Rev Bras Fisiol Exerc. 2024;23:e235580
doi: 10.33233/rbfex.v23i1.5580
ORIGINAL ARTICLE
Agreement between Finometer and Firstbeat
on heart rate variability data in women: a pilot study
Concordância entre Finometer e Firstbeat na variabilidade da frequência cardíaca em mulheres: um estudo piloto
Lucas Rangel Affonso de
Miranda, Carlos Brendo Ferreira Reis, Thales Couto Bergantini,
Victor Hugo Gasparini Neto, Luciana Carletti, Richard Diego Leite
Universidade Federal do
Espírito Santo (UFES), Vitória, ES, Brazil
Received: December 18,
2023; Accepted: January 17,
2024.
Correspondence: Lucas Rangel Affonso de Miranda, lucasram14@gmail.com
How to
cite
Miranda LRA, Reis
CBF, Bergantini TC, Gasparini Neto VH, Carletti L,
Leite RD. Concordance between
Finometer and Firstbeat on heart
rate variability data in women:
a pilot study. Rev Bras Fisiol
Exerc. 2024;23:e235580. doi:
10.33233/rbfex.v23i1.5580
Abstract
Aim: To analyze the agreement
of the Firstbeat
real-time heart rate monitor in comparison
to an ECG in women. Methods: 7 physically active women were recruited
to realize two recordings of RR intervals on two
days separated by 7 days. The recordings were conducted with the volunteers seated on the
Leg Press 45 apparatus. For
the recording of the RR intervals,
a three-lead electrocardiogram
(ECG) recording, coupled to the Finometer,
and the Firstbeat
real-time monitor were used.
Statistical analysis was performed using
SPSS software (26.0). Results: There was no significant
difference on both days (p > 0.05) in the paired T-test.
On day 1, a perfect correlation was found in the
Pearson correlation test (r
= 1.0), and on day 2, a very strong
correlation was observed (r = 0.99). Additionally,
no proportional bias was identified in the Bland-Altman test. The mean of the RR intervals
was consistent between the Finometer
ECG and the Firstbeat monitor in women.
Keywords: electrocardiography;
heart rate determination; autonomic nervous system.
Resumo
Objetivo: Analisar a concordância do monitor
cardíaco em tempo real da Firstbeat em relação a um
ECG em mulheres. Métodos: 7 mulheres fisicamente ativas foram recrutadas
para realizar dois registros dos intervalos RR em dois dias separados por 7
dias. Os registros foram realizados com as voluntárias sentadas no aparelho Leg Press 45. Para o registro dos intervalos RR, foi
realizado um registro eletrocardiográfico (ECG) de três derivações, acoplado ao
Finometer, e o monitor em tempo real da Firstbeat. A análise estatística foi realizada através do
software SPSS (26.0). Resultados: Não houve diferença significativa em
ambos os dias (p > 0,05) no teste T pareado. No dia 1, foi verificada
correlação perfeita no teste de correlação de Pearson (r = 1,0), e no dia 2,
foi observada correlação muito forte (r = 0,99). Além disso, não foi
identificado viés de proporção no teste de Bland-Altman.
A média dos intervalos RR foi concordante entre o ECG do Finometer
e o monitor Firstbeat em mulheres.
Palavras-chave: eletrocardiografia; determinação da
frequência cardíaca; sistema nervoso autônomo.
Introduction
Heart
rate variability (HRV) is a
non-invasive measure that reflects oscillations
in the autonomic nervous system [1]. Higher resting HRV values are related to better
cardiovascular reflexes and cardiovascular health. Lower HRV values are related to reduce
vagal control, slower
cardiovascular reflexes, and a higher
inclination toward
cardiovascular health risks.
HRV analysis utilizes indices
obtained from beat-to-beat intervals (iRR) [1,2]. These intervals can be
measured through ECG, cardiac monitor, and other equipment [1,2]. RR intervals represent the time between each R wave of
the ECG, i.e., the interval between each heartbeat. In this sense, shorter
RR intervals indicate a higher heart rate (HR), while longer RR intervals signify a lower HR [1].
Although easily accessible, the ECG is considered the
standard method for measuring
the intervals between heartbeats and, consequently, for analyzing HRV. However, despite its consolidation in the literature, the ECG is associated
with a high cost and limited mobility
[3].
