Rev Bras Fisiol Exerc. 2024;23:e235573
doi: 10.33233/rbfex.v23i1.5573
REVIEW
Effects of resistance exercises on hemodynamic responses: a systematic review with meta-analysis
Efeitos dos exercícios
resistidos nas respostas hemodinâmicas: uma revisão sistemática de revisões com
meta-análise
Ramon Martins Barbosa1,2,
Alan Carlos Nery dos Santos2, Marvyn de
Santana do Sacramento1,3,4, Tailma Costa
de Jesus5, Jefferson Petto1,3
1Escola Bahiana de Medicina e Saúde
Humana – EBMSP, Salvador, BA, Brazil 2Faculdade
da Região Sisaleira – FARESI, Conceição do Coité, BA, Brazil
3Actus Cordios
Reabilitação Cardiovascular, Salvador, BA, Brazil
4Faculdade Adventista da Bahia, Capoeiruçu, BA, Brazil
5Centro Universitário Social da Bahia,
Salvador, BA, Brazil
Received 2023 November
15; Accepted 2024 February
3
Correspondence: Ramon Martins Barbosa, ramonmartinsbarbosa@hotmail.com
How to
cite
Barbosa RM, Santos
ACN, Sacramento MS, Jesus TC, Petto J. Effects of resistance exercises
on hemodynamic responses: a
systematic review with
meta-analysis. Rev Bras Fisiol Exerc.
2024;23:e235573. doi: 10.33233/rbfex.v23i1.5573
Abstract
Objectives: To analyze the effects
of Resistance Exercise (RE) on hemodynamic responses related to blood pressure.
Methods: Systematic
review, Prospero CRD42023422584, carried out on the following
databases: PubMed/Medline, PEDro, Cochrane and VHL Regional
Portal, between June and December 2023. Descriptors: "Resistance
Training", "Blood Pressure"
and, "Systematic
Reviews. Included: Systematic
reviews, composed of randomized clinical trials and/or
controlled intervention studies, which tested static or
dynamic resistance exercise interventions, in adult individuals, for outcomes associated with hemodynamic responses such as: blood pressure, heart rate and VO2max. There were no restrictions on the time of
publication of the studies. The risk of bias was
assessed using the AMSTAR-2 scale. Results: 174 articles were identified, but after analysis
7 were included. These were published
between 2005 and 2020, totaling a sample of 7,818 individuals of both sexes. The main results indicate
that RE promotes a statistically significant and clinically relevant improvement in systolic blood pressure (SBP), diastolic blood pressure (DBP) and mean arterial pressure (MAP). There were improvements in VO2max
and VO2peak. Conclusion:
We concluded that RE was statistically
significant and clinically relevant for reducing SBP, DBP and MAP. An improvement in VO2max
and VO2peak was also observed. Furthermore, Isometric Resistance Exercise promoted a greater blood pressure reduction when compared to Aerobic
Resistance Exercise and Dynamic Resistance Exercise. These results are supported by the high/moderate
methodological quality of the included
reviews.
Keywords: resistance
training; blood pressure; hypertension
Resumo
Objetivos: Analisar os efeitos do Exercício
Resistido (ER) nas respostas hemodinâmicas relacionadas a pressão arterial. Métodos:
Revisão sistemática, Prospero CRD42023422584, realizada nas bases de dados: PubMed/Medline, PEDro, Cochrane e
Portal Regional da BVS, entre junho e dezembro de 2023. Descritores: “Resistance Training”, “Blood Pressure” e, “Systematic Reviews.
Incluídos: Revisões sistemáticas, composta por ensaios clínicos randomizados
e/ou estudos de intervenção controlados, que testaram intervenções de exercício
resistido estático ou dinâmico, em indivíduos adultos, para desfechos
associados as respostas hemodinâmicas como: pressão arterial, frequência
cardíaca e VO2máx. Não foram realizadas restrições quanto ao tempo
de publicação dos estudos. O risco de viés foi avaliado pela escala AMSTAR-2. Resultados:
Identificamos 174 artigos, contudo, após análise, 7 foram incluídos. Esses
foram publicados entre 2005 e 2020, totalizando amostra de 7.818 indivíduos de
ambos os sexos. Os principais resultados indicam que o ER promove uma melhora
estatisticamente significativa e clinicamente relevante na pressão arterial
sistólica (PAS), pressão arterial diastólica (PAD) e Pressão arterial média
(PAM). Houve melhoras do VO2máx e no VO2 de Pico. Conclusão:
Nós concluímos que o ER foi estatisticamente significativo e clinicamente
relevante para redução da PAS, PAD e PAM. Também foi observada uma melhora no
VO2máx e o VO2 de Pico. Além disso, o Exercício Resistido
Isométrico promoveu uma redução pressórica maior quando comparado ao Exercício
de Resistência Aeróbica e o Exercício Resistido Dinâmico. Esses resultados são
apoiados pela alta/moderada qualidade metodológica das revisões incluídas.
