Rev Bras
Fisiol Exerc. 2023;22:e225387
ORIGINAL ARTICLE
Correlation between respiratory muscle strength and
peripheral muscle strength in patients with closed thoracic drainage
Correlação
entre a força muscular respiratória e a força muscular periférica dos pacientes
com drenagem torácica fechada
Suellen
Silva Moreira1, Letícia de Souza Pereira1, Maristela
Lúcia Soares Campos1,
Lucas
Silvério Borges da Silva1, Anna Paula Nogueira1, Erika
Leticia Gomes Nunes1,
Giulliano Gardenghi2
1Hospital de Urgências de Goiás, Goiânia,
GO, Brazil
2Faculdade CEAFI,
Goiânia, GO, Brazil
Received: January 18, 2023; Accepted: February 25,
2023.
Correspondence: Suellen Silva Moreira,
suellensilvamoreira@outlook.com
Como citar
Moreira SS, Pereira LS, Campos MLS, Silva
LSB, Nogueira AP, Nunes ELG, Gardenghi G. Correlation
between respiratory muscle strength and peripheral muscle strength in patients
with closed thoracic drainage. Rev Bras
Fisiol Exerc 2023;22:e225387. doi: 10.33233/rbfex.v22i1.5387
Abstract
Introduction: Thoracic
trauma comprises a variety of injuries to the rib cage, tissues and organs
located therein. In cases of pneumothorax, hemothorax or hemopneumothorax, the
most common treatment is the placement of an intercostal drain to restore
pleural pressure. The presence of drains, pain and rib fractures may favor the
decline in respiratory muscle strength in these patients. Objective: To
correlate respiratory muscle strength and peripheral muscle strength in
patients with closed thoracic drainage (CTD). Methods: This is an
analytical cross-sectional study. The participants were given the demographic
and clinical evaluation form, Visual Analog Scale, then the Peak cough flow
test, MIP, MEP, palmar grip dynamometry in both limbs and the Medical Research
Council Scale (MRC) for strength assessment. Results: 17 patients
participated, 82.4% male, with a mean age of 32.3 years. There was a strong
correlation between right handgrip dynamometry and MEP (p.0.00; r = 0.72),
between MEP and MRC (p. 0.001; r = 0.79), in addition to a weak association
between MEP and left handgrip strength (p.0.04; r = 0.54). Regarding the
average of predicted values, the participants obtained 46.3% of MIP and 47.4%
of MEP. Of the Peak Cough Flow values performed by the patients, 70.6% were
classified as effective cough. The pain according to the VAS was mostly
moderate. Conclusion: We found a correlation between expiratory muscle
strength and peripheral muscle strength in patients after chest trauma and with
CTD. The strength parameters evaluated were lower than those expected in the literature.
Keywords: thoracic injuries; drainage;
maximum inspiratory pressure; maximum expiratory pressure; Physical therapy.
Resumo
Introdução: O trauma torácico compreende uma
variedade de lesões na caixa torácica, tecidos e órgãos nela localizados. Nos
casos de pneumotórax, hemotórax ou hemopneumotórax o
tratamento mais utilizado é o posicionamento de um dreno intercostal para
restabelecer as pressões pleurais. A presença de drenos, dor e fraturas de
costelas podem favorecer o declínio da força muscular respiratória desses
pacientes. Objetivo: Correlacionar a força muscular respiratória e força
muscular periférica dos pacientes com drenagem torácica fechada (DTF). Métodos:
Trata-se de um estudo transversal analítico. Aos participantes foram aplicados
o formulário de avaliação demográfica e clínica, Escala Visual Analógica. Em
seguida, foram realizados o teste de Pico de fluxo de tosse, PImáx, PEmáx,
a Dinamometria de preensão palmar em ambos os membros
e a Escala Medical Research Council
(MRC) para avaliação da força. Resultados: Participaram 17 pacientes,
82,4% do sexo masculino, com idade média de 32,3 anos. Houve correlação forte
entre dinamometria de preensão palmar direita e PEmáx (p.0,00; r = 0,72), entre a PEmáx e o MRC (p. 0,001; r = 0,79), além de
associação fraca entre a PEmáx e a força
preensão palmar esquerda (p.0,04; r = 0,54). Em relação à média dos valores
preditos, os participantes obtiveram 46,3% da PImáx
e 47,4% da PEmáx. Dos valores do Pico de
Fluxo de Tosse realizados pelos pacientes, 70,6% foram classificados em
tosse eficaz. A dor segundo a EVA foi em maioria, moderada. Conclusão:
Encontramos correlação entre a força muscular expiratória e a força muscular
periférica em pacientes pós-trauma torácico e com DTF. Os parâmetros de força
avaliados se mostraram inferiores aos esperados na literatura.
