Rev Bras Fisiol Exerc 2022;21(5):295-302
doi: 10.33233/rbfex.v21i5.5403
ORIGINAL ARTICLE
Comparison between direct measurement of waist-to-hip ratio and indirect
estimation using the InBody S10 device
Comparação entre a
mensuração direta da relação cintura quadril e a estimação indireta pelo
dispositivo InBody S10
Cirley Pinheiro Ferreira 1,2,
Felipe Machado Brito1, Valmir Oliveira Silvino1,2, Layne Lins Rodrigues da Silva1, Crislane de Moura Costa1, Marcos Antônio Pereira
dos Santos1,2
1Universidade Federal do Piauí, Teresina,
PI, Brazil
2Rede Nordeste de Biotecnologia
(RENORBIO), Maceió, AL, Brazil
Received: September
12, 2022; Accepted: November
11, 2022.
Correspondence: Marcos Antônio Pereira dos Santos,
E-mail: marcosedfisio@gmail.com
How to
cite
Ferreira CP, Brito
FM, Silvino VO, Silva LLR, Costa CM, Santos MAP. Comparison between direct measurement of waist-to-hip ratio and indirect
estimation using the InBody S10 device. Rev Bras Fisiol Exerc. 2022;21(5):295-302. doi: 10.33233/rbfex.v21i5.5403
Abstract
Introduction: The waist-hip ratio (WHR), calculated with the
division between waist and hip measurements, is considered an important tool
for checking the risk of developing cardiovascular diseases. The measuring
tape, regarded as the gold standard tool for assessing WHR, is accessible and
easy to use. However, there are other tools capable of estimating WHR values,
such as the InBody S10 bioimpedance analyzer. This
study aimed to compare the WHR value estimated by the InBody
S10 device with the values measured with the measuring tape. Methods: 98
healthy young subjects (23.9 ± 5.77 years, 68.9 ± 12.67 kg, 1.69 ± 0.1 m) had
their waist and hip measurements directly assed with a measuring tape and
indirectly estimated by the InBody S10 device. The
intraclass correlation coefficient (ICC) and standard error of measurements
(SEM) were used to verify reliability. The Pearson correlation coefficient and
Bland-Altman tests were applied to compare the evaluation methods. Statistical
significance was set at p < 0.05. Results: The InBody
S10 device showed low SEM levels (0.03). However, the InBody
S10 significantly overestimated the WHR values (p < 0.05). Furthermore, the
methods showed a low intra-class correlation between repetitions (ICC = 0.24)
and a low correlation between them (r = 0.26). Conclusion: The InBody S10 device did not display valid values for
estimating the waist-hip ratio. Therefore, it may not be accurate enough for
this estimation in healthy young people.
Keywords: heart disease risk factors; body composition;
waist-hip ratio.
Resumo
Introdução: A relação cintura-quadril (RCQ),
calculada a partir da divisão entre a medida da cintura e do quadril, é considerada
uma importante ferramenta de verificação de risco de desenvolvimento de doenças
cardiovasculares. A fita métrica, ferramenta padrão ouro para a avaliação da
RCQ, é acessível e de fácil utilização. Porém, existem outras ferramentas
capazes de estimar os valores da RCQ, tais como o analisador de bioimpedância InBody S10. Este estudo buscou comparar o valor da RCQ
estimado pelo dispositivo InBody S10 com os valores
mensurados a partir da fita métrica. Métodos: 98 jovens saudáveis (23,9
± 5,77 anos, 68,9 ± 12,67 kg, 1,69 ± 0,1 m) tiveram as medidas da cintura e do
quadril diretamente avaliadas a partir do uso da fita métrica e indiretamente
estimados pelo dispositivo InBody S10. O coeficiente
de correlação intraclasse (CIC) e o erro padrão das medidas (EPM) foram
utilizados para verificar a confiabilidade. Foi aplicado o teste coeficiente de
correlação de Pearson e de Bland-Altman para comparar
os métodos de avaliação. A significância estatística foi estabelecida em p <
0,05. Resultados: O dispositivo InBody S10
apresentou baixos níveis de EPM (0,03). Porém, o InBody
S10 superestimou significativamente os valores da RCQ (p < 0,05). Além
disso, os métodos apresentaram uma correlação intraclasse baixa entre as
repetições (CIC = 0,24) e uma correlação baixa entre si (r = 0,26). Conclusão:
O dispositivo InBody S10 não exibiu valores válidos
quanto à estimação da relação cintura-quadril. Portanto, ele pode não ser
acurado o suficiente para essa estimação em jovens saudáveis.