Palavras-chave: treinamento resistido; pressão
arterial; hipertensão
Introduction
Cardiovascular
diseases are a global public
health problem. They directly
or indirectly resulted in high costs for health agencies, and it is worth mentioning
their negative impacts on morbidity and
mortality, functional and biopsychosocial aspects of the
population affected by such a clinical
condition [1]. Annually, around 17 million people die from cardiovascular diseases, with Arterial Hypertension (AH) being responsible for 9.4 million
deaths and a disease burden of 7% [2]. Added to this,
AH is responsible for 49% of deaths from heart disease and
51% from stroke, however these data may be underestimated,
since the prevalence of AH is higher in middle
and low-income countries, and the number
of unpublished and untreated patients
is large, which may reflect
deficiencies in health services and, making AH an important global health condition [3,4].
Interestingly, a population
study suggested that the prevalence
of AH has almost doubled in the last three
decades. Thus, in the 1980s, around 600 million individuals over the age of 25 had
high blood pressure and, by mid-2008, this number had
already grown to around 1 billion
people [5]. Another point is that physical
inactivity, overweight and obesity, smoking, excess salt in the diet and alcohol
consumption have been described as risk factors that,
once modified, can alter blood
pressure [6]. Furthermore, although a large part of the
population uses antihypertensive
medications, which are effective and most
of the time have minimal side
effects, the costs end up
being high and they may not
be the best
strategy for blood pressure control, since around 50% of patients do not benefit from
such a medication strategy [7].
With this in mind,
the main national and international
recommendations suggest that evidence-based non-pharmacological lifestyle strategies are first-line therapies for attenuating BP. Therefore, weekly moderate physical activity levels close to 150 minutes, weight reduction and smoking are effective strategies that express a statistically significant and clinically relevant reduction in BP [8]. Furthermore, studies suggest that aerobic
exercise is the most prescribed
modality for BP control, however its adherence is reduced, mainly
due to the
time spent and the considerable energy expenditure to obtain such
gains [9,10].
Added to this, although previously associated with exaggerated hypertensive responses, recent studies suggest that resistance exercise (RE) is a safe and effective intervention
to promote BP reduction, being more expressed in studies involving isometric resistance exercise. In this way, it can
be configured as a potential strategy, once properly prescribed,
it can result in lower individual costs, as well as to health
bodies, and perhaps shorter execution time [11,12,13]. Thus, the present study
aims to analyze
the effects of resistance exercise
on hemodynamic responses related to blood
pressure.
Methods
Study type
This is a systematic review composed of systematic reviews with meta-analysis, structured based on the criteria
established by the "Preferred Reporting Items for Systematic Reviews and Meta-Analyses" (PRISMA) guideline
[14], and the methodological guide proposed by Smith et al.
[15], to answer the following clinical
question: What are the chronic effects
of static and dynamic resistance
exercise on hemodynamic responses associated with blood pressure?
The study was prospectively registered in Prospero under the protocol number:
CRD42023422584.
Eligibility criteria
The study included: 1) Systematic reviews; 2) composed of randomized clinical
trials and/or controlled intervention
studies; 3) that tested static or
dynamic resistance exercise interventions; 4) in adult individuals; 5) for outcomes associated with hemodynamic responses such as blood pressure,
heart rate, and maximum oxygen uptake (VO2max). 6) Such
studies should be available in full. There were no restrictions
regarding language or publication time of the studies.
