Rev Bras Fisiol Exerc. 2022;21(6):352-64
doi: 10.33233/rbfex.v21i6.5410
ORIGINAL ARTICLE
Hypotension after high-intensity interval exercise
with elastic resistance: a pilot study
Hipotensão
pós-exercício intervalado de alta intensidade com resistência elástica: um
estudo piloto
Redley da Silva Alves, Leticia Nascimento
Santos Neves, Victor Hugo Gasparini Neto, Luciana Carletti
Universidade
Federal do Espírito Santo, Vitória, ES, Brazil
Received: September 14, 2022; Accepted: December 3,
2022.
Correspondence: Redley da Silva Alves, E-mail: redley.alves@edu.ufes.br
How to cite
Silva RS, Neves LNS, Gasparini Neto VH, Carletti L. Hypotension
after high-intensity interval exercise with elastic resistance: a pilot study. Rev Bras
Fisiol Exerc. 21(6):352-64. doi: 10.33233/rbfex.v21i6.5410
Abstract
Introduction: It is
established that continuous aerobic training reduces post-exercise blood
pressure, known as hypotension post-exercise. Traditional ergometers such as
treadmills and cycle ergometers are commonly used as resources for training.
However, they are expensive and this limits access to the general population.
An alternative is to use elastic resistance running. However, it is not known
whether the application of a high-intensity interval training session, with
elastic resistance, presents favorable post-exercise acute hemodynamic
responses. Objective: To describe and compare the hemodynamic responses
in the recovery of an interval training session performed on the treadmill and
with elastic resistance performed at the same intensity. Methods: Four
healthy adults (24.25 ± 2.75 years old) performed a session of high-intensity
interval training on a treadmill and another session with elastic resistance at
85% of VO2max, with an interval of one week between them and a
control situation. Before and after the sessions, hemodynamic variables were
monitored for 60 minutes: systolic blood pressure, diastolic blood pressure,
heart rate, stroke volume, cardiac output, and peripheral vascular resistance
monitored by infrared photoplethysmography (Finometer).
Results: Interval training with elastic resistance decreased systolic
blood pressure and peripheral vascular resistance concerning the control day.
Comparing the protocols, only elastic resistance caused post-exercise
hypotension (p < 0.05), for up to 40 minutes. Conclusion: The
protocol with elastic resistance promoted post-exercise hypotension for SBP and
reduced peripheral vascular resistance.
Keywords: high intensity interval training;
post-exercise hypotension; hemodynamic monitoring.
Resumo
Introdução: Está estabelecido que o treinamento
aeróbio contínuo reduz a PA no pós-esforço, conhecido como hipotensão
pós-exercício. Ergômetros tradicionais como esteiras e cicloergômetros
são comumente utilizados como meio de treinamento. Eles são caros e isso limita
o acesso à população em geral. Uma alternativa é o uso da corrida com
resistência elástica. Entretanto não se sabe se a aplicação de uma sessão de
treinamento intervalado de alta intensidade, com resistência elástica,
apresenta respostas hemodinâmicas agudas favoráveis pós-exercício. Objetivo:
Descrever e comparar as respostas hemodinâmicas na recuperação de uma sessão de
treinamento intervalado realizada na esteira e a com resistência elástica
realizadas na mesma intensidade. Métodos: Quatro adultos (24,25 ± 2,75
anos) saudáveis executaram uma sessão de treinamento intervalado de alta
intensidade na esteira ergométrica e outra sessão com resistência elástica a
85% do VO2máx, com intervalo entre eles de uma semana e uma situação
controle. Antes e após as sessões, foram monitoradas as variáveis hemodinâmicas
por 60 minutos: pressão arterial sistólica, pressão arterial diastólica,
frequência cardíaca, volume sistólico, débito cardíaco e resistência vascular
periférica monitorados por fotopletismografia por
infravermelho (Finometer). Resultados: O
treinamento intervalado com resistência elástica apresentou resposta
hemodinâmica aguda significativa com a queda da pressão arterial sistólica e da
resistência vascular periférica em relação ao dia controle. Comparando os
protocolos, apenas a resistência elástica causou hipotensão pós-exercício (p
< 0,05), por até 40 minutos. Conclusão: O protocolo com resistência
elástica promoveu hipotensão pós-exercício com queda da pressão arterial
sistólica acompanhada de redução da resistência vascular periférica.
Palavras-chave: treinamento intervalado de alta
intensidade; hipotensão pós-exercício; monitoramento hemodinâmico.
Introduction
The regular practice of physical
exercises exerts positive effects on the cardiovascular, neuromuscular, and
respiratory systems [1]. For patients in clinical conditions, they are even
more effective or act synergistically with drug treatment, minimizing the
negative clinical effects of some diseases [2]. High-intensity interval
training (HIIT) is a modality that has gained prominence, as it presents
evidence that it is a time-efficient therapy to improve the cardiometabolic
health profile of individuals with or without risk of metabolic disease, even
in the absence of weight loss [3]. HIIT is characterized by repeated “near
maximal” efforts (e.g., ≥ 90% HRmax
or ≥ 85% VO2peak) and periods of active or passive recovery [4].
