Rev Bras Fisiol Exerc. 2024;23:e235584
doi: 10.33233/rbfex.v23i1.5584
ORIGINAL ARTICLE
Effect of isometric contraction duration on hemodynamic
responses in hypertensive women
Efeito da duração da
contração isométrica nas respostas hemodinâmicas de mulheres hipertensas
Leudyenne Pacheco de Abreu1,2, Carlos
Brendo Ferreira Reis2, Thiago Gomes Leite1, Cristiano
Teixeira Mostarda1, Richard Diego Leite2, Mário Alves de
Siqueira-Filho1
1Universidade Federal do Maranhão (UFMA),
São Luís, MA, Brazil
2Universidade Federal do Espírito Santo
(UFES), Vitória, ES, Brazil
Received: November 10,
2023; Accepted: January 25,
2024.
Correspondence: Leudyenne
Pacheco de Abreu, leudyennepacheco@gmail.com
How to
cite
Abreu LP, Reis CBF,
Leite TG, Mostarda CT, Leite RD, Siqueira-Filho MA. Effect
of isometric contraction duration on hemodynamic responses in hypertensive women. Rev Bras Fisiol
Exerc 2024;23:e235584. doi:
10.33233/rbfex.v23i1.5584
Abstract
Introduction: Isometric exercise (IE) is one of the
non-pharmacological strategies
for reducing post-exercise blood pressure measurements. Objective: To compare the acute effect of
two protocols with different configurations of isometric exercise prescription on hemodynamic parameters in hypertensive women. Methods: Ten hypertensive women performed 2 sessions of IE at 30% of
1RM on the horizontal bench press with
a guided bar. The protocols
were: 4 sets of 2 minutes of isometric contraction
with 2 minutes of rest (4x2x2); and 16 sets of 30 seconds of
isometric contraction with 24 seconds of rest (16x30x24), with a 7-day interval between sessions. Blood pressure was measured using
a digital sphygmomanometer, pre-exercise,
immediately after exercise, and during
the 60-minute recovery period. Results: Both protocols showed an increase in heart rate and double product (4x2x2, p = 0.002 and p < 0.001; 16x30x24, p = 0.001 and
p = 0.002, respectively). Protocol
4x2x2 increased systolic blood pressure and mean arterial pressure (p = 0.014 and p =
0.034, respectively), while
16x30x24 increased pulse pressure
(p < 0.001) compared to rest immediately after exercise. Normalization of the evaluated values
was observed from 10 minutes of recovery in both protocols. There was no interaction effect between the protocols. Conclusion: Isometric exercise for the upper limbs with
different configurations
(4x2x2 and 16x30x24), when equalized by work-to-rest
ratio, promotes similar acute hemodynamic responses in controlled hypertensive women.
Keywords: isometric exercise; blood pressure; hypertension.
Resumo
Introdução: O exercício isométrico (EI) constitui
uma das estratégias não farmacológicas para redução de medidas da pressão
arterial após o exercício. Objetivo: Comparar o efeito agudo de dois
protocolos com diferentes configurações de prescrição do exercício isométrico
sobre parâmetros hemodinâmicos de mulheres hipertensas. Métodos: 10
mulheres hipertensas realizaram 2 sessões de EI a 30% de 1RM no aparelho supino
horizontal com barra guiada. Os protocolos foram: 4 séries de 2 minutos de
contração isométrica com 2 minutos de descanso (4x2x2); e 16 séries de 30
segundos de contração isométrica com 24 segundos de descanso (16x30x24), com 7
dias de intervalo entre as sessões. A pressão arterial foi medida por
esfigmomanômetro digital, pré, imediatamente após o
exercício e durante os 60 minutos de recuperação. Resultados: Ambos os
protocolos apresentaram elevação dos valores de frequência cardíaca e duplo
produto (4x2x2, p = 0,002 e p < 0,001; 16x30x24, p = 0,001 e p = 0,002,
respectivamente), o protocolo 4x2x2 aumentou a pressão arterial sistólica e a
pressão arterial média (p = 0,014 e p = 0,034, respectivamente), e o 16x30x24
aumentou a pressão de pulso (p < 0,001), quando comparado o repouso com o
momento imediatamente após o exercício. A normalização dos valores avaliados
foi observada a partir dos 10 min de recuperação em ambos os protocolos. Não
houve efeito de interação entre os protocolos. Conclusão: O exercício
isométrico para membros superiores com diferentes configurações (4x2x2 e
16x30x24), quando equalizados pela relação esforço:pausa,
promove respostas hemodinâmicas agudas semelhantes em mulheres hipertensas
controladas.
