Rev Bras Fisiol Exerc. 2023;22:e225481
doi: 10.33233/rbfex.v22i1.5481
REVIEW
Early mobilization in adult patients using
extracorporeal membrane oxygenation
Mobilização
precoce em pacientes adultos sob o uso de oxigenação por membrana extracorpórea
Bruna
Pereira Gomes1, Camila Aparecida Correa1, Érica Nasatto Morais1, Juliana Fernanda de Lima e
Silva1, Marcos Vinícius Costa e Silva1, Vanessa de Aquino
Aleixo Marques1, Jaqueline Aparecida Almeida Spadari1, Giulliano Gardenghi1,2,3,4,5
1Hospital e Maternidade São Cristóvão,
São Paulo, SP, Brazil
2Hospital de Urgências de Goiás,
Goiânia, GO, Brazil
3Faculdade CEAFI, Goiânia, GO, Brazil
4Hospital ENCORE/Kora Saúde, Aparecida de Goiânia, GO, Brazil
5Centro de Ensino e Trinamento da Clínica de Anestesia, Goiânia, GO, Brazil
Received: March 12, 2023; Accepted: June 12, 2023.
Correspondence: Giulliano Gardenghi,
coordenacao.cientifica@ceafi.edu.br
How to cite
Gomes BP, Correa CA, Morais
EN, Lima e Silva JF, Costa e Silva MV, Marques VAA, Spadari
JAA, Gardenghi G. Early mobilization in adult
patients using extracorporeal membrane oxygenation. Rev Bras
Fisiol Exerc. 2023;22:e225481.
doi: 10.33233/rbfex.v22i1.5481
Abstract
Introduction: Extracorporeal
membrane oxygenation is used in patients with respiratory failure and severe
cardiovascular complications with a prognosis of reversal. Early mobilization
in these patients can prevent the complications of immobility, such as
decreased functional capacity, delirium, physical, respiratory and
psychological deficits. A well-trained multidisciplinary team with extensive
knowledge about extracorporeal membrane oxygenation is essential to optimize
patient care. Objective: The objective of this narrative literature
review was to relate the repercussions of early mobilization in these patients,
to optimize care and reduce unfavorable events related to immobility. Methods:
This is an integrative literature review, with research through analysis of
articles on the Pubmed platform, from the years 2014
to 2022, applying the terms: ECMO Rehabilitation, Mobilization ECMO, ECMO and
physiotherapy and ECMO Physiotherapy. Results: 26 articles were found, 9
selected for the study, in a total of 1390 patients on extracorporeal membrane
oxygenation who received at least one physiotherapy session, from activities in
bed to walking. There was no change in relevant hemodynamic parameters,
regardless of the location of the cannula, making early mobilization feasible. Conclusion:
Early mobilization in patients undergoing extracorporeal membrane oxygenation is
beneficial for a better clinical outcome within institutions, which requires
the involvement of the entire aligned and engaged multidisciplinary team.
Keywords: early ambulation; physical
therapy; extracorporeal membrane oxygenation.
Resumo
Introdução: A oxigenação por membrana
extracorpórea é utilizada em pacientes com falência respiratória e complicações
cardiovasculares graves com prognóstico de reversão. A mobilização precoce
nesses pacientes pode evitar as complicações do imobilismo, como diminuição da
capacidade funcional, delirium, déficits físicos, respiratórios e psicológicos.
É fundamental uma equipe multidisciplinar bem treinada e com conhecimentos
amplos sobre a oxigenação por membrana extracorpórea para otimizar a
assistência ao paciente. Objetivo: O objetivo desta revisão narrativa de
literatura é relacionar as repercussões da mobilização precoce nestes
pacientes, a fim de otimizar a assistência e diminuir os eventos desfavoráveis
relacionados ao imobilismo. Métodos: É uma revisão integrativa de
literatura, com pesquisas por meio de análises de artigos na plataforma Pubmed, dos anos 2014 a 2022, aplicando os termos: ECMO Rehabilitation, Mobilization
ECMO, ECMO and physiotherapy
e ECMO Physiotherapy. Resultados: Foram
encontrados 26 artigos, 09 selecionados para o estudo, totalizando 1390
pacientes em oxigenação por membrana extracorpórea que receberam ao menos uma
sessão de fisioterapia, desde atividades no leito à deambulação. Não houve
alteração de parâmetros hemodinâmicos relevantes, independentemente da
localização da cânula, tornando viável a mobilização precoce. Conclusão:
A mobilização precoce em pacientes submetidos a oxigenação por membrana
extracorpórea se mostra benéfica para melhor desfecho clínico dentro das
instituições, o que exige o envolvimento de toda equipe multidisciplinar
alinhada e engajada.
