Rev Bras Fisiol Exerc 2022;21(2):92-100
doi: 10.33233/rbfex.v21i2.5183ORIGINAL ARTICLE
Gait speed and hospital readmission after coronary
artery bypass grafting
Velocidade
de marcha e reinternação hospitalar após cirurgia de
revascularização do miocárdio
Andrea
Oliveira dos Santos1, Thais Jesus dos Santos Soares1,
André Raimundo Guimarães2, André Luiz Lisboa Cordeiro1,3
1.
Faculdade Nobre, Feira de Santana, BA, Brazil
2.
Instituto Nobre de Cardiologia, Feira de Santana, BA, Brazil
3.
Escola Bahiana de Medicina e Saúde Pública, Salvador,
BA, Brazil
Received: May 30, 2022; Accepted: May 31, 2022.
Correspondence: André Luiz Lisboa
Cordeiro, Av. Maria
Quitéria, 2116, Centro, 44001-008 Feira de Santana BA, Brazil
Andrea
Oliveira dos Santos: andreasantos@gmail.com
Thais
Jesus dos Santos Soares: thaissoares@gmail.com
André
Raimundo Guimarães: andremed@bol.com.br
André
Luiz Lisboa Cordeiro: andrelisboacordeiro@gmail.com
Abstract
Introduction: Gait speed can
be applied, predicting outcomes associated with hospital stay such as length of
stay and/or discharge. Despite these studies that correlate gait speed with the
aforementioned outcomes, when we deal with cardiac surgery there is a gap. Objective:
Verify whether gait speed is associated with the risk of hospital readmission
in the postoperative period of coronary artery bypass grafting. Methods:
This is a prospective cohort study. In the preoperative period, all patients
underwent a 10-meter gait speed test and repeated at hospital discharge. After
the repetition of the gait speed test, patients were divided into two groups:
slow and non-slow. Those who were not discharged walked less than 1.0 m/s
occupied the slow group and those who were above 1.0 m/s were classified as not
slow. Patients were followed for six months to observe the primary outcome,
which was the need for hospital readmission. Results: The 6 months rate
of readmission was 58% (14/24, 95% CI 49% to 80%) among slow walkers and 17%
(6/36, 95% CI 13% to 46%) among non-slow walkers (p = 0.002). In univariate
analysis, gait speed, treated as a continuous variable, was associated with the
primary outcome (HR = 0.6, 95% CI 0.2 to 0.9), while age, gender, BMI, MV and CPB
time were not. In the multivariate model including age, gender, BMI, MV and CPB
time, gait speed remained the only variable associated with readmission
(multivariate HR = 0.5, 95% CI 0.1 to 0.7 p = 0.02). Conclusion: Our data
suggest that gait speed is associated with hospital readmission in patients
undergoing to coronary artery bypass grafting.
Keywords: critical care; walk test;
exercise; early walking; intensive care units.
Resumo
Introdução: A velocidade de marcha pode ser
aplicada, prevendo resultados associados à estadia hospitalar, tais como
duração da estadia e/ou alta. Apesar de estudos que correlacionam a velocidade
de marcha com os resultados acima mencionados, quando lidamos com a cirurgia
cardíaca existe uma lacuna. Objetivo: Verificar se a velocidade da
marcha está associada ao risco de readmissão hospitalar no período
pós-operatório de cirurgia de revascularização do miocárdio. Métodos:
Este é um estudo de coorte prospectivo. No período pré-operatório, todos os
pacientes foram submetidos a um teste de velocidade de marcha de 10 metros e
repetido na alta hospitalar. Após a repetição do teste de velocidade de marcha,
os pacientes foram divididos em dois grupos: lentos e não lentos. Os que não
tiveram alta andaram menos de 1,0 m/s ocuparam o grupo lento e os que estavam
acima de 1,0 m/s foram classificados como não lentos. Os pacientes foram
acompanhados durante seis meses para observar o resultado primário, que era a
necessidade de readmissão hospitalar. Resultados: A taxa de readmissão
de 6 meses foi de 58% (14/24; 95% IC 49% a 80%) entre os lentos e 17% (6/36;
95% IC 13% a 46%) entre os não lentos (p = 0,002). Na análise univariada, a velocidade de marcha, tratada como variável
contínua, foi associada ao resultado primário (HR 0,6; 95% IC 0,2 a 0,9),
enquanto que idade, sexo, IMC, VM e tempo de CEC não foram. No modelo
multivariado incluindo idade, sexo, IMC, VM e tempo de CEC, a velocidade de
marcha permaneceu a única variável associada à readmissão (multivariado HR:0,5,
95% IC 0,1 a 0,7, p = 0,02). Conclusão: Os nossos dados sugerem que a
velocidade de marcha está associada à readmissão hospitalar em pacientes
submetidos a cirurgia de revascularização do miocárdio.