Palavras-chave: exercício isométrico; pressão
arterial; hipertensão.
Introduction
Systemic Arterial Hypertension
(SAH) is characterized by a persistent elevation of blood
pressure (BP) at rest [1], with values above 130 mmHg of systolic blood
pressure (SBP) and 80 mmHg of diastolic blood
pressure (DBP) [2]. Hence,
SAH is recognized as one of the
most prevalent chronic non-communicable diseases, developing progressively due to the stiffening
of blood vessels [3]. It is also regarded as a significant risk factor for coronary heart disease and
stroke, contributing significantly to the high global mortality rate associated with cardiovascular diseases [4].
In women, the incidence
of SAH increases [5] after menopause due to a gradual reduction in circulating levels of sex hormones
(estrogen and progesterone) [6]. This reduction and a gradual increase in adiposity lead to elevated circulating
pro-inflammatory markers, and these markers
contribute to the onset and
worsening of insulin resistance, renin-angiotensin system alterations,
sympathetic nervous system hyperactivity, and endothelial dysfunction [6,7]. Moreover, persistent elevations in BP have been increasingly associated with cardiovascular autonomic dysfunction. The autonomic nervous system (ANS) regulates sympathetic modulation of the
myocardium and parasympathetic modulation of the sinus
node, atrioventricular node, and atrial myocardium [8]. Interventions are
needed to assist this demographic
in mitigating the impact of multiple
hypertension risk factors, leading to a consequent reduction in the health complications associated with this condition. While SAH is multifactorial,
it often correlates with environmental factors such as diet, physical
inactivity, and alcohol intake [2,4].
Regarding the impact of physical
activity, the effects of exercise
on controlling and regulating hypertension have been well-documented since the 1960s [9]. However, recent studies have linked
isometric exercise (IE) with enhanced BP control in individuals with hypertension [1,10]. These exercises are characterized by their simplicity and versatility, allowing for effortless
performance with low resistance and different prescription configurations (number of sets, contraction duration, and rest
intervals). Importantly, they maintain consistent
joint angles and typically result in minimal or no changes
to muscle length [1]. These attributes highlight IE as a methodological training alternative
and an accessible
strategy for treating hypertension [10,11,12].
Some effects of IE on
BP have already been established [1,11,12,13,14]. A commonly used configuration
in studies focusing on hypertension treatment involves four sets of 2-minute isometric contractions at 30% of maximum voluntary
force [15]. However, there is limited research
on the various
prescription configurations
of IE and their effects on
controlling SAH and its application alongside commonly practiced gym exercises. Studies analyzing BP responses to different configurations
of these exercises have predominantly involved normotensive individuals [16,17,18,19].
It is conceivable that altering the
configuration of these exercises by manipulating variables such as the duration of
IE could affect one or more training responses. Understanding these effects can aid
practitioners in selecting
a protocol that aligns with their
preferences and goals.
This study aimed to compare the acute effect
of two protocols
with different IE prescription configurations on hemodynamic parameters in hypertensive women. To do this,
we sought to test the
hypothesis that exercise with a short duration of isometric
contraction can promote similar hemodynamic
responses to that performed with a long duration when
equalized by the work-to-rest ratio.
Methods
Participants
The study is a cross-sectional,
quasi-experimental study comprising ten hypertensive women undergoing regular drug treatment for this condition (Table I) with medical clearance to engage in exercise.
This study's
target population was participants in a multidisciplinary
institutional program for people aged 55 and over, which was aimed at
the community living around the university.
The sample was selected based on convenience,
and all volunteers
received prior information about the study's
aims and detailed explanations of the procedures involved. Subsequently, they provided informed
consent by signing the consent
form.
The
procedures in this study adhered to the
guidelines outlined in Resolution No. 466/12 of the National Health Council of the
Ministry of Health. They were conducted only after obtaining
approval from the Research Ethics
Committee of the Federal University of Maranhão (UFMA) (No.43181015.6.0000.5087).