Palavras-chave: oxigenação por membrana extracorpórea;
deambulação precoce; Fisioterapia.
Introduction
In recent years,
early mobilization has been explored as a way to accelerate the recovery of
critically ill patients and reduce risk factors that develop muscle weakness
acquired in the intensive care unit (ICU) [1].
There is a
strong association between weakness and prolonged ventilator dependence, which
is a fundamental result in patient survival after acute respiratory failure,
lasting for months or indefinitely [2].
Functional decline is directly
related to the harmful effects of immobility in the ICU, leading to increased
care costs, decreased quality of life and post-discharge survival [3]. The
patient admitted to the ICU using mechanical ventilation has about a 25% chance
of developing muscle atrophy upon awakening and may even progress to
post-intensive care syndrome (PICS) [4,5].
With technological advances,
extracorporeal life support modalities are adopted in patients with
cardiovascular and pulmonary failures, such as extracorporeal membrane
oxygenation (ECMO). ECMO consists of a closed extracorporeal circuit system,
which works based on adequate oxygenation and temperature modulation. Before
reperfusion occurs, it is necessary for the blood to be heated by the machine
to body temperature and, soon after, this blood will be pumped and return to
the arterial and venous circulatory system [6]. It is important to mention that
among the types of ECMO there are Veno-Arterial (VA)
cannulation, guaranteeing cardiac support with preserved lung function or not.
The drainage cannula is inserted into a venous access and the return cannula
into an arterial one, being classified in two ways: central or peripheral. In
the central one, the drainage cannula is connected directly to the right atrium
and the return cannula to the ascending portion of the aorta artery. In the
peripheral, the blood can be drained through the femoral or jugular veins and
returns to the patient through the carotid, axillary or femoral artery. Venovenous (VV) cannulation is appropriate to support
oxygenation in respiratory failure with preserved cardiac function. In this
case, the drainage cannula is usually inserted into the right femoral vein and
the return cannula into the right internal jugular vein. Another alternative is
the drainage cannula inserted in the jugular vein and the return cannula in the
femoral vein [7].
In case of ECMO failure by VV
cannulation, the patient can undergo a new hybrid or VA configuration.
Different hybrid cannulations can be used depending on the clinical picture.
This category is called veno-arterial veno-venous ECMO (VAVV) [8].
Patients on ECMO are often under
bed rest, immobile, and in most cases under sedation. When treatment lasts for
a long time, the complications generated by immobility can prolong
hospitalization and increase the need for additional health care [9].
Currently, it is increasingly
common for patients to wake up on ECMO for food, communication, active
participation in treatment and rehabilitation programs, promoting the
maintenance of muscle strength and function [8]. In the possibility of physical
activity during ECMO, the improvement in gas exchange after physical exercise
and walking was confirmed. Thus, physical therapy, simultaneously with the
multidisciplinary team, aims to promote functional recovery through human
movement [3,9]. Given the above, it is known that it is essential to reduce the
negative impacts generated by immobility, hospital and psychosocial costs in
patients using ECMO. The present study aims to list the repercussions of
mobilization in patients on ECMO to optimize care and reduce unfavorable
outcomes related to immobility in bed.
Methods
This study consists of a narrative
review of the literature, carried out through the analysis of articles searched
on the Pubmed platform, from the years 2014 to 2022,
applying the terms: ECMO Rehabilitation, Mobilization ECMO, ECMO and
physiotherapy and ECMO Physiotherapy.
This work included randomized
clinical trials, retrospective investigations, case studies, systematic
literature review and cross-sectional observational studies that could
demonstrate the effectiveness of early mobilization in patients using ECMO. The
use of articles that enabled mobilization in adult patients using ECMO was
established as an inclusion criterion.
Results
The results were displayed in Chart
I, where the authors of the various studies, objectives, types of accesses and
conclusions that discuss the theme analyzed are described. The search resulted
in 26 articles, after critical reading 25 were selected, among them 6 excluded,
19 evaluated for eligibility and 9 included for the present study. One thousand
three hundred and ninety (1390) patients on extracorporeal membrane oxygenation
received at least one physiotherapy session, from activities in bed to walking.
There was no change in relevant hemodynamic parameters, regardless of the
location of the cannula, making early mobilization feasible. The article
selection flowchart is shown in figure 1.
