Rev Bras Fisiol Exerc 2022;21(3):204-16
doi: 10.33233/rbfex.v21i3.5282
REVIEW
Diaphragmatic ultrasonography as a predictor of ventilatory weaning: a
systematic review
Ultrassonografia
diafragmática como preditora de desmame ventilatório: uma revisão sistemática
André Luiz Lisboa Cordeiro1,2,
Lucas Oliveira Soares2, Késsia Morgana Vital
Oliveira2, Amanda Maria Garcez de Oliveira de Jesus2
1Escola Bahiana
de Medicina e Saúde Pública, Salvador, BA, Brazil
2Centro Universitário Nobre, Feira de
Santana, BA, Brazil
Received: September
12, 2022; Accepted: September
13, 2022.
Correspondence: André Luiz Lisboa Cordeiro, Faculdade
Nobre, Avenida Maria Quitéria, Kalilândia, Feira de
Santana, BA
André Luiz
Lisboa Cordeiro: andrelisboacordeiro@gmail.com
Lucas
Oliveira Soares: lucassoaresft@gmail.com
Késsia Morgana Vital Oliveira:
kessiamorganav@gmail.com
Amanda
Maria Garcez de Oliveira de Jesus: amanda_garcez21@outlook.com
Abstract
Objective: To review the evidence on diaphragmatic
ultrasonography as a predictor of success in ventilatory weaning, using the
PICO methodology and keywords: Ultrasound, Diagnostic imaging, Diaphragm,
Weaning, Intensive Care Unit, Artificial Respiration, Mechanical Ventilation,
Ventilator Weaning. Methods: Published cohort studies were used without
language and year restrictions that addressed the use of ultrasound to predict
success in weaning and ventilatory extubation. Studies
with patients under 18 years of age, case reports, literature reviews, results
that do not bring a cutoff value for thickness and diaphragmatic excursion and
the definition of failure in the weaning and extubation
process were excluded. Results: 459 were found, and after exclusion due
to duplication and reading of titles and abstract, only 11 were selected by the
inclusion criteria. The samples ranged from 34 to 193 individuals. Conclusion:
We can evidence that the use of USG to assess the thickness and excursion of
the diaphragm in patients undergoing invasive ventilatory support is effective
in predicting success in the weaning and extubation
process. The Diaphragmatic Ultrasonography has great applicability to assess
the ability to predict success or failure in removing invasive ventilatory
support.
Keywords: diaphragmatic ultrasound; mechanical ventilation;
weaning; airway extubation.
Resumo
Objetivo: Revisar as evidências sobre a
ultrassonografia diafragmática como preditor de sucesso no desmame ventilatório,
usando a metodologia PICO e palavras-chave: Ultrassom, Diagnóstico por imagem,
Diafragma, Desmame, Unidade de Terapia Intensiva, Respiração Artificial,
Ventilação Mecânica, Desmame do Ventilador. Métodos: Estudos de coorte
publicados foram usados sem restrições de idioma e ano que abordaram o uso de
ultrassom para prever o sucesso no desmame e extubação ventilatória. Foram
excluídos estudos com pacientes menores de 18 anos, relatos de casos, revisões
de literatura, resultados que não trouxessem valor de corte para espessura e
excursão diafragmática e definição de falha no processo de desmame e extubação.
Resultados: Foram encontrados 459 estudos; após exclusão por duplicação
e leitura de títulos e resumo, apenas 11 foram selecionados pelos critérios de
inclusão. As amostras variaram de 34 a 193 indivíduos. Conclusão:
Podemos evidenciar que o uso da USG para avaliar a espessura e excursão do
diafragma em pacientes submetidos a suporte ventilatório invasivo é eficaz em
predizer o sucesso no processo de desmame e extubação. A ultrassonografia
diafragmática tem grande aplicabilidade para avaliar a capacidade de predizer
sucesso ou falha na remoção do suporte ventilatório invasivo.
Palavras-chave: ultrassom diafragmático; ventilação
mecânica; desmame, extubação.
Introduction
One of the main causes of referral to the intensive
care unit (ICU) is the need for invasive mechanical ventilation (IMV) [1,2].
Patients need IMV when they lose the ability to perform spontaneous ventilation
due to respiratory failure or are unable to protect the airways by lowering the
level of consciousness [3,4].