Experimental design
The study was conducted
at the Strength
Physiology Laboratory of the UFMA Sports Center, where the selected
volunteers were already participating in other ongoing programs.
The
procedures were conducted
over eight sessions on different days,
following this sequence: Session 1 - Introduction of the project, collection
of informed consent signatures, medical history review, and completion of the
IPAQ (International et al.) [20] and PAR-Q (Physical Activity Readiness Questionnaire); Session 2 - Anthropometric and body composition assessments, BP and heart rate (HR) measurements; Sessions 3 and 4 - Familiarization sessions on the horizontal bench press exercise;
Sessions 5 and 6 - Test and retest to
determine maximum voluntary
strength, using the 1-repetition maximum (1RM) test, separated by a 48-hour interval; Sessions 7 and 8 - Implementation of the selected exercise
protocol for the respective days, 48 hours after the 1RM test
and retest. The second protocol was performed seven
days later.
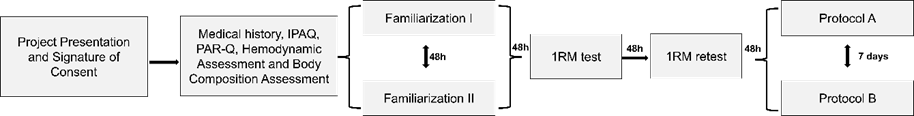
Figure 1 - Experimental study
design
Body assessment
Height was measured using a portable stadiometer (Sanny®,
model ES2060, São Paulo, Brazil) and
body mass using a digital scale (Omron®, model HN-289, Omron Co., Osaka, Japan). Hip, waist, and abdominal circumference measurements were taken using
an anthropometric tape measure (Sanny®, model TR-410, São Paulo, Brazil).
Tetrapolar
electrical bioimpedance
(MALTRON®, model Bf-906, United Kingdom) was employed to assess
body composition. Participants
were instructed to adhere to
the preparation recommendations according to Heyward and
Stolarczyk [21].
Familiarization and
assessment of maximum voluntary strength
The familiarization sessions were conducted over two sessions, separated
by 48 hours. Participants performed the horizontal bench press exercise
during each session using a guided bar (Smith et al. G1-FW161, Matrix Fitness,
United States).
Three sets of 15 repetitions were performed, with a 1-minute rest interval between
sets. The initial load was set as the absolute weight of the bar, and
progressions of 3 to 5% were determined
based on the OMNI-RES scale for rate-perceived effort [22].
The 1-RM test was adapted
following the Baechle and Earle
protocol [23]. Initially, a
warm-up consisting of 10 repetitions was performed using
the load from the familiarization
phase. After a 1-minute rest interval, the 1RM test began.
Participants were allowed up to
5 attempts to determine their maximum load,
with a 3 to 5-minute rest period between
each attempt. The OMNI-RES scale [24] was used as a parameter to increase the
loads after each attempt. Participants
were instructed to remain in the
room and refrain from consuming
food during the protocol. After 48 hours, the same procedures were repeated (retesting) to confirm
the maximum loads obtained.
Hemodynamic parameters
Upon arrival at the laboratory,
volunteers were instructed to remain
seated and refrain from exertion
for 10 minutes before resting.
BP and HR measurements were taken. For our analysis, BP and HR values were
obtained at rest, immediately after IE protocol, and during the
following 60 minutes of recovery, with 10-minute intervals between each measurement (10min, 20min,
30min, 40min, 50min, and 60min). To
obtain these measurements, an automatic pressure device was used (OMRON®, model HEM-742®,
OMRON Corp., São Paulo, Brazil).
Pulse pressure (PP) was calculated as the difference between SBP and diastolic blood
pressure (DBP) [25].
