Rev Bras Fisiol Exerc 2022;21(5):312-21
doi: 10.33233/rbfex.v21i5.5405
ORIGINAL ARTICLE
Correlation between the 6-minute walking test and the cardiopulmonary
exercise test in individuals with heart failure
Correlação entre o
teste de caminhada de 6 minutos e o teste de exercício cardiopulmonar em
indivíduos com insuficiência cardíaca
Valéria Cristina de Faria1,
Ana Carolina Campos Ferreira2, Dayana Magalhães Drummond Oliveira1,
Danielle Aparecida Gomes Pereira1
1Universidade Federal de Minas Gerais
(UFMG), Belo Horizonte, MG, Brazil
2Hospital das Clínicas da Universidade
Federal Minas Gerais (UFMG), Belo Horizonte, MG, Brazil
Received: September 5, 2022; Accepted: October 13, 2022.
Correspondence: Danielle Aparecida Gomes Pereira, E-mail:
danielleufmg@gmail.com
How to cite
Faria VC, Ferreira
ACC, Oliveira DMD, Pereira DAG. Correlation between the 6-minute walking
test and the cardiopulmonary exercise test in individuals with heart failure. Rev Bras
Fisiol Exerc. 2022;21(5):312-21. doi: 10.33233/rbfex.v21i5.5405
Abstract
Objective: This study aimed to verify the correlation between
the 6-minute walking test (6MWT) and the cardiopulmonary exercise test (CPET)
in individuals with heart failure (HF), and to analyze the sensitivity of 6MWT
in differentiating individuals from classes I, II, and III of the New York
Heart Association (NYHA) functional classification system. Methods:
Seventeen individuals (3 class I, 8 class II, and 6 class III) aged 48.09 ±
12.91 years with a left ventricular ejection fraction of 44 ± 11% and VO2peak
of 25.18 ± 6.05 mL·kg-1·min-1 were assessed. Volunteers
performed CPET on a treadmill; after an interval of 48 h to 6 months, they
performed 6MWT. Pearson and Spearman correlations were used, and ANOVA was used
to compare 6MWT variables between NYHA functional classes. An alpha of 5% was
adopted as significant. Results: Significant correlations were found
between distance walked in 6MWT and VO2peak (r = 0.70). Significant
differences were found between NYHA functional classes regarding the distance
walked in 6MWT. For walking performance, significant differences were found
between NYHA classes I and II (p = 0.0001) and between classes I and III (p =
0.0001). Conclusion: The 6MWT is a simple and reliable method to assess
the functional capacity of individuals with HF, proving to be a valid
instrument for clinical practice.
Keywords: stress test; heart failure; 6-minute walking test.
Resumo
Objetivo: Este estudo teve como objetivo
verificar a correlação entre o teste de caminhada de 6 minutos (TC6) e o teste
de exercício cardiopulmonar (TECP) em indivíduos com insuficiência cardíaca
(IC), e analisar a sensibilidade do TC6 em diferenciar indivíduos das classes
I, II e III do sistema de classificação funcional da New York Heart Association (NYHA). Métodos: Dezessete indivíduos (3
classe I, 8 classe II e 6 classe III) com idade de 48,09 ± 12,91 anos, fração de
ejeção do ventrículo esquerdo de 44 ± 11% e VO2pico de 25,18 ± 6,05
mL·kg-1·min-1 foram avaliados. Os voluntários realizaram
TECP em esteira; após um intervalo de 48h a 6 meses, realizaram o TC6.
Correlações de Pearson e Spearman foram usadas, e
ANOVA foi usada para comparar as variáveis do TC6 entre as classes funcionais
da NYHA. Um alfa de 5% foi adotado como significativo. Resultados: Foram
encontradas correlações significativas entre a distância percorrida no TC6 e o
VO2pico (r = 0,70). Diferenças significativas foram encontradas
entre as classes funcionais da NYHA em relação à distância percorrida no TC6.
Para o desempenho da caminhada, foram encontradas diferenças significativas
entre as classes NYHA I e II (p = 0,0001) e entre as classes I e III (p =
0,0001). Conclusão: O TC6 é um método simples e confiável para avaliar a
capacidade funcional de indivíduos com IC, mostrando-se um instrumento válido
para a prática clínica.