Different HIIT protocols are presented in the literature and advocated to
promote benefits in physical fitness [5] and health [6,7]. However, these
studies are limited to the ergometers use, such as treadmills and bicycles,
which are equipped with limited access to the general population, and this can
reduce adherence.
A presented proposal by our group
was the interval exercise practiced in the form of brisk walking or running
with elastic resistance by older women [8]. In this study, favorable acute
effects of post-exercise hypotension (PEH) and glycemic control were observed
in recovery for up to 60 minutes (min).
Investigating immediate responses
to exercise recovery is important, as this information can describe a state of
vulnerability [9] when there is no recovery of hemodynamic variables at a
normal pace, as is the case of heart rate (HR) recovery [10], or a substantial
drop in diastolic blood pressure (DBP) that can reduce myocardial perfusion
[11]. On the other hand, recovery is a phase of opportunity to enhance the
stimuli imposed by physical effort, culminating in autonomic adjustments that
favor the reduction of peripheral vascular resistance (PVR) and systolic blood
pressure (SBP) [9]. HIIT also seems to be more favorable, in terms of
hypotensive response, than continuous moderate-intensity training, as it has a
higher post-exercise excessive oxygen consumption (EPOC) and a higher rate of
accumulated heat [12]. This response may favor the reduction of SBP and,
consequently, the systolic volume (SV) for thermal regulation [12].
Furthermore, it is a type of effort that promotes greater vascular shear stress
during exercise that is associated with better vascular adaptations, increasing
arterial compliance, for example [13,14,15].
HIIT has been a highly acclaimed
method to promote physiological adaptations beneficial to health, but
incremental tests that used elastic resistance indicate a change in the
characteristic of muscle contraction, as it requires a strength component and
even a more exacerbated eccentric phase of contraction [16]. This more intense
request of the muscular system by the elastic resistance can interfere with the
hemodynamic responses to the exercise [17], causing a more exacerbated PEH by
adding the mechanical and metabolic effects of the exercise [18]. Therefore, it
is necessary to clarify whether the elastic resistance application combined
with cardiorespiratory work, as in high-intensity interval training with
elastic resistance (EL-HIIT), presents a more exacerbated acute hypotensive
response than HIIT on a treadmill.
Therefore, the objective was to
describe the pressure and hemodynamic response after a single session of
EL-HIIT compared to traditional HIIT performed on a treadmill.
Methods
This is a cross-sectional study,
supplementary to the OBHIIT project (Obesity Research in High-Intensity
Interval Training), registered in PRPPG nº 93906/2019. The project was approved
by the Ethics Committee for Research with Human Beings of the Federal
University of Espírito Santo (CAAE nº
09109319.2.0000.5542). All participants were informed of the risks and benefits
of the research and consented to participate by signing the informed consent
form (TCLE).
Sample
The characteristics of the
participants are presented in Table I. There were four participants (3 men and
1 woman), healthy young people (BMI ≥ 18 and ≤ 25 kg·m-2),
aged between 18 and 35 years, physically active (≥ 150 min/ week of
physical exercise), free of cardiometabolic diseases and without declared use
of dietary supplements or anabolic steroids. Participants were selected through
invitations and disclosures on social networks. All were assessed by a
physician before inclusion in the survey. In addition, they answered a
questionnaire to assess signs and symptoms of disease, use of medication,
family history of chronic non-communicable diseases, and characterization of
the level of physical activity (IPAQ, short version).
Table I – Characteristics of the
participants
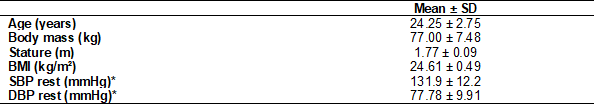
Data presented as mean ± Standard
Deviation. BMI = Body Mass Index; SBP = Systolic Blood Pressure; DBP =
Diastolic Blood Pressure. *Values referring to the control
Anthropometric assessment and body composition
Body mass and height were measured
using a digital anthropometric scale and a one-millimeter precision stadiometer
(Marte Científica, L200,
São Paulo) with a maximum capacity of 210 kg and sensitivity of 50 g. All
procedures were performed by the same evaluator.
Experimental procedures
Each participant visited the
Exercise Physiology laboratory (LAFEX/NUPEM/UFES) on 4 occasions with intervals
of at least 1 week (Figure 1). The visits consisted of Cardiopulmonary Exercise
Test (CPET) and medical anamnesis (day 1), Cardiopulmonary Exercise Test with
Elastic Resistance (CPET) (day 2), and HIIT or EL-HIIT session (days 3 and 4)
organized in a randomized way. Before and after the HIIT and EL-HIIT sessions,
the hemodynamic variables SBP, DBP, HR, SV, PVR, and Cardiac Output (CO) were
collected. Before the procedures of the first or second week, the BP was
measured in the Finometer® for 60 minutes to have the
reference of the control day.