Thus, alternative equipment is needed
that is more accessible and validated in the literature. In this context, equipment for recording iRR, which allows testing
outside the laboratory, has been validated. Studies [4,5,6,7,8] examining HR and HRV suggest the potential use of HR monitors or smartwatches at rest [6], for 24 hours [5], during exercise [4,7], and during recovery
after exercise [8]. However, Firstbeat's real-time
display (RTM) in conjunction with
the Elite HRV app has been an unvalidated
alternative until now.
Furthermore, women are significantly underrepresented in
all newspaper surveys, with their
participation being between 35% and 37% of surveys [9]. Notably, when comparing
the HRV of men and women,
men exhibit higher sympathetic activity in HRV compared to women [10].
In this study, the
aimed was to assess HRV agreement
between the 3-lead ECG of the Finometer
(Finapres Medical System, BV Netherlands) and real-time monitor by Firstbeat in young women.
Methods
Sample
This is a cross-sectional study involving a sample of seven physically active women. Participants
were informed about the study
procedures, importance, relevance,
and duration. All participants read and signed
the informed consent form. The short version of the IPAQ questionnaire
was used to characterize the level of
physical activity. Inclusion criteria required volunteers to be physically
active, without
cardiovascular or metabolic
disease, and available for research meetings. Exclusion criteria included the ingestion
of beverages or food that could
negatively or positively affect HRV, as well as any type
of physical exercise.
The
procedures conducted in this
study adhered to resolution 466/12 of the National
Health Council, as approved
by the Human
Research Ethics Committee of the
Federal University of
Espírito Santo (n. 90076218.0.0000.5542/2018).
Data collection
The study was conducted
at the Center for Research and Extension
in Body Movement Sciences of
the Physical Education and Sports Center
(CEFD) at the Universidade
Federal do Espírito Santo (UFES).
The first session with
the volunteers involved anamnesis, signing of the
informed consent form, IPAQ questionnaire, and familiarization with the equipment
where the iRR was collected.
In the second meeting, after arriving at the laboratory,
the participants were instructed to sit and
rest on the
bench of the Leg Press 45 device (with 90 degrees of hip flexion and 90 degrees of knee flexion)
for at least 10 minutes, maintaining an ambient temperature of 21°C. After the rest period,
volunteers remained in the Leg Press device, and the iRR
was recorded for 10 minutes
using the Finometer ECG and the Firstbeat real-time monitor. During the third
session, we replicated the procedures conducted in the second session (Figure 1).
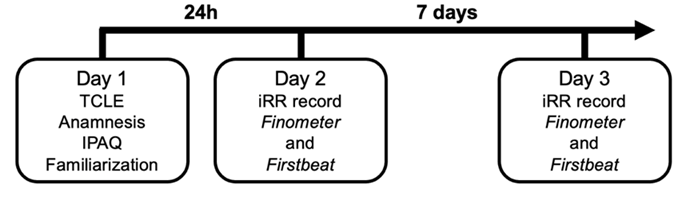
Figure 1 - Study
design
The iRR was recorded
on the Leg
Press device due to exercise performance following collection. The present study aimed to
verify the agreement between equipment for HRV analysis. Another study focused
on analyzing the effects of
exercise performing [11].
The acquisition of iRR through the
Finometer ECG adhered to the three-lead
configuration, following the Einthoven triangle.
The three electrodes were positioned in accordance with the manufacturer's guidelines (Finapres Medical
System, BV Netherlands) [12]. The ground electrode was placed
on the right
side of the
volunteer's thorax, near the sternum,
while the positive electrode was positioned
on the left
side of the
thorax, at the level of
the fifth intercostal space. Additionally, a second positive electrode was placed on
the right side of the
thorax, below the nipple, in the V5 position (Figure 2) [11].