Palavras-chave: fatores de risco de doenças cardíacas;
composição corporal; relação cintura-quadril.
Introduction
Anthropometric measurements are quantitative
assessments of body dimensions, such as height, body mass, and waist and hip
circumferences [1]. The standard anthropometric measurement tool used by the
World Health Organization (WHO) is the Body Mass Index (BMI) as an indicator of
nutritional status and health risks. Waist-to-hip ratio (WHR) is regarded as an
alternative to BMI as an anthropometric measurement [2].
The WHR is calculated by dividing the waist perimeter
measurements for the hip perimeter [3]. This measure can be used to indirectly
verify the health status of individuals, as well as to predict the risk of
cardiovascular diseases [4,5].
A high WHR value is regarded as an indicator of
increased risk of dyslipidemia, hypertension, diabetes mellitus [6], as well as
the appearance of colorectal adenomas, which may progress to cancer [7]. In
addition, WHR can be used to infer the central distribution of body fat [8,9]
and visceral fat indices, which, when elevated, can result in insulin
resistance, metabolic syndromes, and cardiovascular problems [10,11].
Bioimpedance body composition analysis (BIA) is a
fast, non-invasive, relatively accurate, and painless method to obtain body
composition data from different electrical currents, providing information such
as lean mass, fat mass, and fat percentage [9,12]. The Inbody
S10 BIA device (InBody Ltd, Seoul, South Korea) uses
segmental impedance and reactance at various frequencies to determine several
body composition variables, including total body water, extracellular water,
phase angle, fat percentage, and WHR values. This instrument was validated for
estimating body fat in patients with renal failure after a hemodialysis session
[13]. However, there are still no studies verifying its validation regarding
the estimation of the WHR. Once its validation is verified, the InBody S10 device can be an alternative for estimating WHR
for professionals and scientists, despite the practicality and accessibility of
the measuring tape.
This study aimed to verify the validity of the
bioimpedance analyzer InBody S10 in estimating the
WHR in healthy subjects.
Methods
The present study has a cross-sectional and
observational design. Ninety-eight individuals of both sexes (23.9 ± 5.77
years, 68.9 ± 12.67 kg, 1.69 ± 0.1 cm) were included. The sample was recruited
by homogenized convenience. Regarding the inclusion criteria, we selected: (1)
individuals aged between 18 and 50 years; (2) of both sexes and (3) who signed
the consent form. As exclusion criteria, the following were not eligible: (1)
individuals under the age of 18; (2) pregnant women, and (3) pacemaker wearers.
The participation of individuals was voluntary and proceeded after signing the
consent form. This study was approved by the Research Ethics Committee of the
Federal University of Piauí, Teresina, Brazil, under
protocol number 3,131,097 and was conducted in accordance with the guidelines
by the Declaration of Helsinki. Additional characteristics of the participants,
including age, height, body mass and BMI separated by sex are shown in Table I.
Table I - Characteristics of the participants
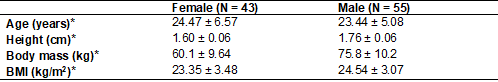
*Mean ± Standard Deviation
Data collection instruments
An anamnesis form was applied for the participants to
verify age, body mass, height, physical integrity, and healthy state at the
beginning of the experiment. To determine the WHR measurements, it was used the
indirect method via BIA with the InBody S10 device (InBody Ltd, Seoul, South Korea) and the direct method, with
the tape measure (Essencial RMC, Brazil).