On the other
hand, the following were excluded: 8) systematic reviews about RE that conducted
mixed protocols with other training modalities (aerobic training and breathing exercises,
and training with blood flow restriction),
9) systematic reviews about
RE e that did not describe the
comparison groups of the included
studies; 10) systematic
reviews that aimed to analyze only
the principles related to the
prescription of RE; and 11) systematic reviews that analyzed only
pre-hypertensive and hypertensive individuals, or those with
other associated comorbidities.
Outcome of interest
For the study, "Hemodynamic Responses" are related
to the movements
and forces involved in the displacement of blood through
the cardiovascular system. "Blood
Pressure" is related to the
pressure exerted by blood on
the walls of the arteries
during ventricular systole,
defined based on the "Medical Subject Headings".
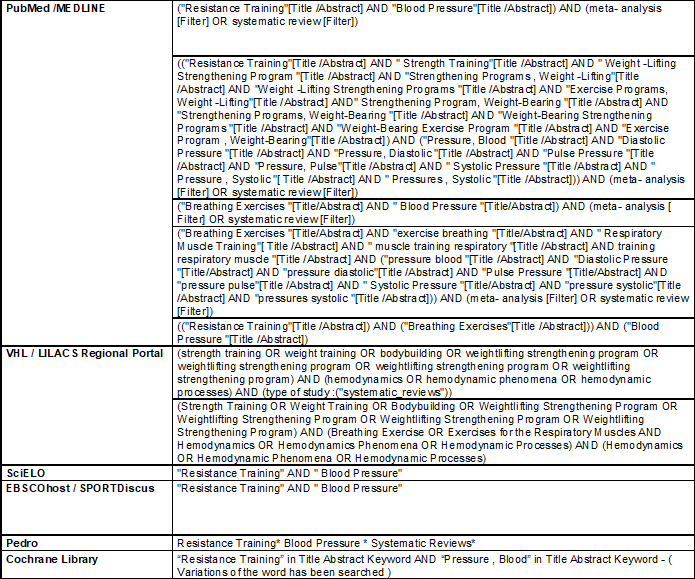
Search strategy
Searches were conducted in the databases: PubMed/Medline, PEDro, COCHRANE, and Regional
Portal of BVS, by two independent authors [R.M.B and A.C.N.S], between June and
December 2023. The descriptors
were selected using the "Medical Subject Headings" - (MESH) and "Health Sciences Descriptors" (DeCS), selecting the following
descriptors: "Resistance
Training", "Blood Pressure",
and "Systematic
Reviews", using the boolean operators [AND], [OR], and [NOT] for the respective intersections, as described in Table I.
Chart I - Search strategies for databases
Searching other resources
Additionally, with the aim of
identifying other published, unpublished, or ongoing studies,
we consulted the PROSPERO prospective register of systematic
reviews and grey literature using Google Scholar. We conducted direct citation tracking of all included studies
(and other relevant studies) using Google Scholar (scholar.google.co.uk/) for additional references to relevant studies.
Study selection and data extraction
Study selection was conducted by
two independent authors [R.M.B] and [A.C.N.S], and in case of any disagreements, a third reviewer was consulted [J.P]. Thus, a thorough review of titles and
abstracts was conducted, with final selection based on the
aforementioned eligibility criteria. As shown in Tables 1 and 2, eligible studies were selected for full-text reading, further
evaluation against the selection criteria,
and data extraction regarding: 1) Author and year of
study publication; 2) Objective of the
systematic review; 3) Type of systematic review/number of studies
included in the review; 4) Population (population characteristics); 5) Intervention
protocol (type of resistance exercise,
weekly frequency, intensity, and duration); 6) Control (control form); 7) Methods (outcome measurements); 8) Outcomes (blood pressure); and 9) Main results
obtained by the studies.
The references reviewed and included In this review were analyzed by
the second reviewer [A.C.N.S], aiming to identify potential
studies not identified in the searches of electronic
databases. Figure 1 summarizes
the study selection strategies that compose the
scope of this systematic review.