IMV can cause deleterious effects for the patient and
diaphragmatic dysfunction (DD) is among the most important, causing weakness
and atrophy due to disuse, prolonging the time spent on mechanical ventilation,
risk of tracheostomy, complications up to one year after discharge from the ICU
and impact on the mortality rate [3,4,5,6,7].
Weaning is a transitory process between the support of
mechanical ventilation and spontaneous ventilation; it is also classified in
categories according to the time of MV. Within intensive care units, and
especially in patients on invasive ventilatory support, weaning becomes one of
the main objectives of the multidisciplinary team. There are several causes for
failure in the weaning process, in this scenario it is important to use
accurate methods to predict success and avoid complications for the patient
[8].
Several diagnostic techniques are used to assess
diaphragmatic functions [9,10]. Among them, diaphragmatic ultrasonography (USG)
has become increasingly used, proving to be very important in the intensive
care environment and in the assessment of the critical patient. This method is
accessible and can evaluate in real time the function and structure of the
diaphragm, being able to detect changes that may difficult the weaning
[1,3,4,11,12].
Parameters such as excursion and thickness are some of
the findings that guide us to identify atrophy, paralysis and other
diaphragmatic dysfunctions [1]. In this sense, Carrie et al. [13]
assessed the performance of diaphragmatic USG to predict failure in weaning in
patients under IMV using the maximum diaphragmatic excursion measurement,
confirmed the ventilator-induced diaphragmatic dysfunction (VIDD) and suggests
that the diaphragm is very sensitive to the absence of activity.
Llamas-Álvarez et al. [14] performed a review
and suggest that diaphragmatic USG is a predictor in ventilatory weaning in
critically ill patients. Therefore, the objective of this study was to review
the evidence on diaphragmatic ultrasonography as a predictor of success in
ventilatory weaning.
Methods
This is a systematic review and the guiding question
of this study was: "What is the current evidence on diaphragmatic
ultrasonography to predict success in weaning?"
The following databases were systematically searched: Pubmed, Scielo (Scientific
Electronic Library Online), Lilacs (Latin American and Caribbean Literature in
Health Sciences), VHL (Virtual Health Library) and Science Direct. The keywords
used were: Ultrasound, Diagnostic imaging, Diaphragm, Weaning, Intensive Care
Unit, Artificial Respiration, Mechanical Ventilation, Ventilator Weaning;
synonyms and related words added by the Boolean operators "AND" and
"OR", according to the Health Sciences Descriptors (DeCS). The survey was conducted in April 2020.
Eligibility criteria
We selected cohort studies without language and year
restrictions which used the ultrasound to predict success in weaning and
ventilatory extubation. Studies with patients under
18 years of age, case reports, literature reviews, results that do not bring a
cutoff value for thickness and diaphragmatic excursion and the definition of
failure in the weaning and extubation process were
excluded and due to difficulty in translation we also excluded articles in
Chinese.
Data extraction
The articles collected through the searches in the
databases were selected by tracking the titles (first stage), abstracts (second
stage) and complete reading (third stage). Then, an exploratory reading of the
selected studies was carried out and, later, selective and analytical reading.
The data extracted from the articles were systematized: authors, title,
journal, year, summary and conclusions, in order to enable the obtaining of
relevant information for the research.
The selection process, data extraction from articles
and identification of methodological aspects was carried out by two independent
reviewers. When there was any disagreement between them, the reviewers read the
entire article again for reassessment. If the disagreement persists, a third
independent reviewer assessed and made the final decision. The research
followed the items of the PRISMA [15] protocol for systematic reviews.
Results
Four hundred and fifty-nine articles were found, and
after exclusion due to duplication and reading of titles and abstracts, only
eleven were selected according to the inclusion criteria. Those studies that
did not make clear the values found with ultrasound to predict success in
weaning / extubation (59) or articles with a
literature review design or case reports (54) were also excluded from the
study. The flowchart in Figure 1 shows all the criteria and databases used to
select the articles.
