Rev Bras Fisiol Exerc. 2024;23(2):e235414
doi: 10.33233/rbfex.v23i2.5414
REVIEW
Effects of preoperative physical training on functional capacity in
esophageal surgery: a systematic review
Efeitos do treinamento
físico pré-operatório na capacidade funcional em cirurgia esofágica: revisão
sistemática
Cleomara Pereira dos Santos1, Ramon
Martins Barbosa2, Alan Carlos Nery dos Santos2, Renata
Ferreira de Moura3, Jefferson Petto2, Welton
Cardoso dos Santos1, Lais Oliveira Santos1, Vinicius
Afonso Gomes2
1Universidade Salvador (UNIFACS),
Salvador, BA, Brazil
2Escola Bahiana de Medicina e Saúde
Pública (EBMSP), Salvador, Brazil
3Instituto Dante Pazzanese de
Cardiologia, Salvador, Brazil
Received: March 8,
2023; Accepted: July 29, 2024.
Correspondence: Cleomara
Pereira dos Santos, clleo.pereiras@gmail.com
How to cite
Santos CP, Barbosa RM, Santos
ACN, Moura RF, Petto J, Santos WC, et al.. Effects of preoperative
physical training on functional capacity in esophageal surgery: a systematic
review. Rev Bras Fisiol Exerc. 2024;23(2):e235514.
doi: 10.33233/rbfex.v23i2.5414
Abstract
Introduction: Physical training is essential to improve
cardiorespiratory function and muscle strength, directly impacting patients'
functional capacity. Esophageal surgery, often performed in cases of cancer, is
associated with high risks of morbidity and mortality. Objective: To
summarize evidence on the effects of physical training on the functional
capacity of individuals in the preoperative period of esophageal surgery. Methods:
Systematic review in the Pubmed, VHL, EBSCOhost, Scielo and PEDro databases.
Two independent reviewers carried out the search and selection of studies using
the terms “Preoperative”, “Esophageal” and “Surgery Training”. Randomized
clinical trials focused on physical training programs for patients in the
preoperative period of esophageal surgery were included. The risk of bias of
the studies was assessed using the PEDro scale. Results: The initial
search identified 188 articles, of which three were considered eligible,
covering a total sample of 149 patients, with 71.71% being men. The exercise
programs ranged from inspiratory muscle training to aerobic and neuromuscular
exercises, lasting 2 to 3 weeks. The majority of patients undergoing esophageal
surgery had been diagnosed with cancer. Analysis of the studies indicated a
moderate to low risk of bias. Conclusion: The evidence suggests that
physical training in the preoperative period of esophageal surgery can improve
functional capacity, muscle strength and cardiorespiratory function. In
addition, these benefits may contribute to a reduction in pulmonary complications,
reintubations and length of hospital stay.
Keywords: functional status; exercise therapy; esophageal
neoplasms
Resumo
Introdução: O treinamento físico é fundamental
para melhorar a função cardiorrespiratória e a força muscular, impactando
diretamente a capacidade funcional dos pacientes. A cirurgia esofágica,
frequentemente realizada em casos de câncer, está associada a altos riscos de
morbidade e mortalidade. Objetivo: Sumarizar evidências sobre os efeitos
do treinamento físico na capacidade funcional de indivíduos no pré-operatório
de cirurgia esofágica. Métodos: Revisão sistemática nas bases de dados Pubmed, BVS, EBSCOhost, Scielo e PEDro. Dois revisores
independentes realizaram a busca e seleção dos estudos usando os termos "Preoperative", "Esophageal"
e "Surgery Training". Foram incluídos
ensaios clínicos randomizados focados em programas de treinamento físico para
pacientes no pré-operatório de cirurgia esofágica. O risco de viés dos estudos
foi avaliado pela escala PEDro. Resultados: A
busca inicial identificou 188 artigos, dos quais três foram considerados
elegíveis, abrangendo uma amostra total de 149 pacientes, com 71,71% sendo
homens. Os programas de exercícios variaram entre treinamento muscular
inspiratório, exercícios aeróbicos e neuromusculares, com duração de 2 a 3
semanas. A maioria dos pacientes submetidos à cirurgia esofágica tinha
diagnóstico de câncer. A análise dos estudos indicou um risco de viés de
moderado a baixo. Conclusão: As evidências sugerem que o treinamento
físico no pré-operatório de cirurgia esofágica pode melhorar a capacidade
funcional, força muscular e função cardiorrespiratória. Além disso, esses
benefícios podem contribuir para a redução de complicações pulmonares, reintubações e tempo de internação hospitalar.
