Rev Bras Fisiol Exerc. 2024;23:e235558
doi: 10.33233/rbfex.v23i2.5558
ORIGINAL ARTICLE
Inspiratory muscle training on sleep quality after coronary artery bypass
grafting
Treinamento dos
músculos inspiratórios na qualidade do sono após a cirurgia de revascularização
do miocárdio
André Luiz Lisboa Cordeiro¹,
Bruna Lima dos Reis¹, Emily Almeida Pereira¹, André Raimundo França Guimarães2
1Centro Universitário Nobre de Feira de
Santana (UNIFAN), Feira de Santana, Bahia, Brazil
2Instituto Nobre de Cardiologia, Feira de
Santana, Bahia, Brazil
Received: December 20,
2023; Accepted: March 20,
2024.
Correspondence: André Luiz Lisboa Cordeiro, andrelisboacordeiro@gmail.com
How to cite
Cordeiro ALL, Reis BL, Pereira
EA, Guimarães ARF. Inspiratory muscle training on sleep quality after
coronary artery bypass grafting. Rev Bras Fisiol
Exerc. 2024;23:e235558. doi:
10.33233/rbfex.v23i2.5558
Abstract
Objective: To evaluate the impact of Inspiratory Muscle Training
(IMT) on sleep quality and pulmonary function after Myocardial
Revascularization (MR). Methods: This is a randomized and controlled
clinical trial. The participants were randomized to the inspiratory muscle
training group (TG) or to the control group (CG). The CG performed the
application of non-invasive ventilation, breathing exercises, kinesiotherapy,
cycle ergometry and ambulation. The TG patients, in addition to the unit's
standard protocol, were submitted to MIP assessment and started inspiratory
muscle training with 40% of MIP. Pulmonary function (vital capacity and peak
expiratory flow), ventilatory muscle strength (maximum inspiratory pressure and
maximal expiratory pressure) and sleep quality (Pittsburgh Sleep Quality Index
(PSQI) and Epworth Sleepiness Scale (EPS)) were evaluated before surgery and at
hospital discharge. Results: 102 patients participated in this study, 54
people in the CG and 48 in the GT. The IMT had a more relevant impact on
sleepiness at hospital discharge (95%CI 7 (6.39 to 7.61) in ESP and PSQI with
95%CI of 8 (7.61 to 8.39). Performed the inspiratory muscle training had a
statistically significant response in the variables MIP (95%CI of 18 (17.14 to
18.86)), MEP 95%CI of 6 (5.37 to 6.63), CV with 95%CI of 2(1.61 to 2.39). On
the other hand, PEF showed no difference between the groups with 95%CI of -5 (-11.78
to 1.78). Conclusion: IMT was effective in reducing the loss of
ventilatory muscle strength and sleep quality after CABG.
Keywords: breathing exercises; sleep; cardiac surgery.
Resumo
Objetivo: Avaliar o impacto do treinamento
muscular inspiratório (TMI) na qualidade do sono e na função pulmonar após a
revascularização do miocárdio (RM). Métodos: Este é um ensaio clínico
randomizado e controlado. Os participantes foram randomizados para o grupo de
treinamento muscular inspiratório (TG) ou para o grupo controle (GC). O GC
realizou a aplicação de ventilação não invasiva, exercícios respiratórios,
cinesioterapia, cicloergometria e deambulação. Os
pacientes do TG, além do protocolo padrão da unidade, foram submetidos à
avaliação da PImáx e iniciaram o
treinamento muscular inspiratório com 40% da PImáx.