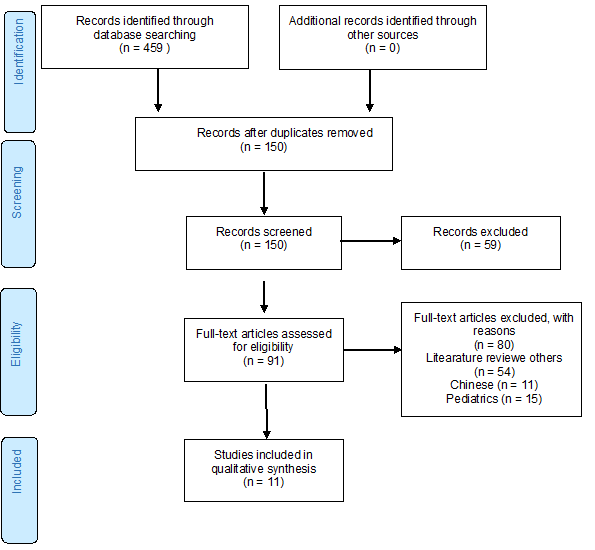
Figure 1 - Flowchart demonstrating how the studies of
cohorts that used ultrasound to assess diaphragmatic thickness and excursion
were obtained
Table I shows the general characteristics of the other
studies. We can observe that some studies were carried out in more than one
unit, among which are wards, general ICU and specialized ICU.
Table I - General characteristics of the studies
It is possible to verify that the authors used very
similar criteria to determine the failure in the weaning / extubation
process, showing that they all started from the same point to define the
failure of the removal of artificial ventilation, such as reconnection in the
mechanical ventilator, reintubation, use of NIV and tracheostomy within 48
hours after extubation. Table II shows the
definitions of each author for failure in weaning / extubation.
Table II - Characteristics of the included studies and
definition of failure in weaning / extubation
The data presented below in Table III show the
objectives and results found in each study using ultrasound to assess thickness
and diaphragmatic excursion as a predictor of success in the weaning / extubation process. The authors identified that patients
with thickness values < 1 cm, 20 < 2.20 + 0.69 mm [21] and < 10 mm
[24] were associated with complications, prolonged MV and failure in weaning
and extubation. Yoo et
al. [26] found values of diaphragmatic thickness < 4 cm and 1.53 cm
respectively are related to failure in weaning and extubation.
These low values were also related to prolonged weaning, increased length of
stay in the ICU, hospital mortality and after discharge from the unit.
Table III - General data from cohort studies using
diaphragmatic USG as a predictor of success in weaning and extubation
Discussion
Based on the findings of this review, we can evidence
that the use of diaphragmatic ultrasound to assess the thickness and excursion
of the diaphragm in patients undergoing invasive ventilatory support is
effective in predicting success in the weaning and extubation
process.
It is essential to evaluate and identify patients able
to remove invasive ventilatory support. Some studies indicate that failure in
this process increases the chance of mortality by 50%. Diaphragmatic USG is
able to identify the result of this process through anatomical and
biomechanical measurements such as thickness and its excursion during normal
operation, with the result of this assessment it is possible to develop
therapeutic strategies to minimize these risks.
After evaluating Tdi, Sklar et al. [16] found that patients with values < 2.3 mm were associated with prolonged weaning, longer
on invasive ventilatory support and had a significantly greater difference in
hospital mortality, especially after discharge from the ICU. It was identified
with the USG that the Tdi obtained on the beginning
of MV was independently associated with prolonged MV and higher mortality
regardless of the severity of the underlying disease [16].
Corroborating with Sklar
[16], Dres et al. [21] found that patients
with higher DTF and ED values proved to be efficient as a predictor
independently associated with failure in weaning and extubation.
They found that in an unelected population of mechanically ventilated patients
considered ready to perform an ERT, the prevalence of DD was twice as high as
the prevalence of ICU-AW, and that DD, not ICU-AW, influenced the outcome,
being present in almost all patients who had failed weaning. This study served
to highlight that DD should be the object of prevention and possible specific
interventions [21].
Khan et al. [22] defined an IRRS cutoff point
of 59 is 79% sensitive and 64% specific and 1.35 cm from DE, observed with
ultrasound, a sensitivity of 74% and specificity of 75% to predict success in
weaning, the greater the DE value the higher the success rate. In this study, they
observed that IRRS better predicts the outcome of weaning, but that when
associating the ND to the IRRS they are optimized in the classification of the
outcome of weaning in guaranteeing extubation and
prevention of reintubation [22].