Palavras-chave: teste de esforço; insuficiência
cardíaca; teste de caminhada de 6 minutos.
Introduction
Heart failure (HF) is a clinical systemic syndrome
characterized by cardiac dysfunction, which leads to a blood supply
insufficient for metabolic needs of tissue [1]. It is the later stage of most
diseases that attack the heart. These diseases are often associated with
disabling symptoms, such as dyspnea and fatigue, which lead to exercise
intolerance [2]. Exercise intolerance leads to a reduction of functional
capacity and is directly associated with the prognosis of the disease [3].
Therefore, valid and reliable methods are vital for the prescription of
appropriate exercise during the rehabilitation process of these patients.
In HF, 2 methods are most commonly used to define the
degree of exercise limitation: the cardiopulmonary exercise test (CPET) and the
6-minute walking test (6MWT) [3]. The CPET is considered the gold standard for
the assessment of functional capacity and prognosis of individuals with HF [4].
It is a non-invasive assessment procedure and provides important information on
the individual’s aerobic capacity [4]. The CPET is highly reliable in patients
with HF and is a well-accepted method of assessment in this population [5].
The CPET aims to assess the clinical, hemodynamic,
electromyographic, metabolic, and ventilatory responses to effort [6]. It is a
test that has the primary variables oxygen consumption (VO2), carbon
dioxide (CO2) production, respiratory rate (RR), tidal volume (VT),
and heart rate (HR) [5]. With these parameters, it is possible to calculate
secondary variables such as pulmonary ventilation (VE), respiratory exchange
rate (RER = VCO2/VO2), expired oxygen fraction (%FEO2),
carbon dioxide expired fraction (%FECO2), oxygen pulse (VO2/FC),
oxygen ventilatory equivalent (VE/VO2), and CO2
ventilatory equivalent (VE/VCO2). Some of these variables have been
described in the literature as predictors of the prognosis of individuals with
HF. Values of VE/VCO2 less than 35 mL·kg-1·min-1
indicate the worst prognosis in these individuals [1,6].
Although the CPET is the gold standard for HF, many
individuals have difficulties in being evaluated by a maximum test, especially
those who are more impaired, unfit, or elderly. The equipment required for this
test is expensive and requires specialized staff. Furthermore, the maximum
exercise performed may not reflect the difficulties of individuals with HF in
performing daily activities [4]. Thus, the CPET may not be the most appropriate
test to assess the functional capacity of these individuals in situations of
lower effort.
The 6MWT has been proposed as another tool for the
assessment of the physical capacity of individuals with HF. It is a safe, valid
(r = 0.687, p < 0.001) [7], and reliable test. It is easily performed, has
low costs, and predicts the survival of individuals with the disease [6]. The
effort during the 6MWT is described as similar to activities of daily living,
enabling the individual to determine the walking rhythm he/she tolerates; this
is an advantage for those with a greater degree of impairment who would not
tolerate the CPET [2,3,6,8,9,10,11,12]. The main variable analyzed in the 6MWT is the
distance walked [6]. In addition, the speed is assessed and the hemodynamic
response to effort is analyzed (HR, BP, and SpO2).
Based on previous evidence, both the 6MWT and the CPET
are indicated to assess functional capacity and establish the prognosis of
individuals with HF [3,6]. However, in the Brazilian population, few studies
have correlated the variables obtained in both tests [13]. In a recent study, Carvalho
et al. [13] verified the reproducibility of the 6MWT in a sample of
Brazilian individuals with HF and correlated the VO2peak obtained by
the CPET with the variables of the 6MWT. No correlations with other
cardiorespiratory variables of important prognostic value for HF, such as
VE/VCO2, were established. Therefore, more studies that investigate
the correlation between the variables used in the CPET and the 6MWT are
necessary in order to confirm the similarity of the results of both tests when
performed on individuals with HF. Furthermore, it is important to analyze if
the existing submaximal tests, such as the 6MWT, are sensitive enough to
stratify individuals with different functional capacity levels.
The present study aimed to verify the correlation
between the variables used in the 6MWT and the CPET in a Brazilian sample of
individuals with HF, attended at the public health service, as well as analyze
if the 6MWT is sensitive enough to differentiate between individuals of the New
York Heart Association (NYHA) functional classes I, II, and III.
