Rev Bras Fisiol Exerc. 2024;23:e235376
doi: 10.33233/rbfex.v23i1.5376
ORIGINAL ARTICLE
Peripheral muscular strength
and functionality as predictors of extubation success
after myocardial revascularization
Força
muscular
periférica e funcionalidade como preditores de sucesso para
extubação após revascularização do
miocárdio
André Luiz Lisboa Cordeiro¹,
Hayssa de Cássia Mascarenhas1, Lucas
Oliveira Soares1, Vitória de Oliveira Pimentel1, Layla Souza e Souza1,
Arthur Marchesini1, Gabriel Velloso Dantas Batista Andrade Ferreira1,
André Raimundo Guimarães2
1Centro Universitário Nobre, Feira de
Santana, BA, Brazil
2Instituto Nobre de Cardiologia, Feira de
Santana, BA, Brazil
Received: January 3,
2023; Accepted: December
15, 2023.
Correspondence: André Luiz Lisboa Cordeiro, andrelisboacordeiro@gmail.com
How to
cite
Cordeiro ALL,
Mascarenhas HC, Soares LO, Pimentel VO, Souza e Souza L,
Marchesini A, Ferreira GVDBA, Guimarães AR. Peripheral
muscular strength and functionality as predictors of extubation success after myocadial revascularization. Rev Bras
Fisiol Exerc. 2024;e235376. doi: 10.33233/rbfex.v23i1.5376
Abstract
Introduction: Maximum inspiratory pressure (MIP) and the rapid
and shallow breathing index are predictors
for successful extubation. Peripheral muscle strength and functionality
appear as possible predictors of success
for extubation in other patient profiles, however, there is little
evidence in patients undergoing to Coronary
Artery Bypass Grafting (CABG). Objective:
To assess peripheral muscle strength and functionality
as predictors of success for extubation in patients undergoing to CABG. Methods: Prospective cohort study. At the time of hospital admission, patients were assessed
for MIP, maximum expiratory
pressure (MEP), Medical Research
Council (MRC), peak of expiratory flow
(PEF) and Functional
Independence Measure (FIM). Patients
were divided into two groups:
Success Group (SG), which remained on spontaneous ventilation for more than 48
hours, and failure group (FG) that required invasive support in less than 48 hours. We compared the influence
of muscle strength, cough and functionality variables between these groups. Results:
74 patients, Success Group (n = 59) and Failure Group (n = 15), were evaluated. The CI 95% was -1 (-5.33 to 3.33) in MIP, 4
(2.14 to 5.86) in MEP, 13 (-35.31 to
61.31) in PEF, 7 (6.27 to 7.73) in the MRC and 9 (8.08 to 9.92) in the FIM. Conclusion: Peripheral, expiratory muscle strength and functionality
demonstrated a statistically
significant influence on the success
of extubation in patients after CABG.
Keywords: airway extubation; thoracic surgery; muscle strength
Resumo
Introdução: A pressão inspiratória máxima (PImáx) e o índice de respiração rápida e superficial são
preditores de extubação bem-sucedida. A força muscular periférica e a
funcionalidade aparecem como possíveis preditores do sucesso da extubação em
outros perfis de pacientes, mas há poucas evidências em pacientes submetidos à
cirurgia de revascularização do miocárdio (RM). Objetivo: Avaliar a
força muscular periférica e a funcionalidade como preditores do sucesso da
extubação em pacientes submetidos à cirurgia de revascularização do miocárdio. Métodos:
Estudo de coorte prospectivo. No momento da admissão hospitalar, os pacientes
foram avaliados quanto à PImáx, pressão
expiratória máxima (PEmáx), Medical Research Council (MRC), pico de
fluxo expiratório (PFE) e Medida de Independência Funcional (MIF). Os pacientes
foram divididos em dois grupos: Grupo Sucesso (GS), que permaneceu em
ventilação espontânea por mais de 48 horas, e grupo fracasso (GF), que
necessitou de suporte invasivo em menos de 48 horas. Comparamos a influência
das variáveis de força muscular, tosse e funcionalidade entre esses grupos. Resultados:
Foram avaliados 74 pacientes, Grupo Sucesso (n = 59) e Grupo Falha (n = 15). O
IC 95% foi de -1 (-5,33 a 3,33) na PImáx,
4 (2,14 a 5,86) na PEmáx, 13 (-35,31 a
61,31) no PFE, 7 (6,27 a 7,73) na MRC e 9 (8,08 a 9,92) na MIF. Conclusão: A
força muscular periférica, expiratória e a funcionalidade demonstraram uma
influência estatisticamente significativa no sucesso da extubação em pacientes
após a cirurgia de revascularização do miocárdio.