In the intensive care setting, it becomes necessary to
identify patients who are able to leave invasive ventilatory support and USG
for diagnosing the patient's condition in real time, being low-cost,
non-invasive and not emitting radiation is a useful tool and essential to
evaluate these patients, its applicability is increasingly evident.
When using USG to assess DTF and DE in patients with
abdominal sepsis Eltrabili et al. [17] found
some results similar to Khan et al. [22], and they noticed a significant
difference in patients who failed and those who were successful. The
diaphragmatic parameters obtained with the USG, a DTF of 30.7%, with
sensitivity of 94.1% and specificity of 100% and DE of 10.4 mm, with a
sensitivity of 94% and specificity of 84% were values to predict successful
withdrawal of mechanical ventilation. They observed that the best cutoff value
to predict the success of weaning was 30.7%, because in other studies it varies
from 20 to 36%, depending on the ventilatory support offered during the
measurement [17].
ED has become a very relevant variable for the
assessment of extubation. With that in mind, Zhang et
al. [19] assessed DE with USG and found that patients who had extubation success had a higher value compared to those who
failed, this value was significantly statistical. In the study, a cutoff value
of DE of 1.72 cm was associated with success in extubation
and observed that the combination of DE 30 and ΔDE
30-5 was more accurate in predicting extubation. Even
if patients are successful in the ERT, they are still at risk of failing extubation, further proving the importance of looking for
another indicator to predict the outcome of extubation
and improve the survival of patients admitted to the ICU [19].
Many authors report the importance of an accurate
evaluation of the diaphragm, especially of DE, which often appears as the main
variable to be analyzed. Palkar et al. [20]
were emphatic and said that DE is an imperfect predictor. Although the
successful extubation group was significantly larger
than the ones that failed, many complexity factors can interfere with the extubation result. They also observed that when measured
between A / C and TRE they obtained a better result than only during the TRE.
Soliman et al. [23] found in patients with
successful weaning a DTF significantly higher than in the group that failed,
with a cutoff value ≥ 29.5, which can predict the success of weaning with
a sensitivity of 88.0% and specificity of 80.0 %. The authors conclude the
study by saying that they support the use of USG to predict weaning failure, to
assess the lung and diaphragm, helping to understand the pathophysiological
effects of weaning and to optimize the clinical condition, increasing the
chances of successful weaning [23].
Using USG to assess the diaphragm of the elderly and
the relationship between diaphragmatic dystrophy and weaning, Huang et al.
[24] defined a cutoff value below 10 mm and used the M mode. They observed a
75% prevalence of DD in ventilated elderly people mechanically and 70% of
weaning failure, having complex factors as reasons behind these weaning
failures [24].
With similar results, Pirompanich
and Romsaiyt [25] found a higher DTF in the
successful group compared to the group that failed. The authors suggest that
the right DTF greater than or equal to 26% is more accurate to predict success
in weaning, being the best and most efficient predictor of success in
ventilatory weaning. The reason the right side is more effective than the left
can be a higher lung volume [25].
According to Yoo et al.
[26] DE values are higher than Tdi in predicting extubation success, suggesting that DE may be more accurate
than Tdi to predict weaning success. It is noteworthy
that the values of the analyzed variables differ between studies, our findings
demonstrate that regardless of the cutoff value established by the authors, the
most relevant to be analyzed is the amount of loss of DTF, Tdi
and DE from the beginning of mechanical ventilation.
Conclusion
Based on the data found, we can conclude that
diaphragmatic ultrasonography has great applicability to assess the ability to
predict success or failure in removing invasive ventilatory support. Values of
thickened fraction, excursion and diaphragmatic thickness differ between
studies according to the authors and the population studied, but the main point
of this review is to show that the loss of diaphragmatic function revealed by a
decrease in the thickening, excursion and thickness fraction diaphragm in
mechanically ventilated patients can predict success or failure in the weaning
and extubation process.
Potential conflict of interest
No conflicts of interests have been reported for this
article.
Funding source
The present study was carried out without funding.