Methods
Sample
A transversal study, approved by the Ethics in
Research Committee of the Universidade Federal de
Minas Gerais (Protocol number 050/09), was conducted. Individuals with HF
having symptoms that indicated effort limitation (NYHA classes I, II and III),
independent of gender and ethnic group, were included. Individuals with HF were
selected by convenience in an ambulatory cardiology service associated with the
institution.
The study included individuals aged between 30 and 59
years with the following characteristics: presence of HF for at least 6 months,
as confirmed by the ambulatory cardiology service; clinically stable condition
for at least 2 months prior to the study; left ventricular ejection fraction
(LVEF) at rest < 45%, recently assessed by the bidimensional echocardiogram
(up to 6 months); and classification as NYHA class I, II, or III and HF stage
C, according to the American College of Cardiology/American Heart Association
guidelines [14]. The individuals included in the study were prescribed
optimized doses of beta-blockers [15,16], ECA inhibitors [15], or angiotensin
receptor blockers and had a body mass index (BMI) < 30 kg/m2.
Individuals who did not meet the criteria that define
the effort test as maximum [6], who presented a peripheral oxygen saturation
(SpO2) lower than 85% during exercise, or who presented any type of
complication such as the flu or a cold, hospital admission, or alterations in
medication prescription between the CPET and the 6MWT were excluded from the
study.
Procedures and data collection
The volunteers attended LabCare.
After signing the written consent form, they were assessed by the CPET (Medical
Graphics® CPX Ultima, Miami, FL, USA) on a treadmill (Millenium
Classic CI®, Inbramed/Inbrasport,
Brazil) using a ramp protocol [17], according to the Brazilian Cardiology
Society on Ergometric Test Guidelines, in order to determine the
cardiorespiratory parameters. During the test, HR was monitored by an
electrocardiogram (Welch Allyn® Cardioperfect, USA)
connected to an ergospirometer. Blood pressure was
measured using a sphygmomanometer (Diasyst®, São José
dos Campos, SP, Brazil) and a stethoscope (Litmann
Classic II S.E 3M®, USA). SpO2 was continuously measured by an
oximeter (Model 300 Series MEDIAD INC., California, USA) connected to the ergospirometer. The subjective effort perception for
dyspnea and lower limb fatigue was assessed by the modified Borg scale.
After a minimum interval of 48 h and a maximum of 6
months, the volunteers returned to LabCare to perform
the 6MWT. The test was performed in a 30-m-long hallway, where the volunteer
was instructed to walk the longest distance possible in 6 min, without running
or trotting. The route was delimited by plastic cones and standard encouraging
phrases, such as “very good, go on” and “let’s go, continue walking as fast as
possible,” were given every minute [11,18]. Before and after the test, blood
pressure was measured using a sphygmomanometer (Diasyst®,
São José dos Campos, SP, Brazil) and a stethoscope (Litmann
Classic II S.E 3M®, USA). The subjective effort perception for dyspnea and
lower limb fatigue was assessed at the end of the test by the modified Borg
scale. The SpO2 was continuously measured during the test by an
oximeter (Ohmeda Tuffsat®),
and the HR by a cardiofrequencimeter (Polar S810®).
The test was interrupted if any of the following
criteria were observed: precordial pain, unbearable dyspnea, oxygen saturation
lower than 85%, muscle cramps, limping gait, discomfort, or dizziness and
paleness [19]. Two tests, with a 15-min interval between them, were performed.
If the difference between the distance walked in the tests was higher than 10%,
a third test was performed [11,18]. Data obtained from the 6MWT were registered
in a patient identification form, which contained personal data and information
on life habits.
Variables
Although the CPET provides information on the
cardiorespiratory system’s response to effort, the variables with higher
interest for this study were VO2peak (primary variable), VE/VCO2,
and PO2 (secondary variables). The distance walked was the primary
variable obtained by the 6MWT with most interest. The following variables were
considered secondary variables: speed, HR, and walking performance
(distance/HR). All these variables were studied in order to establish a
correlation between the tests.