Palavras-chave: traumatismos torácicos; drenagem;
pressão inspiratória máxima; pressão expiratória máxima; Fisioterapia.
Introduction
Chest trauma comprises a variety of
injuries to the rib cage, tissues and organs located therein. The costal arches
and lungs are the most affected. In addition to them, the heart, great vessels,
trachea and esophagus are among the structures that can also be affected [1].
Thoracic traumas are classified according to their trauma mechanism, as closed
and penetrating [2,3].
In relation to the total number of
traumas that occur in the world, 15% are closed thoracic, and among polytrauma
patients, traumas to the rib cage of both types are present in 60% of cases
[2]. In Brazil, these lesions occur predominantly in young and adult men. The
most common fractures are of the spine and ribs, complicated by pneumothorax
and hemothorax with low mortality [4].
In cases
of pneumothorax, hemothorax or hemopneumothorax, the most used treatment is the
placement of an intercostal drain to restore pleural pressures [1]. Closed
chest drainage (CTD) is a minor surgical treatment. Only 10% of blunt trauma
and 30% of penetrating trauma require major surgery [5]. The presence of
drains, pain and rib fractures may favor the decline in respiratory muscle
strength in these patients [6,7,8].
In view of changes in ventilatory
mechanics caused by trauma and associated injuries, there is a high risk of
ventilatory complications, and the patient may progress to acute respiratory
failure with the need for ventilatory support in more severe cases. Thus, it is
important to know what degree of ventilatory compromise is expected and what is
the influence on the length of stay and complications in these patients [9].
Due to pain and immobility,
patients may have reduced inspiratory and expiratory muscle strength, with a
decrease in peak cough flow. In addition to reduced muscle strength in the
upper limbs due to the presence of the chest drain. The aim of this study is to
correlate respiratory muscle strength and peripheral muscle strength in
patients with CTD. It is expected to observe that patients are predominantly
male, with chest trauma due to traffic accidents and falls.
Methods
This is an analytical
cross-sectional study, carried out in the wards of the Hospital de Urgências de Goiás (HUGO), which
is a public unit linked to the Goiás State Secretary,
based on the authorization of the Research Ethics Committee of the HUGO (CAAE:
53746321.8.0000.0033). Patients admitted to the HUGO wards participated in the
study.
Based on the number of patients
admitted to the ward of the participating center, in a time interval similar to
that of our collection, in the historical series of the service, we estimate
that during the study period 48 patients would be evaluated for inclusion,
assuming a possible total population of 54 patients. For this sample, a
confidence interval of 95% and a margin of error of 5% were used.
The inclusion criteria for the
study were: 1) age greater than or equal to 18 years; 2) have a clinical
diagnosis of chest trauma associated with any lung injury, whether
pneumothorax, hemothorax or pulmonary contusion, with or without rib fractures;
3) in use of closed thoracic drainage; 4) sign the Informed Consent and Free
Term (ICFT).
Patients with 1) non-traumatic lung
injuries, such as: spontaneous pneumothorax, iatrogenic injuries and others,
were excluded from the study; 2) patients with cognitive impairment or Glasgow
Coma Scale (GCS) less than 15; 3) patients diagnosed with spinal cord injury
without release for movement; 4) having undergone laparotomy or having lesions
in regions that make it impossible for the testicles to perform ventilatory
muscle strength, such as the mouth and face; 5) population with deprivation of
liberty; 6) incomplete medical record.