A função pulmonar (capacidade vital e pico de fluxo expiratório), a força
muscular ventilatória (pressão inspiratória máxima e pressão expiratória
máxima) e a qualidade do sono (Índice de Qualidade do Sono de Pittsburgh (PSQI)
e Escala de Sonolência de Epworth (EPS) foram
avaliadas antes da cirurgia e na alta hospitalar. Resultados: 102
pacientes participaram deste estudo, 54 pessoas no GC e 48 no GT. O TMI teve um
impacto mais relevante na sonolência na alta hospitalar (IC95% 7 (6,39 a 7,61)
na EPS e PSQI com IC95% de 8 (7,61 a 8,39). A realização do treinamento
muscular inspiratório teve uma resposta estatisticamente significativa nas
variáveis PImáx (IC95% de 18(17,14 a
18,86)), PEmáx com IC95% de 6 (5,37 a
6,63), CV com IC95% de 2 (1,61 a 2,39). Por outro lado, o PFE não mostrou
diferença entre os grupos com IC95% de -5 (-11,78 a 1,78). Conclusão: O
treinamento muscular inspiratório foi eficaz na redução da perda de força
muscular ventilatória e da qualidade do sono após a cirurgia de
revascularização do miocárdio.
Palavras-chave: exercícios respiratórios; sono;
cirurgia cardíaca.
Introduction
Cardiac surgery is considered a complex procedure in the
treatment of cardiovascular diseases, but it is associated with complications
that may arise from a decline in pulmonary function and inspiratory muscle
strength [1]. In this scenario, inspiratory muscle training (IMT) can be useful
to optimize muscle and lung function, decreasing postoperative complications.
Patients with sleep disorders may be less responsive to training, thus
increasing postoperative risk [2].
In 2018, in Brazil, approximately 23,000 heart surgeries
(CC) were performed, including plasties and valve replacements and myocardial
revascularization, among which more than a thousand deaths were recorded [3].
Physiotherapy is important to prevent pulmonary
complications, and one of the techniques used that has positive results is IMT,
showing benefits such as significantly improving inspiratory muscle strength,
resistance, forced vital capacity, forced expiratory volume in a second,
postoperative hospital stay and reduced risk of postoperative pulmonary
complications [4].
During the length of stay in the ICU, studies point to an
incidence of up to 47% in hospitalized patients who have a lower pain
tolerance, greater irritability and longer hospital stay. It is highlighted
that ensuring adequate sleep is one of the factors that favor recovery from
aggravation that led to hospitalization, since they show that the presence of
insomnia causes the second most frequent subjective complaint of patients after
pain, which can worsen the underlying disease and affect daytime functioning,
being less receptive to prescribed exercises such as IMT [5,6].
Despite the few articles on the subject, this study aims
to evaluate the impact of inspiratory muscle training on sleep quality and
pulmonary function in patients undergoing coronary artery bypass grafting.
Methods
Design of study
This is a randomized and controlled clinical trial,
carried out with patients submitted to coronary artery bypass grafting at the
Instituto Nobre de Cardiologia in Feira de Santana, Bahia, from January 2018 to
February 2020. This study is registered in the Brazilian Registry of Clinical
Trials (ReBEC) with the number RBR-8dqrdq.
Inclusion and exclusion criteria
The following inclusion criteria were used: Individual of
both sexes with Coronary Artery Disease (CAD), aged over 18 years and
undergoing coronary artery bypass grafting with cardiopulmonary bypass and
median sternotomy. The exclusion criteria were the use of an intra-aortic
balloon, surgical reintervention, death, valvular heart disease, previous lung
disease, inability to understand how to perform the proposed techniques,
hemodynamic instability during the evaluation or during inspiratory muscle training,
physical limitation, such as amputation, that compromised the performance of
the exercises and inability to answer the applied questionnaires.
Sample calculation
In order to calculate the sample size, we carried out a
pilot study with 10 patients. We used a standard deviation of 63 meters, in the
six-minute walk test, based on the pilot of the final individualized IMT group
and 112 meters in relation to the standard deviation of the conventional IMT
group from the work of Cordeiro et al. [7] We used a difference of 50,
which is related to the clinically relevant distance [7]. For an alpha of 5%
and aiming to reach a power of 80%, 42 patients were needed, 21 in each group.
Ethical aspects
Our study was submitted to and approved by the Ethics and
Research Committee of Faculdade Nobre de Feira de Santana, with opinion number
2,366,995. All participants signed an informed consent form.