Experimental procedure
This study involved two sessions
of IE on the horizontal bench press, utilizing a guided bar, with one protocol employed
per session. Before the first session, a random draw was
conducted to determine the order in which
each participant would undergo the
protocols. The interventions
consisted of the 4x2x2 protocol (comprising long-duration isometric contractions), involving four sets of 2 minutes of isometric contraction
with 2-minute rest intervals, and the 16x30x24 protocol (comprising short-duration isometric contractions), involving 16 sets of 30 seconds of isometric
contraction with 24-second rest intervals. The protocols were executed at an
intensity of 30% of 1RM, maintaining a 90º angle of elbow
flexion, as controlled by a goniometer (Carci®, São Paulo, Brazil). Moreover, the protocols
were equalized using the work-to-rest
ratio proposed by Paulo et al. [26]. The work-to-rest
ratio values were determined using the following
calculations: (I) total time of
muscle tension/total Rest (480s:360s = 1.33), and (II)
total sustained weight/total
rest (480s*0.3:360s = 0.4). A seven-day
interval was observed between the two exercise
sessions.
Statistical analysis
Normality was analyzed using the Shapiro-Wilk test, and the results
were presented as the standard deviation of the Mean
(M±SDM). The two-way ANOVA analysis
of variance for repeated measures was used to
analyze possible effects of the
time factor (Rest, immediately after exercise, and recovery
at 10min, 20min, 30min, 40min, 50min, and 60min), the protocol factor (4x2x2; 16x30x24)
and to detect
possible effects of interactions between the factors,
followed by the Bonferroni post hoc test. The
analyses respected the assumption of sphericity assessed
by the Mauchly
test, and the Greenhouse-Geisser correction applied when necessary. A significance level of p ≤ 0.05 was adopted. The intraclass correlation test (ICC) was used to
analyze the reproducibility of the 1RM test. The data was tabulated in the Office Excel program (Microsoft®, version
2016) and analyzed using SPSS® 25.0 (SPSS, Inc., Chicago).
Results
The study participants exhibited average BP levels indicative of well-controlled hypertension despite being overweight, as evidenced by their
average BMI (Table I). Regarding the loads
employed during the protocols, the intraclass correlation coefficient (ICC) indicated good reliability between the values obtained
in the 1-RM test and retest (ICC = [95% CI = 0.298
- 0.929]; F(9,9) = 7.127; p = 0.004) [27].
Table I - Characteristics of the hypertensive
women (N = 10)
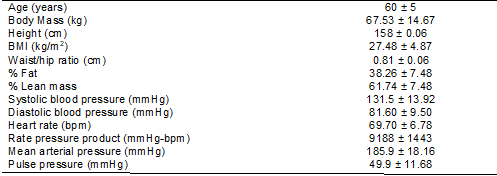
Data are presented as average and standard deviation of the Mean
(M±SDM). kg = kilogram, cm = centimeters,
BMI = body mass index, bpm = beats per minute, m² = square meter, % = percentage
In
response to the IE protocols, it was possible to observe an effect of
the time factor on SBP measurements [F(5%. 7.00) = 12.44; p < 0.001]. In the
4x2x2 protocol, the immediate after-measurement was significantly higher than the
rest (p=0.014). During recovery, there was a decline in SBP at 10min,
20min, 30min, and 50min, compared
to immediately after (p = 0.015; p < 0.001; p = 0.001, and p=0.004, respectively). In the 16x30x24 protocol, Bonferroni post-hoc analysis revealed reductions in SBP in recovery at 10min, 20min, and 60min, compared to immediately after (p = 0.006; p = 0.049; and
p = 0.024, respectively) (Table
II).
There was no influence of the
factors time [F(5%. 7.00) =
1.80; p = 0.101], protocol [F(5%.
1.00) = 0.36; p = 0.563], or interaction
effects between the factors [F(5%.
7.00) = 0.98; p = 0.453] on DBP (Table
II).
We also observed an effect
of time on HR [F(5%. 2.19) = 59.87; p < 0.001]. In each
protocol (4x2x2 or
16x30x24), HR was higher immediately after exercise compared to rest (p = 0.002 and p = 0.001, respectively), and all recovery
measurements showed a reduction when compared to immediately
after in both protocols (p ≤ 0.001 for all
moments) (Table II).
The mean arterial pressure (MAP)
response was influenced by the time factor
[F(5%. 7.00) = 7.99; p < 0.001]. In the 4x2x2 protocol, MAP increased significantly immediately after compared to rest
(p = 0.035). During recovery,
this measurement was lower at
10min, 20min, 30min, and 50min, compared
to immediately after IE (p = 0.003; p < 0.001; p < 0.001; p = 0.013,
respectively). On the other hand,
in the 16x30x24 protocol, the only change
observed was a reduction in MAP 10 minutes after
recovery, compared to immediately after (p = 0.048) (Table II).