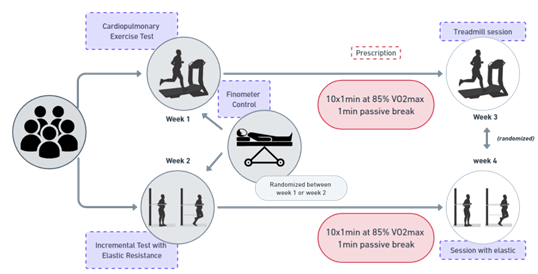
Figure 1 – Experimental study procedures
Pre-assessment care and guidance
Participants were instructed not to
perform physical activities the day before and on the day of the test, to eat
two hours before the stress tests, to present themselves with appropriate
clothing for the tests to be performed, not to drink any energy drink (coffee
or others) on the day of the assessments and not to show up for the assessments
with symptoms that may be associated with COVID-19.
Cardiopulmonary Exercise Test (CPET)
In a silent, air-conditioned room
(21 and 24ºC), blood pressure (BP) was measured following the recommendations
of the 2020 Brazilian Guidelines on Arterial Hypertension [19]. The
participants were instructed on the procedures for carrying out the test, which
included: remaining breathing normally; not using the handrail of the treadmill
as a support during the test, unless necessary; requesting interruption of the
test, in case of chest pain or any other discomfort that prevents the
continuation of the test. The test was performed on a motorized treadmill (Inbra Sport Super ATL, Porto Alegre, Brazil) following an
individualized ramp protocol, aiming at a duration between 10 and 12 min. The
speed was gradually increased until the individual reached exhaustion.
Participants started at a 4 km/h warm-up (3 min) with increments of 1 km/h
every minute, with a 1% incline.
The ventilatory variables were
measured using a metabolic gas analyzer (Cortex Metalyzer
3B model, Germany), with breath-by-breath collection, and then 20-second
averages were calculated and analyzed using the Metasoft
program. The Cortex unit was calibrated by the closed-loop method, using
calibration gas (original 16% O2 and 5% CO2 cylinder,
supplied by the manufacturer). To identify the test as maximum, we analyzed the
following criteria: a) voluntary exhaustion; b) Maximum HR attained of at least
90% of that predicted by age (220-age); c) respiratory exchange ratio equal to
or above 1.05 [20]. The VO2max was extracted between the highest
values of the final 30 seconds of the test.
Elastic Resistance Cardiopulmonary Exercise Test (EL-
CPET)
The EL-CPET environment was the
same as previously described for CPET, as well as the procedures for measuring
BP. All participants were instructed about the test procedures. The EL-CPET was
performed on a rubberized mat marked with 11 lines of 5 cm thick and separated
by spaces of 30 cm between one and the other. The rug measures 4.50 m high x
1.00 m wide. Lines painted in different colors (white and black) comprise
stages 1 to 10 (Figure 2). Two meters of silver elastic tubing (®Thera-band
Tubing, Malaysia) was used, wrapped in an eyelet, and fixed by a steel cable to
a stainless steel support bar.
The protocol was explained and
familiarized before running the session. The belt was adjusted at the height of
the iliac crest, allowing the participant to run forward and backward, changing
stages with constant feedback from the researchers. After a 3 min warm-up, the
test consisted of gradual increments every 1 min. During the test, participants
were encouraged to follow the rhythm emitted by a metronome (Cellphone
application – ®Cifraclub). They were encouraged to
maintain a rhythm of 180 bpm during warm-up and 200 bpm in the following stages.
If the individual reached the last stage and did not become exhausted, 10 bpm
were added until exhaustion. Ventilatory variables and oxygen consumption (VO2)
were measured as described in CPET. This test was proposed by Gasparini-Neto et al. [16].
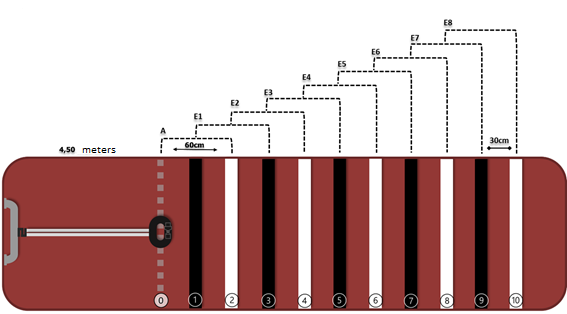
Rubberized mat with a length of
4.50 meters, marked with 11 lines (0-10) – 30 cm between lines. Heating (0) and
eight stages (E1 to E8) – 60 cm between stages, interspersed with black and
white colors. H = Heating; S = stage
Figure 2 – Schematic model of a mat for
incremental testing with elastic resistance
HIIT session on treadmill
Initially, the participant remained
at rest in the lying position (dorsal decubitus) for 10 min and 60 min
post-exercise for each measurement of the hemodynamic variables. Soon after,
the mask was adjusted for ventilatory measures. Ten series of exercises lasting
one minute were performed at 85% of the VO2max determined in CPET,
with a passive interval of one minute between series, protocol 10 x 60s: 60s –
adapted from Little et al. [5]. All were verbally encouraged during the
effort.