Statistical analysis
Data were presented as measures of central tendency
and dispersion. Data distribution was analyzed by the Shapiro–Wilk test. The
correlations were performed using the Pearson correlation coefficient or the
Spearman correlation coefficient, for variables with normal and non-normal
distribution, respectively. One-way ANOVA was used to compare the 6MWT
variables between NYHA functional classes I, II, and III. In all statistical
tests, alpha values of 5% were considered significant. The software Statistical
Package for the Social Sciences® (SPSS, Chicago, IL, USA) version 17.0 was used
for data analysis.
Results
Seventeen individuals (5 women and 12 men) with HF (3
NYHA class I, 8 class II, and 6 class III) participated in the study, with an
average age of 48.09 ± 12.91 years (95% CI = 39.42–56.76), LVEF of 44% ± 11%
(95% CI = 0.36 - 0.51), and BMI of 25.86 ± 2.86 kg/m2 (95% CI =
23.93–27.98). Data from the results obtained for the CPET and 6MWT are shown in
Table I.
Table I - Results of the variables assessed in the
cardiopulmonary exercise test and the 6-minute walking test (N = 17)
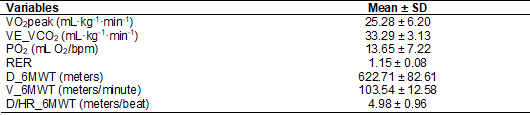
SD = standard deviation; VO2peak = oxygen
consumption at peak effort; VE/VCO2 = ventilatory equivalent for
carbon dioxide; PO2 = oxygen pulse; RER = respiratory exchange rate;
D_6MWT = distance walked in the 6-minute walking test; V_6MWT = velocity
obtained in the 6-minute walking test; D/HR = walking performance
Significant and strong correlations were found between
speed and distance walked in the 6MWT and VO2peak and between
walking performance (D_6MWT/PR) and PO2 (Table II).
Table II - Correlation between the variables of the
6-minute walking test and the cardiopulmonary exercise test
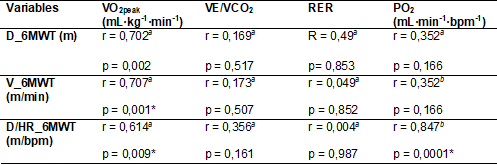
VO2peak = oxygen consumption at peak
effort; VE/VCO2 = ventilatory equivalent for carbon dioxide; RER =
respiratory exchange rate; PO2 = oxygen pulse; D_6MWT = distance
walked in the six-minute walking test; V_6MWT = velocity obtained in the
6-minute walking test; D/HR = walking performance. a = Pearson correlation
coefficient; b = Spearman correlation coefficient; * = p < 0.005
Significant differences were found between NYHA
functional classes with respect to the distance walked in the 6MWT, speed
obtained in the 6MWT, and walking performance (Table III).
Table III - Comparison of the variables of the 6-minute
walking test between the different NYHA functional classes
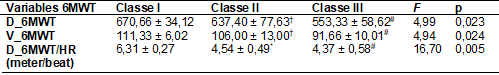
Mean ± SD; SD = standard deviation; D_6MWT = distance
walked in the 6-minute walking test; V_6MWT = velocity obtained in the 6-minute
walking test; D/HR= walking performance. Class I = no symptomatology; Class II
= symptoms during daily activities; Class III = symptoms during small efforts;
F = ANOVA; * = p < 0.05 between classes I and II; # = p < 0.05 between
classes I and III; † = p < 0.05 between classes II and III
There were no significant differences between the
individuals from different NYHA functional classes in relation to age, BMI, and
LVEF.
Discussion
The main finding of the present study was the strong
correlation between the distance walked and the speed reached in 6MWT and the
VO2peak obtained in CPET; this demonstrated the ability of 6MWT to
objectively assess the functional capacity of individuals with HF, especially
considering that the sample represents individuals assisted by the public
health service.
Standard tests are useful to compare and document
changes in the functional capacity of an individual through time [2]. In
individuals with HF, 6MWT has been a submaximal test widely used to assess the
degree of limitation to exercise. The advantages of this test, such as
simplicity, viability, and insignificant cost, have been repeatedly reported
[2,3,6,8,9,10,11,12]. Moreover, since it is a submaximal test in which the individual
determines the walking rhythm he or she tolerates, it has been suggested that
the 6MWT is highly applicable to activities of daily living.