Palavras-chave: estado funcional; terapia por
exercício; neoplasias esofágicas
Introduction
Esophageal surgery (ES) is a complex procedure associated
with high risks of morbidity and hospital mortality [1]. Its importance in
clinical practice is indisputable, and it is often used for both curative and
palliative treatment of various conditions, especially esophageal cancer. In
2016, the National Cancer Institute (INCA) estimated the occurrence of 10,810
new cases of esophageal neoplasia in Brazil, predominantly in older
individuals, especially in the 6th and 7th decades of life [2]. Among the main
risk factors are alcohol consumption, hot drinks and smoking [3].
In the clinical scenario, people with esophageal
involvement usually present with symptoms such as dysphagia and significant
weight loss, which significantly reduces their functional and metabolic
reserves. Furthermore, in the post-operative period of esophagectomy, a further
decline in cardiovascular, pulmonary and muscular function can be observed,
resulting in a marked decrease in functional capacity (FC) and quality of life.
These events make it urgent to identify therapeutic strategies for the recovery
and rehabilitation of the public in question [4,5,6,7].
In this sense, physical training (PT) in the preoperative
period has been shown to be a promising intervention to increase the functional
reserve of patients who will undergo ES. Studies indicate that exercise
training can bring significant benefits from pre- to post-surgery, helping to
improve muscle and cardiopulmonary function [8,9]. Physiologically, PT improves
FC by promoting adaptations in the muscular and respiratory systems [10]. These
effects are particularly noticeable in the increase in maximum oxygen
consumption (VO2peak) and in the strengthening of the inspiratory
muscles, which translates into improvements in peripheral O2 extraction,
dyspnea and quality of life [1,11,12].
However, despite the biological plausibility and possible
clinical benefits, there is still a significant gap in knowledge about the
specific effects of exercise training in the preoperative period of ES.
Understanding these effects is crucial for the development and adoption of
strategies aimed at optimizing the recovery and rehabilitation of these
patients. Therefore, this study aimed to summarize evidence on the effects of
preoperative physical exercise on the functional capacity of individuals undergoing
esophagogastric cancer surgery.
Methods
Type of study
This study is a systematic review, based on the criteria established by the
Preferred Reporting Items for Systematic Reviews and Meta-Analyses - PRISMA
[13], to answer the PICO question: “What are the effects of physical training
on functional capacity during the preoperative period of esophageal surgery?”. The study was registered with PROSPERO under opinion: CRD42021229289.
Eligibility criteria
In order to carry out this systematic review, specific inclusion and
exclusion criteria were established to ensure the selection of relevant,
high-quality studies.
Inclusion criteria: We only included randomized clinical trials. We
considered studies that investigated the effects of preoperative physical
training programs, such as aerobic, resistance or combined programs. The
population of interest included hospitalized adult patients (≥ 18 years)
who were preparing for esophagogastric cancer surgery, covering both esophageal
and gastric cancer. The interventions were to be carried out exclusively in the
preoperative period, i.e. before surgery, to focus on the specific effects of
physical training during this crucial phase. We considered studies that
evaluated outcomes related to functional capacity, such as VO2max
and the six-minute walk test, as well as the incidence of postoperative
complications and recovery time. There were no restrictions on language or
publication period, allowing the inclusion of studies from any year and
language to provide a comprehensive view of the available evidence.