EL-HIIT session
Initially, the volunteer remained
at rest in the lying position (dorsal decubitus) for 10 min and 60 min
post-exercise for each measurement of the hemodynamic variables. Soon after,
the mask was adjusted for ventilatory measures. Ten series of exercises lasting
one minute were performed, prescribed at 85% of the VO2max
determined by the EL-CPET (according to the stage of the mat corresponding to
85% of the VO2max), and one minute of passive interval between the
series, protocols 10 x 60s: 60s – adapted from Little et al. [5].
Hemodynamic analysis
In a quiet room with low lighting,
participants lay on a stretcher. After a 5-min rest in the supine position, BP
monitoring was performed using infrared photoplethysmography with a Finometer® monitor (Finapres
Medical System, BV Netherlands) on a control day, and on two more days, before
and after the training session (10 min at rest and 1 hour after exercise, lying
down). BP was measured on the right arm due to the positioning of the room and
equipment, certified to be positioned at heart level, as recommended by the
equipment itself. For the acquisition of pressure curves, the cuff was placed
on the middle finger, which takes into account the age, body mass, height, and
gender of the participant. To calculate the post-exercise hemodynamic
differences between the protocols, the net effect of exercise was calculated as
the difference between the responses in the exercise and the control situation
[(post-exercise BP – pre-exercise BP) – (post-control BP – BP pre-control)]
[21]. For the analyses, the variables presented in the software (Beat Scope®
software) were considered: Systolic Blood Pressure (SBP), Diastolic Blood
Pressure (DBP), Heart Rate (HR), Systolic Volume (SV), Cardiac Output (CO) and
Peripheral Vascular Resistance (PVR).
Statistical analysis
Data are presented as mean ±
standard deviation and tested for normality using the Shapiro-Wilk test. All
data were tabulated and double-checked by independent researchers. For effect
size (ES), Cohen's d was used [22], classified as: ≤ 0.49 small effect;
0.50 – 0.79 moderate effect; 0.80 – 1.29 large effect; > 1.30 very large
effect [22]. To analyze the differences in hemodynamic parameters, a two-way
ANOVA of repeated measures with post hoc Bonferroni correction (time points vs.
protocols) was used. The software used for static analysis was IBM/SPSS v.
20.0. p < 0.05 was considered.
Results
Table II presents the CPET and
EL-CPET parameters applied before the protocols. The load corresponding to the
percentage of 85% of HRmax was
used for the prescription of training sessions.
Table II – Maximum parameters of
cardiopulmonary tests
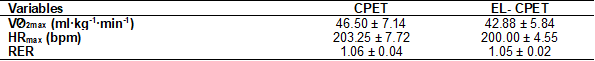
Data
presented as mean ± standard deviation. HRmax = Maximum heart rate;
RER = Respiratory exchange ratio; CPET = Cardiopulmonary treadmill exercise
test; EL- CPET = Cardiopulmonary resistance exercise test; VO2max =
Maximum oxygen consumption
Hemodynamic response: comparison with the control
group
The values obtained during the
control compared to the post-exercise ones are presented in Table III. After
the EL-HIIT session, the SBP presented a decrease in relation to the control at
20 min (12.7%), 30 min (11.8%), and 40 min (7.1%), with very large ES (1.70,
1.72, and 0.82, respectively). DBP was lower only at 30 min (5.2%) of EL-HIIT
with large ES (0.81). HR showed higher values at 20 min (35.7%), 30 min
(29.4%), 40 min (19.1%), 50 min (21.2%), 60 min (16.4%), and 70 min (13.4%)
with large and very large ES (1.17, 2.00, 1.28, 1.71, 1.43, and 1.09,
respectively). SV exhibited higher values at 20 min (6.3%), 30 min (4.8%), and
50 min (4.2%) post-exercise, with large ES (1.13, 0.88, and 0. 88,
respectively). CO values were higher at 20 min (22%), 60 min (11.3%), and 70
min (13.2%) with large ES (1.11, 0.94, and 1.21, respectively), and in the 30th
(11.6%), 40th (9.3%), and 50th (11.6%) minutes, the CO tended to increase in
relation to the control, with a moderate ES (0.64, 0.57, and 0 .75,
respectively). PVR decreased from 20 min (24.7%) to 30 min (13.6%), and at 50 min
(9.6%), 60 min (8.3%), and 70 min (7.9%) with ES from very large to large
(1.46, 0.87, 0.90, 1.02, and 1.16, respectively); and at 40 min (10.4%) with
moderate ES.