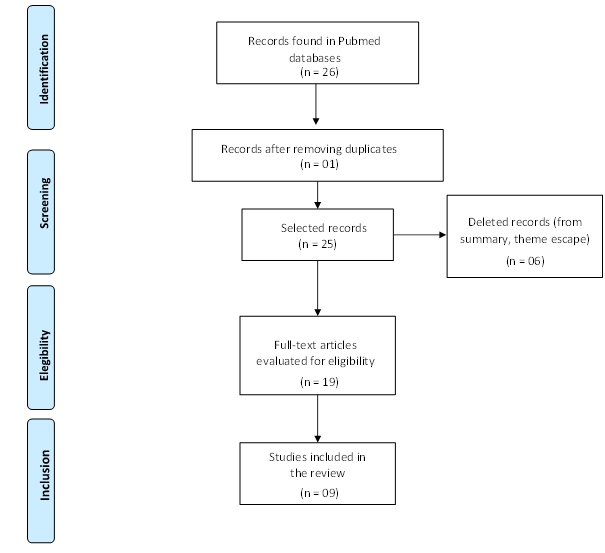
Figure 1 - Flowchart for selection and
inclusion of articles in this study
Chart I - Results of the search for
articles that addressed exercises/mobilization in patients with ECMO
Discussion
Patients with
prolonged stay in ICUs may develop physical and psychological complications and
generalized muscle weakness, caused by the association of muscle and/or nerve
injury, according to Needham [19]. Early rehabilitation has been identified as
a viable intervention in the ICU environment, with a positive response in the
physical function and muscle strength of critically ill patients. However, it
is a strategy that seems to be far from reality in many institutions, says
Adler et al. [20].
According to Cucchi et al. [17], there is a growing practice of
physical therapy in awake patients on ECMO. Despite the limitations, walking is
performed in almost half of the cases examined. The awake ECMO approach aims to
reduce cases of delirium after sedation and analgesia, muscle weakness,
deficits in muscle and respiratory conditioning. This consists of weaning from
sedation and invasive mechanical ventilation, so that the patient actively
participates in decision-making and rehabilitation.
In general, the
main challenges observed by professionals at the time of care are: patient
agitation, respiratory discomfort, positioning and malfunction of the cannula
during mobilization, trauma and local bleeding [17].
Early
mobilization in patients using ECMO may present some adverse events, such as
risks related to walking, which include device and catheter displacement,
circuit interruption, activity intolerance, and others. In addition, there may
be abrupt desaturation, a drop in heart rate and blood
pressure, which will culminate in the use of vasoactive drugs, increased
sedation and even neuromuscular blockers, according to Rickelmann
et al. [21]. In contrast, another randomized controlled study by Hodgson
et al. [22] carried out in three intensive care units of the main ECMO
centers in Australia, observed that patients started early mobilization within
72 hours, maintaining ECMO for 7 days, improved functional independence in
activities of daily living and were discharged from hospital. The authors also
highlighted that this type of mobilization was performed by a trained
multidisciplinary team, with more than 15 years of experience in specialized
centers. Thus, it was possible to state that early mobilization is safe and
feasible.
According to
Lange et al. [23], there is a percentage (10-36%) of patients using ECMO
that evolve with bleeding complications, bleeding at the cannulation site
(VV-ECMO), bleeding at the surgery site (VA-ECMO), and even intracranial
hemorrhage in 6% of these patients. On the other hand, Wells et al. [15]
in a study carried out, also in a specialized ECMO center, they demonstrated
safety in the mobilization of such patients [15]. Once again, it was mentioned
that an important item for such progress was having a very well-prepared
multidisciplinary team to assess, for example, the mental, hemodynamic,
respiratory state and the possible accidents that this patient may suffer, as
well as bringing the study by Cucchi et al.
[15,17].
Considering
Brazil, due to organic instability and vascular cannulation, patients tend to
remain permanently sedated and immobile during ECMO treatment. It should be
noted that it has been widely demonstrated in the literature that deep sedation
and immobilization are related to adverse effects and worse results [18].
ECMO support is
attributed to an inflammatory state due to the patient's clinical condition,
which increases oxygen demand and blood flow. Given this, according to Munshi et
al. [14], there are more suitable cannulas for mobilization, the bicaval double lumen, has its maximum flow capacity reached
and greater oxygen supply [14]. According to Ko et al. [13], with the
technology of cannulas and extracorporeal circuits, ECMO therapy has become
safer to support patients for long periods. From therapy with the physiotherapy
team, it is possible to perform sitting, strengthening, orthostatism,
stationary gait and ambulation, without the occurrence of any serious adverse
event.