Risk of
bias
The quality of each
review was assessed by two independent
authors [R.M.B and
A.C.N.S], using the methodological evaluation criteria proposed by the AMSTAR-2 scale. It consists of a checklist composed of 16 items, which
can be answered
with “Yes”, “Partial Yes”, or “No”, with the
aim not to
generate a final score. It classifies
the review as “High Quality”
= Zero or one non-critical weakness: The systematic review provides a
precise and comprehensive summary of the
results. “Moderate Quality” = More than one non-critical weakness *: The systematic review
has more than one weakness, but
no critical flaws. “Low Quality” = One critical flaw
with or without
non-critical weaknesses:
The review has one critical flaw and
may not provide
a precise and comprehensive
summary of the available studies,
and “Critically Low Quality” = More than one critical
flaw with or without non-critical weaknesses: The review has more than one
critical flaw and should not
be considered to provide a precise and comprehensive summary of the
available studies. This is the
validated and frequently used AMSTAR scale revision.
Results
The search strategies and references analyzed through manual search returned a total of 174 articles. However, after review by the reviewers
[R.M.B and A.C.N.S], 35 were
eliminated due to duplication, leaving 139 studies. After removal based
on title and abstract, 16 studies remained. In another stage, after screening
based on eligibility criteria, another 9 studies were excluded. The main reasons for exclusion were: systematic reviews involving resistance exercise with blood flow
restriction, reviews on resistance exercise in metabolic syndrome, reviews containing mixed protocols of resistance
exercise with cyclic exercise, reviews involving theses and dissertations of master’s and
doctoral degrees, and reviews involving only hypertensive individuals and/or those with
underlying pathologies. Finally, 7 studies [11,16,17,18,19,20,21] met the established
selection criteria, as summarized in Figure 1.
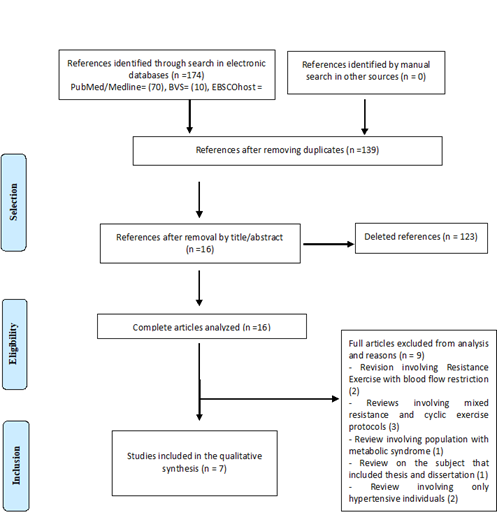
Source: Prepared
by the authors
Figure 1 - Flowchart of
selection of studies that make up the review
According to the data presented in Table I, we can observe that the included
studies were published between 2005 and 2020, and 100% of the studies
were systematic reviews with meta-analyses. Additionally, the number of articles
included in each review varied between 6 and 93 randomized clinical trials and controlled intervention studies, with over 60% of the groups involved
in the clinical trials being normotensive
individuals. Regarding the characteristics of the population,
the sample size ranged from 139 to 5,223 individuals, totaling 7,818 individuals of both sexes,
with reported ages ranging from 19 to 84 years. Furthermore,
the included studies aimed to
analyze the effects of resistance
exercise on blood pressure responses in normotensive, pre-hypertensive, and hypertensive individuals, based on our outcomes
of interest: systolic blood pressure, diastolic blood pressure, mean arterial pressure, heart rate, and VO2max.
