Rev Bras Fisiol Exerc.
2024;23(3): e235594
OPINION
Physical fitness as a vital sign: why are we not using it in clinical
practice?
Aptidão física como
sinal vital: por que não a utilizamos na prática clínica?
Dahan da Cunha Nascimento,
Bruno Viana Rosa, Karla Helena Coelho Vilaça e Silva
Universidade Católica de
Brasília, Brasília, DF, Brazil
Received 2024 May 2; Accepted
2024 Oct 14
Correspondence: Dahan da Cunha Nascimento, E–mail: dahanc@hotmail.com
How to cite
Nascimento DC, Rosa BV, Silva
KHCV. Physical fitness as a vital sign:
why are we not using it in clinical practice? Rev Bras Fisiol
Exerc. 2024;23(3):e235594. doi:
10.33233/rbfex.v23i3.5594
Abstract
Physical inactivity can be considered a disease of the 21st century. Among
several physical parameters, strength and cardiorespiratory fitness stand out
as they are strongly associated with mortality and chronic diseases. Thus, we
propose that physical fitness can be used as a vital sign and that strength and
cardiorespiratory fitness can be applied to assess health in practice. This can
be accomplished using muscular strength cutoff points for the elderly, such as
< 32 kg for men and < 21 for women, using a manual dynamometer, and <
40% of body weight in isometric knee extension. Likewise, several maximal and
submaximal tests, such as a 12-minute running test or step test, can be used as
a low-cost alternative for assessing cardiorespiratory fitness. Therefore, the
assessment of physical fitness parameters can be a promising and low-cost
screening tool to identify participants at risk of disability, chronic
non-communicable diseases and survival prognosis.
Keywords: muscle strength; cardiorespiratory fitness; public
health
Resumo
A inatividade física pode
ser considerada como uma doença do século XXI. Dentre diversos parâmetros
físicos, a força e a aptidão cardiorrespiratória se destacam por estarem
fortemente associadas a mortalidade e doenças crônicas. Dessa forma, propomos
que a aptidão física possa ser utilizada como sinal vital e que força e aptidão
cardiorrespiratória podem ser aplicadas para avaliar a saúde na prática. Isso
pode ser realizado utilizando os pontos de corte de força muscular para idosos,
como < 32 kg para homens e < 21 para mulheres, com uso de dinamômetro
manual, e < 40% do peso corporal na extensão isométrica de joelho. Da mesma
forma, diversos testes máximos e submáximos, como teste de 12 minutos de
corrida ou teste de degrau, podem ser utilizados como alternativa de baixo
custo para avaliação de aptidão cardiorrespiratória. Portanto, a avaliação de
parâmetros da aptidão física podem ser ferramenta de triagem promissora e de
baixo custo para identificar participantes com risco de incapacidade, doenças
crônicas não transmissíveis e prognóstico de sobrevivência.
Palavras-chave: força muscular; aptidão
cardiorrespiratória; saúde pública
Introduction
Physical inactivity and sedentary behavior are the
diseases of the 21st century, which have been linked to chronic
non-communicable diseases (NCDs) such as hypertension, type 2 diabetes, cancer,
and depression [1,2,3,4,5]. It is estimated that, between 2020 and 2023, 500 million
preventable NCDs will occur due to physical inactivity, with 47% being
attributed to hypertension and 43% to depression [6].
However, physical inactivity is still undervalued in
public health and clinical medicine and not given the same importance as
traditional risk factors such as hypertension, obesity, diabetes, and high
cholesterol [2].
It is crucial to consider evaluating components of
physical fitness such as cardiorespiratory, morphological, muscular, metabolic,
and motor in clinical practice. Traditionally, the American College of Sports
Medicine (ACSM) considers strength, flexibility, and cardiorespiratory fitness
as components of health-related physical fitness [7]. However, flexibility does
not seem to be an efficient predictor of cardio-metabolic health and mortality,
despite being beneficial for joint mobility [8].
On the other hand, low levels of muscle strength have
been identified as a predictor of all-cause mortality, functional,
psychological, and social health in the elderly population [9,10,11]. Similarly,
low levels of cardiorespiratory fitness increase the risk of cardiovascular
mortality, cancer mortality in men, and coronary heart disease in both sexes
[2,12,13].
Therefore, we propose the use of physical fitness
components as a vital sign and suggest how strength and cardiorespiratory
fitness can be applied to assess health in clinical practice.