Data collection was carried out by
two duly trained evaluators, lasted five months and was divided into three
moments. Initially, a screening of patients in the wards was carried out,
through the electronic medical record system, to identify those who were
admitted due to chest trauma and then the inclusion and exclusion criteria were
applied. Soon after, the patient able to participate in the research was invited
and explanations about the research were made, reading of the ICFT,
clarification of the evaluations that would be carried out and signature of the
ICFT. Then, the demographic and clinical evaluation form, Scale Visual Analog
(VAS), according to the patient's possibilities, either at the bedside or with
the headboard raised, the Peak Cough Flow test, Maximum Inspiratory Pressure
(MIP), Maximum Expiratory Pressure (MEP), Dynamometry of palmar grip in both
limbs and the Medical Research Council (MRC) strength scale were applied.
The Demographic and Clinical
Evaluation Form contained abbreviation, medical record number, sex, date of
birth, age, height, lifestyle habits (alcoholism, smoking, use of illicit drugs
and physical activity), hospitalization data (day of admission in the hospital,
total days of hospitalization and others), trauma-related data (trauma
mechanism, associated factors and others) and clinical data (severity,
radiological findings, peripheral O2 saturation, heart rate and
others).
The VAS is a simple and sensitive
self-assessment scale of pain perception. It is represented by a numerical line
in ascending order of 10 cm, its score varies from 0, which means complete
absence of pain, to 10, unbearable pain. The examiner showed the scale to the
patient, asking him to grade his pain. Mild pain was considered between 1 and
2, moderate between 3 and 7 and severe pain between 8 and 10 [10].
The Cough Flow Peak test was
performed using a Medicate® device that ranges from 60 L/min to 900 L/min.
After the due explanations about the test, the patient performed a learning
test, just to learn how the device works, then the examiner asked the patient
to perform a maximum inspiration, followed by the closure of the glottis and a
cough. Three measurements were performed with a rest interval according to the
patient's needs between measurements, the best result was considered for data
analysis. Cough was classified as ineffective (less than 160 L/min), weak (160
L/min to 269 L/min) and effective (greater than 270 L/min) [11].
Measurements of MIP and MEP were
performed using an analog manovacuometer device from
the Murenas® brand, to measure the patient's maximum
inspiration and expiration force. The patient was advised that, in order to
assess maximum inspiration, he should actively perform a complete expiration
outside the device, followed by a maximum inspiration with the lips attached to
the mouthpiece. Similarly, to assess maximal expiration force, a full free
inspiration and after a maximal expiration with lips tightly sealed in the
device. Both tests had to be performed with a nose clip, preventing air leakage
through the nose during the procedure. After the proper guidance on the test,
the patient performed a maximum inspiratory and expiratory test that was not
recorded, just to learn how the device was working. Three attempts were
requested with an interval of at least one minute between them, and only the
best result was considered for data analysis. The reference valueswere
obtained through the equations for men MIP = -0.80(age)+155.3; MEP =
-0.81(age)+165.3; and women MIP = -0.49(age)+110.4; MEP = -0.61(age)+115.6
[11,12].
Handgrip strength was measured
using a Saehan® hand held hydraulic dynamometer device, duly calibrated. The
patient was placed in a sitting position with the forearm extended in a lateral
position away from the body, with the wrists in a neutral position. Maximum
grip strength was requested 3 times on each limb, with a 30-second rest
interval between repetitions. Only the best result of each member was
considered [13]. The values that were use d as a reference are described in the
study by Schlussel [14].
The MRC strength scale assesses the
muscle strength of some muscle groups. They are: shoulder abductors, elbow
flexors and wrist extensors in the upper limbs; and hip flexors, knee extensors
and foot dorsiflexors in lower limbs. The patient was asked to perform the
movement, the degree of strength was graded according to the criteria 0 (zero) total
paralysis, 1 (one) sketch of contraction, 2 (two) complete movement as long as
gravity was removed, 3 (three) movement against gravity, 4 (four) overcomes
minimal resistance and 5 (five) overcomes normal resistance. The points were
added and the results were graded from 0 (tetraplegia) to 60 (normal) [15].
Data were categorized and tabulated
in an electronic spreadsheet in Microsoft Excel 2016 software and then analyzed
in the statistical program Statistical Package for Social Sciences, (IBM Corporation,
Armonk, USA) version 26.0. For analysis of categorical variables, absolute
frequency and relative frequency were used, and for continuous variables, mean
and standard deviation. Data normality was verified using the Shapiro-Wilk
test. The relationship between the study's exploratory variables was tested by
applying Spearman's correlation. The significance level adopted was 5% (p <
0.05). With regard to correlations, the following classification was adopted
for positive and negative values: strong correlation, r ≥ 0.70; moderate,
0.31 < r < 0.70; and weak, 0.1r ≤ 0.30 [16].
