Rev Bras Fisiol Exerc. 2024;23:e235562
doi: 10.33233/rbfex.v23i1.5562
ORIGINAL ARTICLE
Assessment of prevalence and
risk factors for early mobilization in an emergency hospital
Avaliação da
prevalência e fatores de risco para mobilização precoce em um hospital de
urgências
Maristela Lúcia Soares
Campos1, Érika Letícia Gomes Nunes1, Letícia de Souza
Pereira2, Bruna Kelly Ferreira1, Isadora Oliveira Freitas
Barbosa1, Jefferson Petto3,4,5, Giulliano
Gardenghi1,6,7,8
1Hospital de Urgências de Goiás, Goiânia,
GO, Brazil
2Secretaria Estadual de Saúde, Goiânia,
GO, Brazil
3Escola Bahiana de Medicina e Saúde
Pública, Salvador, BA, Brazil
4Actus Cordios
Serviço de Reabilitação Cardiovascular e Metabólica, Salvador, BA, Brazil
5Centro Universitário UniFTC,
Salvador, BA, Brazil
6Hospital ENCORE, Aparecida de Goiânia,
GO, Brazil
7Clínica de Anestesia (CLIANEST),
Goiânia, GO, Brazil
8Faculdade CEAFI, Goiânia, GO, Brazil
Received: December 5,
2023; Accepted: January 26,
2024.
Correspondence: Giulliano Gardenghi, coordenacao.cientifica@ceafi.edu.br
How to
cite
Campos MLS, Nunes
ELG, Pereira LS, Ferreira BK, Barbosa IOF, Petto J, Gardenghi
G. Assessment of prevalence
and risk factors for early mobilization in an emergency hospital. Rev Bras Fisiol Exerc.
2024;23:e235562 doi: 10.33233/rbfex.v23i1.5562
Abstract
Introduction: An intensive care unit receives critically
ill patients, which includes specific and comprehensive care. These users
commonly remain confined to bed
for a prolonged period of time, causing inactivity, immobility and severe osteomyoarticular
dysfunction. Aim: To analyze the
prevalence, degree of mobility and
risk factors for early mobilization in patients that occurred
on the seventh
to the tenth
day of hospitalization
in the evaluated units. Methods: This is a cross-sectional
analytical descriptive study. To carry
out the research, a safety assessment, and the Johns Hopkins mobility scale were carried
out, ending with the analysis of
the mobility conduct carried out on the day
of the assessment, both via medical records. Results: 100 patients were included (age: 58±18 years, sex: 65 male). Regarding the performance of early mobilization, only 27% could be described as such. Participants who were on
external ventilation had a higher percentage
of mobilization (63%), when compared to
patients who were on invasive
mechanical ventilation
(33.3%). 73% of patients were classified as 1 (lying down) on
the Johns Hopkins scale.
The greater the number of risks,
including sedation and orotracheal tube, the lower the
mobilization rate. Conclusion:
A significant percentage of patients were
not mobilized. The greater the number
of risks, the lower the
mobilization rate. There was no difference in mobility rates, considering the different diagnoses. Therefore, a greater commitment to health
education for rehabilitation
professionals is necessary.
Keywords: early ambulation; hospitalization; limitation of mobility.
Resumo
Introdução: A unidade de terapia intensiva recebe
pacientes criticamente doentes, que necessitam de cuidados especializados e
integrais. Comumente estes usuários permanecem restritos ao leito por tempo
prolongado, ocasionando inatividade, imobilidade e disfunções osteomioarticulares severas. Objetivo: Analisar a
prevalência, o grau de mobilidade e os fatores de risco para mobilização
precoce em pacientes que estivessem do sétimo ao décimo dia de internação das
unidades avaliadas. Métodos: Trata-se de um estudo descritivo analítico
de característica transversal. Para a execução da pesquisa, foi realizada a
avaliação de segurança, e escala de mobilidade de Johns Hopkins, finalizando
com a análise de condutas de mobilidade realizadas no dia da avaliação, ambos
via prontuário. Resultados: 100 pacientes foram incluídos (idade: 58±18
anos, sexo: 65 masc). Com relação à realização de mobilização precoce, apenas
27% pôde ser caracterizada como tal. Os participantes que estavam em ventilação
espontânea apresentaram percentual maior de mobilização (63%), quando
comparados aos pacientes que estavam em ventilação mecânica invasiva (33,3%).