Exclusion criteria: We excluded studies involving participants under the
age of 18, as physiology and response to exercise training can differ
significantly between adults and children. We also excluded studies that
included additional associated clinical procedures in the preoperative period,
such as concomitant chemotherapy or radiotherapy, to avoid confounding the
results attributed exclusively to physical training. Theses, master's or
doctoral dissertations and other academic papers that were not published in
peer-reviewed scientific journals were also excluded, to ensure that only
studies that had undergone a rigorous review process were considered. In
addition, studies that did not report the outcomes of interest, such as
functional capacity, postoperative complications or recovery time, were
excluded, as these data are essential for answering the review question.
Finally, duplicate studies or those with insufficient data for extraction and
analysis were excluded to maintain the integrity of the review and avoid bias.
Outcome of interest
Functional capacity (FC) is defined in terms of abilities
and independence to perform certain activities. For the purpose of this study,
FC is considered in relation to the performance of the individual's
cardiopulmonary and muscular functions [14].
Search strategy
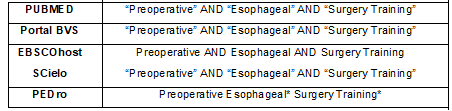
The searches were carried out in the Pubmed, VHL,
EBSCOhost, SCielo and PEDro databases, by two independent authors [C.P.S] and
[V.A.G], between June and November 2022. We used a combination of descriptors
selected from the Medical Subject Headings (MeSH), Health Sciences Descriptors
(DeCS) and keywords: “Preoperative”, “Esophageal”, “Surgery” and “Training”, as
well as their respective synonyms. The specific cross-references for each
database were carried out using the Boolean operators [AND] and [OR], as detailed
in Chart 1.
Chart 1 - Search strategies for the selected databases
Study selection and data extraction
The studies were selected by two independent authors
[C.P.S] and [V.A.G]. In the event of disagreements, a third reviewer [R.M.B]
was consulted. Initially, a thorough reading of the titles and abstracts was
carried out, selecting those that met the previously established eligibility
criteria for the final analysis. As shown in Table I, the eligible studies were
subjected to a complete reading in order to assess the selection criteria and
retrieve the following data: a) Author and year of publication of the study; b)
Main objectives of the study; c) Characteristics of the population (population
sample); d) Intervention protocols (methods of the control and intervention
groups); e) Main results obtained by the studies. The references reviewed and
included in this review were analyzed in order to identify potential studies
not detected in the initial searches in the selected electronic databases.
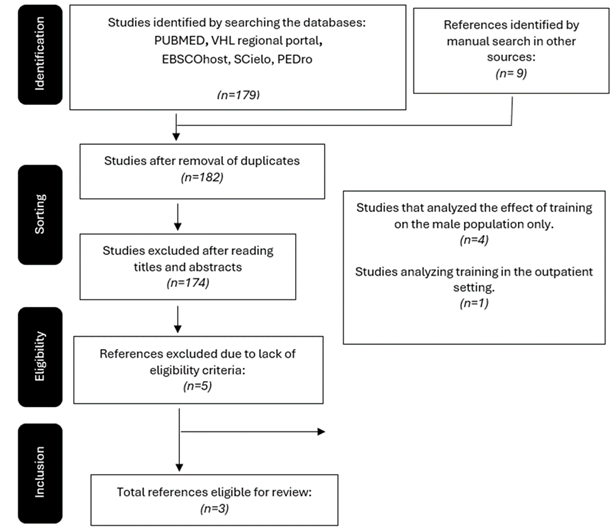
Figure 1 summarizes the strategies for selecting the studies that make up the
scope of this systematic review.