Palavras-chave: cuidados intensivos; teste de marcha;
exercício; deambulação precoce; unidades de terapia intensiva.
Introduction
In recent years, heart disease has
increased considerably, causing a large number of surgical procedures that aim
to increase patient survival [1]. There are several risks and complications of
this form of treatment that can interfere in pulmonary capacity and physical
performance, reducing the functionality of patients. The decrease in daily
activities of life due to prolonged hospitalization can also lead to several
neuromuscular, pulmonary, functional and quality of life problems [2].
Patients after cardiac surgery tend
to have muscle weakness due to lack of movement, loss of physical conditioning,
inflammation, use of drugs such as corticosteroids, muscle relaxants,
neuromuscular blockers, antibiotics and in the presence of associated neuromuscular
syndromes [3]. This weakness may be associated with decreased walking speed in
the postoperative period, with this variable being associated with worse
outcomes such as mortality and hospital readmission in other profiles such as
hypercapnic heart and respiratory failure [4,5].
Gait speed can be assessed using
the 10-meter test [6]. This test can be applied preoperatively, predicting
outcomes associated with hospital stay such as length of stay and/or discharge
[7,8]. Changes in the organism with the surgical procedure cause a decline in
the patient's functional activities in the postoperative phase, making walking
a complex skill, as gait speed tends to decrease due to the physiological
changes that occur such as the reduction of muscle strength [9].
Despite these studies that
correlate gait speed with the aforementioned outcomes, when we deal with
cardiac surgery there is a gap. This answer can be useful for making decisions
and directing appropriate intervention to minimize these adverse results. The
aim of this study was to verify whether gait speed is associated with the risk
of hospital readmission in the postoperative period of coronary artery bypass
grafting.
Methods
Study design
This is a prospective cohort study
that was conducted between January 2018 and July 2019, in patients undergoing
to coronary artery bypass grafting (CABG) at the Instituto Nobre
de Cardiologia / Santa Casa de Misericórdia,
in the city of Feira de Santana (BA). The research was approved by the Research
Ethics Committee of Faculdade Nobre,
under number 796,580 and the patients were included after signing the informed
consent form.
Eligibility criteria
Patients aged over 18 years, of
both sexes, submitted to coronary artery bypass graft surgery who used
cardiopulmonary bypass and median sternotomy were included. Individuals with
some physical limitation, such as sequelae of stroke and lower limb amputation,
uncontrolled arrhythmias, changes in blood pressure at the time of the test
(SBP < 80 or > 160 mmHg), angina, electrocardiographic changes were
excluded.
Study protocol
In the preoperative period, all
patients included in the survey underwent a 10-meter walk test. The following
day, everyone underwent a surgical procedure, was referred to the Intensive
Care Unit (ICU) and, being discharged, was directed to the inpatient unit. In
all these moments, they received routine care from the unit without any
influence from the researchers. All patients were assisted by the
physiotherapist on duty and performed breathing exercises, orthostasis training
on the first postoperative day, sitting in the chair and ambulation on the
second postoperative day when there was no clinical contraindication (use of
vasoactive drugs, uncontrolled pain or infectious changes). On the day of
hospital discharge, patients repeated the 10-meter test.
After the repetition of the gait
speed test, patients were divided into two groups: slow and non-slow. The
cutoff point used was 1.0 m/s based on the study by Odonkor
et al. [10]. Those who were not discharged walked less than 1.0 m/s
occupied the slow group and those who were above 1.0 m/s were classified as not
slow. Patients were followed for six months to observe the primary outcome,
which was the need for hospital readmission. There was a comparison between the
groups of the initial, final butch speed, delta velocity, cardiopulmonary
bypass (CPB), mechanical ventilation (MV), Intensive Care Unit (ICU) time and
hospital stay. It is worth mentioning that readmission in any hospital was
counted for this study, patients were contacted by telephone seeking this type
of information.