73% dos pacientes apresentavam classificação 1 (deitado) na escala de Johns
Hopkins. Quanto maior o número de riscos, entre eles, sedação e tubo
orotraqueal, menor o índice de mobilização. Conclusão: Uma porcentagem significativa dos pacientes não eram
mobilizados. Quanto maior o número de riscos, menor o índice de mobilização.
Não houve diferença nas taxas de mobilidade, considerando os diferentes
diagnósticos. Logo, faz-se necessário um maior empenho em educação em saúde
para os profissionais de reabilitação.
Palavras-chave: deambulação precoce; hospitalização;
limitação da mobilidade.
Introduction
The intensive care unit (ICU) receives critically ill patients who require specialized and comprehensive care. These users commonly
remain confined to bed for a prolonged
period, causing inactivity, immobility and severe musculoskeletal
disorders; This long stay also
promotes physical deconditioning, muscle weakness, increased days of mechanical
ventilation (MV) and prolonged weaning [1].
Early mobilization is directly related to greater life
expectancy and hospital discharge, as well as increased functional capacity and reduced
damage secondary to hospitalization [2]. When performed correctly and cohesively, mobility can prevent
muscle weakness, pressure injuries, atelectasis,
pneumonia, thromboembolic diseases,
delirium and others [3].
For good practice in a critical environment, criteria that permeate
patient eligibility and safety are necessary. The expert consensus of
Hodgson et al. [4] brings concepts
and safety parameters that increase protection, reducing the risk
of adverse events, including cardiovascular, neurological,
and surgical conditions. A good tool to achieve adequate
results is the Johns Hopkins activity and mobility promotion
(JH-AMP) scale, which implements a common, interprofessional
mobility language, in addition to systematizing
and establishing daily goals as a therapeutic plan [5].
The use of scales to
measure, adapt and classify early
mobilization is increasingly important and present in the hospital environment. The physiotherapist is qualified and responsible
for evaluating and identifying which patients have hemodynamic
and functional conditions for the safe execution of activities,
classifying them according to their
individualities [6].
In view of the
issues presented, the need to
implement early mobilization safely and effectively in a hospital environment is evident, also bringing
a common language among professionals of all classes, with standardization and correct and pertinent
evolution for each case.
The aim of this
study was to analyze the
prevalence of early mobilization in patients who were
on the seventh
to tenth day of hospitalization
in two ICUs of an emergency
hospital in Goiás, analyze the
degree of mobility using the JH-AMP scale, analyze which risk
factors are present, in addition to comparing
whether there is a difference in mobility according to the patients'
diagnosis.
Methods
This is a descriptive, cross-sectional analytical study, carried out in two ICUs of an
emergency hospital in Goiás, which
is a public unit linked to
the Goiás State Secretariat, with authorization from the research ethics
committee from HUGO (CAAE:
61739122.5.0000.0033). Patients admitted
to two ICUs
at the hospital in question participated in the study.
The inclusion criteria for the study were:
being admitted to one of
the ICUs evaluated; ≥ 18 years old, of both
sexes, who were on the
seventh to tenth day of
hospitalization, regardless
of the diagnosis;
a responsible family member to sign
the informed consent form (ICF). Patients who had
an incomplete electronic medical record, making
it impossible to fill out the assessment form, were excluded
from the research.
Data collection was carried out by a single properly trained evaluator, lasted four months (January-April) and was divided
into four moments. Initially, patients at the research
site were screened through the electronic
medical records system to identify those who fit the
inclusion criteria. Soon after, the
patient able to participate in the research was
invited to explain the research,
read the ICF, clarify the assessments to be carried
out and sign the ICF. For patients who did not
meet the necessary requirements to understand the
term, the research was explained
to the person
responsible.
After signing the ICF, the patient's
personal and clinical data were collected via medical records and transferred
to the evaluation
form created by the researchers,
followed by a safety assessment and the JH-AMP scale, ending with an
analysis of conduct carried out in the day of
evaluation to check compatibility and whether or
not early mobilization occurred in them, both via medical records.
The evaluation form contained acronym, medical record number, sex, date of birth, age, lifestyle habits, hospitalization data (day on which he
was admitted to the hospital, total days of hospitalization
and others), data related to the
trauma (mechanism trauma, associated
factors and others) and clinical
data (peripheral O2 saturation,
heart rate and others).