Muscle strength as a vital sign
Muscle strength is a stronger predictor of death than
traditional risk factors such as systolic blood pressure [14]. Furthermore,
high levels of muscular strength are significantly associated with a lower risk
of all-cause mortality in hypertensive men, even after controlling for
potential confounders such as age, physical activity, smoking, alcohol intake,
body mass index, systolic and diastolic blood pressure, total cholesterol,
diabetes, abnormal electrocardiogram, family history of cardiovascular disease,
and cardiorespiratory fitness [14,15].
It is comprehensible that low levels of muscular strength
and cardiorespiratory fitness are independent predictors of cardiovascular
hospitalizations, mortality due to suicide, and all-cause mortality.
Furthermore, hospital costs are approximately 20% more expensive in patients
with lower strength, even after controlling for factors such as malnutrition,
patient characteristics, and disease severity [16].
Therefore, the use of cut-off points already displayed in
the scientific literature should be included in clinical practice for older
participants, adults, and children. For older participants, a handgrip strength
of less than 32 kg for men and less than 21 kg for women has been found to be
the best probability of identifying mobility limitations among older adults in
Brazil [17].
However, for measuring mobility, it seems more intuitive
to measure lower limb strength as it has a lower correlation with physical
performance tests related to mobility and a low correlation with handgrip
strength and low correlation with lower limb strength [18,19,20,21,22]. This low
correlation is due to the fact that the lower limb has a greater loss of
strength when compared to the upper limb [23].
Therefore, the test of sitting and standing up from a
chair can be used, as the inability to perform the test or taking more than 15
seconds to complete the test is a good indicator of mobility limitation [24].
Another possibility is to verify isometric knee extension strength, as having a
strength of 40% of body weight (sensitivity was 85.7% and specificity was
82.4%) is a reliable target to verify independence of older participants to
rise from a chair without using upper limbs [25].
In addition to the elderly, populations of other ages,
such as children, adolescents and adults, also have reference values for muscle
strength proposed by several studies [26]. However, for children, studies are
even more necessary to identify reference values normalized by body mass or
height, as these parameters are the ones that most influence the muscular
strength of this population and not necessarily age [27].
Furthermore, it is already established that low strength
in the elderly and adults is a risk factor for mortality from all causes, but
there are few longitudinal studies to show how low strength in childhood and
adolescence could harm you throughout your life.
Cardiorespiratory fitness as a vital sign
Cardiorespiratory fitness is normally measured through VO2max, which is the maximum
capacity to capture, transport and use oxygen [28]. It is an extremely important
measure for cardiovascular health,
being independently associated with mortality from all causes, cancer, and heart disease.
An increase of one metabolic equivalent (MET) in VO2max can reduce the risk
of coronary heart disease by 13% and 15% [29].
There are several ways to measure cardiorespiratory
fitness, the gold standard being ergospirometry - the maximum effort is
performed using a portable gas analyzer [7]. However, this material involves
high cost and specialized human material; indirect tests can offer a valid and
alternative way of measuring VO2max. Therefore, several maximum or submaximal
tests, which generally associate a certain oxygen consumption with a load,
heart rate or time, can be used for this purpose [30].
Among these tests, the 12-minute field tests (r = 0.79;
0.73-0.85) and 2400 m (r = 0.78, 0.72-0.83) have good validity and are
practical and cheap to be used on a daily basis by adults and children [28]. For the elderly, submaximal step tests, treadmill, or cycle ergometer
can be used
[31].
Conclusion
Thus, this opinion article raises the concern of not
utilizing the components of physical fitness, such as muscular strength and
cardiorespiratory fitness, in clinical medicine and clinical practice (Figure
1). These components can be used as a promising screening tool to identify
participants at risk of disability, NCDs, and survival prognosis
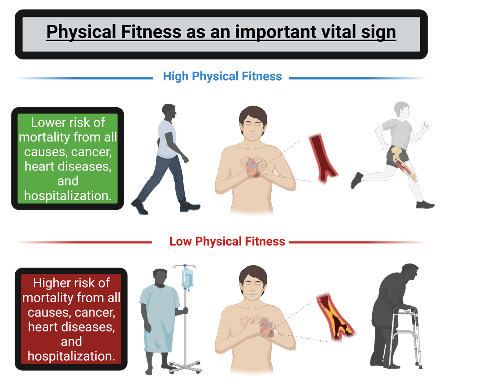
Created in
https://BioRender.com
Figure 1 - Physical fitness as an important vital sign
Conflicts of interest
There are no conflicts of interest.
Sources of funding
There was no funding.