Methodological quality
The quality of the studies was assessed using the PEDro
(Physiotherapy Evidence Database) scale, based on the Delphi list. The PEDro
scale consists of 10 items, each contributing 1 point (except item 1, which is
not scored), resulting in a total score ranging from 0 to 10. This scale
assesses the methodological quality of randomized controlled clinical trials,
focusing on two main aspects: internal validity (credibility of the
observations and results in relation to the reality studied) and the amount of
statistical information sufficient for interpretation. The scale does not
assess the external validity, significance or magnitude of the treatment
effect. The classification of the articles was carried out independently by two
evaluators familiar with the scale. Divergences in the PEDro classification
were discussed between the evaluators and resolved by consensus, establishing
the final score for the studies (Table II). The cut-off point for
distinguishing between studies of high and low methodological quality was
defined as < 6 (low quality) or ≥ 6 (high quality) on the PEDro scale
[15].
Results
The search strategies and manual analysis of the
references returned a total of 188 articles. After the initial review by
authors [C.P.S] and [V.A.G], 6 articles were eliminated due to duplication,
leaving 182 studies. Next, during screening based on the eligibility criteria,
177 studies were excluded after analyzing titles and abstracts, leaving 5
articles for full reading. Subsequently, two (2) of these studies were excluded
because they performed physical training in the preoperative period of esophageal
surgery in an outpatient setting. Finally, three (3) studies met the
eligibility criteria and were included in the review, as summarized in Figure 1
[15,16,17].
Fonte:
os autores
Figura 1 – Flowchart for screening
and selecting articles
As shown in Table I, the included studies aimed to investigate the effects
and aspects of physical training in the preoperative period of esophageal
surgery (ES) [15,16,17]. The total sample of these studies included 145
individuals, of whom 71 were men and 28 women [15,16]. It is worth noting that
the study by Christensen et al. [17] did not differentiate the sample by
sex, so it was not included in the gender distribution. Of these, 68
individuals were allocated to the intervention groups and 77 to the control
groups.
Table I - Characteristics of the selected studies
The methods applied in the control groups varied over
periods of 2 to 3 weeks, with moderate intensity activities and endurance
inspiratory muscle training (IMT-E) [15,16]. In the intervention group,
inspiratory muscle training (IMT) was performed using devices such as the
conical flow resistor and the inspiratory loading device (K3, POWER breathe®)
[15], or through high-intensity inspiratory muscle training (IMT-HI) [16]. The
duration of these interventions was approximately 2 to 3 weeks. In contrast, one
study [17] implemented the intervention with a program of high-intensity
aerobic training and resistance exercises, with sessions held twice a week.
The main results indicate that preoperative physical
training for patients undergoing esophageal surgery provides significant
benefits for the inspiratory muscles [15,16], improved VO2peak and
increased muscle strength [17]. It is important to note that all the
individuals undergoing oesophageal surgery in the studies reviewed had been
diagnosed with oesophageal cancer [15,16,17].
Regarding the risk of bias, the eligible articles ranged
between 5 and 8 points on the PEDro scale, out of a possible 10 points. In the
quality classification, one of the included studies was assessed as “low
quality” [17], while two studies were classified as “high quality” [15,16]. The
average quality of the studies in this review was 7 points on the PEDro scale.
Table II presents a qualitative summary of the original studies included in
this review.
Table II - Risk of Bias Analysis (PEDro Scale)
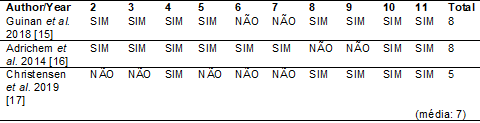
2. Were the
subjects randomly assigned to groups (in a crossover study, the subjects were
randomly assigned to groups according to the treatment they received)? 3. Was
the allocation of subjects secret? 4. Were the groups initially similar with
regard to the most important prognostic indicators? 5. Did all the subjects
participate in the study in a blinded manner? 6. Did all the therapists
who administered the therapy do so in a blinded manner? 7. All evaluators who measured at least
one key outcome
did so in a blinded manner?; 8. Measurements of at least
one key outcome were obtained in more than 85% of the subjects initially
allocated to the groups?; 9. All subjects from whom outcome measurements were
presented received the treatment or control condition as allocated or, when this
was not the case, the data was analyzed for at least one of the key outcomes by
“intention to treat”?; 10. Have the results of the inter-group statistical
comparisons been described?; 11. Does the study present both precision and
variability measures for at least one key outcome?