The safety assessment consists of specific tables,
in which the risk factors for early mobilization present at the
time of the approach were evaluated. These tables come from the study
by Hodgson et al. [4], and
enable the execution of appropriate
mobilization, based on respiratory, cardiovascular, neurological, medical, surgical and other safety
considerations.
The
JH-AMP scale is easy to execute, and its purpose is to assess
mobility and establish a common language for different professionals, systematizing daily goals. Your score is determined according
to the activities
performed. It is made up of
the following classifications: 1 = just lying down, 2 = activities in bed, 3 = sitting on the
edge of the
bed, 4 = transferring out of bed, 5 = standing
for more than or equal to one
minute, 6 = walking ten or more steps, 7 = walking approximately 7.5 m or more (25 feet or more) and
8 = walking approximately
75 m or more (250 feet or more) [5].
The data were categorized and tabulated in an electronic spreadsheet
using the Microsoft Excel
2016 software. The characterization of the patients'
demographic, clinical
profile, ventilation parameters,
vital signs and mobilization risks was performed using
absolute frequency, relative frequency, mean and standard deviation. Data normality was checked using
the Shapiro-Wilk test. The association
between the presence of mobilization
and the patients'
profile was carried out using Pearson's chi-square test and
Student's t test. Data were
analyzed using the Statistical Package for Social Science, (IBM Corporation, Armonk, USA) version 26.0. The significance level adopted was 5% (p < 0.05).
Results
Figure 1 presents the inclusion
flowchart of the population in this study.
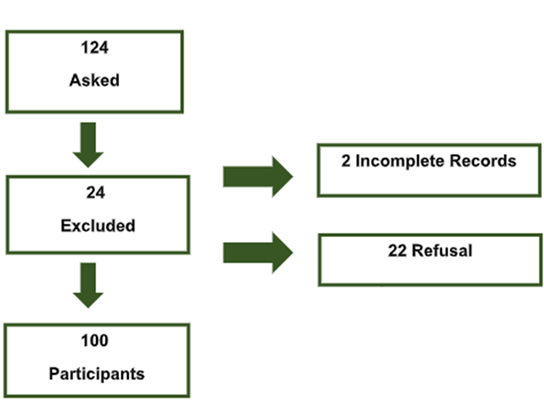
Source: Own
authorship
Figure 1 – Population
inclusion flowchart
Table I shows the patients' profile and association with the presence of
mobilization. It was found that the
average age of the participants was 58.39 ± 18.62 years, with no statistical difference in the different age groups in relation to mobilization
(p = 0.61). Of the participants, 65% (n = 65) were
male (p: 0.46) and 50% (n = 50) of
the total sample were on the 7th day
of hospitalization (p =
0.71). There was no significant difference in mobility in the sectors evaluated (p = 0.07). A mobilization percentage of 27% (n = 27) was found in the ICUs
analyzed, against a scenario in which approximately three quarters of patients
were not mobilized.
Table I - Characterization of the patient
profile and association with the presence
of mobilization (n = 100)
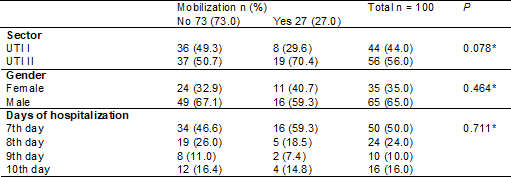
*chi-square; n = absolute frequency; % = relative frequency; ICU = intensive care unit
Table II demonstrates
the characterization of the patients'
clinical profile and association with the presence of
mobilization. A higher
profile of neurological patients was found,
67% (n = 67), followed by
14% (n = 14) clinical, 7% (n = 7) surgical
and 12% (n = 12) others. There was no statistical
significance in relation to diagnosis and
mobilization (p: 0.49), nor
related to the use of neuromuscular blocker (NMB) (p: 0.16) and vasoactive drug (VAD) (p: 0.23). On the other
hand, significance was found in relation
to previous comorbidities, surprisingly, for those who had
comorbidities, they also showed a higher
level of mobilization (p: 0.03). Of these, 67% (n = 31) had systemic arterial hypertension
(SAH) as comorbidities, followed
by 21% (n = 10) with
diabetes mellitus (DM).
