Rev Bras Fisiol Exerc.
2024;23(3):e235608
REVIEW
Relationship of heart failure and major depression disorder and the role of
physical exercise
Relação da
insuficiência cardíaca e transtorno de depressão maior e o papel do exercício
físico
Jéssica Oliveira Florentino1,2,
Wallace Machado Magalhães de Souza1,3, Renata Maria Begni Afonso1,4
1Instituto Superior de Ciências da Saúde
Carlos Chagas, Rio de Janeiro, RJ, Brazil
2Clinica Actus
Reabilitação e Condicionamento Físico, Rio de Janeiro, RJ, Brazil
3Instituto Estadual de Cardiologia
Aloysio de Castro, Rio de Janeiro, RJ, Brazil
4Universidade Federal do Rio de Janeiro,
Rio de Janeiro, RJ, Brazil
Received: November 13,
2024; Accepted: December
15, 2024.
Correspondence: Jéssica Oliveira Florentino, jesikaedf@gmail.com
How to cite
Florentino JO, Souza WMM, Afonso
RMB. Relationship of heart failure and major depression disorder and the role of
physical exercise. Rev Bras Fisiol Exerc. 2024;23:e235608. doi:
10.33233/rbfex.v23i3.5608
Abstract
Introduction: Heart Failure (HF) and Major Depressive Disorder (MDD)
are diseases with high incidence, leading to high rates of morbidity and
mortality. After the COVID-19 pandemic, around 11.5 million Brazilians were
diagnosed with MDD, and in 2022, 192,852 emergency hospitalizations were
registered in Brazil due to HF. The correlation between these two diseases is
so significant that one is considered a risk factor for the other, negatively
impacting the patients' quality of life. Objective: To conduct a
literature review of the physiological mechanisms associated with HF and MDD,
as well as the effect of physical exercise in alleviating the symptoms. Methods:
Narrative literature review with a search in the databases PubMed, Scientific
Electronic Library Online (SciELO), and Google Scholar. Results: Among
observational studies and clinical trials, seven articles were selected. The
main compensatory mechanisms related to these diseases are autonomic nervous
system dysfunction, elevation of inflammatory cytokines, reduction of nitric
oxide synthesis, and decreased cerebral blood flow. Aerobic training was
responsible for improving depression symptoms and cognitive function, without
significant changes in inflammatory biomarkers. Conclusion: There is a
strong association between HF and MDD. Strategies to mitigate the symptoms of
these diseases should be encouraged to improve the clinical outcomes of
patients. Physical exercise is important for the treatment of symptoms in
patients with HF affected by MDD, as it promotes improvements in clinical
outcomes related to both diseases.
Keywords: cardiovascular disease; depression; physical activity;
aerobic training.
Resumo
Introdução: A Insuficiência Cardíaca (IC) e o
Transtorno Depressão Maior (TDM) são doenças de elevada incidência, que geram
altas taxas de morbidade e mortalidade. Após a pandemia de COVID-19, cerca de
11,5 milhões de brasileiros foram diagnosticados com TDM e, em 2022, foram
registradas 192.852 internações de emergência no Brasil por IC. A correlação
entre essas duas doenças é tão significativa que uma é considerada fator de
risco para a outra, gerando impacto negativo na qualidade de vida dos
pacientes. Objetivo: Realizar uma revisão bibliográfica dos mecanismos
fisiológicos associados à IC e ao TDM, bem como o efeito do exercício físico na
atenuação dos sintomas. Métodos: Revisão bibliográfica narrativa com
busca nas bases de dados PubMed, Scientific
Electronic Library Online (SciELO) e Google
Acadêmico. Resultados:
Entre estudos observacionais e ensaios clínicos,
foram selecionados 7 artigos. Os principais mecanismos
compensatórios
correlatos dessas doenças são a disfunção
do sistema nervoso autonômico, a
elevação de citocinas inflamatórias,
diminuição da síntese de óxido
nítrico e a
redução do fluxo sanguíneo cerebral. O treinamento
aeróbico foi responsável por
melhorar os sintomas de depressão e a função
cognitiva, sem alteração
significativa dos biomarcadores inflamatórios. Conclusão: Existe uma
forte associação entre IC e TDM. Estratégias para mitigação dos sintomas dessas
doenças devem ser estimuladas para melhorar o desfecho clínico dos pacientes. O
exercício físico é importante para o tratamento dos sintomas de pacientes com
IC acometidos por TDM, pois promove melhorias nos desfechos clínicos
relacionados a ambas as doenças.