Table I - Characteristics of studies and
population
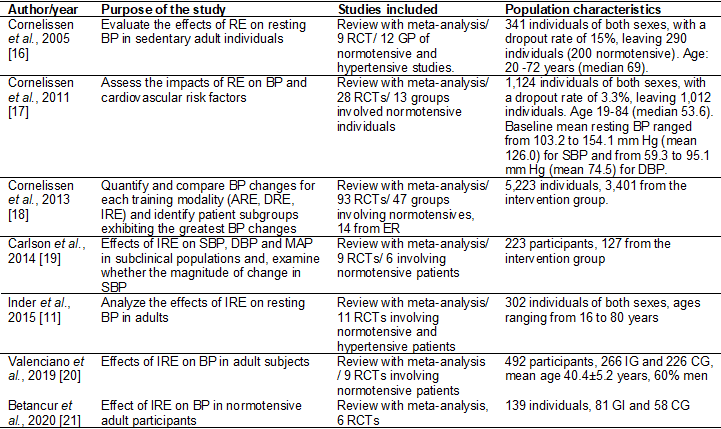
RE = Resistance Exercise; BP = Blood Pressure; RCT = Randomized clinical trial; ARE = Aerobic resistence Exercise; DRE =
Dynamic Resistance Exercise;
IRE = Isometric Resistance Exercise; SBP = Systolic Blood Pressure; DBP = Diastolic Blood Pressure; MAP = Mean arterial Pressure; IG = Intervention Group; CG = Control Group
In Table II, we can
observe that in 100% of the studies, participants
in the intervention group were subjected
to RE for lower limbs, upper limbs,
and trunk, being prescribed in static and/or
dynamic modalities. The intervention protocol for Dynamic
Resistance Exercise (DRE) ranged from 1 to
14 exercises, 1 to 4 sets of 6 to 36 repetitions,
with intensities from 30% to 100% of 1RM, while for Isometric Resistance Exercise (IRE), most protocols used 4 sets of 2 to 3 minutes of manual grip or leg exercises, with intensities from 10% to 40% of maximal voluntary contraction. Training frequency ranged from 1 to
7 times per week, with durations from 3 to 52 weeks. Furthermore,
when examining the comparison methods, the most
used were control group without
any intervention and recommendations to follow a normal lifestyle, maintaining physical activity levels, stretching sessions three times a week, in addition to continued
education sessions and dialogue calls on physical exercise.
Outcomes such as: Systolic Blood Pressure (SBP), Diastolic Blood Pressure (DBP), Mean Arterial Pressure (MAP), Maximum Oxygen Volume (VO2max),
and heart rate were evaluated by methods such
as: automated BP measurements,
auscultation, brachial oscillometry, and ambulatory blood pressure monitoring (ABPM).
Table II - Summary of the evaluation
process, intervention, outcomes and main
results of the studies reviewed
The main results observed
in the studies included in this review indicate that resistance
exercise promotes a statistically significant and clinically relevant improvement in SBP, DBP,
and MAP. Additionally, improvements in VO2max and
VO2peak were observed.
Resistance exercise was statistically significant but not clinically relevant for improving resting heart rate (RHR).
Regarding methodological
quality, as shown in Table III, we can
see that one of the
studies has high methodological quality [21], while the other
six studies have moderate methodological
quality [11,16,17,18,19,20]. The most
critical point was regarding the funding
source of the included studies,
where none of the studies
declared the related information.
Table III - Methodological quality - AMSTAR 2
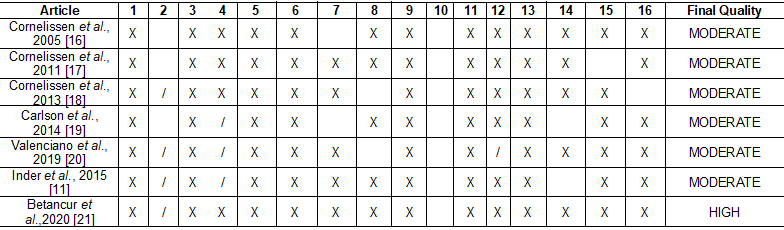
X= Yes; /
= Partial Yes.
1. The research questions and inclusion criteria
for the review included the components of PICO; 2. The review report contained an explicit
statement that the review methods were established before the review was conducted and
the report justified any significant
deviations from the protocol; 3. Review authors explained their selection of study designs for inclusion in the review; 4.
Review authors used a comprehensive literature search strategy; 5. The review authors carried out the study selection
in duplicate; 6. Review authors
performed data extraction
in duplicate; 7. The review authors
provided a list of excluded studies
and justified the exclusions; 8. The review authors described the included studies
in adequate detail; 9 . The review authors used a satisfactory technique to assess
the risk of bias ( RoB
) in individual studies that
were included in the review; 10 . Review authors reported the funding
sources for the studies included in the review; 11. If a meta-analysis was performed,
the review authors used appropriate methods for statistical combination of results; 12. If a meta-analysis was performed,
the review authors assessed the potential
impact of RoB in individual studies on the results
of the meta-analysis or other
evidence synthesis; 13.