Results
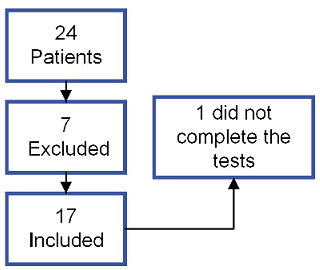
Source: authors
Figure 1 – Population inclusion
flowchart
Figure 1 shows the inclusion
flowchart of the study population. Demographic and clinical data are summarized
in Table I. The mean age of participants was 32.3 years (standard deviation:
15.5; minimum: 18; maximum 72). Regarding the type of trauma, 52.9% were open
and 47.1% were closed. Among the causes, traffic accidents represent 41.2%,
stab wounds 41.2%, perforation by firearms 11.8% and beatings 5.9%. Rib
fractures occurred in 52.9% of cases, of which 55.6% fractured more than one
rib. Lung injuries were pneumothorax (47.05%), hemothorax (11.8%),
hemopneumothorax (41.2%) and pulmonary contusion (29.4%).
Table I - Characterization of the
demographic and clinical profile of patients (n = 17)
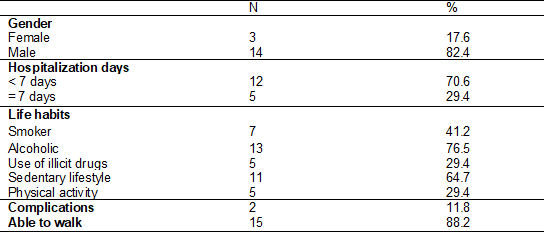
The main associated injuries were
traumatic brain injury, face, injury in upper limbs, lower limbs and abdominal
injury. Complications occurred in two patients, one being a spontaneous
pneumothorax and a large-volume empyema. In this study, there were no deaths
among the participants.
The test results are described in
table II. Regarding the mean of the predicted values, the participants obtained
46.3% of MIP and 47.4% of MEP. The Peak Cough Flow values performed by the
patients were classified as effective cough 70.6% (n:12), weak cough 23.5%
(n:4) and ineffective cough 5.9% (n:1).
The mean of the group in relation
to the predicted values was 85.6% of the grip strength on the right and 89.0%
grip strength on the left. The mean MRC was 89.0% of the predicted value for
this sample. Pain reported by patients was classified as none 23.5% (n:4) VAS
0, mild pain 23.5% (n:4), moderate pain 47.1% (n:8) and only 5.9% (n:1) said
they felt severe pain at the time of the assessment.
Table II – Test results (n = 17)
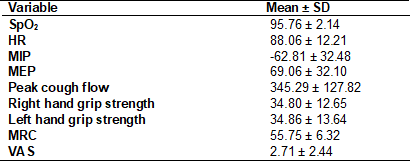
SD = standard deviation; SpO2
= Peripheral O2 saturation; HR = Heart rate; MIP = Maximum
inspiratory pressure; MEP = Maximum expiratory pressure; MCR == Medical
Research Council; VAS = Visual Analog Scale
Table III presents the correlations
between the MIP and MEP tests with the handgrip dynamometry and the MRC. When
the respiratory muscle strength variables were correlated with peak cough flow,
there was a moderate association with MEP (p. 0.01; r = 0.62) and with MIP (p.
0.01; r = 0.60), in addition to these, an association was found between peak
cough flow and peripheral muscle strength, which was also moderate both with
the right palmar grip dynamometry (p. 0.04; r = 0.51) and with the dynamometry
of left palmar grip (p. 0.03; r = 0.58).
Table III - Result of the correlation
between MIP and MEP with handgrip strength and MRC (n = 17)
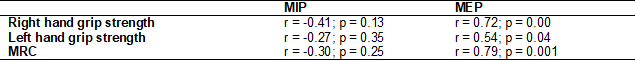
The significance level adopted was
5% (p < 0.05). MIP = Maximum inspiratory pressure; MEP = Maximum expiratory
pressure; MCR = Medical Research Council
Discussion
We observed, through this
analytical cross-sectional study, that only the MEP test results had a strong
correlation between the right handgrip strength and the MRC, and a moderate
correlation with the left handgrip strength. MIP, on the other hand, was not
related to any of the peripheral muscle strength tests.