Palavras-chave: doença cardiovascular; depressão;
atividade física; treinamento aeróbico.
Introduction
Heart failure (HF) can be defined as a complex clinical syndrome in which the heart is
unable to pump blood to the
rest of the
body efficiently to meet tissue demand
or does so under high filling pressure. This condition is caused by structural or functional
dysfunctions with signs and symptoms of low cardiac output and high cardiac
filling pressure during exercise and rest [1].
Epidemiological data show that, in 2022, 192,852
emergency hospital admissions were performed for the treatment of HF in Brazil
[2], and the number of deaths among hospitalized patients was 23,855 in the
same year [3]. In addition, HF is associated with other adverse mental health
outcomes, such as depression and anxiety, which affect the individual's quality
of life [4].
Major Depressive Disorder (MDD) is characterized by the
continuation of five or more symptoms for at least two weeks, such as depressed
mood, lack of pleasure in activities that were previously pleasurable, fatigue,
thoughts of death, feelings of guilt, changes in sleep behavior, weight loss or
gain, difficulty concentrating, and psychomotor agitation [5].
MDD symptoms cause difficulty in social interaction and
interfere in areas of work, personal relationships, or other relationships in
which the individual is involved, causing suffering in personal life. When
performing their tasks, the person with a depressive episode makes an excessive
effort to maintain their functional and autonomic capacity [6].
Worldwide, the number of MDD cases continues to rise.
Before the COVID-19 pandemic, it was estimated that 193 million people had been
diagnosed with this disease; after the pandemic, this number reached 246
million. Brazil leads the ranking of South American countries with
approximately 11.5 million diagnosed cases [7].
Given this scenario of increasing illness from HF and
MDD, it is important to understand the physiological mechanisms that are
associated with these two pathologies and the strategies to alleviate the
symptoms of these diseases to obtain a better clinical outcome. Among the
non-pharmacological strategies to control the symptoms of both HF and MDD,
physical exercise is quite notable [8,9]. Thus, the main objective of this
study is to review the pathophysiological mechanisms of HF and MDD and their
interrelationship, in addition to demonstrating the effect of physical exercise
on mental health, that is, on improving mood, cognitive capacity, reducing
depressive symptoms, psychomotor speed and independence in performing tasks in
patients with HF affected by MDD.
Methods
The research design used in this study was a narrative
bibliographic review with searches in the PubMed, Scientific Electronic Library
Online (SciELO), and Google Scholar databases, using the following keywords:
heart failure; depression; physical exercise; physical activity; strength
training; aerobic training and combined training. The search took place from
May 29, 2023, to June 2, 2023, and articles in Portuguese and English published
in the last 5 years were included.
Results
Seven articles were selected, including observational
studies and clinical trials (Table I).
Table I – Summary of articles selected for review
Discussion
The impairment in HF goes beyond the heart, since
cognitive damage is present in a large proportion of these patients [14]. With
cognitive impairment, the patient's perception of self-care is impaired, which
directly affects their independence: maintaining a balanced diet, taking
medication correctly, and independently perceiving the worsening of their
health status. As age and HF increase, the performance of executive function
worsens, causing impairments in memory, psychomotor speed, and visual memory
[11].
The cognitive deficit of individuals with HF, when
compared to a healthy group and with other comorbidities, showed worse results
in memory, psychomotor speed, and executive function [11]. The severity of HF
and advanced age are risk factors for cognitive deterioration, as is the male
gender [12].
Low cardiac output, production of inflammatory
substances, and vascular hypotension are factors that reduce cerebral blood
flow and compromise cognitive areas (Figure 1).