Palavras-chave: extubação das vias aéreas; cirurgia
torácica; força muscular
Introduction
Cardiac surgery, even though it is a complex procedure, is the most
used for treatment aimed at reducing
mortality and symptoms in patients with coronary artery
disease (CAD) [1]. Coronary
Artery Bypass Grafting (CABG) covers 54.1% of
cases and is the standard for patients with CAD [2].
Some complications can be caused after
the surgical procedure. During the use of cardiopulmonary bypass (CPB), an inflammatory response is produced in the systems that generates movement of fluids
from the intravascular space to the
interstitial space, with this there
is alteration in the blood fluid,
injury or even myocardial cell necrosis, pulmonary dysfunction and, the longer
it is used the more physiological imbalance the patient
will have [3].
Other factors such as anesthesia, time and type of surgery,
intensity of manipulation of the surgery, sternotomy
and drains predispose to altered
pulmonary function, which may progress
to postoperative respiratory complications [4,5].
In addition to reduced pulmonary capacity, the surgical
procedure can develop loss of peripheral
muscle strength [6]. These complications may be associated
with the negative outcomes of the
surgery, one of which is
the increase in the time of Mechanical
Ventilation (MV), which consequently has an impact on
extubation.
Due to such complications, the Functional Independence Measure (FIM) scale is used to
assess these patients, which verifies the functional
restriction of patients and the
Medical Research Council
(MRC) score that analyzes peripheral muscle strength [7,8].
Early extubation has already been used
as a standard in several hospitals
and some benefits are reported, such as reduced length of stay in the
Intensive Care Unit (ICU) and decreased hospital stay [9,10].
It is necessary to
evaluate accurately to identify the
patient who is able to
be extubated. PImáx and the
rapid and shallow breathing index are predictors for successful extubation [11,12]. Peripheral muscle strength and functionality appear as possible predictors of success
for extubation in other patient profiles, however, there is little
evidence in patients undergoing to CABG. Therefore, the aim of this
study is verify whether there is an
association between functionality and muscle strength with successful extubation in patients after myocardial revascularization.
Methods
Study design
This is a prospective cohort study conducted with the group
of patients admitted to the
ICU at the Instituto Nobre de
Cardiologia (INCARDIO) in Feira de Santana, BA, from September 2017 to May 2019. The study was approved
by the Research
Ethics Committee of Faculdade Nobre de Feira de Santana, BA, under the number
917.294. All patients were informed about
the objectives of the study
and signed a free and informed
consent form.
Eligibility criteria
Patients of both sexes, aged
over 18 years, who underwent to CABG with median sternotomy
and cardiopulmonary bypass, undergoing the first spontaneous
breathing test, awake and cooperative,
were included. Patients with hemodynamic
instability with a heart rate greater than 120 beats per minute, systolic
blood pressure greater than 150 mmHg, use of vasoactive drugs
at high flow, with signs of
cardiac arrhythmia, excessive bleeding through the drains
and pneumopathy were excluded.