There was a predominance of open
chest trauma, the main causes being stab wounds and gunshot wounds. This
finding had already been described in a study carried out at the same
institution, published in 2013. These data are linked to the increasing
violence registered in developing countries such as Brazil [17]. In relation to
blunt trauma, traffic accidents that occur mainly in the younger portion of the
population [1,3] stand out, aggravated by the increased circulation of
motorcycles and bicycles, poor road conditions and the recklessness of drivers
[18].
Regardless of which lung injury,
they can generate complications, in this study, they occur in only two cases,
one empyema and one spontaneous pneumothorax after discharge. Some factors may
predispose to complications, such as the poor positioning of the drain and
drainage conditions, such as those performed at the emergency room in
pre-hospital care. Both increase the risk of inadequate drainage of the
contents, either air or pleural fluid, requiring a thoracostomy. In cases where
drainage is performed outside the hospital environment, it favors the
occurrence of infectious processes such as empyema, pneumonia and infection at
the site of the drain [5].
Although smoking and the use of
some types of illicit drugs are predisposing factors for spontaneous
pneumothorax [19], they were not associated with an increased risk of
complications in this sample. However, it is already known that other factors,
such as fractures in the first rib, increase the rate of complications, as they
can cause more serious damage, such as injuries to large vessels such as the
subclavian, tracheobronchial, pulmonary and cardiac injuries. Rib fractures
have been found in all patients with blunt chest trauma, but they alone are not
fatal. In view of this, early assessment and identification is essential for
the proper management of injuries due to their potential risk to life [20]. There
were no deaths in our sample, which can be explained by the fact that thoracic
traumas have a low mortality rate [4], in addition, our sample included
patients evaluated in the ward, possibly at low risk.
Even in the case of a less severe
group, the MIP and MEP values obtained were more than 50% below the predicted
value. MIP and MEP values within the predicted range exclude the presence of
weakness, however values below the ideal do not unquestionably confirm it,
since factors such as the technique used in the measurement and the patient's underexertion can influence the results [21]. To carry out
these tests, it is necessary to use the inspiratory muscles in MIP and the
external and abdominal intercostals in MEP, the weakness of these muscles can
lead to a feeling of tiredness, functional impairment and worsening of quality
of life [22].
Thoracic geometry favors the
conversion of force into pressure. To assess this variable, it is important to
consider the interaction of muscles in the rib cage and abdominal wall. Chest
injuries can cause damage to the two functions of the respiratory muscles,
which are to shorten and develop strength. The measurement of MIP and MEP
reflects the sum of the pressure generated by the muscles and the elastic
recoil force of the lungs from the thoracic cage [23].
Some studies have shown an association between
peripheral muscle strength and respiratory muscle strength. Research has been
carried out both in healthy individuals and in certain groups of patients,
showing moderate correlation between them. To measure the strength of the
peripheral muscles, some tests are performed including: handgrip dynamometry
and the MRC strength scale, which are used in the evaluation of patients in the
hospital environment, as they are easy to apply and inexpensive [24,25,26].
Peripheral muscle training has
benefits on respiratory function, providing strength gains and inspiratory
muscle endurance [27]. Similarly, in patients undergoing phase II cardiac
rehabilitation, the increase in respiratory muscle strength through inspiratory
muscle training reflects an improvement in systemic vasodilation and peripheral
muscle perfusion [28]. Whenever there are no limiting factors, these patients
should be encouraged to mobilize their limbs, sit down and walk [29], in
addition to reducing complications such as deep vein thrombosis and pneumonia,
it also results in an increase in functional capacity and a return to their
routines after discharged [30].
The reduction in respiratory muscle
strength has an impact on the tolerance to perform exercises, activities of
daily living and on the sensation of dyspnea. In the treatment of pathologies
such as COPD, as well as in healthy individuals, training the inspiratory
muscles leads to gains in the functioning of both these muscles and the
expiratory muscles, but it is already known that the abdominal muscles are also
related to the performance of the inspiratory muscles. Therefore, it is enough
that one of the muscle groups has problems; the patient may have potential
functional impairment, since there is a significant correlation between the MIP
and MEP values, and the peak cough flow [22].