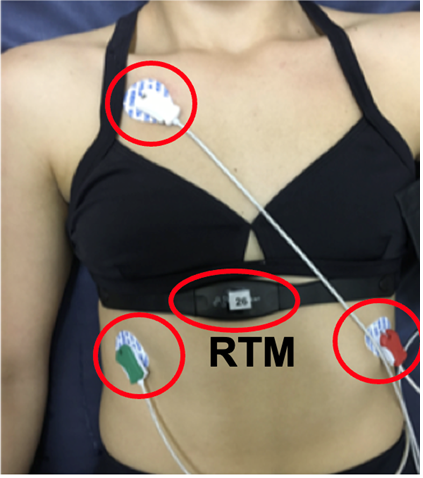
Source: [11]
Figure 2 - Positioning
of the Finometer
electrodes and Firstbeat RTM
At the same time, the iRR was
recorded using the Firstbeat MTR positioned towards the xiphoid process,
connected via Bluetooth to
a mobile device. For iRR recording,
the BeatScope software
(Ontario, Canada) was employed
for the Finometer, and the Elite HRV app was utilized for the Firstbeat MTR data.
Data analysis
The ECG
data was transferred from the computer
using a mobile storage
device, while the Elite HRV
files were transferred via
a USB cable. The analysis of the iRR
was conducted using the Kubios
HRV Standard® software, which calculated
the average of the intervals
in milliseconds.
After computing the mean iRR,
normality was assessed using the Shapiro-Wilk test. After confirming the normal distribution of the data, a paired T-test was used
for mean comparisons.
Pearson correlation coefficients
were interpreted as
follows: 0 = none; 0.1-0.3 = weak;
0.4-0.6 = moderate; 0.7-0.9 = strong;
1 = perfect [13]. Futhermore, linear regression and Bland-Altman plots were conducted
to evaluate the correlation and concordance of HRV data.
In the Bland-Altman analysis, the horizontal and central line represents the mean of the
difference between the instrument measurements. The upper and lower limit
lines represent the 95% confidence intervals (mean of the differences
± 1.96 x standard deviation of
the differences). Excel was used as a database
and IBM SPSS Statistics
26.0 was used for data analysis.
Results
The research participants were aged 24.6 ± 3.8 years, body mass of 60.3 ± 6.9 kg, height of 1.64 ± 0.09 m, and a body mass index of 22.3 ± 0.9 kg/m2.
On both days, there were
no significant differences
in mean iRR scores between the instruments
used (Day 1: p = 0.715; and
Day 2: p = 0.178). On day
1, a perfect correlation was identified (r = 1), while on day
2, a very strong correlation was observed (r = 0.994). Morever, no
proportion bias was detected in the linear regression test on day 1 (p = 0.6) and day 2 (p = 0.942) using the Bland-Altman
analysis (Figure 3 and 4).
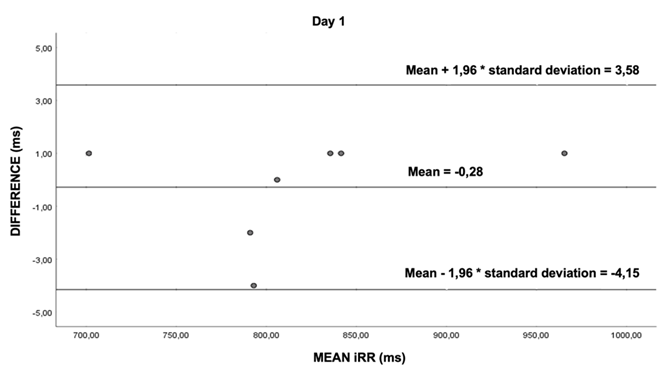
Figure 3 - Bland-Altman
analysis day 1. Each data point in the graph represents the difference between the mean
RR intervals of the Finometer and
the Firstbeat real-time
monitor (in milliseconds)
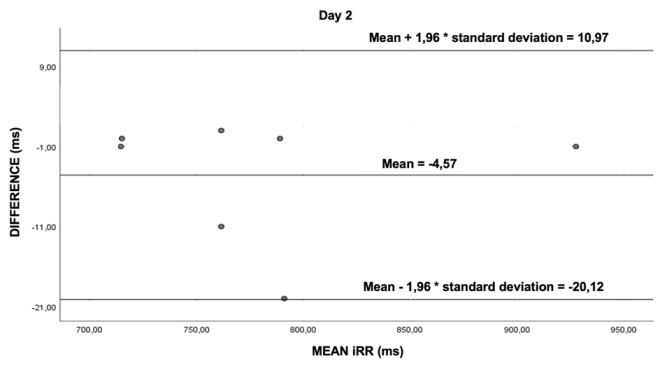
Figure 4 - Bland-Altman
analysis day 2. Each data point in the graph represents the difference between the mean
RR intervals of the Finometer and
the Firstbeat real-time
monitor (in milliseconds)
Discussion
This study aimed to analyze
the HRV concordance between the Finometer
ECG and the Firstbeat MTR. The primary finding of the
study was that the Firstbeat
MTR demonstrated concordant
measurements of RR intervals when compared to the
gold standard (ECG). Therefore,
the Firstbeat MTR can serve as a reliable tool for collecting iRR both at rest
within laboratories and in non-laboratory settings.