Procedures
Participants underwent anthropometric tests (body mass
and height). Afterwards, the WHR measurements were calculated via BIA and using
the tape measure. The direct measurement of WHR was performed based on waist
perimeter (WP) and hip perimeter (HP). The subject was positioned in the
orthostatic position with relaxed abdomen and upper limbs at the side of the
body, feet together and with normal breathing. The WP was measured at the
midpoint between the lower rib and the upper border of the iliac crest. The HP
was considered the largest diameter of the trochanteric region, measured
laterally. Both evaluations were conducted twice, then an average was
performed. For measurements that differed by more than 3 cm, a third
measurement was performed [14,15].
BIA was performed with the InBody
S10 device (InBody Ltd, Seoul, South Korea). The
subjects were positioned in dorsal decubitus, with upper limbs extended along
the body and lower limbs in extension, keeping a distance of 15 to 20 cm
between them. The electrodes were placed on the hands (middle fingers and
thumbs) and on the legs (ankles). The evaluations were performed by a trained
Physical Education professional in an air-conditioned environment, according to
the guidelines proposed by the user's manual. Participants were previously
instructed that, at the time of the test, they were not menstruating, had not
performed physical activity, did not wear a pacemaker, did not use accessories
or metallic clothing, steel, or any conductive materials, to avoid altered
results [16].
Statistical analysis
Shapiro-Wilk and Levene
tests were conducted to verify the normality and homogeneity of data variance,
respectively. To verify the reliability of the data, the intraclass correlation
coefficient (ICC) and the standard error of measurements (SEM) were performed.
Pearson's correlation coefficient was used to assess how strongly the values
are correlated. The magnitude of the correlation adopted was: “very low” (0.00
- 0.25), “low” (0.26 - 0.49), “moderate” (0.50 - 0.69), “strong” (0.70 - 0.89)
and “very strong” (0.90 - 1.00) [17]. The agreement between each pair of
methods was evaluated using the Bland-Altman graphical analysis [18]. The
significance level was set at p < 0.05 for all analyses. For the statistical
analysis, the software SPSS version 20.0 (SPSS Inc., Chicago, IL, USA) was
used.
Results
The paired t-test showed an overestimation of the
values obtained by the InBody S10 device when
compared to the measuring tape (0.87 vs. 0.78, respectively). The ICC showed a
small correlation between repetitions for both methods (ICC = 0.24; 95% CI =
-0.134-0.500; p = 0.006). However, the InBody S10
device demonstrated low levels of SEM (0.03).
Table II - Mean ± Standard Deviation of the WHR determined
by the methods and the absolute and relative differences in relation to the
gold standard method (BIA)
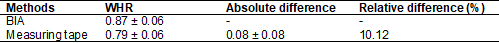
WHR = Waist-to-hip ratio; BIA: Bioimpedance analysis
There was a low correlation between the WHR values
obtained by the InBody S10 bioimpedance analyzer and
measuring tape (r = 0.26; R 2 = 0.07; p = 0.01) (Figure 1).
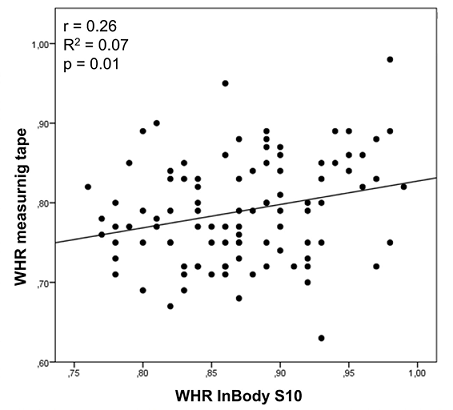
Figure 1 - Correlation between the WHR values estimated by
the measuring tape and the InBody S10 bioimpedance
analyzer
The degree of agreement between the BIA and the
measuring tape was assessed using the Bland-Altman test, within a 95%
confidence interval, as shown in Figure 2. Based on this analysis, it can be
seen that the difference between the instruments is found within the limits of
agreement.