Study protocol
Research participants were randomized to the inspiratory
muscle training group (TG) or to the control group (CG) by a simple draw. There
were two balls, each with a piece of paper indicating the groups, and a member
of the team on duty was asked to choose one of the balls, the result being the
patient's allocation group. No researcher had any influence on the procedures
adopted by the team, and the patient was managed based on the institution's
protocol, which consists of the application of non-invasive ventilation,
breathing exercises, kinesiotherapy, cycle ergometry and ambulation. The TG
patients, in addition to the unit's standard protocol, underwent MIP assessment
and started inspiratory muscle training with a linear pressure loading device
(PowerBreathe Knectic Series®, HaB International, UK), with 40% of MIP,
performing 3 sets with 15 repetitions. This training was performed twice a day,
from the first postoperative day until the day of hospital discharge. Pulmonary
function, ventilatory muscle strength and sleep quality were assessed before
surgery and at hospital discharge.
Clinical and surgical characteristics such as diabetes
mellitus, systemic arterial hypertension, dyslipidemia, acute myocardial
infarction and sedentary lifestyle were collected. All these comorbidities were
known through the medical records of each patient, with the exception of
sedentary lifestyle, which was assessed using the International Physical
Activity Questionnaire (IPAQ) in long format, and evaluates 27 questions
related to physical activities performed in a normal week, with light
intensity, moderate and vigorous with a continuous duration of 10 minutes,
divided into four categories of physical activity such as work, transportation,
domestic activities and leisure. Those who did not perform any physical
activity for at least 10 continuous minutes during the week were considered
sedentary [8].
Measurement of ventilatory muscle strength
The preoperative assessment of inspiratory muscle
strength (Maximum Inspiratory Pressure (MIP)) was performed with an Indumed®
analog manovacuometer. During the evaluation, a maximum expiration was
requested until the residual volume and then a maximum and slow inspiration
until the total pulmonary capacity. This test was done through the method with
the unidirectional valve, being possible a flow through an orifice of one
millimeter in order to exclude the action of the buccinator, and repeated 3
times, using the highest value reached since this value was not the last.
Expiratory muscle strength (Maximum Expiratory Pressure (MEP)) was evaluated
with the same device and the patient was instructed to perform a maximum
inspiration until he reached his Total Pulmonary Capacity, the mask was placed
and after this required a maximum expiration until the residual capacity was
reached. The test was repeated three times, using the result with the highest
value, which could not be the last [9].
Pulmonary function assessment
To assess vital capacity, a facemask connected to the
expiratory branch of the analog ventilometer (Ferraris – Mark 8 Wright
Respirometer, Louisville, CO, USA) was used and the patient was instructed on
all phases of the test. The ventilometer was unlocked, reset to zero and soon
after the facemask was placed on the individual's face. He performed a deep
inspiration until reaching his total pulmonary capacity, soon after a slow and
gradual expiration until reaching his residual volume. After that, the ventilometer
was stopped and the result observed and noted. The test was repeated three
times, considering the highest value result [10].
Peak expiratory flow was assessed using the Mini Wright®
brand peak flow. During the assessment, the patient was seated, with the head
in a neutral position and a nose clip to prevent air from escaping through the
nostrils. The patient took a deep inspiration, up to full lung capacity,
followed by forced expiration with the mouth on the device. After three
measurements, the highest value was chosen, with no difference greater than 40
liters between measurements [10].
Sleep quality assessment
For the assessment, the Pittsburgh Sleep Quality Index
(PSQI) and the Epworth Sleepiness Scale were used.
The Pittsburgh Sleep Quality Index Questionnaire (PSQI)
was developed, and validated in Brazil, in an adult population, by Bertolazi.
The PSQI analyzes seven sleep components: subjective quality, sleep latency,
sleep duration, sleep efficiency, and sleep disorders, medication use and daily
dysfunction roommate. The score can vary from 0 to 3 in each question, when
adding the questions, a maximum score of 21 points is reached. Scores from 0-4
indicate good sleep quality, 5-10 indicate poor sleep quality, and scores above
10 indicate a sleep disorder [11].