Patients using
low-dose vasopressors were fully capable of performing active physical therapy,
without the need for changes in ECMO configuration. However, not all patients
using ECMO are suitable for such mobilization, as is the case of patients who
come to present hemodynamic instability, high-dose vasopressors, deep sedation,
neuromuscular blockade or severe hypoxemic, as described by Abrams et al.
[11].
ICU-acquired
muscle weakness is associated with physical and cognitive deficits, which can
last for years after ICU admission. Thus, there has been a need to keep these
patients awake, with active participation and walking during ECMO. However, as
described by Hayes et al. [10] this practice is not carried out
considering that most patients on ECMO remain in bed and receive passive
exercises. Thus, rehabilitation is established late.
The need to
conduct more studies is highlighted for better practical guidance, such as
defining protocols, minimizing possible barriers, and identifying the quality
of life after the intensive care unit.
Conclusion
Scientific evidence indicates in
clinical practice that early ECMO mobilization is feasible within institutions,
which requires the involvement of the entire aligned and engaged
multidisciplinary team. Physical therapy associated with reduced sedation
minimizes the occurrence of muscle weakness, delirium, physical, respiratory
and psychological deficits, in addition to optimizing patient mobility. It is
extremely important that this mobilization be performed to generate a better
clinical outcome.
Academic affiliation
Article developed for completion of
the Postgraduate Program in Hospital Physiotherapy at Hospital e Maternidade
São Cristóvão.
Conflicts of interest
The authors declare that they have
no conflicts of interest related to this publication.
Financing source
This work did not have funding.
Authors’ contribution
Research conception and
design: Gomes BP, Correa CA, Morais EN, Silva JFL, Silva
MVC, Marques VAA, Gardenghi G, Spadari JAA; Obtaining data: Gomes BP,
Correa CA, Morais EN, Silva JFL, Silva MVC, Marques VAA; Data analysis and
interpretation: Gomes BP, Correa CA, Morais EN, Silva JFL, Silva MVC,
Marques VAA; Writing of the manuscript: Gomes BP, Correa CA, Morais EN,
Silva JFL, Silva MVC, Marques VAA. Critical review of the manuscript for
important intellectual content: Gardenghi G.
References
- Dias AS,
Ramos FF, Silva PE. Fraqueza muscular do doente crítico. In: editor: George Jerre Vieira Sarmento, editor associado: André Luiz Lisboa
Cordeiro. Fisioterapia motora aplicada ao paciente crítico: do diagnóstico à
intervenção. 2ª ed. Santana de Parnaíba,
SP: Manole; 2022. p.1-24
- Griffiths RD, Hall JB. Intensive care unit-acquired
weakness. Crit Care Med. 2010;38(3):779-87. doi: 10.1097/ccm.0b013e3181cc4b53 [Crossref]
- França
EÉT, Ferrari F, Fernandes P, Cavalcanti R, Duarte A, Martinez BP, et al.
Fisioterapia em pacientes críticos adultos: recomendações do Departamento de
Fisioterapia da Associação de Medicina Intensiva Brasileira. Rev
Bras Ter Intensiva. 2012;24(1):6-22. doi: 10.1590/S0103-507X2012000100003 [Crossref]
- De Jonghe B. Paresis acquired in the intensive care unit. a prospective multicenter study. JAMA. 2002;288(22):2859. doi: 10.1001/jama.288.22.2859 [Crossref]
- Levine S, Nguyen T, Taylor N, Friscia ME, Budak MT, Rothenberg P, et al. Rapid disuse atrophy of diaphragm fibers in mechanically ventilated humans. N Eng J Med. 2008;358(13):1327-35. doi: 10.1056/NEJMoa070447 [Crossref]
- Aquim EE, Bernardo WM, Buzzini RF, Azeredo NSG, Cunha LS, Damasceno MCP, et al. Brazilian guidelines for early mobilization in intensive care unit. Rev Bras Ter Intensiva. 2019;31(4). doi: 10.5935/0103-507X.20190084 [Crossref]
- Squiers JJ,
Lima B, DiMaio JM. Contemporary extracorporeal
membrane oxygenation therapy in adults: Fundamental principles and systematic
review of the evidence. The Journal of Thoracic and Cardiovascular Surgery.