Discussion
The main results of this study suggest that physical
training (PT) during the preoperative period of esophageal surgery promotes a
significant improvement in functional capacity, positively influencing outcomes
such as cardiopulmonary function and muscle strength. In addition, the main
condition leading to esophagectomy is esophageal cancer [15,16,17].
Previous studies have shown that this neoplasm is highly
aggressive and is considered the sixth leading cause of cancer death worldwide
[2,19,20]. Patients with this disease often have difficulty swallowing, which
can result in weight loss, anemia and dehydration [21,22,23]. In addition, there
are reductions in cardiopulmonary function, physical fitness and the ability to
perform activities of daily living [5,24,25].
A previous review indicated that TF can optimize
patients' vital and inspiratory capacity [25]. This was also observed in the
studies included in this review, which found an improvement in inspiratory
muscle function, peak VO2 and muscle strength [15,16,17]. One study in
particular suggested that intervention with high-intensity inspiratory muscle
training (HI-IMT) may be promising and effective, capable of reducing the
negative impacts of the postoperative period in patients undergoing
esophagectomy, such as pulmonary complications, reintubations and length of
hospital stay, when compared to endurance inspiratory muscle training (E-IMT).
Both training methods showed a significant increase in maximum inspiratory
pressure (MIP) and lung function [16].
Corroborating these findings, one of the included studies
suggested that IMT can improve the patient's inspiratory muscle strength,
expiratory strength and ventilatory function preoperatively, thus reducing the
risk of pulmonary complications after esophagectomy [26]. In contrast, another
study [15] showed that, despite the gains in MIP with the IMT intervention in
the preoperative period, there was no significant influence on the improvement
in functional capacity, which can be explained by the short period of the
intervention, despite the intensity used (60% MIP). Monitoring the
interventions by means of training diaries and weekly phone calls compromised
the ability to accurately assess training adherence and possible problems in
carrying out the interventions.
It is interesting to note that the changes observed may
be associated with specific subgroups of patients, such as those over 70 who
have undergone invasive or open surgical procedures, patients with chronic
obstructive diseases and those with inspiratory muscle strength of less than 70
cmH2O [15]. Based on this hypothesis, it is plausible to suggest that intrinsic
factors, such as age and comorbidities, and extrinsic factors, such as the type
of surgical procedure, can influence the effect of preoperative physical
training.
Another possible training strategy for this population
involves continuous moderate-intensity aerobic exercise and resistance training
[27]. These strategies have been shown to improve the functional capacity of
individuals, as measured by their performance in the 6-minute walk test [27].
In addition, other exercise prescription strategies can influence the
development of physical fitness, strength and quality of life, such as aerobic
training and high-intensity resistance exercises, performed with a focus on
gaining muscle strength using equipment such as leg presses, knee extensions,
bench presses and seated rowing [17]. It is worth noting that some studies show
that regular exercise can prevent the development of certain types of cancer
[26], probably due to important anti-cancer mechanisms associated with this
practice [27].
Furthermore, another relevant finding is that the highest prevalence of
esophageal surgery occurs in men [15,16]. This can be explained by the higher
consumption of tobacco, hot drinks and alcohol by this population [3,18,28].
Although it was not measured in this study, factors related to age, family
history and genetic predisposition may also be associated with the development
of oesophageal cancer [29].
Based on the data presented, there is a need to implement
policies aimed at caring for patients undergoing oesophagectomy, considering
the high prevalence of morbidity and mortality in this subgroup of the
population. Physical training in the preoperative period can increase
functional capacity, improve quality of life and potentially have an impact on
longevity.
Clinical implications
The findings of this systematic review have important
clinical implications for the management of patients undergoing esophageal
surgery for resection of esophageal cancer. Preoperative physical training has
been shown to improve patients' functional capacity, which can translate into
faster recovery and a reduction in postoperative complications. Integrating
physical training programs into preoperative preparation can be a valuable
strategy to optimize patients' physical status before surgery, especially considering
the high complexity and risks associated with esophagectomy. Furthermore, the
adoption of these interventions can contribute to a more holistic and
patient-centered approach, improving quality of life and surgical results.