Table III – Acute physiological responses
after sessions
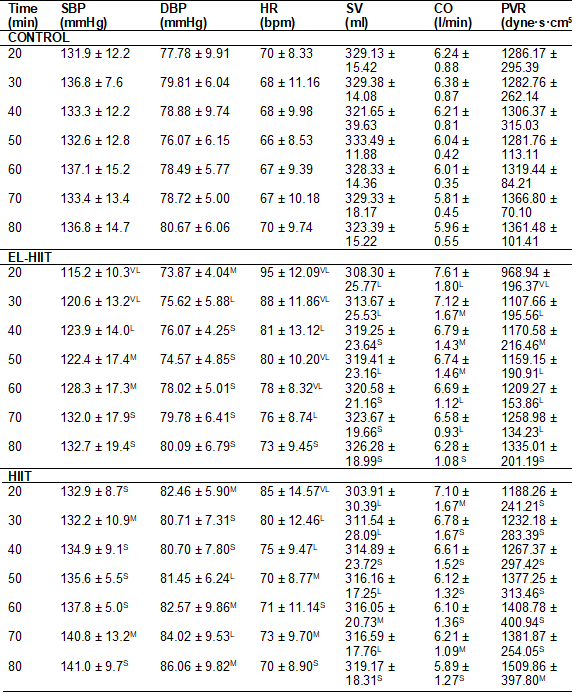
Data presented as mean ± standard
deviation; CO = Cardiac Output; HR = Heart Rate; DBP = Diastolic Blood
Pressure; SBP = Systolic Blood Pressure; PVR = Peripheral Vascular Resistance;
Effect size compared to control day, where S = small ≤ 0.49; M = moderate
≥ 0.50 – 0.79; L = large ≥ 0.80 – 1.29; VL = very large > 1.30;
SV = Systolic Volume
In HIIT, SBP showed a reduction of
(3.4%) and (5.5%) at moments 30 and 70 min after exercise with moderate ES
(0.57 and 0.64, respectively) (Table III). DBP remained higher at minutes 50
(7.1%) and 70 (6.7%) with large ES (1.00 and 0.80, respectively); and at 20 min
(6%), 60 min (5.1%) and 80 min (6.7%) with moderate ES (0.59; 0.10 and 0.10,
respectively). HR remained elevated at minutes 20 (21.4%), 30 (17.6%), and 40
(10.3%), with ES ranging from large to very large (1.45; 1.17 and 0.83,
respectively); and at minutes 50 (6%) and 70 (9%) moderate ES was observed
(0.53 and 0.68, respectively). The SV showed higher values at 20 min (7.7%), 30
min (5.4%), 50 min (5%), and 70 min (3.9%), a large ES (1.20; 0. 92; 1.06 and
0.81, respectively). CO and PVR did not differ compared to the control moment.
Post-exercise hemodynamic differences between EL-HIIT
and HIIT
SBP (Fig. 3 – A) was significantly
lower (p = < 0.05) in EL-HIIT at 20 min (p = 0.021), 30 min (p = 0.012), and
40 min (p = 0.035), showing differences in mmHg of 11.43, 10.93, and 4.15,
respectively. For DBP (Fig. 3 - B), there was no statistical difference between
the protocols. CO values (Fig. 3 - C) were lower in EL-HIIT at 60 min with a
difference of 0.56 L/min (p = 0.022) and a downward trend at 70 min (p =
0.054). HR (Fig. 3 - D) tended to remain higher in EL-HIIT at 30 min (p =
0.059), 40 min (p = 0.053), 50 min (p = 0.055), 60 min (p = 0.059), and 80 min
(p = 0.053). For PVR (Fig. 3 - E), the EL-HIIT modality was significantly
different from HIIT (p = 0.009), showing differences (dyne·s·cm5) with
reductions of 212.75 in 20 min (p = 0.005), 70.62 at 30 min (p = 0.003), and
18.13 at 50 min (p = 0.008).
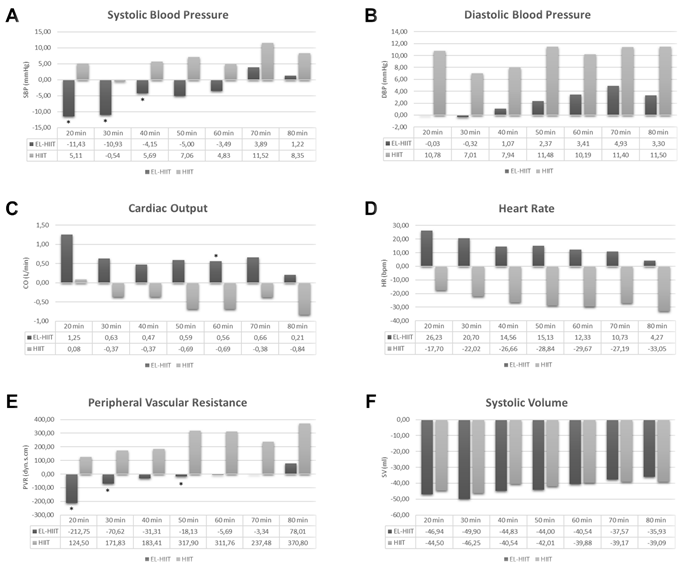
Differences *(p = < 0.05) of hemodynamic
variables in post-exercise. A) Systolic Blood Pressure; B) Diastolic Blood
Pressure; C) Cardiac Output; D) Heart Rate; E) Peripheral Vascular Resistance;
and F) Systolic Volume
Figure 3 - Post-exercise hemodynamic
differences between EL-HIIT vs. HIIT protocols
Discussion
This study aimed to describe and
compare post-exercise hemodynamic responses in normotensive healthy young
subjects submitted to two different HIIT protocols. We noticed that EL-HIIT
presented a more evident acute hemodynamic response, with a drop in SBP and PVR
and maintenance of high HR and CO, compared to the control situation in effect
size. While for HIIT, only high HR and SV were observed in relation to the
control.