Authors' contributions
Conception and design of the research: Nascimento DC; Manuscript writing: Nascimento DC; Critical
revision of the manuscript for important intellectual content: Rosa BV,
Silva KHCV
References
- Arocha Rodulfo
JL. Sedentary lifestyle a disease from XXI century. Clin Investig Arterioscler. 2019;31(5):233-40. doi: 10.3389/fpubh.2023.1304982 [Crossref]
- Blair SN. Physical inactivity: the biggest public health problem of the
21st century. Br J Sports Med. 2009;43(1):1-2.
- Milton K, Gomersall SR, Schipperijn J. Let's get moving: The Global Status Report on Physical Activity 2022 calls for urgent action. J Sport Health Sci. 2023;12(1):5 doi: 10.1016/j.jshs.2022.12.006 [Crossref]
- Myer GD, Faigenbaum AD, Stracciolini A, Hewett TE, Micheli LJ, Best TM. Exercise deficit disorder in youth: a paradigm shift toward disease prevention and comprehensive care. Curr Sports Med Rep. 2013;12(4):248-55. doi: 10.1249/JSR.0b013e31829a74cd [Crossref]
- Myers J, Prakash M, Froelicher V, Do D, Partington S, Atwood JE. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med. 2002;346(11):793-801. doi: 10.1056/NEJMoa011858 [Crossref]
- Organization WH. Global status report on physical activity 2022: World
Health Organization; 2022.
- Medicine ACoS.
Manual do ACSM para avaliação da aptidão física relacionada à saúde: Grupo Gen-Guanabara Koogan; 2011.
- Chodzko-Zajko WJ, Proctor DN, Fiatarone Singh MA, Minson CT, Nigg CR, et al. American College of Sports Medicine position stand. Exercise and physical activity for older adults. Med Sci Sports Exerc. 2009;41(7):1510-30. doi: 10.1249/MSS.0b013e3181a0c95c [Crossref]
- Carbone S, Kirkman DL, Garten RS, Rodriguez-Miguelez P, Artero EG, Lee DC, et al. Muscular Strength and Cardiovascular Disease: an updated state-of-the-art narrative review. J Cardiopulm Rehabil Prev. 2020;40(5):302-9. doi: 10.1097/HCR.0000000000000525 [Crossref]
- Ling CH, Taekema D, de Craen AJ, Gussekloo J, Westendorp RG, Maier AB. Handgrip strength and mortality in the oldest old population: the Leiden 85-plus study. CMAJ. 2010;182(5):429-35. doi: 10.1503/cmaj.091278 [Crossref]
- Newman AB, Kupelian V, Visser M, Simonsick EM, Goodpaster BH, Kritchevsky SB, et al. Strength, but not muscle mass, is associated with mortality in the health, aging and body composition study cohort. J Gerontol A Biol Sci Med Sci. 2006;61(1):72-7. doi: 10.1093/gerona/61.1.72 [Crossref]
- Lee CD, Blair SN. Cardiorespiratory fitness and smoking-related and total cancer mortality in men. Med Sci Sports Exerc. 2002;34(5):735-9. doi: 10.1097/00005768-200205000-00001 [Crossref]
- Ortega FB, Ruiz JR, Labayen I, Lavie CJ, Blair SN. The Fat but Fit paradox: what we know and don't know about it. Br J Sports Med. 2018;52(3):151-3. doi: 10.1136/bjsports-2016-097400 [Crossref]
- Leong DP, Teo KK, Rangarajan S, Lopez-Jaramillo P, Avezum A, Jr., Orlandini A, et al. Prognostic value of grip strength: findings from the Prospective Urban Rural Epidemiology (PURE) study. Lancet. 2015;386(9990):266-73. doi: 10.1016/S0140-6736(14)62000-6 [Crossref]
- Artero EG, Lee DC, Ruiz JR, Sui X, Ortega FB, Church TS, et al. A prospective study of muscular strength and all-cause mortality in men with hypertension. J Am Coll Cardiol. 2011;57(18):1831-7. doi: 10.1016/j.jacc.2010.12.025 [Crossref]
- Guerra RS, Amaral TF, Sousa AS, Pichel F, Restivo MT, Ferreira S, et al. Handgrip strength measurement as a predictor of hospitalization costs. Eur J Clin Nutr. 2015;69(2):187-92. doi: 10.1038/ejcn.2014.242 [Crossref]