Authors’ contributions
Literature search, Data collection, Study design,
Manuscript preparation and Review of manuscript:
Cordeiro ALL, Soares LO, Oliveira KMV, Jesus AMGO
References
- Varón-Vega F, Hernández A, López M, Cáceres E, Giraldo-Cadavid LF,
Uribe-Hernandez AM, Crevoisier S. Usefulness of
diaphragmatic ultrasound in predicting extubation
success. Med Intensiva (Engl
Ed) 2021;45(4):226-33. doi: 10.1016/j.medin.2019.10.007 [Crossref]
- Girard TD, Alhazzani W, Kress JP, Ouellette DR, Schmidt GA, Truwit JD, et al. An Official American Thoracic Society/American College of Chest Physicians Clinical Practice Guideline: Liberation from mechanical ventilation in critically ill adult rehabilitation protocols, ventilator liberation protocols, and cuff leak tests. Am J Respir Crit Care Med 2017;195:120-33. doi: 10.1164/rccm.201610-2075ST [Crossref]
- Grasse A, Ferlicca D, Lupieri E, Calcinati S, Francesconi S, Sala V, et al. Assisted mechanical ventilation promotes recovery of diaphragmatic thickness in critically ill patients: a prospective observational study. Critical Care 2020;24:85. doi: 10.1186/s13054-020-2761-6 [Crossref]
- Goligher EC, Dres M, Fan E, Rubenfeld GD, Scales DC, Herridge MS, et al. Mechanical ventilation-induced diaphragm atrophy strongly impacts clinical outcomes. Am J Respir Crit Care Med 2018;197(2):204-13. doi: 10.1164/rccm.201703-0536OC [Crossref]
- Sklar MC, Dres M, Fan E, Rubenfeld GD, Scales DC, Herridge MS, et al. Association of low baseline diaphragm muscle mass with prolonged mechanical ventilation and mortality among critically ill adults. JAMA Network Open 2020;3(2):e1921520. doi: 10.1001/jamanetworkopen.2019.21520 [Crossref]
- Dres M, Dubé B-P, Mayaux J, Delemazure J, Reuter D, Brochard L, et al. Coexistence and impact of limb muscle and diaphragm weakness at time of liberation from mechanical ventilation in medical intensive care unit patients. Am J Respir Crit Care Med 2017;195(1):57-66. doi: 10.1164/rccm.201602-0367OC [Crossref]
- Medrinal C, Prieur G, Frenoy E, Quesada AR, Poncet A, Bonnevie T, et al. Respiratory weakness after mechanical ventilation is associated with one-year mortality - a prospective study. Crit Care 2016;20(1):231. doi: 10.1186/s13054-016-1418-y [Crossref]
- Geiseler J, Kelbe C. Weaning from mechanical ventilation. Weaning categories and weaning concepts. Med Klin Intensivmed Notfmed 2016;111:208-14. doi: 10.1007/s00063-016-0147-y [Crossref]
- Goligher EC, Fan E, Herridge MS, Murray A, Vorona S, Brace D, et al. Evolution of diaphragm thickness during mechanical ventilation. Impact of inspiratory effort. Am J Respir Crit Care Med 2015;192(9):1080. doi: 10.1164/rccm.201503-0620OC [Crossref]
- Palkar A, Mayo P, Singh K, Koenig S, Narasimhan M, Singh A, et al. Serial diaphragm ultrasonography to predict successful discontinuation of mechanical ventilation. Lung 2018;196:363-8. doi: 10.1007/s00408-018-0106-x [Crossref]
- Öztürk E, Tanıdır İC, Yıldız O, Yükçü B, Ergün S, Haydın S, et al. Ultrasonographic postoperative evaluation of diaphragm function of patients with congenital heart defects. Turk Gogus Kalp Dama 2020;28(1):70-5. doi: 10.5606/tgkdc.dergisi.2020.18458 [Crossref]
- Abbas A, Embarak S, Walaa M, Lutfy SM. Role of diaphragmatic rapid shallow breathing index in predicting weaning outcome in patients with acute exacerbation of COPD. Int J COPD 2018;13:1655-61. doi: 10.2147/COPD.S161691 [Crossref]