Comparing the post-exercise
hemodynamic response between the protocols, the main findings were that a
single session of EL-HIIT caused a reduction in SBP during 40 min
post-exercise, as well as for CO and PVR, compared to HIIT, with no effect on
DBP, HR, and SV. This is the first study that observed PEH using EL-HIIT as a
means of exercising, including the gold standard method usage of blood pressure
analysis by infrared photoplethysmography.
The PEH presented in our findings
corroborates the results that have been previously observed in young individuals
after an exercise session. Angadi et al. [23]
monitored BP in recreationally active young people for 3 hours and observed a
longer-lasting PEH (4 mmHg reduction in SBP) after long HIIT performed on a
cycle ergometer close to the maximum (90-95% HRmax)
compared to continuous exercise (75-80% HRmax).
Dantas et al. [24] reported that a single
low-volume HIIT session (10 x 1 min at 100% of maximum treadmill speed
interspersed with 1 min of recovery) was able to reduce SBP (3 to 5 mmHg)
during the first 5 hours post-exercise in normotensive men. Thus, it is
observed that there is favorable evidence in the literature for the
post-exercise hypotensive response in young people who perform HIIT sessions on
the treadmill or the cycle ergometer. On the other hand, our results broaden
the view on exercise with elastic resistance since it seems to potentiate PEH,
which is linked to a pronounced decrease in BP [25]. However, our results are
only evidence to start exploring the topic since this is a pilot study, and it
was not possible to reproduce the PEH observed in traditional HIIT reported in
previously published studies.
The main novelty of this study was
to show that EL-HIIT caused a more pronounced hypotensive response compared to
HIIT in four young, healthy normotensive individuals of both sexes. Our
findings also show a possible relationship with the drop in PVR, which only
happened in the EL-HIIT modality. The reduction in vascular resistance seems to
be one of the main hemodynamic variables that determine PEH [12,26,27]. The
reduction in systemic vascular resistance can be caused by sustained
post-exercise vasodilation in the lower limbs [26]. The occurrence of this
phenomenon is mediated by complex interactions between local [28] and neural
[27] vasodilator mechanisms, such as the re-establishment of the baroreflex,
which, through sympathoinhibition, will decrease the sympathetic flow leading
to vasoconstriction and activation of histamine receptors resulting in
sustained vasodilation and helping to reduce vascular resistance [14]. However,
there is no information about the associated mechanisms of PEH promoted by
EL-HIIT. Thus, further studies are needed to clarify its post-exercise
hemodynamic responses.
Another factor that may be related
to the more evident hypotensive response is the mechanical demand exerted
during exertion. Stavres et al. [18] reported
that concentric exercise provided greater PEH in healthy young men and women,
compared to eccentric exercise, probably due to metabolic stress combined with
work. Therefore, it is speculated that the type of effort generated running
back and forth performed in EL-HIIT may cause greater vascular shear stress due
to increased blood flow toward the active muscle after EL-HIIT vs. HIIT, which
has been associated with better vascular adaptations [13,15] and consequently
strength-related benefits [16]. More studies should objectively explore the
strength component after the different protocols.
The present study also expands the
tool options for prescribing physical exercise in healthy young men and women.
Pressure response after a single exercise session is considered a simple
predictive clinical resource to manage training prescriptions [9]. Based on our
findings, it is possible to speculate that in the EL-HIIT modality, individuals
will be more responsive to the stimulus [26] to obtain greater assertiveness in
the training prescription. However, these are still speculative findings.
Despite the promising results of
this study, some limitations need to be mentioned. First, the study was carried
out with only four healthy young people, which prevents extrapolations to other
age groups and hypertensive and pre-hypertensive individuals. Therefore,
studies with larger sample sizes, with other publics and age groups, are
necessary. Second, hemodynamic variables were obtained over a short period (80
min), so further investigations should assess responses over longer periods.
Finally, even though there were guidelines for individuals not to practice
physical activity the day before the sessions, nor to drink energy drinks, we
did not assess these factors objectively. On the other hand, our findings pave
the way for new hypotheses and studies that use elastic resistance as a
physical exercise tool.