Measuring instruments
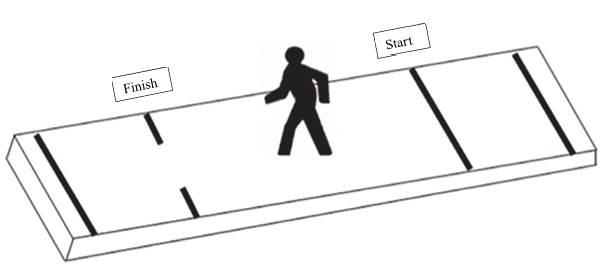
The 10-meter speed test took place
in a corridor with no movement of people. A space of 14 meters was used, the first
two for acceleration and the last two for deceleration [6]. Therefore, the 10
meters were used to assess speed. The test was performed three times and an
average of the three values was calculated. Before and after each repetition,
the patients had their vital signs checked.
For the test, a chronometer was
also used, evaluating the time the patient needed to walk for 10 meters and
expressed in meters/second [7] (Figure 1). All repetitions were performed by a
single examiner.
Statistical analysis
We then adjusted the association of
gait speed with the primary outcome by using a multivariable Cox proportional
hazards model adjusting for age, BMI and sex, and additionally adjusting for
clinically relevant covariates (MV and CPB time). All tests for statistical
significance were two-tailed with an alpha level of 0.05. Analyses were
conducted using SPSS version 20.0 and R version 2.14.113.
Results
During the research period 71
patients were admitted, and fifteen were excluded due to physical limitations.
Thus, 56 patients were evaluated, of these 38 (63%) were male, mean age 61 ± 9
years, with an average BMI of 27 ± 5 km/m2, with the most prevalent
comorbidity being sedentary with 19 (63%). The other data are shown in Table I.
Table I - Clinical, surgical and
functional data of the studied patients
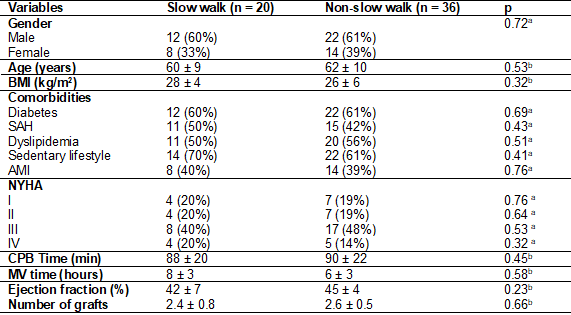
aChi-square; bIndependent
Student's T test; BMI = Body Mass Index; SAH = Systemic Arterial Hypertension;
AMI = Acute Myocardial Infarction; NYHA = New York Heart Association; CPB =
cardiopulmonary bypass; MV = Mechanical ventilation
The average walking speed in the
slow group was 0.6 m/s, while in the non-slow group it was 1.2 m/s. Twenty
patients (40%) were readmitted to the hospital during the observation period of
6 months. Of those, 14 (70%) were slow walkers, as defined by a gait speed of
less than 1.0 m/s, and 6 (30%) were non-slow walkers. The 6 months rate of
readmission was 58% (14/24; 95% CI 49% to 80%) among slow walkers and 17%
(6/36; 95% CI 13% to 46%) among non-slow walkers (p = 0.002). In univariate
analysis, gait speed, treated as a continuous variable, was associated with the
primary outcome (HR 0.6; 95% CI 0.2 to 0.9), while age, gender, BMI, MV and CPB
time were not (table II). In the multivariate model including age, gender, BMI,
MV and CPB time, gait speed remained the only variable associated with
readmission (multivariate HR: 0.5, 95% CI 0.1 to 0.7 p = 0.02 (Table II).
Table II - Univariate and multivariate
associations between predictive variables and readmission
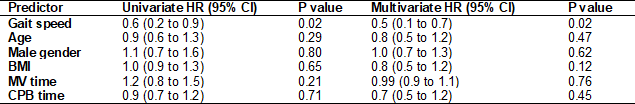
BMI = Body Mass Index; MV =
Mechanical Ventilation; CPB = Cardiopulmonary bypass
Discussion
Based on the results of this
prospective cohort study, gait speed was associated with hospital readmission
of patients undergoing to coronary artery bypass grafting. Walking more slowly
(< 1 m/s) was associated with hospital readmission, but variables such as
age, male gender, BMI, MV and CPB team were not related to the outcome in six
months.