PP was also influenced
by the time factor [F(5%. 7.00) = 18.16; p
< 0.001]. In the 4x2x2 protocol,
there was only a reduction in PP at 50 minutes during recovery, compared to the immediately
after (p = 0.030). Conversely,
in the 16x30x24 protocol,
PP was higher immediately after exercise than rest
(p < 0.001). Additionally, PP was
lower in all recovery measurements than immediately after (p = 0.001; p = 0.003; p = 0.013; p = 0.011, p =
0.007; and p = 0.001, respectively)
(Table II).
When analyzing rate pressure product (RPP), we also observed an
effect of the time factor [F(5%. 2.39) = 64.99; p < 0.001]. In the
4x2x2 protocol, there was an increase
in RPP immediately after exercise compared to Rest (p < 0.001). During recovery, all measurements were significantly lower than immediately
after (p < 0.001 for all
moments).
Table II - Hemodynamic
responses to horizontal supine isometric
exercise in hypertensive women
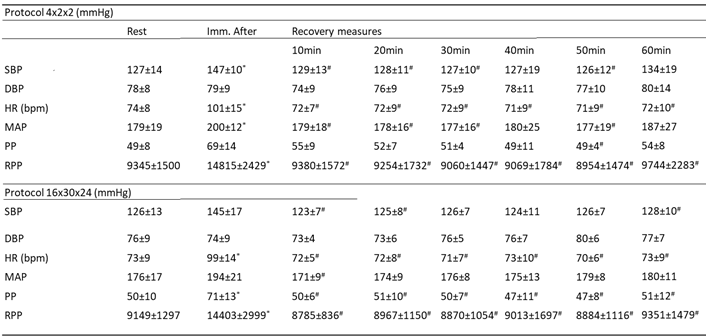
The data are
presented as Mean±Standard Deviation of the
Mean (M±SDM); Imm. After = Immediately after; *represents the difference compared to the
Rest; # represents the difference compared to immediately
after. Fonte: The Authors
Similarly, after performing the 16x30x24 protocol, RPP increased immediately after compared to rest
(p = 0.002). Furthermore, there
was a significant reduction in RPP at all recovery times compared to immediately
after (p = 0.001; p = 0.001; p = 0.002; p = 0.004, p
= 0.002; and p = 0.003, respectively)
(Table II).
In this study, we
observed no differences in hemodynamic parameters when comparing the responses between the protocols utilized
(p ≥ 0.05).
Discussion
This study aimed to compare the acute effect
of two protocols
with different isometric contraction durations on hemodynamic
parameters in hypertensive women. Our main
findings show that exercises performed on the horizontal bench press with
different durations of isometric contraction
but with an equated work-to-rest
ratio promote hemodynamic responses of similar
magnitude in women with controlled hypertension.
In our study, we
observed that there was no difference
in the hemodynamic behavior when analyzing
the measures of SBP, DBP, MAP, HR, PP, and RPP
among the protocols. Considering the individual analysis, in the 4x2x2 protocol, characterized by prolonged isometric muscle contraction, there was a significant
decrease in SBP and MAP between the ten
and 30-minute intervals during the recovery
period compared to the period
immediately after protocol. In the 16x30x24 protocol, characterized by short durations of isometric muscle
contraction, the same behavior was
in SBP for up to 20 minutes
and in MAP for 10 minutes.
In this sense, previous
studies comparing different types of prescriptions equalized by the
work-to-rest ratio have observed similar hemodynamic responses following
single sessions of IE
[17,18,19]. For instance, Mayo
et al. [19] did not
observe significant reductions
in BP after different protocols (5 sets of 8 repetitions with a 3min interval; 10 sets of 4 repetitions with an 80sec interval; and 40 sets of 1 repetition with an 18.5sec interval; equalized at 40reps:720sec at 10-RM) in up to 40 minutes performed on the Leg
Press 45º. In another study,
Mayo et al. [18] did
not observe significant reductions in SBP and DBP in any of the
protocols (protocol with rest between
repetitions vs. protocol going to muscle
failure) compared to rest in different
exercises (bench press vs. free squat). Similarly, Río-Rodríguez,
Iglesias-Soler, & Olmo [17] also observed no hypotensive effect in the protocols
(protocol with rest between repetitions
vs. protocol going to muscle failure
in isometrics on the extension chair).