Several authors have assessed the use and clinical
applicability of the 6MWT in different populations with diverse levels of
severity [6,12,20,21,22,23,24,25,26,27]. The present study assessed individuals with HF of mild
severity (VO2max > 20 mL·kg-1·min-1),
according to the classification proposed by Weber [28].
The results of the present study agree with the
findings of Guazzi et al. [3], who assessed
253 individuals with HF NYHA classes II and III. In their study, the distance
walked in the 6MWT was strongly correlated with the VO2peak (r =
0.788; p = 0.001), and there was a weak, but significant, correlation between
the 6MWT and VE/VCO2 (r = 0.46; p = 0.001). Moreover, the distance
walked in the 6MWT decreased significantly with the progression of the
functional classes proposed by Weber et al. [28].
Other authors have also verified these correlations by
finding similar results. Cahalin et al. [20]
assessed 45 individuals with HF and obtained correlations of moderate magnitude
between the distance walked in the 6MWT and VO2peak (r = 0.64; p =
0.001). According to these authors, the 6MWT was a strong predictor for the
occurrence of undesirable events, such as death and hospitalization. Compared
to individuals who walked longer distances, individuals who walked less than
300 meters in the 6MWT showed an increased death risk in 6 months. A study by Pulz et al. [27] assessed the ability of submaximal
tests, such as the 6MWT and the shuttle walking test (SWT), in predicting a
decrease in O2 consumption and establishing a prognosis in
individuals with HF. Significant correlations were found between VO2peak
and the distance walked in the 6MWT (r = 0.76; p = 0.001) and the SWT (r =
0.79; p = 0.001). The sensitivity of both tests in predicting reduced levels of
O2 consumption (VO2max < 14 mL·kg-1·min-1)
was 490 m, predominantly in individuals with mild functional impairment (Weber
classes A and B), and submaximal tests were not considered good predictors of
mortality in this population.
Although other authors have also reported significant
correlations between the distance in the 6MWT and other cardiorespiratory
variables with important prognostic value, such as VE/VCO2 [3,20],
the results of the present study did not exhibit these correlations. A larger
number of individuals with HF may be necessary to reach a sufficient size to
obtain statistical significance. The sample calculation of the present study
considered the number of individuals necessary to establish a correlation
between the 6MWT and VO2peak of the CPET, the primary variables of
the study.
Another CPET variable with clinical prognostic and
mortality value for HF is PO2 [29,30,31]. PO2 is considered one of the
most important variables assessed by ergospirometry.
The variable is related to the systolic volume and the arteriovenous O2
difference, representing an indirect index of the O2 transport at
each cardiac systole [31,32,33]. In our study, the walking performance variable
showed a strong correlation with the PO2 determined by ergospirometry and may be related to the tissue efficiency
in using the offered O2. In other populations, such as individuals
with peripheral obstructive arterial disease, this variable has been used to
infer the cardiovascular conditioning [34] and is a variable of interest in the
assessment of therapeutic interventions. Thus, if an individual is able to walk
a longer distance while reaching lower HR values after physical training, it
can be inferred that the physical capacity has been enhanced.
Functional capacity has shown a significant
correlation with HF severity [35]. A simple and widely used method to quantify
the impact of HF on the individual’s daily life is the classification proposed
by NYHA. According to this classification, individuals with HF can be
categorized into 1 of 4 classes according to the intensity of the symptoms and
the degree of limitation in performing daily activities [1]. The NYHA
functional classification is a subjective estimation of the individual’s real
functional capacity and is significantly correlated with the objective measure
of VO2 determined by the CPET [36].
The CPET is sensitive enough to differentiate between
individuals of NYHA functional classes I, II, and III [36]; however, limited
data are available on the sensitivity of the 6MWT in stratifying individuals
from different functional classes. In the present study, it was possible to
observe significant differences between NYHA functional classes I and III, and
between classes II and III in the comparisons that involved distance and speed
in the 6MWT. No significant differences were found between classes I and II.