Previous studies suggest that gait
speed is an independent variable for mortality and hospital readmission in
survivors of acute hypercapnic respiratory failure and heart failure [11,12].
Being an extremely simple and feasible test for the application of the
practice, we suggest its adoption by hospital services aiming at reducing hospital
readmissions, thus minimizing costs, improving the survival and quality of life
of these patients.
Afilalo et
al. [13] demonstrated that patients with low gait speed in the preoperative
period have a higher rate of morbidity and mortality during the ICU stay. They
also found that factors such as female gender and diabetics made up the slow
speed group. In our study, we did not find any difference regarding gender, age
or comorbidities, which may be associated with a smaller sample size in the present
study. This result only reinforces the need to stratify patients with a higher
risk of complications or hospital readmission, and gait speed is a useful tool.
In this rationale, Sawatzky et al. [14] found that the application of a
program in the preoperative period can increase gait speed, with this effect
remaining for up to three months after the procedure. On the other hand, Cerqueira et al. [15] did not demonstrate any impact
when applied to neuromuscular electrical stimulation in the postoperative
period.
A possible explanation for reducing
gait speed and increasing the risk of hospital readmission is fragility. It is
considered a multidimensional syndrome resulting from the reduction of
physiological reserves and an increase in physical and functional decline when
exposed to external stressors [16]. After cardiac surgery, factors such as
cardiopulmonary bypass, surgical incision, pleurotomy and duration of
mechanical ventilation generate pulmonary dysfunction and decrease in
physiological reserves [17]. Bed restriction time contributes to physical and
functional decline [18,19]. Our group demonstrated that after myocardial
revascularization it generates a decrease in functional capacity, observed
through the six-minute walk test [20]. We found that performing inspiratory
muscle training helps to minimize this decline and improve clinical outcomes
such as length of hospital stay [20,21].
Lal et al. [22] demonstrated
that the frailty assessed using the Edmonton scale is a predictor for the length
of hospital stay and risk of readmission up to twelve months in elderly
patients undergoing cardiac surgery. The combination of frailty assessment with
gait speed will give the therapist fundamental information for the organization
of an intervention protocol.
In Castro et al. [23], it
was evidenced that the greater distance covered in the 6MWT was associated with
a shorter hospital stay, as a quick recovery after the surgical procedure
allows walking autonomy that allows the transfer of this patient earlier for
rehabilitation, and consequently reduce hospitalization time. In the study by Aikawa et al. [24], they say that immediate
post-surgical rehabilitation can be a means that enables the more agile
development and recovery of these patients and found in the 6MWT that there was
a significant increase in the distance covered and gait speed of these
patients. Thus, comparing the studies presented, it can be understood that an
early rehabilitation of patients after CABG is linked to a shorter hospital
stay, consequently generating an improvement in gait speed when evaluated by
the 6MWT.
According to Oliveira et al.
[25], it was evaluated that the CPB time has minimal influence on the patient’s
ability to walk, the research shows that despite the occurrence of muscle
inefficiency, generating a loss of postoperative strength, it does not
interfere in the gait of patients themselves. Reinforcing with the results of
this study, we analyzed that the CPB time had no correlation with the patients'
gait, as it statistically had no influence.
Borges et al. [26] showed
that patients undergoing cardiac surgery suffer adverse risks during
hospitalization in the postoperative period, when they become more fragile due
to some physiological changes that occur during the intervention, such as:
motor disabilities and physical limitations that can be prolonged, and,
consequently, which may lead to future readmissions, the author also identified
a vicious cycle of slow gait after surgery. The results of this study were
similar to ours, in which it showed that patients undergoing CABG showed a
decrease in gait speed due to several associated and already mentioned factors,
and that it may possibly be associated with the risk of a hospital readmission.
The limitations of this study
include the sample calculation, limiting the extent of its findings, absence of
information on pulmonary function, which may have an influence on the
performance of the gait speed test and the lack of a spirometric
test.