Healthcare professionals, including surgeons, physical therapists, and
rehabilitation teams, should consider including exercise training regimens into
standard clinical practice for patients with esophageal cancer. This proactive
approach can not only improve the immediate outcomes of surgery, but also
contribute to the overall health and longevity of patients.
Limitations
The limitations of this systematic review should be
considered when interpreting the results. First, the data are specific to
patients undergoing esophageal surgery for cancer resection, limiting
generalizability to other populations or surgeries. Furthermore, the limited
number of studies included may affect the robustness of the conclusions. The
heterogeneity of the training modalities analyzed also complicates the
comparison of results, as different approaches can generate varied responses.
Monitoring training adherence, carried out through diaries and phone calls, can
introduce measurement biases due to dependence on participant accuracy.
Finally, the included studies generally had small sample sizes, which may limit
the detection of significant effects. Despite these limitations, the results
are consistent with existing literature, indicating benefits of preoperative
physical training in complex esophageal surgeries.
Conclusion
The findings of this research demonstrate that physical
training in the preoperative period of esophageal surgery promotes an
improvement in functional capacity, muscle strength and cardiopulmonary
function. This can lead to a reduction in pulmonary complications, the risk of
reintubations and the length of hospital stay. However, further studies with
greater methodological rigor are needed to confirm these results in this
population.
Interest conflicts
No conflicts of interest
Financing source
There was
no funding for the study
Authors' contributions
Conception and
design of the research: Santos CP, Barbosa RM, Moura RF, Gomes VA, Santos
ACN, Petto J; Data collection: Santos CP, Barbosa RM,
Moura RF, Gomes VA, Santos ACN, Petto J; Data analysis
and interpretation: Santos
CP, Barbosa RM, Moura RF, Gomes VA, Santos ACN, Petto J; Data collection: Santos CP, Barbosa RM, Moura RF, Gomes VA,
Santos ACN, Petto J; Manuscript writing:
Santos CP, Barbosa RM, Moura RF, Gomes VA, Santos ACN, Petto J; Data collection: Santos CP, Barbosa RM, Moura RF, Gomes VA,
Santos ACN, Petto J, Santos WC, Santos LO; Critical
review of the manuscript for important intellectual content: Santos CP,
Barbosa RM, Moura RF, Gomes VA, Santos ACN, Petto J; Data collection:
Santos CP, Barbosa RM, Moura RF, Gomes VA, Santos ACN, Petto J, Santos LO,
Santos WC
References
- Patel N, Powell AG, Wheat JR, Brown C, Appadurai IR, Davies RG, et al. Cardiopulmonary fitness predicts
postoperative major morbidity
after esophagectomy for patients with cancer.
Physiol Rep. 2019;7(14). doi: 10.14814/phy2.14112 [Crossref]
- Weston AC, Bonamigo EL,
Braga DC, Andreis B, Sakae TM, Freitas AF, et al.
Sistemas nacionais de transplante – Brasil versus Holanda: aprimoramento para
garantia da continuidade da vida. Rev Bras Transpl. 2020;(8):23–35
- Li S, Chung DC, Mullen JT. Screening high-risk populations for esophageal and gastric cancer.
J Surg Oncol.
2019;120(5):831–46. doi: 10.1002/jso.25656 [Crossref]
- Sinclair RCF, Phillips AW, Navidi M, Griffin SM, Snowden CP. Pre-operative
variables including fitness
associated with complications after oesophagectomy. Anaesthesia.