A lower degree of
mobilization was also observed in those who used
sedation/analgesia (p: 0.001). Regarding
the main drugs used, the
sedation of choice, in 60% (n = 30) of patients, was the
association between fentanyl and midazolam,
followed by 34% (n = 17) fentanyl alone. Regarding the use of DVA, of those
who used the therapy, 65% (n = 15) used norepinephrine.
Table II - Characterization of the patients'
clinical profile and association with the presence of
mobilization (n = 100)
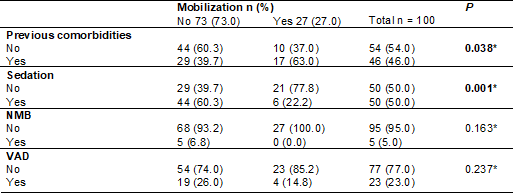
*chi-square; n = absolute frequency; % = relative frequency; NMB = neuromuscular blockade;
VAD - vasoactive drug
Table III represents
the ventilation and mobilization parameters. Participants who were on
spontaneous breathing (SB) had a higher percentage
of mobilization, 63% (n =
17), when compared to patients who
were on IMV (p < 0.001),
corroborating the following finding, where 86% (n = 63) of those who used
IMV were not mobilized (p < 0.001). Of the individuals who were mobilized,
66% (n = 18) performed bedside
procedures, while 29% (n = 8) performed
bedside mobilizations (p
< 0.001). No association was
found between mobilization and ventilation parameters.
Table III - Characterization of the profile of ventilatory parameters and association with the presence of
mobilization (n = 100)
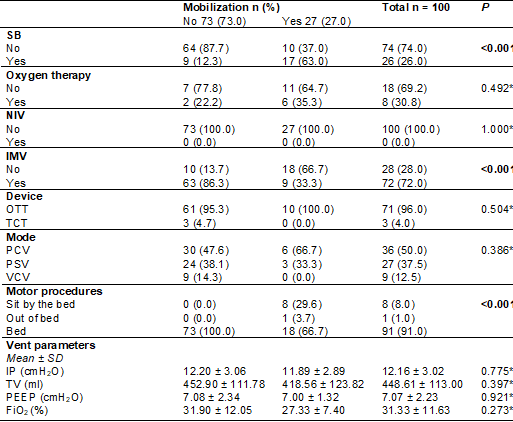
*chi-square; **Student's t-test; n = absolute frequency; % = relative frequency; SD = standard deviation;
SB = spontaneous breathing;
NIV = non-invasive ventilation;
IMV = invasive mechanical ventilation; OTT = orotracheal
tube; TCT = tracheostomy; PCV = pressure
controlled volume; PSV = support
pressure; VCV = controlled
volume; IP = inspiratory pressure;
TV = tidal volume; PEEP = positive pressure at the
end of expiration;
FiO2 – fraction of
inspired oxygen
Table IV provides a
characterization between the risks of
mobilization and its execution, where the number of
mild risks in bed and outside
the bed (p < 0.001), potential in bed (p = 0.03) and significant potential outside the bed (p = 0.002) was inversely proportional
to mobilization; the greater the
number of risks, the lower
the mobilization rate.
Table IV - Characterization of the profile of vital signs and risks of
mobilization and comparison with the presence of
mobilization (n = 100). Expert consensus by Hodgson et al. [4] 2014
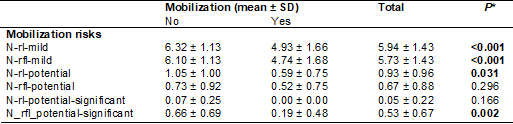
*Student's t-test; SD = standard deviation; n-rl-light = number of mild
risks on the bed; n-rfl-potential = number of potential risks
outside the bed; n-rl-significant-potential
= number of significant potential risks in the bed;
n_rfl_significant-potential = number
of significant potential risks outside the bed
In the JH-AMP scale classification, 73% (n = 73) of patients had classification
1 (lying down), followed by 18% (n = 18) 2 (transfers/activities in bed), 8% (n = 8) 3 (sitting at the bedside)
and only 1% (n = 1) classification 4 (transfer outside the bed).
None of the
patients were in categories from 5 (1 min in standing position) to 8 (ambulation for 75 meters or more).
Discussion
We observed through this study
that sedation, IMV and number of
risks were directly associated with lower mobilization
rates, and that previous comorbidities and SB were associated
with greater mobilization. Furthermore, the mobilization rate was found to
be 27%, which in the authors' opinion
is considered extremely low.