- Carrie C, Gisbert-Morae C, Bonnardel E, Gauche B, Matthieu B, Vargas F, et al. Ultrasonographic diaphragmatic excursion is inaccurate and not better than the MRC score for predicting weaning-failure in mechanically ventilated patients. Anaesth Crit Care Pain Med 2016:1-27. doi: 10.1016/j.accpm.2016.05.009 [Crossref]
- Llamas-Álvarez AM, Tenza-Lozano EM, Latour-Pérez J. Diaphragm and lung ultrasound to predict weaning outcome: systematic review and meta-analysis. Chest 2017;52(6):1140-50. doi: 10.1016/j.chest.2017.08.028 [Crossref]
- Moher D, Liberati A, Tetzlaff
J, Altman DG, The PRISMA Group. Preferred Reporting Items for Systematic
Reviews and Meta-Analyses: The PRISMA Statement. PLoS
Med.2009;6(7):e1000097
- Sklar MC, Dres M, Fan E, Rubenfeld GD, Scales DC, Herridge MS, et al. Association of low baseline diaphragm muscle mass with prolonged mechanical ventilation and mortality among critically Ill Adults. JAMA Network Open. 2020;3(2):e1921520. doi: 10.1001/jamanetworkopen.2019.21520 [Crossref]
- Viver E, Muller M, Putegnat Jean-Baptiste, Steyer J, Barrau S, Boissier F, et al. Inability of diaphragm ultrasound to predict extubation failure a multicenter study. Chest 2019;155(6):1131-9. doi: 10.1016/j.chest.2019.03.004 [Crossref]
- Eltrabili HH, Hasanin AM, Soliman MS, Lofty AM, Hamimy WI, Mukhtar AM. Evaluation of diaphragmatic ultrasound indices as predictors of successful liberation from mechanical ventilation in subjects with abdominal sepsis. Respir Care 2019;64(5):564-9. doi: 10.4187/respcare.06391 [Crossref]
- Zhang X, Yuan J, Zhan Y, Wu J, Liu B, Zhand P, Yu T, et al. Evaluation of diaphragm ultrasound in predicting extubation outcome in mechanically ventilated patients with COPD. Ir J Med Sci 2020;189(2):661-8. doi: 10.1007/s11845-019-02117-1 [Crossref]
- Palkar A, Mayo P, Singh K, Koenig S, Narasimhan, Singh A, et al. Serial diaphragm ultrasonography to predict successful discontinuation of mechanical ventilation. Lung 2018;196(3):363-8. doi: 10.1007/s00408-018-0106-x [Crossref]
- Dres M, Dube Bruno-Pierre, Mayaux J, Delemazure J, Reuter D, Brochard L, et al. Coexistence and impact of limb muscle and diaphragm weakness at time of liberation from mechanical ventilation in medical intensive care unit patients. Am J Respir Crit Care Med 2017;195(1):57-66. doi: 10.1164/rccm.201602-0367OC [Crossref]
- Khan M, Munawar K, Hussain S, Qadeer A, Saeed ML, Shad ZS, et al. Comparing ultrasound-based diaphragmatic excursion with rapid shallow breathing index as a weaning predictor. Cureus 2018;10(12):3710. doi: 10.7759/cureus.3710 [Crossref]
- Soliman SB, Ragab F, Soliman RA, Gaber A, Kamal A. Chest Ultrasound in predication of weaning failure. Open Access Maced J Med Sci 2019;7(7):1143-47. doi: 10.3889/oamjms.2019.277 [Crossref]
- Huang D, Ma H, Zhong W, Wang X, Wu Y, Qin T, et al. Using M-mode ultrasonography to assess diaphragm dysfunction and predict the success of mechanical ventilation weaning in elderly patients. J Thorac Dis 2017;9(9):3177-86. doi: 10.21037/jtd.2017.08.16 [Crossref]
- Pirompanich P, Romsaiyut S. Use of diaphragm thickening fraction combined with rapid shallow breathing index for predicting success of weaning from mechanical ventilator in medical patients. J Intensive Care 2018;6:6. https://10.1186/s40560-018-0277-9 [Crossref]
- Yoo Jung-Wan, Lee SJ, Lee JD, Kim HC. Comparison of clinical utility between diaphragm excursion and thickening change using ultrasonography to predict extubation success. Korean J Intern Med 2018;33:331-9. doi: 10.3904/kjim.2016.152.e1 [Crossref]