To the best of our
knowledge, the present study is
the first to compare the agreement between the Firstbeat MTR with the ECG. However,
previous studies have already validated
other equipment for heart rate and HRV collection and analysis. Nunan et al. [7]
assessed the validity of resting
HRV measurements using the Polar S810 compared to the 12-lead ECG on three different
days, with a 1-week interval between days. The Polar S810 showed a
high correlation (0.85 - 0.99) with
the ECG. In this sense, the Polar S810 appears to exhibit
an agreement with the gold
standard similar to the result found for Firstbeat's MTR.
In addition to heart
monitors, Nelson et al. [8] examined the accuracy
of the HR measurement from the Apple Watch 3 and Fitbit Charge 2 smartwatches during five daily activities
(sitting, walking, running,
activities of daily living, and sleeping) compared to 24-hour ambulatory ECG. This study found
high accuracy in the
24-hour condition for both
devices, with an average difference of -1.8 beats per minute (bpm) for the
Apple Watch 3 and -3.47 bpm
for the Fitbit Charge 2 compared to the
gold standard. Similarly, our study revealed
comparable results when comparing mean RR intervals to the gold
standard, showing -0.28 on day 1 and 4.57 on day 2.
In addition to the
tools for acquiring RR intervals,
the present study utilized the Elite HRV application on a smartphone for recording. This app was previously
validated for supine resting
and orthostatic challenge in a study by Gambassi et al. [4], where it compared recording made through the Elite HRV app connected to the
Polar H7 transmitter with the 3-lead ECG. This validation supports the use of the
Polar H7 app and transmitter,
at least for measurements in the supine
position or during orthostatic challenges. In this study, demonstrated
an almost perfect correlation of r = 0.99 in the supine
position. In our study, a perfect correlation was observed on
day 1 (r = 1), and a very strong correlation
was found on day 2 (r = 0.99).
However, Horton et al. [12] have demonstrated that variations in exercise intensities can impact the
accuracy of heart monitors. Furthermore, concordance between ECG and other devices may fluctuate based on equipment calibration,
software updates, and measurement
conditions. A limitation of this study
includes the modest sample size, measurements performed only in women, and assessments carried out only in a resting condition. Additionally, the data in this study are constrained by the inability to
compare with studies conducted in sitting or supine positions, as well as during exercise.
Nevertheless, the study is advantageous
as it establishes that, in
a state of preparation for a physical exercise protocol, involving heightened alertness, Firstbeat's RTM showed agreement with the gold
standard method (ECG). This
demonstrates the method’s feasibility for applications in studies requiring pre-exercise HRV measurements.
We also highlight the significance
of validating the measurements from various heart
monitors and smartwatches compared to the gold
standard in diverse conditions
(rest and exercise). Addittionally, we examined the
consistency across various exercise intensities, encompassing both aerobic and
resistance exercise, and in male individuals.
Conclusion
The mean RR intervals exhibited concordance between the Finometer
3-lead ECG and the Firstbeat real-time monitor in women.
These findings provide opportunities for the utilization Firstbeat in studies where portability plays a crucial
role in facilitating HRV recording
at rest, especially in women.
Acknowledgement
We would
like to express our gratitude to
Professor MsC Andre Berzoti for providing the equipment and
offering invaluable assistance during its use.
Academic affiliation
This article
represents part of the scientific
initiation study of Lucas Rangel Affonso de Miranda.
Conflict of
interest
No known financial conflicts of interest or
personal relationships that
might have influenced the work reported in this article exist.
Financing
This research
is self-funded. The author of the
research had a Scientific Initiation scholarship from the Federal University of Espírito Santo.