Most of the sample was
made up of
males, 65% (n = 65), which corroborates
similar studies found in the literature [7,8]. This fact can
be explained due to behavioral
and social habits, such as alcohol consumption, smoking, sedentary lifestyle and low
demand for health promotion and prevention
services [9]. It is also a research hospital, a reference in trauma.
Fontela et al. [10] found
the use of sedation among the main risk
factors for mobilization. Of our patients,
50% (n = 50) used this therapy, and of
these, only 22% (n = 6) were mobilized, therefore, sedation also presented a strong barrier in our study.
As previously presented, early mobilization has numerous benefits
and should be applied routinely,
reducing the harmful effects caused by immobility.
Therefore, as soon as possible, sedation should be reduced
to facilitate the implementation of early mobilization
[11]. Still, it is worth remembering that, according to the
expert consensus of Hodgson et al. [4], sedation, at its different levels, does not present an
absolute risk for mobilization, and the risks and
benefits must be analyzed.
There is a low level of
mobilization in ICUs, and when this
occurs, exercises are mostly performed in bed [1]. In our study, a percentage of 66% (n = 18) exercised in bed, classification number 2 on the
JH-AMP scale, was found, followed by 29% (n = 8) at the bedside. Fontela
et al. [10] showed a similar result, in which 60% of their mobilized
patients also received only bed
exercises. In a previous study, our group
discussed exercises in the ICU, reinforcing their importance in minimizing complications during immobilization and the safety
of their execution, even in patients with risk
factors such as the use of VAD, invasive monitoring and high cardiovascular lability
[12].
IMV proved to be
an important barrier to mobilization.
In our study, 86% (n = 63) of those who
used this therapy were not
mobilized and of those who
were mobilized, 63% (n =
17) did not receive this support.
Similar data was presented
in the study by Jolley et al. [13], in which 48% of SB patients were mobilized
vs 26% of mobilization in the mechanically ventilated ones. In this same
study, they also pointed out as the main explanation
for the higher level of mobilization
in patients with tracheostomy (TCT), or without an artificial airway, the smaller
amount of equipment and the
lower risk of complications during execution. However, Nydahl et al.
[14], in their systematic
review, revealed a minimal proportion of adverse events in patients with an artificial airway, reaffirming the safety of
mobilization in these patients. It is also worth highlighting
that according to Hodgson et al. [4], the
presence of an orotracheal tube (OTT) constitutes a mild risk for exercises in bed and outside
the bed.
It is essential to
consider the importance of the
participation of a trained and qualified
team to carry
out the mobilization, as discussed in the study by Curtis et al.
[15], presenting that the experience of the activity
must be kept in mind and developed by
a competent team, and this competence
is developed through training, protocols and tireless hours of practice.
This study has limitations that must be highlighted.
All data presented were obtained via medical records and may
suffer interference from those responsible
for the records. Regarding those who used VAD’s,
the doses used were not quantified,
which could also generate changes
in the results.
Conclusion
The present study made
it possible to analyze the prevalence
of mobilization, as well as the degree
of mobility and risks present
in ICU patients. From the data presented, it is possible to
conclude that a significant percentage of patients were
not mobilized. The greater the number
of risks, including sedation and OTT, the lower
the mobilization rate. There was no difference
in mobility rates, considering
the different diagnoses. Therefore, greater commitment to health
education for rehabilitation
professionals is necessary, so that
there is a more effective, early and safe mobilization, even in patients who present risks.
It is suggested that new studies be carried out that evaluate this
same profile of individuals in situ and at the bedside,
with the aim of discovering
new outcomes.
Potential conflict
of interest
The authors declare that they have no conflicts
of interest in publishing this study.
Financing source
The authors did not
receive funding of any kind
to carry out this study.
Authors' contributions
Conception and
design of the study: Campos MLS, Nunes ELG, Souza lP,
Gardenghi G; Data collection:
Campos MLS; Statistical analysis:
Campos MLS, Nunes ELG, Souza lP, Gardenghi
G; Data interpretation: Campos MLS, Nunes ELG,
Gardenghi G; Text
composition: Campos MLS, Nunes ELG, Souza lP, Gardenghi G; Approval of the final version to be published:
Campos MLS, Ferreira BK, Barbosa IOF, Nunes ELG, Souza lP,
Gardenghi G, Petto J.