Review authors took RoB into consideration
in individual studies when interpreting/discussing review results; 14. The review authors provided a satisfactory explanation for, and discussion of, any observed heterogeneity
in the review results; 15. If they performed
a quantitative synthesis, the review authors performed an adequate
investigation of publication bias (minor study bias) and discussed its likely impact on the
review results; 16. Review authors
have reported any potential sources
of conflict of interest, including
any funding they received to
conduct the review
Discussion
In
response to the objectives of this
systematic review, we identified that resistance exercise was statistically significant and clinically relevant for reducing SBP, DBP, and MAP. Additionally, an improvement in VO2max and
VO2peak was observed.
Moreover, IRE promoted greater blood pressure
reductions compared to Aerobic Resistance
Exercise (ARE) and DRE. These results are supported by the
high/moderate methodological
quality of the included reviews.
Regarding the reduction of SBP and DBP, the included
studies suggest a statistically significant and clinically relevant reduction [11,16-21]. In
fact, evidence suggests that a clinically relevant reduction is around
2 mmHg for SBP and 3 mmHg for DBP [22]. Additionally, this data is crucial, as studies suggest that a decrease at this
level may reduce the risk
of coronary artery disease by 5%, stroke by
8%, and all-cause mortality by 4% [23].
Furthermore, the studies suggest some physiological mechanisms that may justify
the reduction in blood pressure after resistance exercise. Thus, research has indicated
that resistance exercise can increase
the release of nitric oxide metabolites and vasodilatory substances, which may result in a reduction in peripheral vascular resistance and consequently cardiac output
[11,16,19]. Indeed, IRE can
promote an acute stimulus to the metaboreflex
aiming to re-establish muscle blood flow, which
may result in lower tissue oxidative
stress, improved vascular endothelial
function, and baroreflex sensitivity as well as long-term autonomic balance, associated with increased parasympathetic activation
[11,19,24,25,26].
Moreover, when other related variables
were evaluated, there was a reduction
in VO2max and VO2peak [16,17]. Thus, resistance exercise can promote
improvements in cardiorespiratory
conditioning. In fact, a recent review suggests that much of
this improvement is due to
the release and action of myokines
[27]. They induce local changes
in muscle regulating muscle development/function, as they can potentiate metabolic pathways and attenuate inflammatory
responses, which would increase maximum oxygen consumption by muscle tissue
[27,28]. Another point is that a significant portion of the
prescribed exercises were bi-articular, thus involving various muscle groups, a fact that may have
potentiated metabolic demand and consequently
increased VO2max and
VO2peak. Thus, the
amount of muscle mass used
during exercise seems to be
one of the
determinants for the increment of the
aerobic component during resistance exercise. Improvement in this valence has
been associated with physical fitness improvement, which is commonly associated
with reduced cardiovascular
event deaths and increased longevity [29].
Another interesting finding is that
IRE promoted greater blood pressure reductions compared to ARE and DRE [18]. Thus, studies suggest
that IRE is capable of promoting sustained arterial occlusion during training, resulting in a rebound effect, capable of inducing
arterial vasodilation, related
to the release of substances by
the vascular endothelium, improving peripheral vascular resistance [30]. In addition, the literature has been pointing
to an IRE protocol, composed of 4 sets of 2-3 minutes, with 3 minutes of interval between repetitions, with intensity of 10-40% of MVC, being able
to promote such systemic effects
[17,18,19,20,21].
In addition to the
aspects discussed above, the findings
have some limitations that need to
be discussed. First, most of
the included reviews did not report
an average of the blood
pressure levels of the studies
included in the reviews, which limits the
analysis of the findings. Secondly,
there was great heterogeneity related to intervention
protocols, which limits data extrapolation, as well as the definition
of a minimally effective protocol, especially related to DRE. Another point is regarding the
outcome measurement methods, which varied between studies, thus limiting
comparison of measurement methods. Finally, the evidence
quality of most studies included
in the reviews was moderate, which indicates that the true effect
is close to that estimated, but there is
a possibility of being substantially different. However, these limitations do not invalidate the presented data, as they are consistent with others presented
in the literature.
Conclusion
We conclude that resistance exercise was statistically
significant and clinically relevant for reducing SBP, DBP, and MAP. Additionally, an improvement in VO2max and
VO2peak was observed. Moreover, IRE promotes greater blood pressure
reduction compared to ARE and DRE. These results are supported by the
high/moderate methodological
quality of the included reviews.