As for cough, the participants of
this study predominantly obtained a cough classified as effective (70.6%).
Coughing is a reflex mechanism for protecting the airways. This process depends
on the generation of large volumes and the length of the total lung capacity
(TLC) pause before initiating forced expiration. The combination of these factors
displaces secretion or a foreign body to the pharynx and mouth, where they are
eliminated [10]. In the same institution, in 2018, a study was carried out that
evaluated the effectiveness of the cough of patients hospitalized in the ward,
those with thoracoabdominal injuries stood out with a higher percentage of
ineffective cough compared to the other profiles of injuries and pathologies
[31] .
We found no correlation between
pain complaints and respiratory function tests. Pain was assessed using the VAS
scale, and 47.1% of participants in our study reported moderate pain. Pain is a
significant symptom in the presence of rib fractures, due to the existence of
costal nerves located at their edges [32]. Even individuals who do not need
surgical interventions report deep pain, mainly in the first three days
following the injury. Pain management improves vital capacity, chest expansion
and inspiratory capacity. This implies a shorter hospital stay and more
efficiency in performing breathing exercises and mobilization [7,33].
The present study has a marked
limitation that must be highlighted. The sample calculation predicted 48
patients. For reasons beyond our control, in the period foreseen for data
collection, the incidence of patients with FTD was lower than that observed in
the historical series of the hospital service. The low number of patients
enrolled in this study may not actually reflect the findings presented here.
Conclusion
We found a correlation between
expiratory muscle strength and peripheral muscle strength in patients after
chest trauma and with CTD. The strength parameters evaluated were lower than
those expected in the literature.
Conflicts of interest
The authors declare that they have
no conflicts of interest in the publication of this study.
Funding sources
The authors did not receive funding
of any kind to carry out this study.
Authors' contributions
Conception and design of the study:
Moreira SS, Souza LP, Gardenghi G; Data collection:
Moreira SS, Campos MLS; Statistical analysis: Silva LSB, Gardenghi
G; Data interpretation: Moreira SS, Nunes ELG, Nogueira AP, Gardenghi
G; Text composition: Moreira SS; Approval of the final version to be published:
Moreira SS, Pereira LS, Campos MLS, Silva LSB, Nogueira AP, Nunes ELG, Gardenghi G
References
- Zhang S, Tang M, Ma J, Yang J, Qin X, Jin W, et al. Thoracic trauma: a descriptive review of 4168
consecutive cases in East China. Medicine. 2019;98(14). doi: 10.1097/MD.0000000000014993 [Crossref]
- Dogrul BN, Kiliccalan I, Asci E, Peker SC. Blunt trauma related chest wall and pulmonary injuries: An overview. Chinese Journal of Traumatology 2020;23(3):125-38. doi: 10.1016/j.cjtee.2020.04.003 [Crossref]
- Barbosa GDS. Análise
comparativa do perfil de vítimas de trauma contuso e penetrante atendidas na
sala de emergência: estudo longitudinal. [Tese]. São Paulo: Universidade de São
Paulo [Internet]. 2020 [cited 2022 Nov 3]; Available from: https://www.teses.usp.br/teses/disponiveis/7/7139/tde-24022021-093321/en.php
- Pasquali GF,
Kock KS. Epidemiological profile of chest trauma and predictive factors for
length of hospital stay in a hospital in Southern Brazil. Int J Burns Trauma.