References
- Pissolato JSP, Schlottfeldt
CF. Mobilização precoce na unidade de terapia intensiva adulta. Fisioter Bras. 2018;19(3):377. doi: 10.33233/fb.v19i3.690 [Crossref]
- Kappel Se, Larsen-Engelkes
TJ, Barnett RT, Alexander JW, Klinkhammer Nl, Jones MJ, et al. Creating a culture of mobility.
Am J Nurs. 2018;118(12):44-50. doi: 10.1097/01.naj.0000549690.33457.bb [Crossref]
- Klein LM, Young D, Feng D, Lavezza A, Hiser S, Daley KN, Hoyer EH. Increasing patient mobility through an individualized goal-centered hospital mobility program: a quasi-experimental quality improvement project. Nurs Outlook. 2018;66(3):254-62. doi: 10.1016/j.outlook.2018.02.006 [Crossref]
- Hodgson CL, Stiller K, Needham DM, Tipping CJ, Harrold M, Baldwin CE, et al. Expert consensus and recommendations on safety criteria for active mobilization of mechanically ventilated critically ill adults. Crit Care. 2014;18(6). doi: 10.1186/s13054-014-0658-y [Crossref]
- Johns Hopkins. Tools user manual. Baltimore, 2022 [citado 2022 Abr 7]. Disponível em:
https://www.hopkinsmedicine.org/physical_medicine_rehabilitation/education_t raining/amp/conference/index.html
- Jette DU, Stilphen M, Ranganathan VK, Passek SD, Frost FS, Jette AM. Am-pac “6-clicks” functional assessment scores predict acute care hospital discharge destination. Phys Ther. 2014;94(9):1252-61. doi: 10.2522/ptj.20130359 [Crossref]
- Prece A, Cervantes J, Mazur CS, Visentin A. Perfil de
pacientes em terapia intensiva: necessidade do conhecimento para organização do
cuidado. Cadernos da Escola de Saúde. 2016;2(16):35-48. Disponível em:
https://portaldeperiodicos.unibrasil.com.br/index.php/cadernossaude/article/view/2462
- Rodriguez AH, Bub MB, Perão OF, Zandonadi G, Rodriguez MD. Características epidemiológicas e causas de óbitos em pacientes internados em terapia intensiva. Rev Bras Enferm. 2016;69(2):229-34. doi: 10.1590/0034-7167.2016690204i [Crossref]
- Marques CR, Santos MR,
Passos KS, Naziazeno SD, Sá LA, Santos ES.
Caracterização do perfil clínico e sociodemográfico de pacientes admitidos em
uma unidade de terapia intensiva. Interfaces Cient
Saúde Ambient. 2020;8(2):446-56. doi: 10.17564/2316-3798.2020v8n2p446-456 [Crossref]
- Fontela PC, Forgiarini Júnior LA, Friedman G. Clinical attitudes and perceived barriers to early mobilization of critically ill patients in adult intensive care units. Rev Bras Ter Intensiva. 2018;30(2). doi: 10.5935/0103-507x.20180037 [Crossref]
- Cunha IP, Ultra PO. Uso da
mobilização precoce em pacientes em ventilação mecânica na UTI. Revista do
Fisioterapeuta [internet]. 2023;22:30-38. Disponível
em:
https://revistadofisioterapeuta.com.br/revistadown/edicao22-uso-mobilizacao-precoce.pdf
- Gardenghi G. Exercício em unidades de terapia
intensiva, segurança e monitorização hemodinâmica. Rev
Bras Fisiol Exerc. 2020;19(1):3-12. doi: 10.33233/rbfe.v19;1.3981 [Crossref]
- Jolley SE, Moss M, Needham DM, Caldwell E, Morris PE, Miller RR, et al. Point prevalence study of mobilization practices for acute respiratory failure patients in the United States. Crit Care Med. 2017;45(2):205-15. doi: 10.1097/ccm.0000000000002058 [Crossref]
- Nydahl P, Ruhl AP, Bartoszek G, Dubb R, Filipovic S, Flohr HJ, et al. Early mobilization of mechanically ventilated patients. Crit Care Med. 2014;42(5):1178-86. doi: 10.1097/ccm.0000000000000149 [Crossref]
- Curtis l, Irwin J. Ambulation of patients who are mechanically ventilated: nurses’ views. Nurs Manag. 2017;24(4):34-9. doi: 10.7748/nm.2017.e1599 [Crossref]