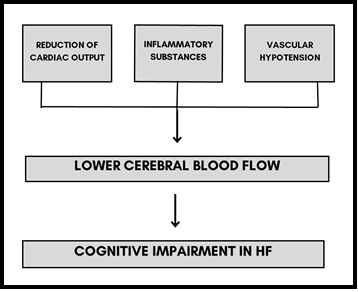
Adapted from Leto & Feola, 2014 [17]
Figure 1 – Physiological mechanisms contributing to cognitive
impairment in heart failure
The increase in inflammatory cytokines, such as tumor
necrosis factor-alpha (TNF-α), interleukin-6 (IL-6), brain natriuretic
peptide (BNP), and asymmetric dimethylarginine (ADMA), present in individuals
with MDD, increases the risk of endothelial injury, development of thrombi and
increased risk of stroke [18]. Another change in MDD is the reduction in the
bioavailability of nitric oxide, which may be associated with the formation of
atherosclerosis due to the increase in nitric oxide inhibitors and the cell
reduction that contributes to endothelial repair and angiogenesis [19].
The association of cognitive impairment with severe HF
presents a higher risk of mortality [11]. Regarding the severity of the
disease, MDD is associated with a greater number of hospitalizations and
mortality, regardless of the LVEF condition. In patients with depressive
symptoms and HF with reduced LVEF, the mortality rate and hospitalizations
related to heart disease were 55% higher compared to other patients with the
same condition of HF with reduced LVEF without depressive symptoms [20].
Physical exercise is indicated for both the prevention
and treatment of HF and MDD. Participation in a regular physical exercise
program positively impacts the lives of patients with these comorbidities,
improving well-being and self-care [21]. Treatment with physical exercise in
MDD is recommended because it reduces stress levels, improves sympathovagal
balance, stimulates new synapses, increases the hippocampus, and synthesizes
Brain-Derived Neurotrophic Factor (BDNF), which acts on the brain and stimulates
neurogenesis [22].
BDNF is an important marker for heart and brain health.
It plays a role in endothelial health, in addition to generating a positive
effect on angiogenesis. In the brain, BDNF contributes positively to brain
plasticity, associated with a lower risk of neurodegenerative diseases.
Physical exercise is capable of increasing BDNF levels, protecting the brain
from possible cognitive damage. In cardiac function, increased BDNF reduces
cardiovascular risk associated with physical activity and cardiorespiratory fitness
[23].
The practice of physical exercise is important for
psychological responses in patients with HF. Ducan et al. [10] evaluated
the psychological responses generated by physical exercise, combining aerobic
training and muscular resistance, and observed improvements in self-efficacy
for physical exercise in the first three weeks of exercise. Those who performed
more physical exercise over 24 weeks showed better results in levels of
depression, self-efficacy, and confusion.
Abdelbasset & Alqahtani [15] evaluated the effect of
continuous moderate-intensity aerobic training on symptoms of depression in
individuals with HF. For 12 weeks, the intervention group performed three
sessions of 40 to 50 minutes of walking between 60 and 70% of HRmax; the
control group received recommendations for performing home activities,
relaxation, and self-care. There was a reduction in the depression scale in
both groups, but the group that performed physical exercise reduced it by 81%
compared to 46% in the control group.
When comparing the effect of different intensities of
aerobic exercise on the level of depressive disorders in patients with HF,
Abdelbasset et al. [13] divided the sample into three groups: Group 1:
Started with 6 weeks of low-intensity aerobic training (40 to 50% HRmax) and
progressed to another 6 weeks of moderate-intensity aerobic training (50 to 70%
of HRmax) lasting 20 to 30 minutes. Group 2: Performed 12 weeks of continuous
moderate-intensity aerobic training (60 to 70% of HRmax). Group 3 received only
guidance on home activities and self-care. The groups that performed physical
exercise, regardless of intensity, presented similar positive results, with no
significant difference in depression rates.
The effect of physical exercise on MDD symptoms and
cognitive function in patients with HF was assessed in groups that performed
physical exercise for 16 weeks, with two weekly 60-minute sessions of Tai Chi
Chuan training, elastic resistance training, or the control group (no
exercise). The results found reinforce the positive effect of physical exercise
on cognitive function and symptoms of depression without altering inflammatory
levels [16]. The main limitation of this study was the scarcity of articles that
evaluated different types of physical exercise on MDD symptoms in patients with
HF. For example, the benefit of strength training in improving functional
capacity, increasing muscle strength, improving quality of life, and reducing
the risk of mortality in patients with HF is well established [24]. However,
studies using this type of training to evaluate the attenuation of depressive
symptoms in patients with HF are incipient.