The Epworth Sleepiness Scale is used to assess the degree
of excessive daytime sleepiness. Eight questions are asked, which can be scored
from 0 to 3 and the maximum total score goes up to 24, with 0-6 indicating
normal sleep, 7-8 average sleepiness and 9-24 abnormal sleepiness [12].
Statistical analysis
For data analysis, the Statistical Package for Social
Sciences (SPSS) version 20.0 was used. Normality was verified using the
Shapiro-Wilks test. Continuous variables were expressed as mean and standard
deviation. Chi-square was used to compare categorical variables. The analysis
between groups was performed using the independent Student's t test and
intra-group using the paired Student's t test. A delta was generated by
subtracting the hospital discharge values from the preoperative period. A
p < 0.05 was considered significant.
Results
One hundred and two patients participated in this study,
54 in the control group and 48 in the inspiratory muscle training group (Figure
1), mean age 66 years, most of the patients were male 62 (60.5%), BMI between
24 and 25 kg/m², and the most common comorbidity was systemic arterial
hypertension with 47 patients (47.5%), other data are shown in table I.
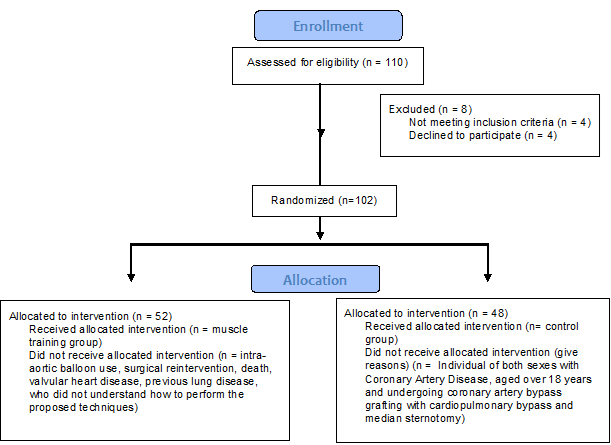
Figure 1 – Patient flow throughout the study
Table I - General data of the patients
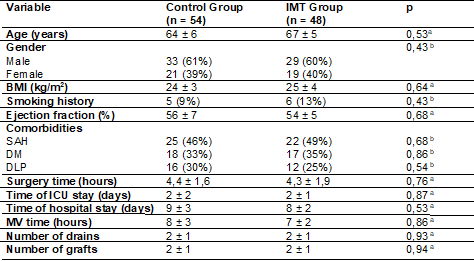
a = Independent Student's t-test; b = Chi-square; IMT =
Inspiratory Muscle Training; BMI = Body Mass Index; SAH = Systemic Arterial
Hypertension; DM = Diabetes Mellitus; DLP = Dyslipidemia; ICU = Intensive Care
Unit; MV = Mechanical Ventilation
Table II shows the comparison between preop rative and
hospital discharge on two questionnaires, the Pittsburgh Sleep Quality Index
and the Epworth Sleepiness Scale. It can be see that the group that received
IMT had a more relevant impact on sleepiness at hospital discharge (95%CI 7
(6.39 to 7.61) on the ESP and on the PSQI with a 95%CI of 8 (7.61 to 8.39).
Table II - Findings from the questionnaires in our study
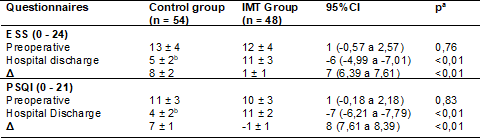
a = Independent Student's t-test; b = Paired Student's
T-test with p < 0.05 comparing preoperative with hospital discharge; CI =
Confidence Interval; ESS = Epworth Sleepiness Scale; PSQI = Pittsburgh sleep
quality index; IMT = Inspiratory Muscle Training
The group of patients who underwent inspiratory muscle
training had a statistically significant response in the variables MIP (95%CI
of 18 (17.14 to 18.86)), MEP (95%CI of 6 (5.37 to 6.63), VC with 95%CI of 2
(1.61 to 2.39). The PEF showed no difference between groups with 95%CI of -5
(-11.78 to 1.78). All values are shown in table III.