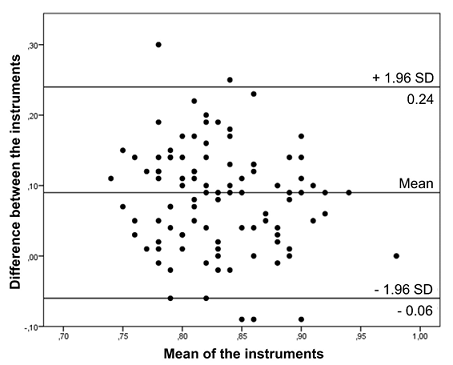
Figure 2 - Analysis of the Bland-Altman scatter plot of the
difference and mean of measurements recorded by the InBody
S10 instruments and the measuring tape
Discussion
The present study compared the estimates of central distribution
of body fat through WHR, obtained by a measuring tape and the InBody S10 bioimpedance analyzer. The indirect method of
estimating the WHR showed a statistically significant difference when compared
to the gold standard method. When the relationship between the methods was
evaluated, weak correlations were found between the measuring tape and the InBody S10 device through the ICC test that was used to
assess the agreement between the results.
The WHR assessment can be of great value in the
practice of healthcare professionals, since its quantification allows the
assessment of the risk of cardiovascular diseases [5,19], prediction of the
risk of type 2 diabetes [20], contributing to an early diagnosis, which may
help in the treatment of these possible complications [21].
Previous studies aimed to evaluate the body
composition results obtained using the InBody device,
especially the InBody 720 model [22], analyzing the
accuracy and reliability of the device for several purposes. According to Ling et
al. [23], BIA is considered a simple and non-invasive device to assess body
composition when compared to dual-energy X-ray absorptiometry (DXA). Through
BIA, it is possible to analyze segmental tissue and lean mass [23,24] of
healthy subjects, of patients on hemodialysis [13,25], of patients undergoing
treatment with peritoneal dialysis [26], and children at 6 years of age or
older [27,28].
A study comparing the results of visceral fat obtained
by BIA with the measurement performed through computed tomography demonstrates
that the results of BIA correlated significantly with the other method,
suggesting that BIA can be used as a more convenient alternative to perform
this measurement [29]. Other studies, analyzing the distribution of body water
measured by BIA in comparison with the deuterium oxide dilution method showed
similarity between the results obtained between the two methods [30,31].
Analyzing the results of body fat percentage in 3
different BIA devices (SF-BIA4: single frequency with four tactile electrodes;
SF-BIA8: single frequency with eight tactile electrodes; and MF-BIA8:
multifrequency with eight tactile electrodes) and comparing with reference
values by DXA and hydrostatic weighing (HW), it was found that the MF-BIA had the
highest correspondence with the references and the lowest estimation error
compared to the other BIA devices. Furthermore, it was found that the BIA
analyses showed a tendency to overestimate the percentage in obese individuals
and underestimate it in athletes [32].
In a study comparing the percentage of fat measured by
BIA with another method considered the gold standard (DXA), they had findings
similar to ours, where the authors found in their results a low correlation (r
= 0.30) between the methods, concluding that bioimpedance underestimates the
percentage of body fat [33].
The literature indicates that BIA has been widely used
to assess body composition [34,35]. However, so far, this is the first study
aiming to assess the reliability of the WHR estimation made by the InBody S10 system in comparison with the assessment
performed with the measuring tape.
The results of the study indicate that the Inbody S10 system significantly overestimates the WHR data
when compared to the measuring tape. Therefore, further research is suggested,
including a larger and broader sample among university students, that is,
including a greater number of underweight and obese individuals, so that the
results found can be generalized to a young and relatively healthy public.
Conclusion
The results of the present study show that the WHR
values assessed with the measuring tape and the values estimated by the InBody S10 device differed significantly from each other.
The InBody S10 overestimated the WHR values, in
addition to presenting a weak correlation when compared to the gold standard.
Therefore, it is suggested that health professionals use the measuring tape as
a tool to measure the waist-to-hip ratio in healthy young people.