Conclusion
Our data suggest that gait speed is
associated with hospital readmission in patients undergoing to coronary artery
bypass grafting.
Potential conflict of
interest
No conflict of interest for this
article have been reported
Financing source
There were no external sources of
funding for this study
Authors’ contribution
Conception and research
design: Cordeiro ALL, Santos AO, Soares TJ; Data collection:
Cordeiro ALL, Santos AO, Soares TJ; Data analysis and interpretation:
Cordeiro ALL, Santos AO, Soares TJ; Writing of the manuscript: Cordeiro
ALL, Santos AO, Soares TJ; Critical revision of the manuscript for important
intellectual content: Cordeiro ALL, Guimarães AR
References
- Cordeiro
ALL, Brito AAOR, Santana NMA, Silva INMS, Nogueira SCO, Guimarães ARF, et al. Analysis
of functional pre degree of independence and tall in ICU patients undergoing
cardiac surgery. Revista
Pesquisa em Fisioterapia 2015;5(1):21-27. doi: 10.17267%2F2238-2704rpf.v5i1.574 [Crossref]
- Fonseca L, Vieira FN, Azzolin KO. Fatores associados ao tempo de ventilação mecânica no pós-operatório de cirurgia cardíaca. Rev Gaúcha Enferm 2014;35(2):67-72. doi: 10.1590/1983-1447.2014.02.44697 [Crossref]
- Jesus FS, Paim DM, Brito JO, Barros IA, Nogueira TB, Martinez BP, et al. Mobility decline in patients hospitalized in an intensive care unit. Rev Bras Ter Intensiva 2016;28(2):114-9. doi: 10.5935/0103-507X.20160025 [Crossref]
- Karege G, Zekry D, Allali G, Adler D, Marti C. Gait speed is associated with death or readmission among patients surviving acute hypercapnic respiratory failure. BMJ Open Respir Res 2020;7(1):e000542. doi: 10.1136/bmjresp-2019-000542 [Crossref]
- Nakamura T, Kamiya K, Hamazaki N, Matsuzawa R, Nozaki K, Ichihawa T, et al. Quadriceps strength and mortality in older patients with heart failure. Can J Cardiol 2020;S0828-282X(20)30582-1. doi: 10.1016/j.cjca.2020.06.019 [Crossref]
- Fritz S, Lusardi M. White paper: "walking speed: the sixth vital sign". J Geriatr Phys Ther 2009;32(2):46-9. doi: 10.1519/00139143-200932020-00002 [Crossref]
- Studenski S, Perera S, Patel K, Rosano C, Faulkner K, Inzitari M, et al. Gait speed and survival in older adults. JAMA 2011;305:50-8. doi: 10.1001/jama.2010.1923 [Crossref]
- Kahlon S, Pederson J, Majumdar SR, Belga S, Lau D, Fradette M, et al. Association between frailty and 30-day outcomes after discharge from hospital. CMAJ 2015;187:799-804. doi: 10.1503/cmaj.150100 [Crossref]
- Jones SE, Maddocks M, Kon SSC, et al. Sarcopenia in COPD: prevalence, clinical correlates and response to pulmonary rehabilitation. Thorax 2015;70:213-8. doi: 10.1136/thoraxjnl-2014-206440 [Crossref]
- Odonkor CA, Schonberger RB, Dai F, Shelley KH, Silverman DG, Barash PG. New utility for an old tool: can a simple gait speed test predict ambulatory surgical discharge outcomes? Am J Phys Med Rehabil 2013;92(10):849-63. doi: 10.1097/PHM.0b013e3182a51ac5 [Crossref]
- Karege G, Zekry D, Allali G, Adler D, Marti C. Gait speed is associated with death or readmission among patients surviving acute hypercapnic respiratory failure. BMJ Open Respir Res 2020;7(1):e000542. doi: 10.1136/bmjresp-2019-000542 [Crossref]
- Reeves GR, Forman DE. Gait speed: stepping towards improved assessment of heart failure patients. JACC Heart Fail 2016;4(4):299-300. doi: 10.1016/j.jchf.2016.02.002 [Crossref]
- Afilalo J, Eisenberg MJ, Morin JF, Bergman H, Monette J, Noiseaux N, et al. Gait speed as an incremental predictor of mortality and major morbidity in elderly patients undergoing cardiac surgery. J Am Coll Cardiol 2010;56(20):1668-76. doi: 10.1016/j.jacc.2010.06.039 [Crossref]