[Internet]. 2021 [cited 2022 Nov 3];11(1):54. Available from:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8012872/
- Mendes
CA, Hirano ES. Fatores preditores de complicações da
drenagem de tórax em pacientes vítimas de trauma. Rev Col Bras
Cir. 2018;45(2). doi: 10.1590/0100-6991e-20181543 [Crossref]
- Husch HH, Watte G, Zanon M·, Pacini S, Birriel D, Carvalho PL, et al. Effects of transcutaneous
electrical nerve stimulation on pain, pulmonary function, and respiratory
muscle strength after posterolateral thoracotomy: a randomized controlled
trial. Lung. 2020;198(2):345-53. doi: 10.1007/s00408-020-00335-4 [Crossref]
- Baker E, Xyrichis A, Norton C, Hopkins P, Lee G. Building consensus on inpatient discharge pathway components in the management of blunt thoracic injuries: An e-Delphi study amongst an international professional expert panel. Injury. 2021;52(9):2551-9. doi: 10.1016/j.injury.2021.03.061 [Crossref]
- Kerti M, Balogh Z, Kelemen K, Varga JT. The relationship between exercise capacity and different functional markers in pulmonary rehabilitation for COPD. Int J Chron Obstruct Pulmon Dis. 2018;13:717-24. doi: 10.2147/COPD.S153525 [Crossref]
- Wu W, Zhao T, Li Y, Guo X, He W, Yang Y. Preliminary study of the characteristics of rib fractures and their impact on pulmonary ventilatory function. J Cardiothorac Surg. 2021;16(1):1-6. doi: 10.2147/COPD.S153525 [Crossref]
- Sousa
FF, Silva JD. A métrica da dor (dormetria): problemas
teóricos e metodológicos. Revista Dor [Internet]. 2005 [cited 2022 Nov 3];6(1):469-513.
Available from: https://www.researchgate.net/publication/284979775_A_metrica_da_dor_dormetria_Problemas_teoricos_e_metodologicos
- Bombardelli HL, Rossetto M, Dal Magro IDOF. Assessment of the respiratory function of farmers exposed to pesticides in the municipality of Quilombo (state of Santa Catarina, Brazil): relationship between health and occupational protection. Revista Brasileira de Medicina do Trabalho. 2021;19(1):27. doi: 10.47626/1679-4435-2021-551 [Crossref]
- Neder J, Andreoni S, Lerario M, Nery L. Reference values for lung function tests: II. Maximal respiratory pressures and voluntary ventilation. Braz J Med Biol Res. 1999;32(6):719-27. doi: 10.1590/S0100-879X1999000600007 [Crossref]
- Jeong M, Kang HK, Song P, Park HK, Jung H, Lee SS, et al. Hand grip strength in patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2017;12:2385-90. doi: 10.2147/COPD.S140915 [Crossref]
- Schlüssel MM, Anjos LA, Vasconcellos MTL, Kac G. Reference values of handgrip dynamometry of healthy adults: a population-based study. Clin Nutr. 2008;27(4):601-7. doi: 10.1016/j.clnu.2008.04.004 [Crossref]
- Lima CA, Siqueira TB, Travassos è. DF, Macedo CMG, Bezerra AL, Paiva Junior MDS, et al. Influência da força da musculatura periférica no sucesso da decanulação. Rev Bras Ter Intensiva. 2011;23(1):56-61. doi: 10.1590/S0103-507X2011000100010 [Crossref]
- Capela C, Marques AP, Assumpção A, Sauer JF, Cavalcante AB, Chalot SD, et al. Associação da qualidade de vida com dor, ansiedade e depressão. Fisioter Pesqui. 2009;16(3):263-71. doi: 10.1590/S1809-29502009000300013 [Crossref]
- Souza
VS, Santos AC, Pereira L v. Perfil clínico-epidemiológico de vítimas de
traumatismo torácico submetidas a tratamento cirúrgico em um hospital de
referência. Sci med [Internet]. 2013 [cited 2022 Nov
3];23(2):96–101. Available from: https://revistaseletronicas.pucrs.br/ojs/index.php/scientiamedica/article/download/11174/9652/0
- Rios PAA, Mota ELA, Ferreira LN, Cardoso JP, Santos GJ, Rodrigues TB. Acidentes de trânsito com condutores de veículos: incidência e diferenciais entre motociclistas e motoristas em estudo de base populacional. Rev Bras Epidemiol. 2019;22. doi: 10.1590/1980-549720190054 [Crossref]
- Agrafiotis AC, Rummens P, Lardinois I. Pneumothorax in otherwise healthy non-intubated patients suffering from COVID-19 pneumonia: a systematic review. J Thorac Dis. 2021;13(7):4519. doi: 10.21037/jtd-21-208 [Crossref]
- Sammy IA, Chatha H, Lecky F, Bouamra O, Fragoso-Iniguez M, Sattout A, et al. Are first rib fractures a marker for other life-threatening injuries in patients with major trauma? A cohort study of patients on the UK Trauma Audit and Research. Emergency Medicine Journal. 2017;34(4):205-11. doi: 10.21037/jtd-21-208 [Crossref]
- Bessa
EJC, Lopes AJ, Rufino R. A importância da medida da força muscular respiratória
na prática da pneumologia. Pulmão RJ
[Internet]. 2015 [cited 2022 Nov 3];24(1):37-41. Available from:
https://pesquisa.bvsalud.org/portal/resource/pt/lil-764339
- Tsukamoto T, Kato M, Kurita Y, Uchida M, Kubo A, Maruyama H. The efficacy of expiratory muscle training during inspiratory load in healthy adult males: a randomized controlled trial. Healthcare. 2022;10(5):933. doi: 10.3390/healthcare10050933 [Crossref]
- American Thoracic Society. ATS/ERS Statement on
respiratory muscle testing. Am J Respir Crit Care
Med. [Internet]. 2002 [cited 2022 Nov 3];166:518–624.