Preoperative evaluation
At the time of hospital admission, patients were assessed for ventilatory, peripheral muscle strength, cough effectiveness and functionality. Muscle strength corresponded to maximum inspiratory pressure (MIP) and maximum expiratory pressure (MEP), the peripheral was assessed through the MRC, cough by the peak
of expiratory flow and functionality
by the Functional
Independence Measure (FIM). In addition
to this information,
clinical data such as comorbidities, IMC, left ventricular ejection fraction and surgical
risk were collected at this
time.
Perioperative
CABG was performed through
median sternotomy and cardiopulmonary bypass. Graft from
the left internal thoracic artery or saphenous
vein was used. The surgical procedure was always carried
out by the same team and
ended with the positioning of a subxiphoid drain, intercostal on the left and
sternorrhaphy. Analgesia was
optimized for all patients and was
referred to the ICU.
Postoperative
Upon arrival at the ICU, the
patients were connected to the
Servo-S mechanical ventilator (Maquet Critical Care AB, Sweden) in volume-controlled ventilation mode, tidal volume of 6 to 8 ml/kg, respiratory rate of 15 incursions per minute, flow of 40 L/min, positive pressure at the
end of expiration
(PEEP) of 5 cmH2O and
fraction of inspired oxygen (FiO2)
at 60%. After that moment, all
were managed by the team
according to the unit's rules
and conduct, without any influence
from the researchers.
With the start of the ventilatory
drive, the ventilation mode was changed
to ventilation with pressure support
(PSV) with sufficient support to generate
a volume of 6 to 8 ml/kg,
PEEP 5 cmH2O and minimum
FiO2 that maintained
peripheral saturation between 94-97%. At that moment, variables were evaluated to start MV interruption, such as hemodynamic stability (without or with minimal
flow of vasoactive
drugs), respiratory stability (arterial oxygen pressure above 60 mmHg, with PEEP < 8% and FiO2
< 50%), absence of active bleeding through the drains,
absence of postoperative arrhythmias and acid-base balance.
With these criteria and a satisfactory level of consciousness (Glasgow > 8), weaning was carried out and extubation was performed. Low-flow oxygen support was promptly
instituted with sufficient concentration to maintain target saturation (94-97%). All patients were followed
up for 48 hours to assess the success
or failure of weaning. Return
to invasive MV was considered unsuccessful within the first 48 hours after extubation. At that time, patients were divided into
two groups: Success Group, which remained on spontaneous ventilation for more than 48
hours, and failure group that required
invasive support in less than 48 hours. We compared the
influence of muscle strength, cough and functionality
variables between these groups.
Assessment tools
Preoperative assessment of
inspiratory muscle strength, MIP, was performed using an Indumed® (São Paulo, Brazil) analogue manovacuometer. During the evaluation, a maximal expiration until the residual volume was requested, and then a maximal and slow inspiration to the total lung
capacity was required. This test was done
using the unidirectional valve method, being possible
a flow through a hole of one
millimeter, aiming to exclude the
action of the buccinator, and repeated for three times, being used the highest
value reached, as long as this value
was not the
last. MEP was evaluated using the same apparatus
and the patient
was instructed to perform a maximal inspiration until he reached his
total pulmonary capacity, the mask was
placed, and after that a maximum
expiration was requested until the residual capacity was reached. The test was repeated
three times and it was considered the highest value
result, as long as this value was
not the last
[13]. Both tests were performed with the patient seated,
lower limbs resting on the
ground.
The Functional Independence Measurement
that aims to measure what
the person really accomplishes, regardless of the
diagnosis, generating valid score for limitation or not. This
scale assesses the patient's ability
to develop body care, sphincter control, transfer and locomotion, as well as cognitive function such as communication and memory. A score from 1 to 7 is
attributed, with the lowest value
corresponding to the patient totally
dependent and the maximum value
was that patient completely independent from the functional point of view, reaching
a maximum value of 126 points when all variables were
added together [7].