Conflicts of interest
The authors declare no conflict of interest.
Funding source
This research
was supported by Coordenação de Aperfeiçoamento de Pessoal de Nível
Superior (CAPES, Brazil) and
Fundação de Amparo à Pesquisa e ao Desenvolvimento Científico e Tecnológico do
Maranhão (FAPEMA).
Authors’ contributions
Conception and
design of the research: Ferreira CP, Brito FM, Silvino VO; Data collection: Ferreira CP, Brito FM, Silvino VO, Silva
LLR, Costa C; Data analysis and
interpretation: Ferreira CP, Silvino VO; Statistical analysis:
Ferreira CP, Silvino VO; Study coordination: Santos MAP; Writing
of the manuscript:
Ferreira CP, Brito FM, Silvino VO; Critical
review of the manuscript for important intellectual content:
Ferreira CP, Silvino VO.
References
- Rodríguez-Guerrero E,
Romero-Saldaña M, Fernández-Carbonell
A, Molina-Luque R, Molina-Recio G. New simplified diagnostic decision trees for the detention of
metabolic syndrome in the elderly. Int
J Environ Res Public
Health. 2020;17(14):5191. doi: 10.3390/ijerph17145191 [Crossref]
- Fauziana R, Jeyagurunathan A, Abdin E, Vaingankar J, Sagayadevan V, Shafie S, et al. Body mass index, waist-hip ratio and risk of chronic medical condition in the elderly population: results from the Well-being of the Singapore Elderly (WiSE) Study. BMC Geriatr. 2016;16(1):125. doi: 10.1186/s12877-016-0297-z [Crossref]
- Veghari G, Salehi A, Vaghari M. The comparison of waist circumference,
waist-to-hip ratio, and waist-to-height ratio among rural women adults in the
North of Iran, between the years 2004 and 2013. ARYA Atheroscler.
2018;14(4). doi: 10.22122/arya.v14i4.1518 [Crossref]
- Srikanthan P, Seeman TE, Karlamangla AS. Waist-hip-ratio as a predictor of all-cause mortality in high-functioning older adults. Ann Epidemiol. 2009;19(10):724-31. doi: 10.1016/j.annepidem.2009.05.003 [Crossref]
- Staiano A, Reeder B, Elliott S, Joffres M, Pahwa P, Kirkland S, et al. Body mass index versus waist circumference as predictors of mortality in Canadian adults. Int J Obes. 2012;36(11):1450-4. doi: 10.1038/ijo.2011.268 [Crossref]
- Després JP. Body fat distribution and risk of cardiovascular disease: an update. Circulation. 2012;126(10):1301-13. doi: 10.1161/CIRCULATIONAHA.111.067264 [Crossref]
- Liu ZH, Zhang GX, Zhang H, Jiang L, Deng Y, Chan FS, Fan JK. Association of body fat distribution and metabolic syndrome with the occurrence of colorectal adenoma: A case-control study. J Dig Dis. 2021;22(4):222-9. doi: 10.1111/1751-2980.12979 [Crossref]
- Cornier MA, Després JP, Davis N, Grossniklaus DA, Klein S, Lamarche B, et al. Assessing adiposity: a scientific statement from the American Heart Association. Circulation. 2011;124(18):1996–2019. doi: 10.1161/CIR.0b013e318233bc6a [Crossref]
- Ling CHY, Meskers CGM, Maier AB. Can anthropometric measures be used as proxies for body composition and physical function in geriatric outpatients? Arch Gerontol Geriatr. 2021;94:104379. doi: 10.1016/j.clnu.2011.04.001 [Crossref]
- Chen CH, Chen YY, Chuang CL, Chiang LM, Chiao SM, Hsieh KC. The study of anthropometric estimates in the visceral fat of healthy individuals. Nutr J. 2014;13(1):46. doi: 10.1186/1475-2891-13-46 [Crossref]
- Gadekar T, Dudeja P, Basu I, Vashisht S, Mukherji S. Correlation of visceral body fat with waist–hip ratio, waist circumference and body mass index in healthy adults: A cross sectional study. Med J Armed Forces India. 2020;76(1):41-6. doi: 10.1016/j.mjafi.2017.12.001 [Crossref]
- Paz LSC, Couto AV. Avaliação nutricional em pacientes críticos: revisão de literatura. BRASPEN J [Internet]. 2016 [cited 2022 Jan 24];31(3):269-77. Available from: http://www.braspen.com.br/home/wp-content/uploads/2016/11/16-Avalia%C3%A7%C3%A3o-nutri-em-pacentes-criticos.pdf
- Jayanama K, Putadechakun S, Srisuwarn P, Vallibhakara SA, Chattranukulchai SP, Sritara C, et al. Evaluation of body composition in hemodialysis Thai patients: comparison between two models of bioelectrical impedance analyzer and Dual-Energy X-Ray Absorptiometry. Journal of Nutrition and Metabolism. 2018; 2018:1-11. doi: 10.1155/2018/4537623 [Crossref]
- Cuppari L. Nutrição clínica no adulto. 2 ed.