Authors' contributions
Conception and
design of the research: Miranda LRA, Reis CBF, Leite RD; Data collection: Miranda LRA, Reis CBF, Bergatini
TC, Gasparini-Neto VH; Data analysis and interpretation: Miranda
LRA, Reis CBF, Gasparini-Neto VH; Statistical
analysis; Miranda LRA, Reis CBF, Gasparini-Neto
VH; Writing of the manuscript: Miranda LRA,
Reis CBF, Bergatini TC, Carletti L, Leite RD; Critical revision of the manuscript
for important intellectual content: Miranda LRA, Reis CBF, Bergatini
TC, Ribeiro ALB, Gasparini-Neto VH, Carletti L, Leite RD.
References
- Carlos L, Vanderlei M, Pastre CM, Hoshi RA, Carvalho TD,
Fernandes De Godoy MF. Basic notions of heart rate variability
and its clinical applicability. vol. 24. 2009. Rev
Bras Cir Cardiovasc. 2009;24(2):205-17. doi: 10.1590/s0102-76382009000200018 [Crossref]
- Guidelines. Guidelines Heart rate variability. Eur Heart J. 1996;17:354–81. doi: 10.1161/01.CIR.93.5.1043 [Crossref]
- Pernice R, Javorka M, Krohova J, Czippelova B, Turianikova Z, Busacca A, et al. Reliability of short-term heart rate variability indexes assessed through photoplethysmography. 2018 40th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Honolulu, HI, USA;2018:5610–5513. doi: 10.1109/EMBC.2018.8513634 [Crossref]
- Boudreaux BD, Hebert EP, Hollander DB, Williams BM, Cormier CL, Naquin MR, et al. Validity of wearable activity monitors during cycling and resistance exercise. Med Sci Sports Exerc. 2018;50:624–33. doi: 10.1249/MSS.0000000000001471 [Crossref]
- Nelson BW, Allen NB. Accuracy of consumer wearable heart rate measurement during an ecologically valid 24-hour period: intraindividual validation study. JMIR Mhealth Uhealth. 2019;7:e10828. doi: 10.2196/10828 [Crossref]
- Nunan D, Donovan G, Jakovljevic DG, Hodges LD, Sandercock GRH, Brodie DA. Validity and reliability of short-term heart-rate variability from the polar S810. Med Sci Sports Exerc. 2009;41:243–50. doi: 10.1249/MSS.0b013e318184a4b1 [Crossref]
- Gillinov S, Etiwy M,
Wang R, Blackburn G, Phelan D, Gillinov
AM, et al. Variable accuracy of
wearable heart rate monitors during aerobic exercise. Med Sci Sports Exerc. 2017;49:1697–703. doi: 10.1249/MSS.0000000000001284 [Crossref]
- Tsitoglou KI, Koutedakis Y, Dinas PC. Validation of the Polar RS800CX for assessing heart rate variability during rest, moderate cycling and post-exercise recovery. F1000Res 2018;7:1501. doi: 10.12688/f1000research.16130.1 [Crossref]
- Costello JT, Bieuzen F, Bleakley CM. Where are all the female participants in Sports and Exercise Medicine research? Eur J Sport Sci 2014;14:847–51. doi: 10.1080/17461391.2014.911354 [Crossref]
- Geovanini GR, Vasques ER, de Oliveira Alvim R, Mill JG, Andreão RV, Vasques BK, et al. Age and sex differences in heart rate variability and vagal specific patterns – Baependi Heart Study. Glob Heart. 2020;15. doi: 10.5334/GH.873 [Crossref]
- Reis C. Efeito agudo de dois
protocolos isométricos equalizados na relação esforço:pausa
(work-to-rest ratio):
respostas hemodinâmicas e autonômicas [Dissertação]. Vitoria: Universidade
Federal do Espirito Santo; 2020
- Gambassi BB, Neves VR, Zeus E, Brito A, Sobral
D, Fernandes S, et al. A validation study of a smartphone application for heart rate variability assessment in asymptomatic
adults. Am J Cardiovasc Dis. 2020;10(3):219-29. Available
from:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7486523/
- Akoglu H. User’s guide to correlation coefficients. Turk J Emerg Med. 2018;18:91–3. doi: 10.1016/j.tjem.2018.08.001 [Crossref]