- Sawatzky JA, Kehler DS, Ready AE, Lerner N, Boreskie S, Larmont D, et al. Prehabilitation program for elective coronary artery bypass graft surgery patients: a pilot randomized controlled study. Clin Rehabil 2014;28(7):648-57. doi: 10.1177/0269215513516475 [Crossref]
- Fontes Cerqueira TC, Cerqueira Neto ML, Cacau LAP, et al. Ambulation capacity and functional outcome in patients undergoing neuromuscular electrical stimulation after cardiac valve surgery: A randomized clinical trial. Medicine (Baltimore) 2018;97(46):e13012. doi: 10.1097/MD.0000000000013012 [Crossref]
- Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet 2013;381:752-62. doi: 10.1016/S0140-6736(12)62167-9 [Crossref]
- Guizilini S, Viceconte M, Esperança GT, Bolzan DW, Vidotto M, Moreira RSL, et al. Pleural subxyphoid drain confers better pulmonary function and clinical outcomes in chronic obstructive pulmonary disease after off-pump coronary artery bypass grafting: a randomized controlled trial. Rev Bras Cir Cardiovasc 2014;29(4):588-94. doi: 10.5935/1678-9741.20140047 [Crossref]
- Patel BK, Hall JB. Perioperative physiotherapy. Curr Opin Anesthesiol
[Internet] 2013 [cited 2022 June 1];26(2):152-6. Available from:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6015730/
- França EET, Ferrari F, Fernandes P, Cavalcanti R, Duarte A, Martinez BP, et al. Fisioterapia em pacientes críticos adultos: recomendações do Departamento de Fisioterapia da Associação de Medicina Intensiva Brasileira. Rev Bras Ter Intensiva 2012;24(1):6-22. doi: 10.1590/S0103-507X2012000100003 [Crossref]
- Cordeiro ALL, Mascarenhas HC, Landerson L, Araújo JS, Borges DL, Melo TA, et al. Inspiratory muscle training based on anaerobic threshold on the functional capacity of patients after coronary artery bypass grafting: clinical trial. Braz J Cardiovasc Surg 2020. doi: 10.21470/1678-9741-2019-0448 [Crossref]
- Cordeiro AL, Melo TA, Neves D, Luna J, Esquivel MS, Guimarães ARF, et al. Inspiratory muscle training and functional capacity in patients undergoing cardiac surgery. Braz J Cardiovasc Surg 2016;31(2):140-4. doi: 10.5935/1678-9741.20160035 [Crossref]
- Lal S, Gray A, Kim E, Bolzan DW, Vidotto M, Moreira RSL, et al. Frailty in elderly patients undergoing cardiac surgery increases hospital stay and 12-month readmission rate. Heart Lung Circ 2019;S1443-9506(19)31488-X. doi: 10.1016/j.hlc.2019.10.007 [Crossref]
- Castro VMN, Vitorino PVO. Revisão integrativa sobre a fisioterapia na reabilitação cardiovascular no Brasil. Revista de Ciências Ambientais e Saúde 2013;40(4):479-87. doi: 10.18224/est.v40i4.3053 [Crossref]
- Aikawa P, Cintra ARS, Oliveira AS, Silva CTM, Pierucci JD, Afonso MS, et al. Reabilitação cardíaca em pacientes submetidos à cirurgia de revascularização do miocárdio. Rev Bras Med Esporte 2014;20(1). doi: 10.1590/S1517-86922014000100011 [Crossref]
- Oliveira GU, Carvalho VO, Cacau LPA, Araújo AAF, Cerqueira MLN, Silva WMJS, et al. Determinants of distance walked during the six-minute walk test in patients undergoing cardiac surgery at hospital discharge. J Cardiothorac Surg 2014;9:95. doi: 10.1186/1749-8090-9-95 [Crossref]
- Borges DL, Silva MG, Silva LN, Fortes JV, Costa ET, Assunção RP, et al. Effects of aerobic exercise applied early after coronary artery bypass grafting on pulmonary function, respiratory muscle strength and functional capacity: a randomized controlled trial. J PhysAct Health 2016;13(9):946-51. doi: 10.1123/jpah.2015-0614 [Crossref]