Barueri: Manole; 2005.
- Fonseca PCA, Carvalho CA,
Machado SP, Sousa AG. Obesidade central e doenças não transmissíveis em
servidores idosos de uma universidade federal. Geriatria
& Gerontologia
[Internet]. 2012 [cited 2022 Ago
10];6(4):332-40. Available from:
http://ggaging.com/details/174/pt-BR/obesidade-central-e-doencas-nao-transmissiveis-em-servidores-idosos-de-uma-universidade-federal
- Kyle UG, Bosaeus I, Lorenzo AD, Deurenberg P, Elia M, Manuel Gómez J, et al. Bioelectrical impedance analysis—part II: utilization in clinical practice. Clinical Nutrition. 2004;23(6):1430-53. doi: 10.1016/j.clnu.2004.09.012 [Crossref]
- Portney LG, Watkins MP. Foundations of Clinical Research: Applications to Practice. Surv Ophthalmol. 2002;47(6):598. doi: 10.1016/S0039-6257(02)00362-4 [Crossref]
- Bland JM, Altman DG. Statistical methods for assessing agreement between
two methods of clinical measurement. Lancet [Internet]. 1986 [cited 2022 Ago
12];327(8476):307-10. Available from: https://pubmed.ncbi.nlm.nih.gov/2868172/
- Saadati HM, Sabour S, Mansournia MA, Mehrabi Y, Nazari SS. O efeito direto do índice de massa corporal nos resultados cardiovasculares entre participantes sem obesidade central pela estimativa por máxima verossimilhança direcionada. Arq Bras Cardiol 2021;116(5):879-86. doi: 10.36660/abc.20200231 [Crossref]
- Zhang FL, Ren JX, Zhang P, Jin H, Qu Y, Yu Y, et al. Strong association of Waist Circumference (WC), Body Mass Index (BMI), Waist-to-Height Ratio (WHtR), and Waist-to-Hip Ratio (WHR) with diabetes: a population-based cross-sectional study in Jilin Province, China. J Diabetes Res. 2021:8812431. doi: 10.1155/2021/8812431 [Crossref]
- Brenner DR, Tepylo K, Eny KM, Cahill LE, El-sohemy A. Comparison of body mass index and waist circumference as predictors of cardiometabolic health in a population of young Canadian adults. Diabetology & Metabolic Syndrome. 2010;2(1):28. doi: 10.1186/1758-5996-2-28 [Crossref]
- Rocha JS, Ogando BM, Reis VM, Ávila WR, Carneiro AG, Gabriel RE, et al. Impacto de um programa de exercício físico na adiposidade e na condição muscular de mulheres pós-menopáusicas. Rev Bras Ginecol Obst. 2012;34(9). doi: 10.1590/s0100-72032012000900005 [Crossref]
- Ling CH, Craen AJ, Slagboom PE, Gunn DA, Stokkel MP, Westendorp RG, et al. Maier AB. Accuracy of direct segmental multi-frequency bioimpedance analysis in the assessment of total body and segmental body composition in middle-aged adult population. Clinical Nutrition. 2011;30(5):610-5. doi: 10.1016/j.clnu.2011.04.001 [Crossref]
- Esco MR, Snarr RL, Leatherwood MD, Chamberlain NA, Redding ML, Flatt AA, et al. Comparison of total and segmental body composition using DXA and multifrequency bioimpedance in collegiate female athletes. J Strength Cond Res 2015;29(4):918-25. doi: 10.1519/jsc.0000000000000732 [Crossref]