2017;72(12):1501–7. doi: 10.1111/anae.13987 [Crossref]
- Elliott JA, Doyle SL, Murphy
CF, King S, Guinan EM, Beddy P, et al. Sarcopenia:
Prevalence and impact on operative and oncologic outcomes in the multimodal
management of locally advanced esophageal cancer. Ann Surg. 2017;266(5):822–30. doi: 10.1097/SLA.0000000000002388 [Crossref]
- Valkenet K, Trappenburg JCA, Ruurda JP, Guinan EM, Reynolds JV, Nafteux P, et al. Multicentre randomized clinical trial of inspiratory muscle training versus usual care before surgery for oesophageal cancer. Br J Surg. 2018;105(5):502–11. doi: 10.1002/bjs.10798 [Crossref]
- Bosch DJ, Muijs CT, Mul VEM, Beukema JC, Hospers GAP, Burgerhof JGM, et al.
Impact of neoadjuvant chemoradiotherapy on postoperative course after
curative-intent transthoracic esophagectomy in esophageal cancer patients. Ann
Surg Oncol. 2014;21(2):605–11. doi: 10.1245/s10434-013-3384-x [Crossref]
- Carli F, Gillis C, Scheede-Bergdahl C. Promoting a culture of
prehabilitation for the surgical cancer patient. Acta Oncol (Madr).
2017;56(2):128–33. doi: 10.1080/0284186X.2016.1266081 [Crossref]
- Pouwels S, Hageman D, Gommans LNM, Willigendael EM, Nienhuijs SW,
Scheltinga MR, et al. Preoperative exercise therapy in surgical care: a scoping
review. J Clin Anesth. 2016;33:476–90. doi: 10.1016/j.jclinane.2016.06.032 [Crossref]
- Milliken D, Schofield N. Entendendo a pré-habilitação. World Fed Soc
Anaesthesiol [Internet]. 2018
[citado 2024 Jun 12];1–5. Disponível em:
https://www.wfsahq.org/components/com_virtual_library/media/3f438e4c23829ae6b294abb36e11479a-394-ATOTW-PORTUGUES.pdf
- Guinan EM, Dowds J, Donohoe C, Reynolds JV, Hussey J. The physiotherapist and the esophageal cancer patient: From prehabilitation to rehabilitation. Dis Esophagus. 2017;30(1):1–12. doi: 10.1111/dote.12535 [Crossref]
- Medeiros AIC, Brandão DC,
Souza RJP, Fuzari HKB, Barros CESR, Barbosa JBN, et
al. Effects of daily inspiratory muscle training on respiratory muscle strength
and chest wall regional volumes in haemodialysis patients: a randomised
clinical trial. Disabil Rehabil
[Internet]. 2019;41(26):3173–80. doi: 10.1080/09638288.2018.1485181 [Crossref]
- Itens P, Revis
R, Uma P. Principais itens para relatar revisões sistemáticas e meta-análises:
a recomendação PRISMA. Epidemiol Serv
Saúde. 2015;24(2):335–42. doi: 10.5123/S1679-49742015000200017 [Crossref]
- Ramos LR. Fatores
determinantes do envelhecimento saudável em idosos residentes em centro urbano:
Projeto Epidoso, São Paulo. Cad
Saude Publica. 2003;19(3):793–7. doi: 10.1590/S0102-311X2003000300022 [Crossref]
- Guinan EM, Forde C, Neill LO, Gannon
J, Doyle SL, Valkenet K, et al. Effect of
preoperative inspiratory muscle training on physical functioning following
esophagectomy. Dis Esophagus. 2018;31(9):1–8. doi: 10.1093/dote/doy034 [Crossref]
- Adrichem EJ, Meulenbroek L, Plukker JTM, Groen H. Comparison of two
preoperative inspiratory muscle training programs to prevent pulmonary
complications in patients undergoing esophagectomy: a randomized controlled
pilot study. Dis Esophagus. 2014;27(6):2353–60. doi: 10.1111/dote.12090 [Crossref]
- Christensen JF, Simonsen C, Herrstedt A. Safety and feasibility of
preoperative exercise training during neoadjuvant treatment before surgery for
adenocarcinoma of the gastro-oesophageal junction. Scand J Gastroenterol.