This finding may be related to the fact that individuals from functional
classes I and II are in the initial stages of the disease, when there are fewer
repercussions for functional capacity. Another aspect that may have contributed
to the limitation of the 6MWT in stratifying these individuals was the overall
percentage of NYHA I individuals, which was considered relatively small (17%)
when compared to the other functional classes. A significant difference was
observed between classes I and II for the variable of walking performance. This
finding may be explained by the fact that this variable has additional distance
values compared to the HR data. This may have increased the variable’s
sensitivity and ability to stratify these individuals, even in initial stages
of the disease when there are fewer negative repercussions for function.
One limitation of our study was that the sample was
composed predominantly of individuals with HF and mild functional impairment
(Weber classes A and B). Therefore, other studies are necessary to demonstrate
such results in individuals with HF and moderate-to-severe functional
impairment.
Conclusion
In the present study, the 6MWT correlated with the
direct measure of VO2peak (gold standard for functional capacity
assessment) and was able to stratify individuals with different levels of
functional capacity according to the classification proposed by NYHA. Thus, the
6MWT proved to be a simple and valid clinical tool for the assessment of
individuals with HF, and with special external validity for individuals
assisted by the public health service.
Conflict of interest
There are no conflicts of interest.
Financing
There was no funding.
Authors' contribution:
Conception and design of the research: Ferreira ACC and Pereira DAG; Data collection: Ferreira ACC and
Oliveira DMD; Analysis and interpretation of data: Ferreira ACC,
Oliveira DMD and Pereira DAG; Statistical analysis: Ferreira ACC and
Pereira DAG; Manuscript writing: Ferreira ACC and Oliveira DMD; Critical
review of the manuscript for important intellectual content: Faria VC and Pereira DAG
References
- Comitê Coordenador da
Diretriz de Insuficiência Cardíaca. Diretriz Brasileira de Insuficiência
Cardíaca Crônica e Aguda. Arq Bras
Cardiol. 2018;111(3):436-539. doi: 10.5935/abc.20180190 [Crossref]
- Braunschweig F, Linde C, Adamson PB, Magalski A, Erdmann E, Kjellstrom B, Bennett T. Continuous central haemodynamic measurement during the six-minute walk test and daily life in patients with chronic heart failure. Eur J Heart Fail. 2009;11:594-601. doi: 10.1093/eurjhf/hfp045 [Crossref]
- Guazzi M, Dickstein K, Vicenzi M, Arena R. Six-Minute Walk Test and Cardiopulmonary Exercise Testing in patients with chronic heart failure: a comparative analysis on clinical and prognostic insights. Circ Heart Fail. 2009;2:549-555. doi: 10.1161/CIRCHEARTFAILURE.109.881326 [Crossref]
- Bittner V. Exercise testing in heart failure. Maximal, submaximal, or
both? J Am Coll Cardiol. 2003;42:123-5. doi: 10.1016/s0735-1097(03)00501-1 [Crossref]
- Arena R, Myers J, Guazzi M. The clinical importance of cardiopulmonary exercise testing and aerobic training in patients with heart failure. Braz J Phys Ther. 2008;12:75-87. doi: 10.1590/S1413-35552008000200002 [Crossref]
- Guimaraes GV, Bellotti G, Bacal F, Mocelin A, Bocchi EA. Can the Cardiopulmonary 6-Minute Walk Test reproduce the usual activities of patients with heart failure? Arq. Bras. Cardiol. 2002;78:557-60. doi: 10.1590/S0066-782X2002000600003 [Crossref]
- Hamilton DM, Haennel RG. Validity and reability of the 6-Minute Walk Test in a cardiac rehabilitation population. J Cardiopulm Rehabil. 2000;20:156-164. doi: 10.1097/00008483-200005000-00003 [Crossref]
- Pinna G, Opasich C. Reproducibility of the six-minute walking test in chronic heart failure patients. Stat Med. 2000;19:3087-94. doi: 10.1002/1097-0258(20001130)19:22<3087::aid-sim628>3.0.co;2-g [Crossref]
- Enright P. The Six-Minute Walk Test. Respir Care [Internet]. 2003 [cited
2022 Feb 20];48:783-5. Available from:
https://pubmed.ncbi.nlm.nih.gov/12890299/
- Faggiano P, D´aloia A, Gualene A, Brentana L, Dei Cas L. The 6 minute walking test in chronic heart failure: indications, interpretation and limitations from a review of the literature. Eur J Heart Fail. 2004;6:687-91. doi: 10.1016/j.ejheart.2003.11.024 [Crossref]
- Britto RR, Sousa LAP. Teste
de caminhada de seis minutos uma normatização brasileira Six Minute Walk Test –
A Brazilian Standardization.