Conclusion
HF and MDD are strongly correlated, and their deleterious
effects negatively impact the quality of life, hinder treatment adherence, and
contribute to the high mortality resulting from these diseases. The main
correlated pathophysiological mechanisms are dysfunction of the autonomic
nervous system, reduction of nitric oxide, and blood flow, which may contribute
to the worsening of HF and the development of MDD.
Low and moderate-intensity aerobic exercise is beneficial
for reducing MDD symptoms in patients with HF. In addition to aerobic training,
exercises such as Tai Chi Chuan and elastic resistance have shown positive
results in reducing symptoms of depression. The use of these exercises as a
non-pharmacological treatment has been shown to be effective for individuals
with HF and MDD. Further studies with different training modalities (e.g.,
strength training) are needed to evaluate MDD symptoms in patients with HF.
Academic affiliation
This article was developed based on the final work by
Jéssica Oliveira Florentino of the Lato Sensu Postgraduate Program in Cardiac
Rehabilitation for graduates in Physical Education of the Carlos Chagas Higher
Institute of Health Sciences (IPGMCC)
Conflict of interest
No conflict of interest was reported by the authors in
the publication of this study
Sources of funding
There were no external sources of funding for this study
Authors' contributions
Conception and design of the research: Florentino JO, Souza WMM; Obtaining data: Florentino JO, Souza
WMM; Data analysis and interpretation: Florentino JO, Souza WMM; Manuscript
writing: Florentino JO, Souza WMM; Critical revision of the manuscript
for important intellectual content: Begni RM
References
- Rohde LEP, Montera
MW, Bocchi EA, Clausell NO, Albuquerque DC, Rassi S,
et al. Diretriz brasileira de insuficiência cardíaca crônica e aguda. Arq Bras Cardiol.
1o de setembro de 2018;111(3):436–539. doi: 10.5935/abc.20180190 [Crossref]
- DATASUS. Procedimentos
hospitalares do SUS - por local de internação - Brasil [Internet].
tabnet.datasus.gov.br. [cited 2024 May 15].
Disponível em: http://tabnet.datasus.gov.br/cgi/tabcgi.exe?sih/cnv/qiuf.def
- DATASUS. Procedimentos
hospitalares do SUS - por local de internação, óbitos segundo procedimento -
Brasil [Internet]. tabnet.datasus.gov.br. [cited 2024
May 15]. Disponível em:
http://tabnet.datasus.gov.br/cgi/tabcgi.exe?sih/cnv/qiuf.def
- Dekker RL, Lennie TA, Doering L V, Chung ML, Wu JR, Moser DK. Coexisting anxiety and depressive symptoms in patients with heart failure. Eur J Cardiovasc Nurs. 2014;13(2):168–76. doi: 10.1016/j.pcad.2021.10.003 [Crossref]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5). 5th ed. American Psychiatric
Publishing; 2013.
- Laks J, Deslandes
AC, Helena M. Exercício físico, envelhecimento e saúde mental. Rio de Janeiro:
Instituto Vital Brazil, Centro de Estudo e Pesquisa
do Envelhecimento (CEPE), Instituto de Psiquiatria UFRJ FAPERJ; 2014
- World Health Organization. Depression and Other Common Mental Disorders
Global Health Estimates [Internet]. 2017.