The MRC assesses peripheral muscle strength through the ability
to overcome the load of
six muscle groups (shoulder abductors, elbow flexors, wrist extensors, hip flexors, knee extensors and ankle dorsiflexors),
scoring bilaterally each group from
0 to 5, where zero represents absence of contraction and five the
patient wins the maximum resistance
imposed by the examiner. The minimum score for this test is 0 (quadriplegia) and can reach
up to 60 points (muscle strength preserved). A value less than 48 can
be suggestive of a polyneuromyopathy [8].
Peak expiratory flow was evaluated
using the peak flow of
the Mini Wright® brand. During
the evaluation, the patient was
seated, with his head in a neutral position and a nasal clip to prevent air from
escaping through the nostrils. The patient took a deep breath, until
total pulmonary capacity, followed by forced
expiration with the mouth in the
device. After three measurements, the highest value was
chosen and there could be
no difference > 40 liters
between measurements [14].
Statistical analysis
For data analysis, the Statistical
Package for Social Sciences
(SPSS) version 20.0 was used. Normality was verified using
the Shapiro-Wilks test.
Data were expressed as mean and standard deviation or median
and interquartile range.
For the analysis of categorical variables, Chi-square was used. For comparison
between groups, the independent Student's T-test or Mann-Whitney was used. Pearson’s correlation test was used to
correlate the data. Statistical
significance was set at p < 0.05.
Results
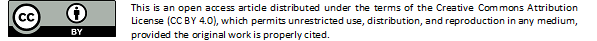
The research was carried
out with seventy-four individuals. With a predominance of males with 49 (68%) patients, aged between 63 ± 5 years and having
an average Body Mass Index
(BMI) of 26 ± 3 kg/m2. The prevalent
comorbidity was Systemic Arterial Hypertension in
45 (76%). The other values
are shown in table I.
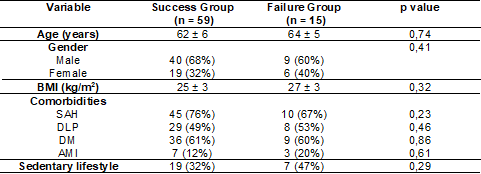
Among the surgical variables, it can be seen
that there was no difference in the characteristics evaluated (Table II).
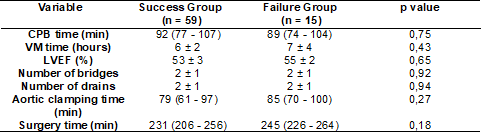
Table III shows the
functional characteristics of the sample. Strength variables and PEF showed no statistical difference between groups. However, the MRC and MIF variables showed a statistically significant difference, with Group Success
(GS) 58 ± 1 vs Group Failure (GI) 51 ± 2; (p = 0.03) and
GS 125 ± 1 vs GI 116 ± 3; (p = < 0.001), respectively.
The blood gas values
are expressed in the table below and
show that there was a similarity between the groups,
not influencing their final result (Table IV). Other correlation analysis is displayed
in Table V.
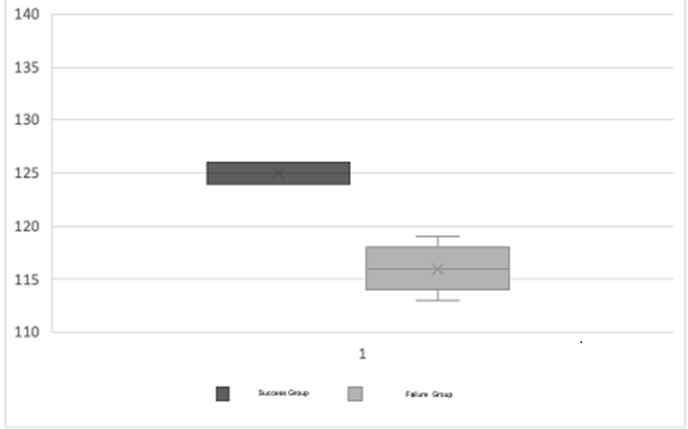
The
figure below shows the interquartile behavior of the MRC in the
Success Group, which ranged from
57 ± 1 to 59 ± 1 vs Unsuccessful Group 49 ± 2 to 53 ± 2 (Figure 1).