Conclusion
EL-HIIT promoted PEH with a drop in
SBP accompanied by PVR. These findings suggest EL-HIIT may be a new tool for
exercising in healthy young men and women with beneficial effects on the
cardiovascular system.
Academic affiliation
This article is the result of the
Institutional Scientific Initiation Program of the Federal University of Espírito Santo (UFES), by undergraduate student Redley da Silva Alves, supervised by Professor Luciana Carletti, PhD in Physiological Sciences, UFES.
Conflict of interests
All authors are responsible for the
content of the manuscript and approved its final version. No commercial party
that supports this article and has a direct financial interest in the research
results confers or will confer financial benefits on the authors or any
organization with which the authors are associated. The authors declare that
there are no known competing financial conflicts of interest or personal
relationships that may have influenced the work reported in this article.
Funding
This work was carried out with the
support of the National Council for Scientific and Technological Development – CNPq (Proc. 148613/2021-7).
Authors´contributions
Conception and design
of the research: Carletti
L, Neves LNS, Gasparini-Neto VH; Obtaining data:
Neves LNS, Gasparini-Neto VH; Data analysis and
interpretation: Alves RS, Neves LNS, Carletti L,
Gasparini-Neto VH; Statistical analysis: Alves
RS, Neves LNS; Obtaining financing: Carletti
L; Writing of the manuscript: Alves RS, Carletti
L, Neves LNS, Gasparini-Neto VH; Critical review
of the manuscript for important intellectual content: Alves RS, Carletti L, Neves LNS, Gasparini-Neto
VH.
References
- Garber CE, Blissmer B,
Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, et al. Quantity and quality of
exercise for developing and maintaining cardiorespiratory, musculoskeletal, and
neuromotor fitness in apparently healthy adults: Guidance for prescribing
exercise. Med Sci Sports Exerc. 2011;43:1334-59. doi: 10.1249/MSS.0b013e318213fefb [Crossref]
- Pedersen BK, Saltin B. Exercise as medicine - Evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand J Med Sci Sports. 2015;25:1-72. doi: 10.1111/sms.12581 [Crossref]
- Sabag A, Little JP, Johnson NA. Low-volume high-intensity interval training for cardiometabolic health. J Physiol. 2022;600:1013-26. doi: 10.1113/JP281210 [Crossref]
- Buchheit M, Laursen PB. High-intensity interval training, solutions to the programming puzzle: Part I: Cardiopulmonary emphasis. Sports Med. 2013;43:313-38. doi: 10.1007/s40279-013-0029-x [Crossref]
- Little JP, Safdar A, Wilkin GP, Tarnopolsky MA, Gibala MJ. A practical model of low-volume high-intensity interval training induces mitochondrial biogenesis in human skeletal muscle: Potential mechanisms. J Physiol 2010;588:1011-22. doi: 10.1113/jphysiol.2009.181743 [Crossref]
- Clark A, De AB, Rosa L, Derevere JL, Todd , Astorino A. Effects of various interval training regimes on changes in maximal oxygen uptake, body composition, and muscular strength in sedentary women with obesity. Eur J Appl Physiol. 2019;119:879-88. doi: 10.1007/s00421-019-04077-x [Crossref]
- Kong Z, Sun S, Liu M, Shi Q. Short-term high-intensity interval training on body composition and blood glucose in overweight and obese young women. J Diabetes Res. 2016;e4073618. doi: 10.1155/2016/4073618 [Crossref]
- Gasparini-Neto VH, Caldas LC, Lira CAB, Carletti L, Leite RD, Nikolaidis PT, et al. Profile of blood pressure and glycemic responses after interval exercise in older women attending (in) a public health physical activity program. J Bodyw Mov Ther. 2021;25:119-25. doi: 10.1016/J.JBMT.2020.10.011 [Crossref]
- Luttrell MJ, Halliwill JR. Recovery from exercise: Vulnerable state, window of opportunity, or crystal ball? Front Physiol. 2015;6:204. doi: 10.3389/FPHYS.2015.00204/BIBTEX [Crossref]
- Okutucu S, Karakulak UN, Aytemir K, Oto A.
Heart rate recovery: a practical clinical indicator of abnormal cardiac
autonomic function. Expert Rev Cardiovasc Ther. 2011;9(11):1417-30. doi: 101586/Erc11149 [Crossref]
- Negrão
CE, Barretto ACP, Rondon MUPB. Cardiologia do
exercício: do atleta ao cardiopata. São Paulo: Manole; 2010.