Table III - Pulmonary function and muscle strength test
findings in our study
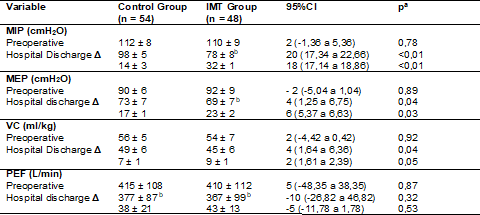
a = Independent Student's T test; b = Paired Student's T
test with p < 0.05 comparing preoperative with hospital discharge; CI =
Confidence Interval; IMT = Inspiratory Muscle Training; MIP = Maximal
Inspiratory Pressure; MEP = Maximal Expiratory Pressure; VC = Vital Capacity;
PEF = Peak Expiratory Flow
Discussion
Based on the data observed in the results, we can analyze
that the inspiratory muscle training performed in patients after cardiac
surgery had an impact on the improvement of daytime sleepiness and sleep
quality, evaluated through the Epworth Sleepiness Scale and Pittsburgh sleep
quality index, respectively. In addition, we found that there was less loss of
inspiratory and expiratory muscle strength and vital capacity in the group of
patients exposed to IMT.
We know that some factors can negatively affect the
quality of sleep in ICU patients. Factors such as brightness, noise, alarms,
and respiratory discomfort are the main reports in the literature [13]. Muscle
weakness can generate a biomechanical disadvantage, increasing ventilatory
demand, which leads to respiratory discomfort. Thinking about the application
of a protocol, IMT contributes to the decrease of this disadvantage. For this
reason, we noticed that the group of patients who underwent IMT had better
sleep quality and also increased muscle strength.
In 2003, a group from London defended that there was a
need to promote sleep improvement after cardiac surgery and that this outcome
would be achieved through rest [14]. Currently, our group argues that the
performance of exercise, particularly in this study, IMT, is able to modulate
sympathetic activity, generating a greater feeling of relaxation after the
protocol. This greater relaxation generates a decrease in heart rate and blood
pressure, promoting better sleep quality, as seen through the PSQI [15].
Yayla et al. [16] had already demonstrated that an
early mobilization protocol decreased the length of hospital stay and improved
sleep after surgery, a result similar to that verified by our study. Although
the results corroborate, the protocol used by Yayla et al. [16]
consisted of positioning in bed, use of incentive inspirometry, passive and
active kinesiotherapy, and transfer to an armchair. This approach is routinely
used in our study, with the differential being inspiratory muscle training,
i.e., IMT was able to optimize the results already verified in the literature.
The improvement in muscle strength can be attributed to
the attenuation of respiratory metaborreflex, increasing blood supply to the
periphery and decreasing the energy expenditure of the diaphragm [17]. In
addition, exercises performed in accordance with early mobilization practices
cause tissue oxygenation levels to increase [16].
Tafelmeier et al. [18] showed that the presence of
central apnea was associated with increased risk for pulmonary complications
after cardiac surgery. In our study, we did not evaluate or stratify the
presence or severity of sleep disorders; however, we can infer that the sample
included patients with this profile, given the high prevalence of this
condition in patients with heart disease.
It is important to understand that other factors can
affect sleep during the hospital stay. Among these factors, we can mention the
interaction of the staff with the patient to perform some procedure or
administer medication. This condition, verified by Casa et al. [19], is
common between midnight and 6 am. This makes the patient less willing and less
active the next day, resulting in a slower recovery of muscle strength and
functionality. Within this context, the application of IMT can minimize the
loss, as seen in this study, but other interventions need to coincide to
optimize postoperative functional capacity.
Although the presence of sleep disorders was not assessed
before surgery, Spielmanns et al. [20] found that the results obtained
during rehabilitation after cardiac surgery were not influenced by the presence
of sleep apnea. In the pediatric population the relationship between exercise
and sleep quality is already well established [21], but this is the first paper
to demonstrate a positive impact of IMT on daytime sleepiness and sleep quality
after cardiac surgery.