[Internet]. 2016 Jul [cited 2021 Jun 2];152(1):20-32. Available from:
https://www.jtcvs.org/action/showPdf?pii=S0022-5223%2816%2900424-4
- Romano TG, Mendes PV, Park M, Costa ELV. Extracorporeal respiratory support in adult patients. J Bras Pneumol. 2017;43(1):60-70. doi: 10.1590/S1806-37562016000000299 [Crossref]
- Garcia
JP, Iacono A, Kon ZN,
Griffith BP. Ambulatory extracorporeal membrane oxygenation: A new
approach for bridge-to-lung transplantation. The Journal of Thoracic and
Cardiovascular Surgery. 2010;139(6):e137-9. doi: 10.1016/j.jtcvs.2009.12 [Crossref]
- Hayes K, Holland AE, Pellegrino VA, Young M, Paul E, Hodgson CL. Early rehabilitation during extracorporeal membrane oxygenation has minimal impact on physiological parameters: A pilot randomized controlled trial. Australian Critical Care. 2021;34(3):217-25. doi: 10.1016/j.aucc.2020.07.008 [Crossref]
- Abrams D, Javidfar J, Farrand E, Mongero LB, Agerstrand CL, Ryan P, et al. Early mobilization of patients receiving extracorporeal membrane oxygenation: a retrospective cohort study. Critical Care. 2014;18(1):R38. doi: 10.1186/cc13746 [Crossref]
- Abrams D, Madahar P, Eckhardt CM, Short B, Yip NH, Parekh M, et al. Early mobilization during ECMO for cardiopulmonary failure in adults: factors associated with intensity of treatment. Ann Am Thorac Soc. 2021;19(1):90-98. doi: 10.1513/AnnalsATS.202102-151OC [Crossref]
- Ko Y, Cho YH, Park YH, Lee H, Suh GY, Yang JH, et al. Feasibility and safety of early physical therapy and active mobilization for patients on extracorporeal membrane oxygenation. ASAIO Journal. 2015;61(5):564-8. doi: 10.1097/MAT.0000000000000239 [Crossref]
- Munshi L, Kobayashi T, DeBacker J, Doobay R, Telesnicki T, Lo V, et al. Intensive care physiotherapy during extracorporeal membrane oxygenation for acute respiratory distress syndrome. Ann Am Thorac Soc. 2017;14(2):246-53. doi: 10.1513/AnnalsATS.201606-484OC [Crossref]
- Wells CL, Forrester J, Vogel J, Rector R, Tabatabai A, Herr D. Safety and feasibility of early physical therapy for patients on extracorporeal membrane oxygenator. Crit Care Med. 2018;46(1):53-9. doi: 10.1097/CCM.0000000000002770 [Crossref]
- Mayer KP, Pastva AM, Du G, Hatchett SP, Chang M, Henning AN, et al. Mobility levels with physical rehabilitation delivered during and after extracorporeal membrane oxygenation: a marker of illness severity or an indication of recovery? Phys Ther. 2021;102(3). doi: 10.1093/ptj/pzab301 [Crossref]
- Cucchi M, Mariani S, Piero ME, Ravaux JM, Kawczynski MJ, Di Mauro M, et al. Awake extracorporeal life support and physiotherapy in adult patients: A systematic review of the literature. Perfusion. 2022;026765912210960. doi: 10.1177/02676591221096078 [Crossref]
- Marhong JD, DeBacker J, Viau-Lapointe J, Munshi L, Del Sorbo L, Burry L, et al. Sedation and mobilization during venovenous extracorporeal membrane oxygenation for acute respiratory failure. Crit Care Med. 2017;45(11):1893-9. doi: 10.1097/CCM.0000000000002702 [Crossref]
- Needham DM, Davidson J, Cohen H, Hopkins RO, Weinert C, Wunsch H, et al. Improving long-term outcomes after discharge from intensive care unit. Crit Care Med. 2012;40(2):502-9. doi: 10.1097/CCM.0b013e318232da75 [Crossref]
- Adler J, Malone D. Early mobilization in the intensive
care unit: a systematic review. Cardiopulm Phys Ther J. 2012;23(1):5-13. doi: 10.1097/01823246-201223010-00002 [Crossref]
- Rickelmann C, Knoblauch DJ. Incorporating safe patient-handling techniques to mobilize our most complex patients on extra corporeal membrane oxygenation. Crit Care Nurs Q. 2018;41(3):272-81. doi: 10.1097/CNQ.0000000000000206 [Crossref]
- Hodson CL, Hayes K, Linnane M, Transtad O. Early mobilization during extracorporeal membrane oxygenation was safe and feasible: a pilot randomized controlled trial. Intensive Care Med. 2020;46(5):1057-9. doi: 10.1007/s00134-020-05994-8 [Crossref]
- Lange DW, Sikma MA, Meulenbelt J. Extracorporeal membrane oxygenation in the treatment of poisoned patients. Clin Toxicol. 2013;51(5):385-93. doi: 10.3109/15563650.2013.800876 [Crossref]