However, studies that did not
control the work-to-rest ratio showed that the
amount of muscle mass involved
and the total volume of training can determine whether a hypotensive response occurs [28]. One physiological mechanism that can explain
the influence of volume and exercise
involving large muscle groups is
the increase in vasodilator substances released from the
endothelial region induced by the
increase in blood flow post-exertion and the reduction
in peripheral vascular resistance
[29].
Furthermore, our study observed that immediately after the protocols,
SBP, MAP, HR, and RPP remained
significantly elevated compared to Rest,
regardless of the configuration. Conversely, Río-Rodríguez, Iglesias-Soler, and Olmo [17] observed that only HR remained
high compared to the resting value
in the protocol with the longest
time under tension (until failure), compared to the
protocol performed with rest between
repetitions, both performed in isometry on the leg
extension. Therefore, we posit that
the persistent increase in HR after an exercise session
is likely attributable to delayed vagal recovery in the heart, baroreflex
withdrawal, and potential cardiovascular overload
induced by exercise with a significant increase in RPP
[30,31]. Consequently, analyzing
sympathovagal balance would
be crucial to confirm this hypothesis,
necessitating further studies to deepen
our understanding. Nevertheless, considering that the observed
increase is transient, it does not preclude hypertensive individuals from participating in IE programs, from which they can
derive chronic hypotensive effects after at
least four weeks, potentially even greater in magnitude than those observed in dynamic strength or aerobic training [1].
Additionally, the 16x30x24
protocol exhibited the most significant
effect on PP change, as evidenced by the higher
values immediately after compared to rest and
about all measurements during the 60-minute recovery. Therefore, the pronounced increase in PP immediately following stress in this protocol may
be attributed to the short time interval allotted for recovery between sets. Given that this
condition might necessitate Valsalva maneuvers, the rise in arterial stiffness due to elevated
intrathoracic and abdominal
pressure could directly impact peripheral arteries and the aorta [32].
We recognize limitations in our study, such as the small sample size consisting solely of female
participants. Additionally,
BP measurements relied on an indirect
method, lacking 24-hour ambulatory monitoring for accuracy and protocol
assessment. Furthermore, the
study only examined one session
per protocol, focusing solely on upper
limb muscle groups.
Conclusion
When equalized by the
work-to-rest ratio, IE for the upper limbs
with different configurations (4x2x2 and
16x30x24) promotes similar acute
hemodynamic responses in controlled
hypertensive women.
As practical applications based on this
study, we propose that IE for the upper limbs
(bench press with the help of
a guided bar) with a longer or shorter
duration of muscle contraction (4x2x2 and 16x30x24) can be used to
help control BP levels in people with SAH, without any additional
cardio hemodynamic risk being observed.
In addition, the protocol with a shorter duration under isometric tension can serve as an alternative for people who use this type of
exercise but have complaints about the sensation
of effort caused by prolonged
isometric contractions, as both protocols promote equivalent hemodynamic responses. Although this condition still needs to be
tested, it can serve as a guide when choosing
between these protocols.
Academic affiliation
This article
represents the final coursework of Leudyenne
Pacheco de Abreu, supervised by
Professor Mário Alves de Siqueira-Filho at the Federal University of Maranhão.
Conflict of
interest
The authors declare that no known competing financial conflicts of interest
or personal relationships may have influenced
the work reported in this article.
Financing source
No funding/use of authors' resources.
Authors’ contribution
Conception and
design of the research: Abreu LP, Leite TG, Mostarda CT, Siqueira-Filho MA, Leite
RD; Data collection: Abreu LP, Leite TG,
Siqueira-Filho MA; Data analysis and interpretation: Abreu LP,
Reis CBF, Siqueira-Filho MA; Statistical analysis: Abreu LP, Reis CBF, Siqueira-Filho MA; Manuscript writing:
Abreu LP, Reis CBF, Siqueira-Filho MA; Critical
review of the manuscript for important intellectual content: Leite
RD, Siqueira-Filho MA.