[cited 2024 May 15]. Disponível em:
https://iris.who.int/bitstream/handle/10665/254610/WHO-MSD-MER-2017.2-eng.pdf?sequence=1
- Wheat HL, Fedson S, Bozkurt B, Josephson RA. Cardiac rehabilitation in heart failure: Indications for exercise training based on heart failure phenotype. Prog Cardiovasc Dis. 2022;70:16–21. doi: 10.1016/j.pcad.2021.10.003 [Crossref]
- Zhao J, Jiang W, Wang X, Cai Z, Liu Z, Liu G. Exercise, brain plasticity, and depression. CNS Neurosci Ther. 2020;26(9):885–95. doi: 10.1111/cns.13385 [Crossref]
- Duncan K, Pozehl B, Hertzog M, Norman JF. Psychological responses and adherence to exercise in heart failure. Rehabil Nurs. 2014;39(3):130–9. doi: 10.1002/rnj.106 [Crossref]
- Pressler SJ, Subramanian U, Kareken D, Perkins SM, Gradus-Pizlo I, Sauvé MJ, et al. Cognitive deficits in chronic heart failure. Nurs Res. 2010;59(2):127–39. doi: 10.1097/NNR.0b013e3181d1a747 [Crossref]
- Pressler SJ, Kim J, Riley P, Ronis DL, Gradus-Pizlo I. Memory dysfunction, psychomotor slowing, and decreased executive function predict mortality in patients with heart failure and low ejection fraction. J Card Fail. 2010;16(9):750–60. doi: 10.1016/j.cardfail.2010.04.007 [Crossref]
- Abdelbasset WK, Alqahtani BA, Alrawaili SM, Ahmed AS, Elnegamy TE, Ibrahim AA, et al. Similar effects of low to moderate-intensity exercise program vs moderate-intensity continuous exercise program on depressive disorder in heart failure patients: A 12-week randomized controlled trial. Medicine (United States). 2019;98(32). doi: 10.1097/MD.0000000000016820 [Crossref]
- Bandeira GMS, Flores PVP, Alencar PC, Jardim PP, Tinoco JMVP, Cavalcanti ACD. Avaliação da função cognitiva de pacientes com insuficiência cardíaca crônica: estudo transversal. Online Braz J Nurs 22 de junho de 2020;18(4). doi: 10.17665/1676-4285.20196327 [Crossref]
- Abdelbasset WK, Alqahtani BA. A randomized controlled trial on the impact of moderate-intensity continuous aerobic exercise on the depression status of middle-aged patients with congestive heart failure. Medicine (United States). 2019;98(17). doi: 10.1097/MD.0000000000015344 [Crossref]
- Redwine LS, Pung MA, Wilson K, Bangen KJ, Delano-Wood L, Hurwitz B. An exploratory randomized sub-study of light-to-moderate intensity exercise on cognitive function, depression symptoms and inflammation in older adults with heart failure. J Psychosom Res. 2020;128. doi: 10.1016/j.jpsychores.2019.109883 [Crossref]
- Leto L, Feola M. Cognitive impairment in heart failure patients. Vol. 11, J Geriatric Cardiol. 2014(11):316–28. doi: 10.11909/j.issn.1671-5411.2014.04.007 [Crossref]
- Sbolli M, Fiuzat M, Cani D, O’Connor CM. Depression and heart failure: the lonely comorbidity. Eur J Heart Fail. 2020;22(11):2007–17. doi: 110.1002/ejhf.1865 [Crossref]
- Rashid S, Qureshi AG, Noor TA, Yaseen K, Sheikh MAA, Malik M, et al. Anxiety and depression in heart failure: an updated review. Curr Probl Cardiol. 2023;48(11):101987. https://doi.org/10.1016/j.cpcardiol.2023.101987 [Crossref]
- Newhouse A, Jiang W. Heart failure and depression. Heart Fail Clin. 2014;10(2):295–304. https://doi.org/10.1016/j.hfc.2013.10.004 [Crossref]
- Cardoso G, Trancas B, Luengo
A, Reis D. Insuficiência cardíaca e depressão: uma associação com relevância
clínica [8] [Internet]. [citado 2024 Out 30]. Disponível em:
https://repositorio.hff.min-saude.pt/bitstream/10400.10/162/1/Cardoso.pdf
- Sanches A, Costa R, Marcondes FK, Cunha TS. Relationship among stress, depression, cardiovascular and metabolic changes and physical exercise. Fisioter Mov. 2016;29(1):23–36. https://doi.org/10.1590/0103-5150.029.001.AO02 [Crossref]
- Trombetta IC, DeMoura JR, Alves CR, Carbonari-Brito R, Cepeda FX, Lemos JR. Níveis Séricos do BDNF na Proteção Cardiovascular e em Resposta ao Exercício. Arq Bras Cardiol. 2020;115(2):263–9. https://doi.org/10.36660/abc.20190368 [Crossref]
- Giuliano C, Karahalios A, Neil C, Allen J, Levinger I. The effects of resistance training on muscle strength, quality of life and aerobic capacity in patients with chronic heart failure — A meta-analysis. Int J Cardiol. 2017(227):413–23. https://doi.org/10.1016/j.ijcard.2016.11.023 [Crossref]