Ranjbaran et al. [22] showed that performing an
exercise protocol improved the quality of sleep in patients undergoing CABG,
but the study was conducted after hospital discharge. Thus, our study is the
first to demonstrate an improvement in sleep quality in patients undergoing
cardiac surgery while still in the nosocomial environment.
Our group had already demonstrated that postoperative IMT
reduces the loss of ventilatory muscle strength, which has a direct impact on
the functional capacity of these patients. In addition, a recent meta-analysis
showed that IMT improves inspiratory muscle strength, pulmonary function, and
functional capacity, and reduces the length of hospital stay in patients
undergoing cardiac surgery [23].
A limitation of the present study is that polysomnography
was not used to verify the presence of sleep disorders in patients hospitalized
for cardiac surgery. However, it should be emphasized that our aim was not to
verify an improvement in the disorder, but in the quality of sleep.
Conclusion
Based on the values found in our study, we conclude that
inspiratory muscle training in patients after coronary artery bypass grafting
was effective in improving the quality of sleep and lung function in these
individuals.
Conflict of interest
This study has no conflict of interest
Sources of financing
There was
no funding for the study
.
Authors' contributions
Conception and
design of the research: Cordeiro ALL; Data collection:
Cordeiro ALL, Reis BL, Pereira EA; Data analysis and interpretation: Cordeiro
ALL, Reis BL, Pereira EA; Statistical analysis: Cordeiro ALL; Manuscript
writing: Cordeiro ALL, Reis BL, Pereira EA; Critical review of the manuscript: Guimarães ARF
References
- Reisdorfer AP, Leal SMC, Mancia
JR. Nursing care for patient in post operatory heart surgery in the Intensive
Care Unit. Rev Bras Enferm. 2021;74(2):e20200163. doi: 10.1590/0034-7167-2020-0163 [Crossref]
- Wang S, Xin HN, Vico CCL, Liao JH, Li SL, Xie NM, Hu RF. Effect of an ICU diary on psychiatric disorders, quality of life, and sleep quality among adult cardiac surgical ICU survivors: a randomized controlled trial. Crit Care. 2020;24:81. doi: 10.1186/s13054-020-2797-7 [Crossref]
- Assis CR, Fortino CK, Saraiva CAS, Frohlich LF, Silva RE, Omizzollo S. Perfil clínico e sucesso na extubação de pacientes pós cirurgia cardíaca. Rev Pesqui Fisioter. 2020;10(1):25-32. doi: 10.17267/2238-2704rpf.v10i1.2619 [Crossref]
- Neto MG, Martinez BP, Reis HF, Carvalho VO. Pre- and postoperative inspiratory muscle training in patients undergoing cardiac surgery: systematic review and meta-analysis. Clin Rehabil. 2017;31(4):454–64. doi: 10.1177/0269215516648754 [Crossref]
- Dessotte M, Aparecida C, Rodrigues F, Furuya K, Rossi R, Aparecida L, et al. Estressores percebidos por pacientes no pós-operatório imediato de cirurgia cardíaca. Rev Bras Enferm. 2016;69(4):741-750. doi: 10.1590/0034-7167.2016690418i [Crossref]
- Sanz AH, Villamor
AO, Hernández JE, Berdura SG, Rovira RR, Rivero EG. Incidencia y factores
condicionantes del insomnio
en pacientes ingresados en hospital de alta tecnologia. Rev
Cuba Enferm. 2019 [cited
2023 Mar 12];35(2):e1718. Available from:
https://www.medigraphic.com/cgi-bin/new/resumen.cgi?IDARTICULO=100727
- Cordeiro AL, Melo TA, Neves D, Luna J, Esquivel MS, Guimarães AR, et al. Inspiratory muscle training and functional capacity in patients undergoing cardiac surgery. Braz J Cardiovasc Surg. 2016;31(2):140-4. doi: 10.5935/1678-9741.20160035 [Crossref]