References
- Carlson DJ, Dieberg G, Hess NC, Millar PJ, Smart
NA. Isometric exercise
training for blood pressure
management: A systematic review and
meta-analysis. Mayo Clin
Proc. 2014;89:327–34. doi: 10.1016/j.mayocp.2013.10.030 [Crossref]
- Pescatello LS, Buchner DM, Jakicic JM, Powell KE, Kraus WE, Bloodgood B, et al. Physical activity to prevent and treat hypertension: a systematic review. Med Sci Sports Exerc. 2019;51:1314–23. doi: 10.1249/MSS.0000000000001943 [Crossref]
- Hartog R, Bolignano D, Sijbrands E, Pucci G, Mattace-Raso F. Short-term vascular hemodynamic responses to isometric exercise in young adults and in the elderly. Clin Interv Aging. 2018;13:509–14. doi: 10.2147/CIA.S151984 [Crossref]
- Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Himmelfarb CD, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: Executive summary: A report of the American College of Cardiology/American Heart Association Task. 2018;71. doi: 10.1161/HYP.0000000000000066 [Crossref]
- Amiri M, Ramezani Tehrani F, Behboudi-Gandevani S, Bidhendi-Yarandi R, Carmina E. Risk of hypertension in women with polycystic ovary syndrome: A systematic review, meta-analysis and meta-regression. Reproductive Biology and Endocrinology. 2020;18:1–15. doi: 10.1186/s12958-020-00576-1 [Crossref]
- Leite RD, Prestes J, Pereira GB, Shiguemoto GE, Perez SEA, Deapartment PS, et al. Menopause: Highlighting the effects of resistance training 2010:761–7. Int J Sports Med. 2010;31:761-7. doi: 10.1055/s-0030-1263117 [Crossref]
- Chedraui P, Escobar GS, Ramírez C, Pérez-López FR, Hidalgo L, Mannella P, et al. Nitric oxide and pro-inflammatory cytokine serum levels in postmenopausal women with the metabolic syndrome. Gynecol Endocrinol. 2012;28:787–91. doi: 10.3109/09513590.2012.671395 [Crossref]
- Aubert AE, Seps B, Beckers F. Heart rate variability in athletes. Sports Med. 2003;33:889–919. doi: 10.2165/00007256-200333120-00003 [Crossref]
- Heller EM. Rehabilitation after myocardial infarction: practical experience with a graded exercise
program. Can Med Assoc J [cited 2023 jun 12]. 1967;97:22–7. Available from:
https://www.semanticscholar.org/paper/Rehabilitation-after-myocardial-infarction%3A-with-a-Heller/e6537f3fd8583577fba1fa4ed0fc26974020e038
- Smart NA, Way D, Carlson D, Millar P, McGowan C, Swaine I, et al. Effects of isometric resistance training on resting blood pressure: Individual participant data meta-Analysis. J Hypertens. 2019;37:1927–38. doi: 10.1097/HJH.0000000000002105 [Crossref]
- Cornelissen VA, Smart NA. Exercise training for blood pressure: a systematic review and meta-analysis. J Am Heart Assoc 2013;2:1–9. doi: 10.1161/JAHA.112.004473 [Crossref]
- Wiles JD, Goldring N, Coleman D. Home-based isometric exercise training induced reductions resting blood pressure. Eur J Appl Physiol 2017;117:83–93. doi: 10.1007/s00421-016-3501-0 [Crossref]
- Taylor AC, McCartney N, Kamath M V., Wiley RL. Isometric training lowers resting blood pressure and modulates autonomic control. Med Sci Sports Exerc. 2003;35:251–6. doi: 10.1249/01.MSS.0000048725.15026.B5 [Crossref]
- Smart NA, Gow J, Bleile B, Van der Touw T, Pearson MJ. An evidence-based analysis of managing hypertension with isometric resistance exercise—are the guidelines current? Hypertension Research 2020;43:249–54. doi: 10.1038/s41440-019-0360-1 [Crossref]
- Baffour-Awuah B, Pearson MJ, Dieberg G, Smart NA. Isometric resistance training to manage hypertension: systematic review and meta-analysis. Curr Hypertens Rep 2023;25:35–49. doi: 10.1007/S11906-023-01232-W [Crossref]