- Fürstenberg A, Davenport A. Comparison of multifrequency bioelectrical impedance analysis and dual-energy X-ray absorptiometry assessments in outpatient hemodialysis patients. Am J Kidney Dis 2011;57(1):123-9. doi: 10.1053/j.ajkd.2010.05.022 [Crossref]
- Fürstenberg A, Davenport A. Assessment of body composition in peritoneal dialysis patients using bioelectrical impedance and dual-energy X-Ray absorptiometry. Am J Nephrol. 2011b;33(2):150-6. doi: 10.1159/000324111 [Crossref]
- Kriemler S, Puder J, Zahner L, Roth R, Braun-Fahrländer C, Bedogni G. Cross-validation of bioelectrical impedance analysis for the assessment of body composition in a representative sample of 6- to 13-year-old children. Eur J Clin Nutr. 2008;63(5):619-26. doi: 10.1038/ejcn.2008.19 [Crossref]
- Lim JS, Hwang JS, Lee JA, Kim DH, Park KD, Jeong JS, Cheon GJ. Cross-calibration of multi-frequency bioelectrical impedance analysis with eight-point tactile electrodes and dual-energy X-ray absorptiometry for assessment of body composition in healthy children aged 6-18 years. Pediatrics International. 2009;51(2):263-8. doi: 10.1111/j.1442-200x.2008.02698.x [Crossref]
- Ogawa H, Fujitani K, Tsujinaka
T, Imanishi K, Shirataka H,
Kantani A, et al. InBody
720 as a new method of evaluating visceral obesity. Hepatogastroenterology
[Internet]. 2011 [cited 2022 Jan 25];58(105):42-4. Available from:
https://pubmed.ncbi.nlm.nih.gov/21510284/
- Bedogni G, Malavolti M, Severi S, Poli M, Mussi C, Fantuzzi A, Battistini N. Accuracy of an eight-point tactile-electrode impedance method in the assessment of total body water. Eur J Clin Nutr. 2002;56(11):1143-8. doi: 10.1038/sj.ejcn.1601466 [Crossref]
- Sartorio A, Malavolti M, Agosti F, Marinone PG, Caiti O, Battistini N, et al. Body water distribution in severe obesity and its assessment from eight-polar bioelectrical impedance analysis. Eur J Clin Nutr. 2004;59(2):155-60. doi: 10.1038/sj.ejcn.1602049 [Crossref]
- Demura S, Sato S, Kitabayashi T. Percentage of total body fat as estimated by three automatic bioelectrical impedance analyzers. J Physiol Anthropol Appl Hum Sci. 2004;23(3):93-9. doi: 10.2114/jpa.23.93 [Crossref]
- Eisenmann JC, Heelan KA, Welk GJ. Assessing body composition among 3- to 8-year-old children: anthropometry, bia, and dxa. Obes Res. 2004;12(10):1633-40. doi: 10.1038/oby.2004.203 [Crossref]
- Faria ER, Gontijo CA, Franceschini SCC, Sylvia CC, Peluzio MCG, Priore SE. Body composition and risk for metabolic alterations in female adolescents. Rev Paul Pediatr. 2014;32(2):207-15. doi: 10.1590/0103-0582201432215313 [Crossref]
- Silva FVM, Almonfrey FB, Freitas CMN, Fonte FK, Sepulvida MBC, Almada-Filho CM, et al. Associação da composição corporal com rigidez arterial em longevos. Arq Bras Cardiol 2021;457-62. doi: 10.36660/abc.20190774 [Crossref]