2019;54(1):74–84. doi: 10.1080/00365521.2018.1550318 [Crossref]
- Thrift AP. The epidemic of oesophageal carcinoma: where are we now? Cancer Epidemiol. 2016;41:88–95. doi: 10.1016/j.canep.2016.01.013 [Crossref]
- Monteiro NML, Araújo DF, Bassetti-Soares E, Vieira JPFDB, Santos MRM, Júnior PPLDO, et al. Câncer de esôfago: perfil das manifestações clínicas, histologia, localização e comportamento metastático em pacientes submetidos a tratamento oncológico em um centro de referência em Minas Gerais. Rev Bras Cancerol. 2009;55(1):27–32. doi: 10.32635/2176-9745.RBC.2009v55n1.1673 [Crossref]
- Cunha FMR, Borges MC, Fanan JMV, Oliveira PF, Volpe MS, Crema E. Evaluation of the
effectiveness of preoperative outpatient pulmonary preparation in patients undergoing esophageal surgery. Fisioter Mov. 2018;31:1–10. doi: 10.1590/1980-5918.031.ao20 [Crossref]
- Phelps BJ, Tiley YM, Skrove JL, Berry AC, Mohan K. Acute dysphagia caused by sarcomatoid squamous cell carcinoma of the esophagus. Cureus. 2019;11(2). doi: 10.7759/cureus.4074 [Crossref]
- Fagevik Olsén M, Kjellby Wendt G, Hammerlid E, Smedh U. Effects of a training intervention for enhancing recovery after Ivor-Lewis esophagus surgery: a randomized controlled trial. Scand J Surg. 2017;106(2):116–25. doi: 10.1177/1457496916664361 [Crossref]
- Pereira EEB, Santos NB, Sarges ESNF. Avaliação da capacidade funcional do paciente oncogeriátrico hospitalizado. Rev
Pan-Amazônica Saúde. 2014;5(4):37–44. doi: 10.5123/S2176-62232014000400005 [Crossref]
- Allen S, Brown V, Prabhu P, Scott M, Rockall T,
Preston S, et al. A randomised controlled trial to assess whether
prehabilitation improves fitness in patients undergoing neoadjuvant treatment
prior to oesophagogastric cancer surgery: study protocol. BMJ Open. 2018;8(12). doi: 10.1136/bmjopen-2018-023190 [Crossref]
- Bolger JC, Loughney L, Tully R, Cunningham M, Keogh S, McCaffrey N, et al.
Perioperative prehabilitation and rehabilitation in esophagogastric
malignancies: a systematic review. Dis Esophagus. 2019;32(9):1–11. doi: 10.1093/dote/doz025 [Crossref]
- Cunha FMR, Borges MC,
Carvalho FA, Volpe MS, Júnior VR, Crema E. Eficácia do treinamento muscular
inspiratório pré-operatório utilizando o Threshold
IMT em pacientes submetidos à cirurgia esofágica: um ensaio clínico
randomizado. Rev Pesqui em Fisioter. 2019;9(3):361–8. doi: 10.17267/2238-2704rpf.v9i3.2512 [Crossref]
- Minnella EM, Awasthi R, Loiselle SE, Agnihotram RV, Ferri LE, Carli F.
Effect of exercise and nutrition prehabilitation on functional capacity in
esophagogastric cancer surgery: a randomized clinical trial. JAMA Surg.
2018;153(12):1081–9. doi: 10.1001/jamasurg.2018.1645 [Crossref]
- Dados-e-Numeros-Prevalencia-Tabagismo @ Www.Inca.Gov.Br
[Internet]. Available from:
https://www.inca.gov.br/observatorio-da-politica-nacional-de-controle-do-tabaco/dados-e-numeros-prevalencia-tabagismo
- Robertson EV, Jankowski JA. Genetics of gastroesophageal cancer: paradigms, paradoxes, and prognostic utility. Am J Gastroenterol. 2008;103(2):443–9. doi: 10.1111/j.1572-0241.2007.01691.x [Crossref]