- Paulo AC, Tricoli V, Queiroz ACC, Laurentino G, Forjaz CLM. Blood pressure response during resistance training of different work-to-rest ratio. J Strength Cond Res 2019;33:399–407. doi: 10.1519/JSC.0000000000002074 [Crossref]
- Río-Rodríguez D, Iglesias-Soler E, Olmo MF. Set configuration in resistance exercise: Muscle fatigue and cardiovascular effects. PLoS One 2016;11:1–18. doi: 10.1371/journal.pone.0151163 [Crossref]
- Mayo X, Iglesias-Soler E, Fariñas-Rodríguez J, Fernández-Del-Olmo M, Kingsley JD. Exercise type affects cardiac vagal autonomic recovery after a resistance training session. J Strength Cond Res 2016;30:2565–73. doi: 10.1519/JSC.0000000000001347 [Crossref]
- Mayo X, Iglesias-Soler E, Carballeira-Fernández E, Fernández-Del-Olmo M. A shorter set reduces the loss of cardiac autonomic and baroreflex control after resistance exercise. Eur J Sport Sci. 2016;16:996–1004. doi: 10.1080/17461391.2015.1108367 [Crossref]
- Matsudo S, Araújo T, Matsudo V, Andrade D, Andrade E, Oliveira LC, et al. Questionário internacional de atividade física (ipaq): estudo de validade e reprodutibilidade no Brasil. Revista Brasileira de Atividade Física & Saúde 2001;6:5–18. doi: 10.12820/RBAFS.V.6N2P5-18 [Crossref]
- Heyward VHSLM. Avaliação da composição corporal
aplicada: fundamentos da composição corporal. São Paulo: Editora Ma; 2000.
- Lagally KM, Robertson RJ. Construct validity of the OMNI Resistance Exercise Scale. J Strength Cond Res. 2006;20:252–6. doi: 10.1519/R-17224.1 [Crossref]
- Baechle TR, Earle RW.
Essentials of strength
training and conditioning.
NSCA -National Strength
& Conditioning Association;
2000.
- Lagally KM, Robertson RJ. Construct validity of the OMNI resistance exercise scale. J Strength Cond Res. 2006;20:252–6. doi: 10.1519/R-17224.1 [Crossref]
- Mendes-Pinto D, Rodrigues-Machado MG. Aplicabilidade dos marcadores de rigidez arterial na doença arterial periférica. J Vasc Bras. 2019;18:1–9. doi: 10.1590/1677-5449.009318 [Crossref]
- Paulo CA, Roschel H, Ugrinowitsch C, Kobal R, Tricoli V. Influence of different resistance exercise loading schemes on mechanical power output in work to rest ratio – equated and – nonequated conditions. J Strength Cond Res. 2012;26:1308–12. doi: 10.1519/JSC.0b013e31822e89d0 [Crossref]
- Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15:155–63. doi: 10.1016/J.JCM.2016.02.012 [Crossref]
- Polito MD, Farinatti PDTV. Comportamento da pressão arterial após exercícios contra-resistência: Uma revisão sistemática sobre variáveis determinantes e possíveis mecanismos. Rev Bras Med Esporte. 2006;12:386–92. doi: 10.1590/s1517-86922006000600017 [Crossref]
- Halliwill JR, Buck TM, Lacewell AN, Romero SA. Postexercise hypotension and sustained postexercise vasodilatation: What happens after we exercise? Exp Physiol. 2013;98:7–18. doi: 10.1113/expphysiol.2011.058065 [Crossref]
- MacDougall JD, Tuxen D, Sale DG, Moroz JR, Sutton JR. Arterial blood pressure response to heavy resistance exercise. J Appl Physiol. 1985;58:785–90. doi: 10.1152/jappl.1985.58.3.785 [Crossref]
- Williams MA, Haskell WL, Ades PA, Amsterdam EA, Bittner V, Franklin BA, et al. Resistance exercise in individuals with and without cardiovascular disease: 2007 update: A scientific statement from the American Heart Association Council on Clinical Cardiology and Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2007;116:572–84. doi: 10.1161/CIRCULATIONAHA.107.185214 [Crossref]
- Mendes R, Themudo Barata JL. Envelhecimento e pressão arterial. Acta Med Port. 2008;21:193–8.