The FIM had a variation in its mean score of 125 ± 1 in the Success Group
vs 116 ± 3 in the Failure Group and
half of the
patients in the Failure Group had
a score less than 116
(Figure 2).
Table I - Clinical characteristics of the studied
patients
*Student’s T test for independent samples; BMI = body mass index (weight / height²); SAH = systemic
arterial hypertension; DLP = dyslipidemia; DM = diabetes mellitus; AMI = acute myocardial infarction
Table II - Surgical characteristics of the studied patients
*Student’s T test for independent samples; # Mann-Whitney test; CPB = cardiopulmonary bypass; V =
mechanical ventilation; LVEF = left ventricular ejection fraction
Table III - Functional characteristics of the studied patients
*Student’s T test for independent samples; CI 95% = confidence interval 95%; MIP = Maximum inspiratory
pressure; MEP = maximum expiratory pressure; PEF = Peak Expiratory Flow; MRC = Medical
Research Council; FIM = Functional Independence Measure
Table IV - Pre-extubation gasometric variables of the studied
patients
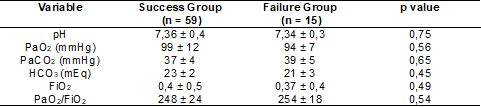
*Student’s T test for independent samples; pH = Hydrogen potential; PaO2 = Partial Oxygen Pressure;
PaCO2 = Partial Pressure of Carbon Gas; HCO3 = Bicarbonate; FiO2 = Inspired Oxygen Fraction; PaO2/
FiO2: Partial Oxygen Pressure and Inspired Oxygen Ratio
Table V - Correlation between extubation success and functional
characteristics
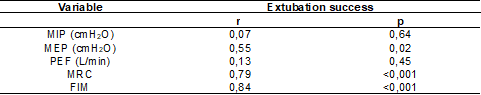
*Pearson correction test; MIP = maximum inspiratory pressure; MEP = maximum expiratory pressure;
PEF = peak expiratory flow; MRC = Medical Research Council; MIF = functional independence measure
FIM = Functional Independence Measure
Figure 1 - FIM behavior
between the groups studied
Discussion
Based on our results, peripheral
muscle strength, expiratory force and functionality demonstrated a statistically significant influence on the
success of extubation in patients after CABG.
The influence of ventilatory
muscle strength as a predictor of failure
in the weaning and extubation process is already
known [15], but the participation of peripheral muscle
strength in this process in patients undergoing cardiac surgery was still questioned. We found that the
highest MRC score was associated with the success of
extubation and there may be
a direct relationship with the ventilatory force. There are studies that correlate these two forces, showing that the increase
in ventilatory muscle function is reflected
as improvement in peripheral
strength [16,17].
Patients with lower values on
the functionality scale were more dependent since the preoperative period may have
influenced a later mobilization
in the postoperative period and are associated with worse results on
extubation. It is known that the
late start of this therapy has a direct impact on the
ventilatory and peripheral muscle strength of patients
in the postoperative period [18,19,20].
The ventilatory muscle strength did not
show statistical difference
between the groups and this
is justified by the fact
that this evaluation was performed before the surgical process
and, consequently, before the possible
intraoperative damages. A reduction in the strength values is expected after
the procedure, however, as these patients were not evaluated
in the postoperative period, there is
a gap regarding the decline
of this variable
and its possible contribution to the outcome.
Thille et al. [16] considered
the muscle weakness acquired in the ICU assessed from the MRC as one of the
important characteristics that influence extubation failure. In addition to reduced
muscle strength, ineffective coughing was also associated
with extubation failure in this study. Peak expiratory
flow is a sign of the
effectiveness of cough, with values
below 60 L/min associated with an inability
to protect the airways [17].