Conflicts of
interest
The authors declare that they have no conflict
of interest.
Financing source
The authors did not
receive any direct or indirect funding
for their research.
Authors' contribution
Conception and
design of the research: Barbosa RM, Santos ACN; Data acquisition:
Barbosa RM, Santos ACN; Data analysis and interpretation: all authors; Manuscript
writing: all authors; Critical
review of the manuscript for important intellectual content: Petto
J, Santos ACN.
References
- Roth GA, Mensah
GA, Johnson CO, Addolorato G, Ammirati
E, Baddour LM, et al. GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019:
Update from the GBD 2019 Study. J Am Coll Cardiol. 2020 Dec 22;76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010 [Crossref]
- World Health Organization. Global Status Report on
Noncommunicable Diseases
2014. Geneva, Switzerland: World Health Organization; 2014.
- Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. 2020 Apr;16(4):223-37. doi: 10.1038/s41581-019-0244-2 [Crossref]
- Sarki AM, Nduka CU, Stranges S, Kandala NB, Uthman OA. Prevalence of hypertension in low- and middle-income countries: a systematic review and meta-analysis. Medicine (Baltimore). 2015 Dec;94(50):e1959. doi: 10.1097/MD.0000000000001959 [Crossref]
- World Health Organization. A Global brief on hypertension: silent killer, global public health crisis. Geneva, Switzerland: World Health Organization;
2013.
- Ng R, Sutradhar R, Yao Z, Wodchis WP, Rosella LC. Smoking, drinking, diet and physical activity-modifiable lifestyle risk factors and their associations with age to first chronic disease. Int J Epidemiol. 2020 Feb 1;49(1):113-30. doi: 10.1093/ije/dyz078 [Crossref]
- Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988-2000. JAMA. 2003 Jul 9;290(2):199-206. doi: 10.1001/jama.290.2.199 [Crossref]
- Warburton DE, Nicol CW, Bredin SS. Health benefits of physical activity: the evidence. CMAJ. 2006 Mar 14;174(6):801-9. doi: 10.1503/cmaj.051351 [Crossref]
- Kelley GA, Kelley KA, Tran ZV. Aerobic exercise and resting blood pressure: a meta-analytic review of randomized, controlled trials. Prev Cardiol. 2001 Spring;4(2):73-80. doi: 10.1111/j.1520-037x.2001.00529.x [Crossref]
- Igarashi Y, Akazawa N, Maeda S. Regular aerobic exercise and blood pressure in East Asians: A meta-analysis of randomized controlled trials. Clin Exp Hypertens. 2018;40(4):378-89. doi: 10.1080/10641963.2017.1384483 [Crossref]
- Inder JD, Carlson DJ, Dieberg G, McFarlane JR, Hess NC, Smart NA. Isometric exercise training for blood pressure management: a systematic review and meta-analysis to optimize benefit. Hypertens Res. 2016 Feb;39(2):88-94. doi: 10.1038/hr.2015.111 [Crossref]
- Baffour-Awuah B, Pearson MJ, Dieberg G, Smart NA. Isometric resistance training to manage hypertension: systematic review and meta-analysis. Curr Hypertens Rep. 2023 Apr;25(4):35-49. doi: 10.1007/s11906-023-01232-w [Crossref]
- Smart NA, Way D, Carlson D, Millar P, McGowan C, Swaine I, Baross A, Howden R, Ritti-Dias R, Wiles J, Cornelissen V, Gordon B, Taylor R, Bleile B. Effects of isometric resistance training on resting blood pressure: individual participant data meta-analysis. J Hypertens. 2019 Oct;37(10):1927-38. doi: 10.1097/HJH.0000000000002105 [Crossref]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal. pmed.1000097 [Crossref]
- Smith V, Devane D, Begley CM, Clarke M. Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Med Res Methodol. 2011;11(1):1–6. doi: 10.1186/1471-2288-11-15 [Crossref]
- Cornelissen VA, Fagard RH. Effect of resistance training on resting blood pressure: a meta-analysis of randomized controlled trials. J Hypertens. 2005 Feb;23(2):251-9. doi: 10.1097/00004872-200502000-00003 [Crossref]