- Guedes DP, Lopes CC, Guedes JERP. Reproducibility and validity of the international physical activity questionnaire in adolescents. Rev Bras Med Esporte. 2005;11(2):147e-154e. doi: 10.1590S1517-86922005000200011 [Crossref]
- Neder JA, Andreoni S, Lerario MC, Nery LE. Reference values for lung function tests. II. Maximal respiratory pressures and voluntary ventilation. Braz J Med Biol Res. 1999;32(6):719-27. doi: 10.1590/s0100-879x1999000600007 [Crossref]
- American Thoracic Society/European Respiratory Society. ATS/ERS Statement on respiratory muscle testing. Am J Respir Crit Care Med. 2002;166(4):518-624. doi: 10.1164/rccm.166.4.518 [Crossref]
- Bertolazi AN, Fagondes SC, Hoff LS, Dartora EG, Miozzo ICS, Barba MEF, et al. Validation of the Brazilian Portuguese version of the Pittsburgh sleep quality index. Sleep Med. 2011;12(1):70-5. doi: 10.1016/j.sleep.2010.04.020 [Crossref]
- Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540-5. doi: 10.1093/sleep/14.6.540 [Crossref]
- Balogh D, Kittinger E, Benzer A, Hackl JM. Noise in the ICU. Intensive Care Med. 1993;19(6):343-6. doi: 10.1007/BF01694709 [Crossref]
- Njawe P. Sleep and rest in patients undergoing cardiac surgery. Nurs Stand. 2003;.3-9;18(12):33-7. doi: 10.7748/ns2003.12.18.12.33.c3513 [Crossref]
- Russo M. Normal sleep, sleep physiology and sleep deprivation: general
principles. EMedicine. [cited 2023 Oct 30]. Available from:
http://www.emedicine.com/neuro/topic444.htm
- Yayla A, Özer N. Effects of early mobilization protocol performed after
cardiac surgery on patient care outcomes. Int J Nurs Pract. 2019;25(6):e12784. doi: 10.1111/ijn.12784 [Crossref]
- Crisafulli A, Salis E, Tocco F, Melis F, Milia R, Pittau G, et al. Impaired
central hemodynamic response and exaggerated vasoconstriction during muscle
metaboreflex activation in heart failure patients. Am J Physiol Heart Circ
Physiol. 2007;292(6):H2988-96. doi: 10.1152/ajpheart.00008.2007 [Crossref]
- Tafelmeier M, Luft L, Zistler E, Floerchinger B, Camboni D, Creutzenberg M,
et al. Central sleep apnea predicts pulmonary complications after cardiac
surgery. Chest. 2021;159(2):798-809. doi: 10.1016/j.chest.2020.07.080 [Crossref]
- Casida JM, Davis JE, Zalewski A, Yang JJ. Night-time care routine interaction and sleep disruption in adult cardiac surgery. J Clin Nurs. 2018;27(7-8):e1377-e1384. doi: 10.1111/jocn.14262 [Crossref]
- Spielmanns M, Pantev S, Turk A, Barthelmes J, Schindler M, Hermann M. Does
an undetected obstructive sleep apnea influence the natural course and success
of cardiac rehabilitation after cardiac surgery? Eur J Phys Rehabil Med.
2021;57(1):148-157. doi: 10.23736/S1973-9087.20.06340-6 [Crossref]
- Hedlund ER, Villard L, Lundell B, Sjöberg G. Physical exercise may improve sleep quality in children and adolescents with Fontan circulation. Cardiol Young. 2019;29(7):922-29. doi: 10.1017/S1047951119001136 [Crossref]
- Ranjbaran S, Dehdari T, Sadeghniiat-Haghighi K, Majdabadi MM. Poor sleep
quality in patients after coronary artery bypass graft surgery: an intervention
study using the precede-proceed model. J Tehran Heart Cent. 2015;10(1):1-8.
Available from: https://pubmed.ncbi.nlm.nih.gov/26157457
- Dsouza FV, Amaravadi SK, Samuel SR, Raghavan H, Ravishankar N. Effectiveness of inspiratory muscle training on respiratory muscle strength in patients undergoing cardiac surgeries: a systematic review with meta-analysis. Ann Rehabil Med. 2021;45(4):264-73. doi: 10.5535/arm.21027 [Crossref]