Fisioter Mov [Internet].
2006 [cited 2022 Feb 21];19:49-54. Available from:
https://pesquisa.bvsalud.org/portal/resource/pt/lil-469101
- Rubim VSM, Neto CD, Romeo JLM, Montera MW. Valor prognóstico do teste de caminhada de seis minutos na insuficiência cardíaca. Arq Bras Cardiol. 2006;86:120-5. doi: 10.1590/S0066-782X2006000200007 [Crossref]
- Carvalho EEV, Costa DC, Crescêncio JC, Santi GL, Papa V, Marques F, et al. Insuficiência cardíaca: comparação entre o teste de caminhada de seis minutos e o teste cardiopulmonar. Heart failure: comparison between six-minute walk test and cardiopulmonary test. Arq Bras Cardiol. 2011;97:59-64. doi: 10.1590/S0066-782X2011005000056 [Crossref]
- Heidenreich PA, Fonarow GC, Breathett K, Jurgens CI, Pisani BA, Pozehl
BJ, et al. 2020 ACC/AHA Clinical performance and quality measures for adults
with heart failure. A report of the American College of Cardiology/American
Heart Association Task Force on Performance Measures. Circ Cardiovasc Qual
Outcomes. 2020;11. doi: 10.1161/HCQ.0000000000000099 [Crossref]
- Kell R, Haunstetter A, Dengler TJ, Zugck C, Kübler W, Hass M. Do cytokines enable risk stratification to be improved in NYHA functional class III patients? Eur Heart J. 2002;23:70-8. doi: 10.1053/euhj.2001.2780 [Crossref]
- Nessler J, Nessler B, Kitliński M, Gackowski A, Piwowarska W, Stepniewski M.
Concentration of BNP, endothelin 1, pro-inflamatory
cytokines (TNF-α, IL-6) and exercise capacity in patients with heart
failure with carvedilol. Kardiol Pol [Internet]. 2008
[cited 2022 Feb 21];66:144-51. Available from: https://pubmed.ncbi.nlm.nih.gov/18344152/
- Pereira DAG, Vieira DSR,
Samora GAR, Lopes FL, Alencar MCN, Lage SM, Pereira VF, Velloso M, Moreira MCV,
Britto RR. Reprodutibilidade da determinação do Limiar Anaeróbico em Pacientes
com insuficiência cardíaca. Arq Bras
Cardiol. 2010;94:771-8. doi: 10.1590/S0066-782X2010005000044 [Crossref]
- ATS Statement: Guidelines for the six-minute walk test. Am J Cri. Care Med. 2002;166:111-7. doi: 10.1164/ajrccm.166.1.at1102 [Crossref]
- Rondelli RR, Oliveira AN,
Corso SD, Malaguti C. Uma atualização e proposta de padronização do teste de
caminhada dos seis minutos. Fisioter Mov.
2009;22:249-59.
- Cahalin LP, Mathier MA, Semigran MJ, Dec GW, DiSalvo TG. The six-minute walk test predicts peak oxigen uptake and survival in patients with advanced heart failure. Chest. 1996;110:325-32. doi: 10.1378/chest.110.2.325 [Crossref]
- Miyamoto S, Nagaya N, Satoh T, Kyotani S, Sakamaki F, Fujita M, et al. Clinical correlates and prognostic significance of six-minute walk test in patients with primary pulmonary hypertension. comparison with cardiopulmonary exercise testing. Am J Respir Crit Care Med. 2000;161:488-92. doi: 10.1164/ajrccm.161.2.9906015 [Crossref]
- Zugck C, Krüger C, Dürr S, Gerber SH, Haunstetter A, Hornig K, et al. Is the 6-minute walk test a reliable substitute for peak oxygen uptake in patients with dilated cardiomyopathy? Eur Heart J. 2000;21:540-4. doi: 10.1053/euhj.1999.1861 [Crossref]
- Demers C, McKelvie RS, Negassa A, Yusuf S. Reliability, validity, and responsiveness of the six-minute walk test in patients with heart failure. Am Heart J. 2001;142:698-703. doi: 10.1067/mhj.2001.118468 [Crossref]
- Opasich C, Pinna GD, Mazza A, Febo O, Riccardi R, Riccardi PG, et al. Six-minute walking performance in patients with moderate-to-severe heart failure Is it a useful indicator in clinical practice? Eur Heart J. 2001;22:488-96. doi: 10.1053/euhj.2000.2310 [Crossref]
- Rodrigues SL, Mendes HF, Viegas CAA. Six Minutes Walk Test: Study of the effect of learning in
chronic obstructive pulmonary disease patients. J Bras Pneumol.