In our study, we
found that peak flow was
not associated with a worse extubation
outcome, but maximum expiratory pressure, which also corresponds to coughing capacity,
was reduced. This could represent
a confounding variable, however, as PEF had no influence on the
result, we cannot attribute the ineffective cough to the
failure of extubation.
Kutchak et al. [21] mention
in their research carried out with neurological patients, that there are differences in the motor activation of expiratory
and accessory muscles during voluntary and reflex
cough and that this could
generate significant differences at the time of the
extubation procedure. The data concluded
that the PEF is a potential predictor of the
success or failure of extubation
in patients who pass the Spontaneous
Breath Test.
Even the study presented
some limitations, such as risk of bias in the lack of
performing the sample calculation, lack of evaluation of
the pain and the lack
of follow-up in relation to functional outcomes.
It was possible to obtain a positive result with regard
to peripheral muscle strength and mainly functionality,
however, we suggest further studies with a complete evaluation aiming to avoid complications
and thus lead to extubation failure.
Conclusion
We concluded that peripheral and expiratory muscle strength and functionality demonstrated a statistically significant influence on the success
of extubation in patients after coronary artery bypass grafting.
Conflicts of
interest
There are no conflicts of interest.
Financing source
No funding.
Authors' contribution
Conception and
design of the research, obtaining data and writing the
manuscript: Cordeiro ALL, Mascarenhas HC, Soares LO,
Pimentel VO, Souza LS, Marchesini A, Ferreira GVDBA; Critical review of the manuscript for important intellectual content: Guimarães ARF
References
- Santos TD, Pereira SN,
Portela LOC, Cardoso DM, Lago PD, Guarda SN, et al. Moderate-to-high intensity inspiratory muscle training
improves the effects of combined training on exercise capacity
in patients after coronary artery bypass graft surgery:
A randomized clinical trial. Int J Cardiol.
2019 Mar 15;279:40-46. doi: 10.1016/j.ijcard.2018.12.013 [Crossref]
- Paez RP, Hossne Junior NA, Santo JADE, Berwanger O, Santos RHN, Kalil RAK, et al. Coronary artery bypass surgery in Brazil: Analysis of the National Reality Through the BYPASS Registry. Braz J Cardiovasc Surg. 2019;34(2):142-148. doi: 10.21470/1678-9741-2018-0313 [Crossref]
- Torrati, FG, Dantas, RAS. Circulação extracorpórea e complicações no período pós-operatório imediato de cirurgias cardíacas. Acta Paul Enferm. 2012;25(3):340-5. doi: 10.1590/S0103-21002012000300004 [Crossref]
- Cordeiro ALL, Silva LGR, Pinto MO, Araújo JS, Guimarães AR, Petto J. Behavior of pulmonary function after hospital discharge in patients submitted to myocardial revascularization. Int J Cardiovasc Sci. 2019;32(2)104-09. doi: 10.5935/2359-4802.20180092 [Crossref]
- Westerdahl E, Jonsson M, Emtner M. Pulmonary function and health-related quality of life 1-year follow up after cardiac surgery. J Cardiothorac Surg. 2016;11(1):99. doi: 10.1186/s13019-016-0491-2 [Crossref]
- Cordeiro ALL, Queiroz GO,
Souza MM, Guimarães AR, Araújo TM, Junior MAV, et al. Mechanical
ventilation time and peripheral muscle strength in post-heart surgery. Int J Cardiovasc Sci.
