, Fayt C, Oostendorp R. Central sensitization and altered central pain processing in chronic low back pain: fact or myth? Clin J Pain 2013;29(7):625-38. doi: 10.1097/AJP.0b013e31826f9a71 [Crossref]