- Delinocente MLB, de Carvalho DHT, Maximo RO, Chagas MHN, Santos JLF, Duarte YAO, et al. Accuracy of different handgrip values to identify mobility limitation in older adults. Arch Gerontol Geriatr. 2021;94:104347. doi: 10.1016/j.archger.2021.104347 [Crossref]
- Harris-Love MO, Benson K, Leasure E, Adams B, McIntosh V. The Influence of Upper and Lower Extremity Strength on Performance-Based Sarcopenia Assessment Tests. J Funct Morphol Kinesiol. 2018;3(4):53. doi: 10.3390/jfmk3040053 [Crossref]
- Martien S, Delecluse C, Boen F, Seghers J, Pelssers J, Van Hoecke AS, et al. Is knee extension strength a better predictor of functional performance than handgrip strength among older adults in three different settings? Arch Gerontol Geriatr. 2015;60(2):252-8. doi: 10.1016/j.archger.2014.11.010 [Crossref]
- Bohannon RW. Dynamometer measurements of grip and knee extension strength: are they indicative of overall limb and trunk muscle strength? Percept Mot Skills. 2009;108(2):339-42. doi: 10.2466/PMS.108.2.339-342 [Crossref]
- Felicio DC, Pereira DS, Assumpcao AM, de Jesus-Moraleida FR, de Queiroz BZ, da Silva JP, et al. Poor correlation between handgrip strength and isokinetic performance of knee flexor and extensor muscles in community-dwelling elderly women. Geriatr Gerontol Int. 2014;14(1):185-9. doi: 10.1111/ggi.12077 [Crossref]
- Rodacki ALF, Boneti Moreira N, Pitta A, Wolf R, Melo Filho J, Rodacki CLN, et al. Is handgrip strength a useful measure to evaluate lower limb strength and functional performance in older women? Clin Interv Aging. 2020;15:1045-56. doi: 10.2147/CIA.S253262. eCollection 2020 [Crossref]
- Samuel D, Wilson K, Martin HJ, Allen R, Sayer AA, Stokes M. Age-associated changes in hand grip and quadriceps muscle strength ratios in healthy adults. Aging Clin Exp Res. 2012;24(3):245-50. doi: 10.1007/BF03325252 [Crossref]
- Cesari M, Kritchevsky SB, Newman AB, Simonsick EM, Harris TB, Penninx BW, et al. Added value of physical performance measures in predicting adverse health-related events: results from the Health, Aging And Body Composition Study. J Am Geriatr Soc. 2009;57(2):251-9. doi: 10.1111/j.1532-5415.2008.02126.x [Crossref]
- Bohannon RW. Body weight-normalized knee extension strength explains sit-to-stand independence: a validation study. J Strength Cond Res. 2009;23(1):309-11. doi: 10.1519/JSC.0b013e31818eff0b [Crossref]
- Benfica PDA, Aguiar LT,
Brito SAF, Bernardino LHN, Teixeira-Salmela LF, Faria
C. Reference values for muscle strength: a systematic review with a descriptive meta-analysis. Braz J
Phys Ther.
2018;22(5):355-69. doi: 10.1016/j.bjpt.2018.02.006 [Crossref]
- McKay MJ, Baldwin JN, Ferreira P, Simic M, Vanicek N, Burns J, et al. N [Crossref]ormative reference values for strength and flexibility of 1,000 children and adults. Neurology. 2017;88(1):36-43. doi: 10.1212/WNL.0000000000003466 [Crossref]
- Taylor HL, Buskirk E, Henschel A. Maximal oxygen intake as an objective measure of cardio-respiratory performance. J Appl Physiol. 1955;8(1):73-80. doi: 10.1152/jappl.1955.8.1.73 [Crossref]
- Kodama S, Saito K, Tanaka S, Maki M, Yachi Y, Asumi M, et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA. 2009;301(19):2024-35. doi: 10.1001/jama.2009.681 [Crossref]
- Mayorga-Vega D, Bocanegra-Parrilla R, Ornelas M, Viciana J. Criterion-related validity of the distance- and time-based walk/run field tests for estimating cardiorespiratory fitness: a systematic review and meta-analysis. PLoS One. 2016;11(3):e0151671. doi: 10.1371/journal.pone.0151671 [Crossref]
- Smith AE, Evans H, Parfitt G, Eston R, Ferrar K. Submaximal exercise-based equations to predict maximal oxygen uptake in older adults: a systematic review. Arch Phys Med Rehabil. 2016;97(6):1003-12. doi: 10.1016/j.apmr.2015.09.023 [Crossref]