2004;30:121-5. doi: 10.1590/S1806-37132004000200008 [Crossref]
- Casas JRA, Vilaro J, Rabinovich R, Mayer A, Barberà J, Roisin RR. Encouraged 6-min walking test indicates maximum sustainable exercise in COPD patients. Chest. 2005;128:55-61. doi: 10.1378/chest.128.1.55 [Crossref]
- Pulz C, Diniz R, Alves A, Tebexreni A, Carvalho A, Paola A, Almeida D. Incremental shuttle and six-minute walking tests in the assessment of functional capacity in chronic heart failure. Can J Cardiol. 2008;24:131-5. doi: 10.1016/s0828-282x(08)70569-5 [Crossref]
- Weber KT, Kinasewitz GT, Janicki JS, Fishman AP. Oxigen utilization and ventilation during exercise in patients with chronic cardiac failure. Circulation. 1982;65:1213-23. doi: 10.1161/01.cir.65.6.1213 [Crossref]
- Lavie CJ, Milani RV, Mehra MR. Peak exercise oxygen pulse and prognosis in chronic heart failure. Am J Cardiol. 2004;93:588-93. doi: 10.1016/j.amjcard.2003.11.023 [Crossref]
- Costa RV, Junior AO, Serra
SM, Nóbrega ACL. Respostas ventilatórias e do pulso de oxigênio ao exercício
dinâmico: correlação com a massa muscular esquelética em portadores de
insuficiência cardíaca crônica avaliados pela ergoespirometria.
Revista da SOCERJ
[Internet]. 2005 [cited 2022 Jun 13];18:283-7.
Available from:
http://sociedades.cardiol.br/socerj/revista/2005_04/a2005_v18_n04_art01.pdf
- Oliveira RB, Myers J, Araujo CG, Arena R, Mandic S, Bensimhon D, et al. Does peak oxygen pulse complement peak oxygen uptake in risk stratifying patients with heart failure? Am J Cardiol. 2009;104:554-8. doi: 10.1016/j.amjcard.2009.04.022 [Crossref]
- Serra S. Considerações sobre
ergoespirometria. Arq Bras Cardiol [Internet]. 1997;68:301-4. Available from:
http://publicacoes.cardiol.br/abc/1997/6804/68040014.pdf
- Stein R. Teste
cardiopulmonar de exercício: noções básicas sobre o tema. Revista da Sociedade
de Cardiologia do Rio Grande do Sul [Internet]. 2006 [cited 2022
June 13];15:1-4. Available from:
http://sociedades.cardiol.br/sbc-rs/revista/2006/09/Artigo_01_Teste_Cardiopulmonar.pdf
- Stewart KJ, Hiatt WR, Regensteiner JG, Hirsch
AT. Exercise training for claudication. The N Engl J
Med. 2002;24:1941-9. doi: 10.1056/NEJMra021135 [Crossref]
- Mady C, Salemi VMC, Ianni BM, Ramires FJA, Arteaga E. Maximal functional capacity, ejection fraction, and functional class in chagas cardiomyopathy. are these indices related? Arq Bras Cardiol. 2005;84:152-5. doi: 10.1590/S0066-782X2005000200011 [Crossref]
- Russell SD, Saval MA, Robbins JL, Ellestad MH, Gottlieb SS, MD, Handberg EM, et al. New York Heart Association functional class predicts exercise parameters in the current era. Am Heart J. 2009;158:24-30. doi: 10.1016/j.ahj.2009.07.017 [Crossref]