Available from: https://ci.nii.ac.jp/naid/10026628070/
- Lopes LCD, Araujo AM, Lopes TS, Pires BS, Anjos JLM. Capacidade funcional e força muscular de indivíduos internados em uma unidade de terapia intensiva cirúrgica. Revista Pesquisa em Fisioterapia. 2018;8(3):361-7. doi: 10.17267/2238-2704rpf.v8i3.2048 [Crossref]
- Ferreira
VD, Cunha TM, Nogueira PADMS, Fonsêca AMC. Relação
entre força muscular periférica e funcionalidade em pacientes críticos. ConScientiae Saúde. 2018;17(3):315-21. doi: 10.5585/conssaude.v17n3.8420
- Oliveira AMPS, Assis EV, Souza PM, Isidódio SUA, Melo ML V. Associação entre a força de preensão palmar e a força muscular respiratória de jovens por sexo. Revista Interdisciplinar em Saúde . 2020;7(1):1318-31. https://doi.org/10.35621/23587490.v7.n1.p1318-1331 [Crossref]
- Alves V, Avanzi O. Respiratory muscle strength in idiopathic scoliosis after training program. Acta Ortop Bras. 2016;24(6):296-9. https://doi.org/10.1590/1413-785220162406120752 [Crossref]
- Hermes BM, Cardoso DM, Gomes TJN, Santos TD, Vicente MS, Pereira SN, et al. Short-term inspiratory muscle training potentiates the benefits of aerobic and resistance training in patients undergoing CABG in phase II cardiac rehabilitation. Brazillian Journal of Cardiovascular Surgery. 2015;30(4):474-81. https://doi.org/10.5935/1678-9741.20150043 [Crossref]
- Clark DE, Lowman JD, Griffin RL, Matthews HM, Reiff DA. Effectiveness of an early mobilization protocol in a trauma and burns intensive care unit: a retrospective cohort study. Phys Ther. 2013;93(2):186-96. https://doi.org/10.2522/ptj.20110417 [Crossref]
- Lima VP, Bonfim D, Risso TT, Paisani DM, Junior JFF, Chiavegato LD, et al. Influência do dreno pleural sobre a dor, capacidade vital e teste de caminhada de seis minutos em pacientes submetidos à ressecção pulmonar. J Bras Pneumol. 2008;34(12):1003-7. https://doi.org/10.1590/S1806-37132008001200004 [Crossref]
- Dias LS, Moreira SMBP, Vieira LL. Análise de pico de fluxo de tosse voluntária de pacientes em um hospital de urgências. Revista Pesquisa em Fisioterapia. 2018;8(3):305-12. https://doi.org/10.17267/2238-2704rpf.v8i3.1957 [Crossref]
- Witt CE, Bulger EM. Comprehensive approach to the management of the patient with multiple rib fractures: a review and introduction of a bundled rib fracture management protocol. Trauma Surg Acute Care Open. 2017;2(1):e000064. https:/doi.org/10.1136/tsaco-2016-000064 [Crossref]
- Billings JD, Khan AD, Clement LP, Douville AA, Brown EW, Schroeppel TJ. A clinical practice guideline using percentage of predicted forced vital capacity improves resource allocation for rib fracture patients. J Trauma Acute Care Surg. 2021;90(5):769-75. https://doi.org/10.1097/TA.0000000000003083 [Crossref]