- Cornelissen VA, Fagard RH, Coeckelberghs E, Vanhees L. Impact of resistance training on blood pressure and other cardiovascular risk factors: a meta-analysis of randomized, controlled trials. Hypertension. 2011 Nov;58(5):950-8. doi: 10.1161/HYPERTENSIONAHA.111.177071 [Crossref]
- Cornelissen VA, Smart NA. Exercise training for blood pressure: a systematic review and meta-analysis. J Am Heart Assoc. 2013 Feb 1;2(1):e004473. doi: 10.1161/JAHA.112.004437 [Crossref]
- Carlson DJ, Dieberg G, Hess NC, Millar PJ, Smart NA. Isometric exercise training for blood pressure management: a systematic review and meta-analysis. Mayo Clin Proc. 2014 Mar;89(3):327-34. doi: 10.1016/j.mayocp.2013.10.030 [Crossref]
- López-Valenciano A, Ruiz-Pérez I, Ayala F, Sánchez-Meca J, Vera-Garcia FJ. Updated systematic review and meta-analysis on the role of isometric resistance training for resting blood pressure management in adults. J Hypertens. 2019 Jul;37(7):1320-1333. doi: 10.1097/HJH.0000000000002022 [Crossref]
- Loaiza-Betancur AF, Pérez Bedoya E, Montoya Dávila J, Chulvi-Medrano I. Effect of isometric resistance training on blood pressure values in a group of normotensive participants: a systematic review and meta-analysis. Sports Health. 2020 May/Jun;12(3):256-262. doi: 10.1177/1941738120908070 [Crossref]
- Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018 Jun;71(6):1269-324. Erratum in: Hypertension. 2018 Jun;71(6):e136-e139. Erratum in: Hypertension. 2018 Sep;72(3):e33. doi: 10.1161/HYP.0000000000000066 [Crossref]
- Tian D, Meng J. Exercise for prevention and relief of cardiovascular disease: prognoses, mechanisms, and approaches. Oxid Med Cell Longev. 2019 Apr 9;2019:3756750. doi: 10.1155/2019/3756750 [Crossref]
- Green DJ, Maiorana A, O'Driscoll G, Taylor R. Effect of exercise training on endothelium-derived nitric oxide function in humans. J Physiol. 2004:15;561(Pt 1):1-25. doi: 10.1113/jphysiol.2004.068197 [Crossref]
- Lawrence MM, Cooley ID, Huet YM, Arthur ST, Howden R. Factors influencing isometric exercise training-induced reductions in resting blood pressure. Scand J Med Sci Sports. 2015 Apr;25(2):131-42. doi: 10.1111/sms.12225 [Crossref]
- Taylor AC, McCartney N, Kamath MV, Wiley RL. Isometric training lowers resting blood pressure and modulates autonomic control. Med Sci Sports Exerc. 2003;35(2):251-6. doi: 10.1249/01.MSS.0000048725.15026.B5 [Crossref]
- Smart TFF, Doleman B, Hatt J, Paul M, Toft S, Lund JN, Phillips BE. The role of resistance exercise training for improving cardiorespiratory fitness in healthy older adults: a systematic review and meta-analysis. Age Ageing. 2022 Jun 1;51(6):afac143. doi: 10.1093/ageing/afac143 [Crossref]
- Gonzalez-Gil AM, Elizondo-Montemayor L. The Role of exercise in the interplay between myokines, hepatokines, osteokines, adipokines, and modulation of inflammation for energy substrate redistribution and fat mass loss: a review. Nutrients. 2020 Jun 26;12(6):1899. doi: 10.3390/nu12061899 [Crossref]
- Kokkinos P, Faselis C, Samuel IBH, Pittaras A, Doumas M, Murphy R, Heimall MS, Sui X, Zhang J, Myers J. Cardiorespiratory fitness and mortality risk across the spectra of age, race, and sex. J Am Coll Cardiol. 2022 Aug 9;80(6):598-609. doi: 10.1016/j.jacc.2022.05.031 [Crossref]
- Badrov MB, Bartol CL, DiBartolomeo MA, Millar PJ, McNevin NH, McGowan CL. Effects of isometric handgrip training dose on resting blood pressure and resistance vessel endothelial function in normotensive women. Eur J Appl Physiol. 2013;113(8):2091-100. doi: 10.1007/s00421-013-2644-5 [Crossref]