2016;29(2):134-38. doi: 10.5935/2359-4802.20160021 [Crossref]
- Borges JBC, Ferreira DLMP, Carvalho SMR, Martins AS, Andrade RR, Silva MAM. Pain intensity and postoperative functional assessment after heart surgery. Braz J Cardiovasc. 2006;21(4):393-402. doi: 10.1590/S0102-76382006000400009 [Crossref]
- Vento DA, Faria AM, Silva LG, Ferreira JCM, Guimarães VA. Utilização da Escala do Medical Research Council no Desmame em Pacientes Críticos: Revisão de Literatura. Rev Educ Saúde. 2018;6(2):125-32. doi.org/10.29237/2358-9868.2018v6i2.p125-132 [Crossref]
- Flynn BC, He J, Richey M, Wirtz K, Daon E. Early extubation without increased adverse events in high-risk cardiac surgical patients. Ann Thorac Surg. 2019;107(2):453-59. doi: 10.1016/j.athoracsur.2018.09.034 [Crossref]
- Wong WT, Lai VK, Chee YE, Lee A. Fast-track cardiac care for adult cardiac surgical patients. Cochrane Database Syst Rev. 2016;9(9):CD003587. doi: 10.1002/14651858.CD003587.pub3 [Crossref]
- Souza LC, Guimarães FS, Lugon J. Evaluation of a new index of mechanical ventilation weaning: the timed inspiratory effort. Journal of Intensive Care Medicine. 2015;30(1):37-43. doi: 10.1177/0885066613483265 [Crossref]
- Souza LC, Guimarães FS, Lugon J. The timed inspiratory effort: a promising index of mechanical ventilation weaning for patients with neurologic or neuromuscular diseases. Respir Care 2015;60(2):231–38. doi: 10.4187/respcare.03393 [Crossref]
- Caruso P, Albuquerque ALP, Santana PV, Cardenas LZ, Ferreira JG, et al. Métodos diagnósticos para avaliação da força muscular inspiratória e expiratória. J Bras Pneumol. 2015;41(2):110-123. doi: 10.1590/S1806-37132015000004474 [Crossref]
- Ruchkys CV, Dias, RM, Sakurai E, Camargos PAM. Acurácia de medidores do pico do fluxo expiratório (peak-flow) da marca MiniWright. J Pediatr. (Rio J.). 2000;76(6):447-52. doi: 10.2223/JPED.92 [Crossref]
- Khemani RG, Sekayan T, Hotz J, Flink RC, Rafferty GF, Iyer N, et al. Risk factors for pediatric extubation failure: the importance of respiratory muscle strength. Crit Care Med. 2017 Aug;45(8):e798-e805. doi: 10.1097/CCM.0000000000002433 [Crossref]
- Thille AW, Boisser F, Ghezala HB, Razazi K, Mekontso-Dessap A, Brun-Buisson C. Risk factors for and prediction by caregivers of extubation failure in ICU patients: a prospective study. Crit Care Med. 2015;43(3):613-20. doi: 10.1097/CCM.0000000000000748 [Crossref]
- Jiang C, Esquinas A, Mina B. Evaluation of cough peak expiratory flow as a predictor of successful mechanical ventilation discontinuation: a narrative review of the literature. J Intensive Care 2017;5:(33);1-5. doi: 10.1186/s40560-017-0229-9 [Crossref]
- Wang TH, Wu CP, Wang LY. Chest physiotherapy with early mobilization may improve extubation outcome in critically ill patients in the intensive care units. Clin Respir J. 2018;12(11):2613-2621. doi: 10.1111/crj.12965 [Crossref]
- Jang MH, Shin MJ, Shin YB. Pulmonary and physical rehabilitation in critically ill patients. Acute Crit Care. 2019;34(1):1-13. doi: 10.4266/acc.2019.00444 [Crossref]
- Corcoran JR, Herbsman JM, Bushnik T, Van Lew S, Stolfi A, Parkin K, et al. Early rehabilitation in the medical and surgical intensive care units for patients with and without mechanical ventilation: an interprofessional performance improvement project. PM R. 2017;9(2):113-119. doi: 10.1016/j.pmrj.2016.06.015 [Crossref]
- Kutchak FM, Debesaitys AM, Rieder MM, Meneguzzi C, Skueresky AM, Junior LAF, et al. Reflex cough PEF as a predictor of successful extubation in neurological patients. J Bras Pneumol. 2015;41(4):358-64. doi: 10.1590/S1806-37132015000004453 [Crossref]