- Morales-Palomo F, Ramirez-Jimenez M, Ortega JF, Pallarés JG, Mora-Rodriguez R. Acute hypotension after High-Intensity Interval Exercise in metabolic syndrome patients. Int J Sports Med. 2017;38:560-7. doi: 10.1055/s-0043-101911 [Crossref]
- Green DJ, Hopman MTE, Padilla J, Laughlin MH, Thijssen DHJ. Vascular adaptation to exercise in humans: Role of hemodynamic stimuli. Physiol Rev. 2017;97:495-528. doi: 10.1152/PHYSREV.00014.2016 [Crossref]
- Halliwill JR, Buck TM, Lacewell AN, Romero SA. Hot Topic Review Hot Topic Review Postexercise hypotension and sustained post-exercise vasodilatation: what happens after we exercise? Exp Physiol. 2013;98:7-18. doi: 10.1113/expphysiol.2011.058065 [Crossref]
- Williams JS, Giudice M, Gurd BJ, Pyke XKE. Reproducible improvement in endothelial function following two separate periods of high-intensity interval training in young men. J Appl Physiol. 2020;129:725-31. doi: 10.1152/jappl [Crossref]
- Gasparini Neto VH, Santos Neves LN, Kalva-Filho CA, Schwingel PA, Leite RD, Carletti L. Exercise testing with elastic resistance: a new reproducible proposal for determination of ventilatory thresholds and maximum oxygen consumption. J Sports Sci Med. 2022;21:426-34. doi: 10.52082/jssm.2022.426 [Crossref]
- Keir DA, Copithorne DB, Hodgson MD, Pogliaghi S, Rice CL, Kowalchuk JM. The slow component of pulmonary O2 uptake accompanies peripheral muscle fatigue during high-intensity exercise. J Appl Physiol. 2016;121:493-502. doi: 10.1152/JAPPLPHYSIOL.00249.2016 [Crossref]
- Stavres J, Fischer SM, McDaniel J. Exaggerated post exercise hypotension following concentric but not eccentric resistance exercise: Implications for metabolism. Eur J Sport Sci. 2019;19:983-93. doi: 10.1080/17461391.2018.1564368 [Crossref]
- Barroso WKS, Rodrigues CIS, Bortolotto LA, Mota-Gomes MA, Brandão AA, Feitosa ADM, et al. Diretrizes Brasileiras de Hipertensão Arterial - 2020. Arq Bras Cardiol. 2021;116:516-658. doi: 10.36660/abc.20201238 [Crossref]
- Slawinski JS, Billat VL. Difference in mechanical and energy cost between highly, well, and nontrained runners. Med Sci Sports Exerc. 2004;36:1440-6. doi: 10.1249/01.MSS.0000135785.68760.96 [Crossref]
- Fecchio RY, Chehuen M, Brito LC, Peçanha T, Queiroz ACC, Moraes Forjaz CL. Reproducibility (Reliability and Agreement) of Post-exercise Hypotension. Int J Sports Med. 2017;38:1029-34. doi: 10.1055/s-0043-118009 [Crossref]
- Santo HE, Daniel FB. Calcular e apresentar tamanhos do efeito em trabalhos científicos (1): As limitações do p < 0,05 na análise de diferenças de médias de dois grupos. Revista Portuguesa de Investigação Comportamental e Social 2015;1:3-16. doi: 10.7342/ISMT.RPICS.2015.1.1.14 [Crossref]
- Angadi SS, Bhammar DM, Gaesser GA. Postexercise hypotension after continuous, aerobic interval, and sprint interval exercise. J Strength Cond Res. 2015;29:2888-93. doi: 10.1519/JSC.0000000000000939 [Crossref]
- Dantas TCB, Farias LF, Frazão DT, Silva PHM, Sousa AE, Costa IBB, et al. A single session of low-volume high-intensity interval exercise reduces ambulatory blood pressure in normotensive men. J Strength Cond Res 2017;31:2263-9. doi: 10.1519/JSC.0000000000001688 [Crossref]
- Marçal IR, Goessler KF, Buys R, Casonatto J, Ciolac EG, Cornelissen VA. Post-exercise hypotension following a single bout of high intensity interval exercise vs. a single bout of moderate intensity continuous exercise in adults with or without hypertension: a systematic review and meta-analysis of randomized clinical trials. Front Physiol. 2021;12:863. doi: 10.3389/FPHYS.2021.675289/BIBTEX [Crossref]
- Costa EC, Dantas TCB, de Farias LF, Frazão DT, Prestes J, Moreira SR, et al. Inter- and intra-individual analysis of post-exercise hypotension following a single bout of high-intensity interval exercise and continuous exercise: a pilot study. Int J Sports Med. 2016;37:1038-43. doi: 10.1055/S-0042-112029/ID/R5575-0030 [Crossref]
- Cote AT, Bredin SSD, Phillips AA, Koehle MS, Warburton DER, Phillip K, et al. Greater autonomic modulation during post-exercise hypotension following high-intensity interval exercise in endurance-trained men and women. Eur J Appl Physiol. 2015;115:81-9. doi: 10.1007/s00421-014-2996-5 [Crossref]
- Lee SK, Kim CS, Kim HS, Cho EJ, Joo HK, Lee JY, et al. Endothelial nitric oxide synthase activation contributes to post-exercise hypotension in spontaneously hypertensive rats. Biochem Biophys Res Commun. 2009;382:711-4. doi: 10.1016/J.BBRC.2009.03.090 [Crossref]